Abstract
To elucidate the accuracy, efficacy, and safety of percutaneous iliosacral screw (ISS) and trans-iliac trans-sacral screw (TITS) insertion using a single C-arm fluoroscopy intensifier. Additionally, the potential risk factors that might cause mal-positioned screws were identified. Patients with pelvic ring injuries who underwent percutaneous screw fixation in a single medical institute were divided into an ISS group (n = 59) and a TITS group (n = 62) and assessed. The angles deviated from ideal orientation (ADIO) of the implanted screw were measured, and potential risk factors for mal-positioned screws were analyzed. Overall, the reduction quality of the pelvic ring was good or excellent in 70 patients (82.4%) by Matta’s criteria and in 48 patients (56.5%) by Lefaivre’s criteria. ADIO measurements of the ISS and TITS groups via multi-planar computed tomography were 9.16° ± 6.97° and 3.09° ± 2.8° in the axial view, respectively, and 5.92° ± 3.65° and 2.10° ± 2.01° in the coronal view, respectively. Univariate statistical analysis revealed body mass index as the single potential risk factor of mal-positioned screws. With careful preoperative planning and intraoperative preparations, placing ISS and TITS under the guidance of single C-arm fluoroscopy intensifier is a reliable and safe technique. Caution should be exercised when performing this procedure in patients with a high body mass index.
Similar content being viewed by others
Introduction
Pelvic fractures represent 5–9.3% of all traumatic fractures, and 10–20% of poly-traumatized patients have pelvic fractures1,2,3. The treatment of pelvic fracture can be challenging, owing to the complexity of fracture patterns, individual anatomical variations, and nearby vital structures4. As the posterior pelvic ring provides 60–70% of the stability of the pelvis, anatomical reduction with adequate fixation is crucial in cases with posterior pelvic ring injury5. Therefore, the operative strategy for pelvic ring injury should be individualized and optimized according to each patient’s clinical presentation, including options of surgical approach, choice of implants, and the operation setting.
Since restoring pelvic anatomy and providing sufficient stability of the posterior pelvic ring are the keystones of treatment of pelvic ring injury, anatomical reduction should be performed prior to osteosynthesis. After achieving reduction of the fracture, by either closed or open methods, there are several options to maintain the reduction, reduce the gap, and achieve stability6,7,8. Among the fixation choices, percutaneous screw fixation via either closed or open reduction is usually preferred because it is less invasive, has minimal blood loss, a shorter surgical time, and adequate stability9,10,11. Despite its advantages, several concerns persist regarding this percutaneous technique, including the disadvantages of frequent X-rays, great cumulative radiation exposure, high screw position error rate, and nerve injury12,13,14.
Percutaneous treatment for posterior pelvic ring was first described by Matta et al. in 1980s15. The original description of the method was conducted under real-time image examination by a single-arm fluoroscopic intensifier. Since that time, several real-time image modifications have been proposed to improve the accuracy and safety of this technique, such as 2-arm fluoroscopy, O-arm fluoroscopy, intraoperative computed tomography, and navigation system16,17,18,19. Although reports from these new image-assisted surgery have revealed their efficacies, the advanced image tools are expensive and not routinely available to each orthopedic surgeon and facility. Therefore, the usefulness of these advanced image tools for the percutaneous treatment of posterior pelvic ring may be limited.
The aim of this study was to report the surgical outcomes using the most commonly available intraoperative image evaluation, the single fluoroscopic intensifier, in treating posterior pelvic ring injuries by either iliosacral screw (ISS) or trans-iliac trans-sacral screw (TITS) insertion. Additionally, the risk factors of potentially mal-positioned screws were evaluated.
