Abstract
Although both long and short cephalomedullary devices (CMDs) are used in the treatment of extracapsular hip fractures, the advantages of either option are subject to debate. This study aims to evaluate the differences in clinical outcomes with long versus short CMDs for extracapsular hip fractures. Studies included must have included subjects with at least 1 year of follow-up and reported on at least one of the following outcomes: rate of reoperation; rate of peri-implant fracture; operating time; blood loss; complication rate; length of hospital stay; 1-year mortality. Only articles written in the English language were included in this study. A search was conducted across the databases of Medline, Embase, CENTRAL (Cochrane Central Register of Controlled Trials), CINAHL and Scopus for articles published from the inception of the database to 1 November 2020. Included studies were assessed for their risk of bias using the Risk of Bias Tool (RoB2) and the risk-of-bias in non-randomized studies – of interventions (ROBINS-I) tool. A total of 8460 fractures from 16 studies were included in the analysis, with 3690 fixed with short, and 4770 fixed with long CMDs. A meta-analysis of the results revealed that short CMDs offer peri-operative advantages, while long CMDs could offer longer-term advantages. Limitations of this study include a lack of randomized control trials included in the analysis. In conclusion, when planning for the treatment of extracapsular hip fractures, a patient specific approach may be necessary to make a decision according to the individual risk profile of the patient.
Similar content being viewed by others
Introduction
Hip fractures are known to be increasing in frequency globally due to an ageing and active global population, with annual incidences set to rise to 6.26 million by 20501. Furthermore, with a 1-year mortality rate of about 20%, being able to choose the optimal treatment of a hip fracture is of increasing importance and relevance2,3. Of the different types of hip fractures, extracapsular fractures such as basicervical neck of femur fractures and intertrochanteric (IT) fractures are thought to be the most associated with falls from a standing height in elderly patients who have osteoporosis4.
Currently there is an increasing trend towards the using a cephalomedullary device (CMD) to manage both stable and unstable extracapsular hip fractures (EHFs) as these nails act as an intramedullary buttress to prevent excessive shaft medialization5,6,7. When compared with previous surgical options for management, CMDs have shown more favourable long term outcomes and a lower rate of complications8. CMDs which are < 250 mm in length are generally considered to be short, while those longer than 250 mm are classified as long CMDs, the difference being short CMDs do not cross the isthmus of the femur9.
Previous studies have compared the biomechanical properties of long and short CMDs and their effectiveness in fixation of EHFs. While it has been found that axial stiffness is greater in the use of short CMDs, the overall results show no significant differences between short or long CMDs and suggest that either option can be employed for fixation of unstable EHFs10,11.
Although both long and short CMDs are used in the treatment of EHFs, the theoretical advantages of either option are subject to debate12. In recent years, research into this topic has shown advantages of short CMDs over long CMDs, with better intra-operative outcomes, including a shorter operative time, less blood loss and lower rate of transfusion13,14. Conversely, there are also advantages for the use of long CMDs over short CMDs. The longer nail length theoretically provides increased stability in unstable patterns due to the possible distal subtrochanteric extension10,15. There have also been lower reported rates on the incidence of peri-implant fractures, possibly due to the full-length nail providing protection to the entire femoral shaft16,17. But these differences have not affected long term outcomes in patients, with both groups showing no significant difference in reoperation rates, complication rates or 1-year mortality rates18,19.
However, these findings have not been clearly shown in large scale review papers and meta-analyses. This systematic review and meta-analysis of current literature aims to evaluate the differences in clinical outcomes with long versus short cephalomedullary devices (CMDs) for extracapsular hip fractures with the primary outcome being operative time and secondary outcomes being complications such as blood loss and peri-implant fractures.
Methods
The systematic review was planned, conducted, and reported according to the PRISMA guidelines.
Eligibility criteria
To be included in this study, articles had to be either randomized controlled trials, retrospective or prospective cohort studies. These studies must have also reported on simple or multifragmentary EHFs (AO classification 31-A1, A2, and A3) and compared results from patients treated with long CMDs versus short CMDs. The studies must have also had subjects with at least 1 year of follow up, and reported on at least one of the following outcomes, operating time; estimated blood loss; length of hospital stay; overall rate of peri-implant fracture; overall rate of reoperation; overall complication rate; 1-year mortality. Only articles written in the English language were included in this study.
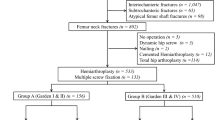
Case reports, case series, systematic reviews and meta-analyses were excluded from this study. Additionally, articles which did not include both short and long CMD cohorts for comparison, had less than 1 year follow up, or included pathological fractures due to tumours were also excluded (Fig. 1).
Search strategy
A systematic search was conducted across the databases of Medline, Embase, CENTRAL (Cochrane Central Register of Controlled Trials), CINAHL and Scopus for articles published from the inception of the database to 1 November 2020. The search strategy used was based on: (Hip Fractures or Intertrochanteric Fractures or pertrochanteric fracture*) and (Fracture Fixation, Intramedullary or cephalomedullary nail* or cephalomedullary nail* or intermedullary nail*).