Materials and methods
Patient enrollment
We retrospectively collected patients’ medical records from the fracture registration database of our institute to identify those who were diagnosed with pelvic ring injury and underwent percutaneous screws fixation (ISS, TITS, or both) either through closed reduction and internal fixation or open reduction and internal fixation (ORIF) between January 2017 and June 2020. The medical records and pre- and postoperative radiological images were meticulously reviewed. All the operative procedures were performed with an established operative protocol by a single surgeon (Y.-H.Y.). The review process was approved by the Chang Gung medical foundation institutional review board (IRB No. 202100620B0).
Resuscitation and perioperative protocol
The patients were sent to the emergency department (ED) directly from trauma scenes or transferred from primary medical institutes. Advanced Trauma Life Support® resuscitation protocol was followed in the ED, and then patients were transferred to the ordinary ward or intensive care unit, as required. Osteosynthesis for the pelvic fracture was performed immediately after the patient was hemodynamically stabilized. Image examinations, including X-rays [anteroposterior (AP), inlet, and outlet views] and multi-planar computed tomography (mpCT), were required for preoperative planning. Subsequently, the rehabilitation protocol was individualized according to the patient’s concomitant injuries and fractures. Similar postoperative image examinations were performed to examine the reduction quality of the pelvic ring and the position of the implants.
Operative technique
Patients were positioned in supine or prone position, according to the planned procedures and the concomitant injuries observed on a radiolucent table (Modular Table System; Mizuho OSI, California, USA) under general anesthesia. In patients for whom a prone position was contraindicated because of concomitant injuries or anesthesia requirements, a supine position was preferred. However, a prone position was necessary for ORIF of posterior pelvic ring injuries, such as dislocated sacroiliac joint and vertical displacement of the sacral fracture. The osteosynthesis strategy for anterior and posterior pelvic ring injury could be performed simultaneously or sequentially. Posterior pelvic ring reduction and fixation was always performed prior to anterior pelvic ring procedure, except in cases with pelvic ring injury to AO B2.120 with significant internal rotational deformity of the affected hemipelvis.
AP, inlet, outlet, 2 Judet views, and sacrum lateral views were examined prior to surgical draping to ensure that all the images could be obtained clearly without limitations. The intraoperative images were obtained from a single-arm fluoroscopic intensifier (Ziehm Solo; Ziehm Imaging GmbH, Nuremberg, Germany). The ideal orientation of the ISS was perpendicular to the sacroiliac joint, whereas that for TITS was parallel to the groundline. After the position and orientation of the K-wire was confirmed, a 7.0-mm cannulated screw (Cannulated Screw 7.0 mm; Syntec Technology Co., Hsinchu, Taiwan) was applied as the target implant. All images were examined repeatedly throughout the procedures. Moreover, the radiation dose and time were recorded thoroughly during percutaneous screw osteosynthesis.
Analysis of screw placement and reduction quality of the pelvis
Standard X-rays (AP, inlet, outlet views) and mpCT were obtained postoperatively for each patient. Radiological interpretations were performed by two independent medical doctors (J.-P.C. and P.-J.T.), who were not involved in the surgeries, using the PACS system (Centricity Enterprise Web V3.0; GE Healthcare, Chicago, USA).
The morphology variability of the sacrum, in terms of sacral dysmorphism, was examined prior to osteosynthesis. We adapted the criteria by Routt21 to define a dysmorphic sacrum which are the signs from X-rays, including (1) mammillary bodies; (2) tongue-in-groove morphology; (3) collinearity; (4) dysmorphic neural foramina; (5) residual sacral disc space. When the sacral dysmorphism was anticipated from preoperative image evaluation, percutaneous osteosynthesis by TITS would be applied more frequently than that by ISS because of the narrow corridor of S1.
Several classifications and grading systems for fracture pattern, reduction quality evaluation, and screw positions were adapted in this study. We classified the fracture pattern according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) system or pelvic ring injury20. For those fractures with sacral involvements, the Denis classification were applied22. The reduction qualities of the pelvic ring injuries were evaluated from the pelvic AP, inlet, and outlet X-rays, and axial and coronal views of the mpCT. We adapted the criteria from Matta and Tornetta for vertical reduction quality15,23 and from Lefaivre for symmetrical reduction quality24. Accordingly, we classified the reduction quality of the pelvic ring injury as excellent, good, fair, or poor.