Study selection
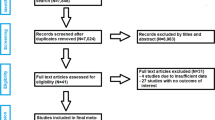
Duplicate studies were identified and removed by Covidence, a systematic review tool which uses the Cochrane technology platform. Two independent reviewers then screened the identified studies for relevance. Full manuscripts of included studies were assessed according to the eligibility criteria and the data was extracted. Any inconsistency was resolved through discussion between the two reviewers.
Statistical analysis
All statistical analyses were performed using Cochrane Revman 5.3 Software (Cochrane Collaboration 2014). Risk ratios and 95% confidence intervals were calculated. A p value of < 0.05 was considered significant for this study.
Results
Systematic review
Study selection
A total of 4143 studies were identified through the database searches, with 16 meeting the inclusion criteria and being included in this study (Fig. 2). A total of 8460 fractures were included in the analysis, with 3690 fixed with short, and 4770 fixed with long CMDs. The study with the largest sample size was also the most recently published, by Sadeghi et al. with 5526 patients20. Detailed information on the studies included are included in Table 1.
Study characteristics
Three studies, Sellan et al., Okcu et al. and Shannon et al., had a randomised controlled trail (RCT) design27,28,33. The remaining thirteen studies were retrospective cohort studies. Half of the studies were performed in the USA, with the remaining from Europe and Asia.
Device models
Data on the device models were collected from most studies, demonstrating a wide spectrum of device preferences across the board. Majority of the studies used a fixed device brand with nails of varying length for comparison, with the notable exception of Kleweno et al., which opted to include the Gamma 2 nail as a choice of long nail despite not including it under the short nail devices23.
Sample population characteristics
Most of the included studies had largely similar demographics of gender and age. However, Hou et al. noted a significant preponderance of females over males18. Boone et al. and Guo et al. also included significant differences in the ages of patients offered short and long nails, with older patients tending towards a short nail25,26. The included studies have a range of mean follow-up duration of 10.2–40.6 months post-operatively. Additionally, each study had at least one patient who was followed up for a minimum of 12 months post-operatively. ASA score was reported in four studies, ranging from 1 to 418,20,29,30.
Fracture pattern
Twelve studies reported on the fracture classification, with ten further subclassifying the fractures under the length of nail used. Many (n = 6) focused on 31A1/2 fractures, but some studies (n = 4) also elected to include patients from all 31A fractures. Of note, Okcu et al. only studied patients with 31A3 fractures28.
Operative time
Twelve studies included data on operative times for the surgical procedures. All but one study reporting a significantly longer operating time for long CMDs as compared to short CMDs, with Hong being the only dissenting study18,22,23,24,25,26,27,28,29,30,31,33.
Blood loss
Eight studies reported on the estimated blood loss from either procedure, with 7 studies reporting statistically significantly higher mean estimated blood loss in long CMD operations as opposed to short CMDs20,24,25,26,30,31,33. Five studies included information on the number of patients requiring blood transfusion, however only Boone et al. reported that there was a statistically significant difference in transfusion rates18,25,26,27,31.
Length of stay (LOS)
A total of 9 studies included the LOS of patients post-operatively, with 8 of the studies reporting no significant difference in LOS between the two groups18,20,22,25,26,27,28,29,31.
Information on intraoperative results have been reported in Table 2.
Post-operative results and complications
Seven studies reported on the 1-year mortality rates of patients, with none of them finding any significant difference between the two groups18,21,22,27,28,29,31.
1-year complication rate was reported in 11 studies, with only Li et al. reporting statistically fewer incidences in the long CMD group12,18,21,22,23,26,27,28,30,32,33.
The 1-year reoperation rate was reported to be statistically similar in the 8 studies which included the information18,20,22,23,28,29,31,33.
Peri-implant fracture rates 1-year post-operatively were reported in 10 studies, with only Frisch et al. reporting a statistically higher rate of fractures on the short CMD group12,18,20,21,23,24,26,27,29,32,33.
Peri-implant infection rates 1-year post-operatively were also reported to be similar in the 6 studies which reported on them18,20,24,26,32,33.
Only three studies noted patient reported outcomes under the Harris Hip Score 1-year post-operatively. Of the studies, only Shannon et al. reported a significant difference between the groups, with the short CMD group reporting higher results28,30,33.
Detailed information on post-operative results and complications can be found in Table 3.
Meta-analysis
We performed a meta-analysis to compare several outcomes of interest between long and short CMD groups. The outcomes analysed were mean operating time, mean estimated blood loss, mean length of stay, peri-implant fracture rates, reoperation rates and 1-year mortality rates. All 16 included studies were included in the meta-analysis.
Mean operating time
A total of 8 studies were used to analyse the difference in mean operating time between the two groups. Results from the analysis favoured the group which used short CMDs, reporting a statistically significant lower mean operating time of 13.99 min (95% CI − 15.15 to − 12.84; p value < 0.00001) (Fig. 3).