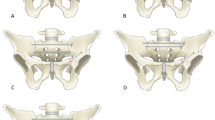
For ISS, we collected the angles between the screw and sacroiliac joint obtained in the axial and coronal views of the mpCT. The angular differences between the implanted screw and the ideal orientation of the ISS, which should be perpendicular to the sacroiliac joint in each view, were measured and termed as the angles deviated from ideal orientation (ADIO) (Fig. 1A). For TITS, the angular difference between the implanted screw and the ideal orientation, which should be parallel to the groundline in both axial and coronal views of the mpCT scan, were recorded (Fig. 1B).
(A) The ideal angles between ISS (line S) and sacroiliac joint (line J) are 90° in both the axial and coronal views. The actual angles deviated from these ideal orientations are defined as the ADIO of ISS. (B) In both axial and coronal views, the ideal angle between TITS (line S) and groundline (line C) is 0°. The actual angles deviated from these ideal orientations are defined as the ADIO of TITS. ISS iliosacral screw, TITS trans-iliac trans-sacral screw, ADIO angle deviated from ideal orientation.
To qualitatively define mal-positioned ISS and TITS, a screw that penetrated, encroached, or touched the neuroforamina of the sacrum or a newly appeared postoperative neurological deficit was defined as a mal-positioned screw, and Smith’s grading system (Table 1), which classified the position of the screw from grade 0 to 3, was applied to quantify those with mal-positions25.
Statistical analysis
The Chi-square test or the Fisher’s exact test was used where appropriate to analyze categorical data. Nonparametric Mann–Whitney U test was applied for between-group comparisons in numerical data. Logistic regression was applied for analysis of risk factors. Statistical significance was defined as p < 0.05. Statistical analysis was carried out by SPSS 24.0 program for Windows (IBM SPSS Statistics for Windows, Version 24.0; IBM Corp, NY, USA).
Ethics approval and consent to participate
Informed consent was obtained from all subjects and approval from the Chang Gung medical foundation institutional review board (202100620B0) was acquired. All methods were performed in accordance with Declaration of Helsinki.
Results
Demographics
From January 2017 to June 2020, 85 patients with a mean age of 39 ± 19 were included in this study. We divided the enrolled patients into two groups: ISS and TITS. Among the 59 cases in the ISS group, 47 had an AO type B injury and 12 had a type C injury. Meanwhile, among the 62 patients in the TITS group, there was 1 with AO type A injury, 48 with type B injury, and 13 with type C injury. Thirty-six patients received both ISS and TITS treatments. Twenty-four patients had diastatic sacroiliac joints, 17 of whom received open reduction (70.8%). Eight patients were found to have sacral dysmorphism (incidence: 6.6%). The details of demographic data are listed in Table 2.
Surgical results
The reduction quality of the pelvic ring injury was classified as excellent or good in 70 patients (82.4%) by Matta’s criteria and in 48 patients (56.5%) by Lefaivre’s criteria. The ADIO measurements of the ISS and TITS groups were 9.16° ± 6.97° and 3.09° ± 2.8° in the axial view, respectively, and 5.92° ± 3.65° and 2.10° ± 2.01° in the coronal view, respectively (Table 3). The radiation dose in ISS and TITS groups were 40.67 ± 15.42 mGy and 42.55 ± 18.35 mGy, respectively. Further, radiation time was 118.23 ± 29.22 s for a single ISS, and 132.58 ± 38.19 s for a single TITS. Additionally, according to the definition by Smith et al.24, the evaluations of ISS in both views had grade 1 mal-angulation and grade 0 perforation, whereas those of TITS showed grade 0 mal-angulation and grade 0 perforation.
Complications
One surgical site infection from the percutaneous wound was found 7 days after the index surgery. The wound finally healed uneventfully with implant retention after surgical debridement, proper wound care, and adequate systemic antibiotic treatment.
Risk factors analyses
To determine the potential risk factors that might cause a mal-positioned screw from this percutaneous procedure, a logistic regression analysis was carried. The chosen factors are shown in Table 4. Because of the relatively small number of enrolled patients, a stepwise method of logistic regression test was applied. However, we failed to find a significant risk factor for mal-positioned screw using logistic regression analysis. Using the receiver operating characteristic, the area under the curve in the axial and coronal views was 0.813 and 0.671, respectively, in the ISS group (Fig. 2A), and 0.461 and 0.792 respectively, in the TITS group (Fig. 2B).
Several univariate analyses were conducted to attempt to find potential risk factors for mal-positioned screws (Table 5). No significant risk factors were found in the ISS group, regardless of mpCT view. Although no risk factor was found in the coronal view for the TITS group, the patient’s body mass index (BMI) was identified as a single significant risk factor (p = 0.02) in the axial view.
Discussion
In this study, we reviewed the efficacy and safety of percutaneous ISS and TITS insertion using a single-arm fluoroscopic intensifier intraoperatively in 85 patients with pelvic ring injuries. The results revealed a satisfactory fracture reduction quality and a low rate of mal-positioned screws. Although BMI was a potential risk factor of screw mal-positioning according to the Mann–Whitney U test, it failed to show significance in logistic regression analysis.
The application of ISS and TITS has been widely accepted for the treatment of posterior pelvic ring injuries26,27,28. However, mal-positioned screws can cause devastating consequences, such as injuries to superior gluteal vessels, iliac vessels, lumbosacral nerve roots, and sympathetic chain4,9,29,30,31. Therefore, for effective and safe osteosynthesis, it is critical to perform this procedure under intraoperative real-time image guidance.
The optimal corridors of the ISS and TITS are narrow, and the procedure requires a high degree of technical skill. Therefore, several intraoperative image assessment technologies have been applied to enhance the accuracy of screw placement. Peng et al. compared the one and two C-arm fluoroscope technique, finding similar mal-positioned and clinical complication rates, but the two C-arm group had a shorter operation time (16 vs. 45 min, p < 0.001) and lower radiation exposure (4.5 vs. 5.7 min, p < 0.001)16. A recent study by Ciolli et al., showed satisfactory accuracy using the O-arm, with a complication rate and mal-positioning of screw varying from 0 to 15%17. Berger-Groch et al. compared fluoroscope-based conventional technique with 2D navigation procedures and found similar rates of malposition, but the radiation dose using the conventional technique was twice that of the 2D navigation procedure32. Richter et al. found that intraoperative computed tomography significantly reduced screw perforation rate compared to that when using conventional 3-dimensional navigation18. Although the advantages of advanced image systems cannot be ignored, the clinical utility might be limited to a few medical institutes. Because the single-arm fluoroscopic intensifier is the most common image assessment tool in most facilities, preoperative preparation is critical; personal protections from radiational exposure, such as keeping surgeon’s hand out of the field, covering thyroid and body with lead cloths, wearing lead spectacles, laser guidance, and radiation awareness, are crucial for medical staff in the operation theater33,34.
The reduction quality of the pelvic ring injuries in this study were comparable to those of previous reports35,36,37,38, which could be due to the treatment sequence. Before implanting the screws percutaneously, all the fractures should be reduced as possible. For AO B2.1 injuries, the reduction of the pelvic ring was initiated from the anterior pelvic ring to externally rotate the affected hemipelvis. A similar reduction sequence was indicated for AO B3.1 and B3.2 injuries. A considerable percentage (70.8%) of the patients underwent open reduction for diastatic sacroiliac joints because as long as anatomical reduction was achieved, a well-positioned screw could be inserted despite a prone position takes additional time to correct positioning of the patients and is more bothersome to anesthesiologists39. Patients with vertically unstable sacral fractures underwent a cranial-caudal orientation reduction prior to osteosynthesis. Using this “reduction first” concept, we achieved a low malposition rate, with no implantation-related complications.
A high BMI may limit the application of percutaneous surgeries40,41,42. We identified that a higher BMI was the single risk factor of TITS screw angle error under axial view of computed tomography (p = 0.02). This finding may result from the cumbersome patient positioning, blurry fluoroscopic images, or difficulty in instrument application for obese patients. However, it failed to reveal its significance during logistic regression analysis. We postulated that the reasons of inconsistence between two statistical results were due to our relatively small case number and the low malposition rate (4.8%) of the percutaneously applied screws.
Sacral dysmorphism is defined as upper sacral segment dysplasia and have a higher risk in mal-positioned implant during percutaneously placing ISS and TITS43. In dysmorphic sacrum, narrow but adequate corridor for ISS at S1 segment can be found; however, it carries a considerable rate of malalignment43,44. Currently, it is believed that the use of a 3D navigation system during operation confers a lower rate of mal-positioned screw44,45. The incidence of sacral dysmorphism in our cohort was 6.6%. All dysmorphic sacrum underwent percutaneous TITS osteosynthesis, and there were no complications that required revised surgeries under single C-arm fluoroscope intensifier examination. Additionally, the morphology variation of the sacrum was not a factor in mal-angulation of the screws. A similar concept reported by Rommens et al.43 showed that using 2D-fluoroscopic-guided ISS osteosynthesis would be a safe procedure in clinical practice if a thorough preoperative evaluation of the morphology of the upper sacrum, recognition of all the necessary anatomical landmarks, and careful operative procedure were performed.
This study has several limitations. First, its retrospective design study has inherited limitations. The cohort was treated using a single intraoperative image evaluation without a comparative method such as navigation-assisted percutaneous screw osteosynthesis. Second, only a small number of patients were enrolled. Third, the treatment protocol might have some divergence for patients with a similar fracture type such as supine or prone position and closed or open reduction. Fourth, all the operations were performed by a single surgeon, whose experience might have affected the surgical outcomes. However, we found that the radiation dose exposure and reduction quality of the pelvis was acceptable, and no screws penetrated the neuroforamen.
Conclusions
With careful preoperative planning and intraoperative preparations, percutaneous ISS and TITS implantation under a single-arm fluoroscopic intensifier examination is reliable and safe. Further prospective studies applying different intraoperative image systems should be conducted to identify their potential advantages over this surgical technique.
References
Incagnoli, P. et al. Early management of severe pelvic injury (first 24 hours). Anaesth. Crit. Care Pain Med. 38, 199–207. https://doi.org/10.1016/j.accpm.2018.12.003 (2019).
Giannoudis, P. V. et al. Prevalence of pelvic fractures, associated injuries, and mortality: The United Kingdom perspective. J. Trauma 63, 875–883. https://doi.org/10.1097/01.ta.0000242259.67486.15 (2007).
Alwaal, A. et al. The incidence, causes, mechanism, risk factors, classification, and diagnosis of pelvic fracture urethral injury. Arab. J. Urol. 13, 2–6. https://doi.org/10.1016/j.aju.2014.08.006 (2015).
Esses, S. I., Botsford, D. J., Huler, R. J. & Rauschning, W. Surgical anatomy of the sacrum. A guide for rational screw fixation. Spine (Phila Pa 1976) 16, S283–S288. https://doi.org/10.1097/00007632-199106001-00021 (1991).
Petryla, G. et al. Comparison of one-year functional outcomes and quality of life between posterior pelvic ring fixation and combined anterior–posterior pelvic ring fixation after lateral compression (B2 type) pelvic fracture. Medicina (Kaunas) https://doi.org/10.3390/medicina57030204 (2021).
Flint, L. & Cryer, H. G. Pelvic fracture: The last 50 years. J. Trauma 69, 483–488. https://doi.org/10.1097/TA.0b013e3181ef9ce1 (2010).
Bishop, J. A. & Routt, M. L. Jr. Osseous fixation pathways in pelvic and acetabular fracture surgery: Osteology, radiology, and clinical applications. J. Trauma Acute Care Surg. 72, 1502–1509. https://doi.org/10.1097/TA.0b013e318246efe5 (2012).
Wright, R. D. Jr. Indications for open reduction internal fixation of anterior pelvic ring disruptions. J. Orthop. Trauma 32, S18-23. https://doi.org/10.1097/BOT.0000000000001252 (2018).
Carlson, D. A., Scheid, D. K., Maar, D. C., Baele, J. R. & Kaehr, D. M. Safe placement of S1 and S2 iliosacral screws: The “vestibule” concept. J. Orthop. Trauma 14, 264–269. https://doi.org/10.1097/00005131-200005000-00007 (2000).
Zhang, L., Peng, Y., Du, C. & Tang, P. Biomechanical study of four kinds of percutaneous screw fixation in two types of unilateral sacroiliac joint dislocation: A finite element analysis. Injury 45, 2055–2059. https://doi.org/10.1016/j.injury.2014.10.052 (2014).
Le, V. H. et al. Biomechanical evaluation of supplemental percutaneous lumbo-sacro-iliac screws for spinopelvic fixation following total sacrectomy. J. Spinal Disord. Tech. 28, E181–E185. https://doi.org/10.1097/BSD.0000000000000241 (2015).
Mastrangelo, G. et al. Increased cancer risk among surgeons in an orthopaedic hospital. Occup. Med. (Lond.) 55, 498–500. https://doi.org/10.1093/occmed/kqi048 (2005).
Pavelka, T., Salášek, M. & Weisová, D. Complications associated with surgical treatment of pelvic ring fractures. Acta Chir. Orthop. Traumatol. Cech. 80, 208–215 (2013).
Comai, A., Zatelli, M., Haglmuller, T. & Bonatti, G. The role of transcatheter arterial embolization in traumatic pelvic hemorrhage: Not only pelvic fracture. Cureus 8, e722. https://doi.org/10.7759/cureus.722 (2016).
Matta, J. M. & Saucedo, T. Internal fixation of pelvic ring fractures. Clin. Orthop. Relat. Res. 242, 83–97 (1989).
Peng, K. T., Huang, K. C., Chen, M. C., Li, Y. Y. & Hsu, R. W. Percutaneous placement of iliosacral screws for unstable pelvic ring injuries: Comparison between one and two C-arm fluoroscopic techniques. J. Trauma 60, 602–608. https://doi.org/10.1097/01.ta.0000200860.01931.9a (2006).
Ciolli, G. et al. Navigated percutaneous screw fixation of the pelvis with O-arm 2: Two years’ experience. Med. Glas. (Zenica) 18, 309–315. https://doi.org/10.17392/1326-21 (2021).
Richter, P. H., Gebhard, F., Dehner, C. & Scola, A. Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 47, 402–407. https://doi.org/10.1016/j.injury.2015.11.023 (2016).
Florio, M. et al. 3D-Navigated percutaneous screw fixation of pelvic ring injuries—A pilot study. Injury 51, S28-33. https://doi.org/10.1016/j.injury.2020.07.025 (2020).
Marsh, J. L. et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 21, S1-133. https://doi.org/10.1097/00005131-200711101-00001 (2007).
Routt, M. L. Jr., Simonian, P. T., Agnew, S. G. & Mann, F. A. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: A cadaveric and clinical study. J. Orthop. Trauma 10, 171–177. https://doi.org/10.1097/00005131-199604000-00005 (1996).
Denis, F., Davis, S. & Comfort, T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 227, 67–81 (1988).
Tornetta, P. 3rd. & Matta, J. M. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin. Orthop. Relat. Res. 329, 186–193. https://doi.org/10.1097/00003086-199608000-00022 (1996).
Lefaivre, K. A., Starr, A. J., Barker, B. P., Overturf, S. & Reinert, C. M. Early experience with reduction of displaced disruption of the pelvic ring using a pelvic reduction frame. J. Bone Jt. Surg. Br. 91, 1201–1207. https://doi.org/10.1302/0301-620X.91B9.22093 (2009).
Smith, H. E., Yuan, P. S., Sasso, R., Papadopolous, S. & Vaccaro, A. R. An evaluation of image-guided technologies in the placement of percutaneous iliosacral screws. Spine 31, 234–238. https://doi.org/10.1097/01.brs.0000194788.45002.1b (2006).
Iorio, J. A., Jakoi, A. M. & Rehman, S. Percutaneous sacroiliac screw fixation of the posterior pelvic ring. Orthop. Clin. N. Am. 46, 511–521. https://doi.org/10.1016/j.ocl.2015.06.005 (2015).
Tidwell, J. et al. Percutaneous sacroiliac screw technique. J. Orthop. Trauma 30, S19-20. https://doi.org/10.1097/BOT.0000000000000606 (2016).
Liuzza, F. et al. Comparison between posterior sacral plate stabilization versus minimally invasive transiliac-transsacral lag-screw fixation in fractures of sacrum: A single-centre experience. Int. Orthop. 43, 177–185. https://doi.org/10.1007/s00264-018-4144-z (2019).
Thakkar, S. C. et al. 2D versus 3-D fluoroscopy-based navigation in posterior pelvic fixation: Review of the literature on current technology. Int. J. Comput. Assist. Radiol. Surg. 12, 69–76. https://doi.org/10.1007/s11548-016-1465-5 (2017).
Sagi, H. C. & Lindvall, E. M. Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J. Orthop. Trauma 19, 130–133. https://doi.org/10.1097/00005131-200502000-00010 (2005).
Licht, N. J., Rowe, D. E. & Ross, L. M. Pitfalls of pedicle screw fixation in the sacrum. A cadaver model. Spine 17, 892–896. https://doi.org/10.1097/00007632-199208000-00006 (1992).
Berger-Groch, J. et al. Accuracy of navigated and conventional iliosacral screw placement in B- and C-type pelvic ring fractures. Eur. J. Trauma Emerg. Surg. 46, 107–113. https://doi.org/10.1007/s00068-018-0990-z (2020).
Kaplan, D. J., Patel, J. N., Liporace, F. A. & Yoon, R. S. Intraoperative radiation safety in orthopaedics: A review of the ALARA (as low as reasonably achievable) principle. Patient Saf. Surg. 10, 27. https://doi.org/10.1186/s13037-016-0115-8 (2016).
Matityahu, A. et al. The great unknown—A systematic literature review about risk associated with intraoperative imaging during orthopaedic surgeries. Injury 48, 1727–1734. https://doi.org/10.1016/j.injury.2017.04.041 (2017).
Araiza, E. T. et al. Comparing the efficiency, radiation exposure, and accuracy using C-arm versus O-arm with 3D navigation in placement of transiliac-transsacral and iliosacral screws: A cadaveric study evaluating an early career surgeon. J. Orthop. Trauma 34, 302–306. https://doi.org/10.1097/BOT.0000000000001724 (2020).
Pieske, O. et al. CT-guided sacroiliac percutaneous screw placement in unstable posterior pelvic ring injuries: Accuracy of screw position, injury reduction and complications in 71 patients with 136 screws. Injury 46, 333–339. https://doi.org/10.1016/j.injury.2014.11.009 (2015).
Matityahu, A. et al. Three-dimensional navigation is more accurate than two-dimensional navigation or conventional fluoroscopy for percutaneous sacroiliac screw fixation in the dysmorphic sacrum: A randomized multicenter study. J. Orthop. Trauma 28, 707–710. https://doi.org/10.1097/BOT.0000000000000092 (2014).
Long, T. et al. Comparative study of percutaneous sacroiliac screw with or without TiRobot assistance for treating pelvic posterior ring fractures. Orthop. Surg. 11, 386–396. https://doi.org/10.1111/os.12461 (2019).
Schep, N. W., Haverlag, R. & van Vugt, A. B. Computer-assisted versus conventional surgery for insertion of 96 cannulated iliosacral screws in patients with postpartum pelvic pain. J. Trauma 57, 1299–1302. https://doi.org/10.1097/01.ta.0000133573.53587.2e (2004).
Byhahn, C., Lischke, V., Meininger, D., Halbig, S. & Westphal, K. Peri-operative complications during percutaneous tracheostomy in obese patients. Anaesthesia 60, 12–15. https://doi.org/10.1111/j.1365-2044.2004.03707.x (2005).
Yao, Y. et al. Risk factors for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg. 100, 1–6. https://doi.org/10.1016/j.wneu.2016.12.089 (2017).
Zhou, X. et al. Effect of obesity on outcomes of percutaneous nephrolithotomy in renal stone management: A systematic review and meta-analysis. Urol. Int. 98, 382–390. https://doi.org/10.1159/000455162 (2017).
Wendt, H. et al. Recommendations for iliosacral screw placement in dysmorphic sacrum based on modified in-out-in corridors. J. Orthop. Res. 37, 689–696. https://doi.org/10.1002/jor.24199 (2019).
Teo, A. Q. A., Yik, J. H., Jin Keat, S. N., Murphy, D. P. & O’Neill, G. K. Accuracy of sacroiliac screw placement with and without intraoperative navigation and clinical application of the sacral dysmorphism score. Injury 49, 1302–1306. https://doi.org/10.1016/j.injury.2018.05.027 (2018).
Weigelt, L. et al. Sacral dysmorphism and its implication on the size of the sacroiliac joint surface. Clin. Spine Surg. 32, e140–e144. https://doi.org/10.1097/BSD.0000000000000749 (2019).
Acknowledgements
The authors thank the statistical assistance and wish to acknowledge the support of the Maintenance Project of the Center for Big Data Analytics and Statistics (Grant CLRPG3D0048) at Chang Gung Memorial Hospital for study design and monitor, data analysis and interpretation.
Funding
There was no external funding.
Author information
Authors and Affiliations
Contributions
J.P.C. and Y.H.Y. wrote the main manuscript text. Y.H.Y. was the main contributor in updating and revising the original report. P.W.L. did the statistical analysis. P.J.T., C.Y.S., I.C.T., Y.C.C., and I.J.C. took part in reading and approving the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, JP., Tsai, PJ., Su, CY. et al. Percutaneous iliosacral screw and trans-iliac trans-sacral screw with single C-arm fluoroscope intensifier is a safe treatment for pelvic ring injuries. Sci Rep 12, 368 (2022). https://doi.org/10.1038/s41598-021-04351-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04351-z
This article is cited by
-
Higher pelvic incidence values are a risk factor for trans-iliac trans-sacral screw malposition in sacroiliac complex fracture treatment
Journal of Orthopaedics and Traumatology (2023)
-
A novel biplanar positioning technique to guide iliosacral screw insertion: a retrospective study
BMC Musculoskeletal Disorders (2023)
-
Imaging of pelvic ring fractures in older adults and its clinical implications-a systematic review
Osteoporosis International (2023)
-
Complications of conventional percutaneous sacroiliac screw fixation of traumatic pelvic ring injuries: a systematic review and meta-analysis
European Journal of Orthopaedic Surgery & Traumatology (2023)
-
Simultaneous reduction and fixation of concomitant acetabular fracture and ipsilateral sacroiliac joint injury through the pararectus approach: a technical report and early radiological outcome
European Journal of Orthopaedic Surgery & Traumatology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.