Mean estimated blood loss
A total of 6 studies were used to analyse the difference in mean estimated blood loss between the two groups. Results from the analysis favoured the group which used short CMDs, reporting a statistically significant lower estimated blood loss with a difference of 28.81 mL (95% CI − 33.86 to − 23.76; p value < 0.00001) (Fig. 4).
Mean length of stay
A total of 6 studies were used to analyse the difference in mean length of stay between the two groups. Results from the analysis favoured the group which used short CMDs, however this difference was found to not be statistically significant (95% CI − 0.35 to 0.09; p value = 0.23) (Fig. 5).
Peri-implant fractures
A total of 10 studies were used to analyse the overall risk ratio for peri-implant fractures between the two groups, with results showing a statistically significant difference, favouring the group with long CMDs. The risk ratio of peri-implant fractures among patients with short CMDs was 1.85 (95% CI 1.14–2.98; p value = 0.01) times as likely as the risk among patients who had long CMDs (Fig. 6).
Reoperation rate
A total of 6 studies were used to analyse the risk ratio of reoperation rate among patients, with results showing no statistically significant differences between the groups. The risk ratio of peri-implant fractures among patients with short CMDs was 1.08 (95% CI 0.78–1.49; p value = 0.63) times as likely as the risk among patients who had long CMDs (Fig. 7).
1-Year Mortality Rate
A total of 7 studies were used to analyse the risk ratio for 1-year mortality rate between the two groups, with results showing no statistically significant differences between the groups. The risk ratio of 1-year mortality rate among patients with long CMDs was 1.03 (95% CI 0.83–1.27; p value = 0.78) times as likely as the risk among patients who had short CMDs (Fig. 8).
Discussion
The aim of the study was to evaluate differences in clinical outcomes between using short and long CMDs in the treatment of extracapsular hip fractures. With the current lack of pooled analysis and comparison between these CMDs, it is difficult for surgeons to decide with conviction the optimal nail length for their patients. Through this systematic review and meta-analyses, we have found that long and short CMDs have different short-term and long-term outcomes. Short CMDs offered significant advantages in some of the peri-operative outcomes over the long CMDs. These were shorter operative times and less blood loss. However, long CMDs have shown advantages over short CMDs in their long-term benefits. With a significant reduction in risk of peri-implant fracture rate, the longer survivorship of the prosthesis could be a reflection of the theoretical increased stability provided by having a long CMD (Table 4).
Mean operating time between the two groups showed a significantly shorter operating time when using a short CMD as compared to a long CMD. This finding is in agreement with what has been reported in the existing literature where the number of steps and their complexity is lower when using a short CMD. This has been attributed to the additional time needed for reaming, as well the freehand placement of distal interlocking screws when inserting long CMDs36,37.
Estimated blood loss between the groups favoured the use of short CMDs over long CMDs, with the pooled data showing a statistically significant difference between the two groups. This has also been reported in the existing literature, with short CMDs showing a consistently lower blood loss over long CMDs36,38. The lower blood loss may also confer more advantages towards the use of a short nail, such as a reduction in the transfusion requirements, which had also been reported in 2 of the studies included25,26.
The short CMD group displayed a shorter LOS post-operatively as compared to the long CMD group. While this difference was not statistically significant, the difference in the length of stay could be due to a multitude of factors involving the condition and care of the patient. This may include the availability of community healthcare resources for the patient to be discharged to, rehabilitation services such as physiotherapy or other patient specific factors which may have altered their LOS. Another postulation is that patients who required long CMDs in the studies could have had a more complex or unstable fracture pattern which could have delayed their post-operative rehabilitation.
Rates of peri-implant fractures were significantly higher in the short CMD group, with a risk ratio of 1.85 times as compared to the long CMD group. The differences in these results may be due to the nail spanning the full length of the femur, and therefore providing additional stability and strength to the bone16,17. Peri-implant fractures were reported to be at the distal tip of the implant in several cases of long nails18,23,33. In some reports, the peri-implant fractures were due to identifiable incidents of trauma, such as falls from standing height12,23,25,32,33. Kleweno et al. reported no significant difference in the time to peri-implant fracture between the short and long nail cohorts23. In the studies included, the range of incidence for post-operative peri-implant fracture rates was reported to be from as early as 21 days post-operatively, up to 563 days post-operatively. It has been proposed that the timing of peri-implant fracture rates is not predictable as there is a large range of timings of reported incidence of this complication24.
Reoperation rates were similar in both groups, with no significant differences calculated. While the rate of peri-implant fractures 1-year post-operatively was higher in the short CMD group, rates of other complications was not well reported and thus a pooled analysis for the overall complication rate was not possible.
Finally, the 1-year mortality rate between the groups was found to be similar, with no significant difference between them. While the 1-year mortality rate has been reported to be as high as up to 58%, the current study has found significantly lower mortality rates across the groups39. The included studies have a 1-year mortality rate ranging from 0 (0/20) to 47% (33/70), with the vast majority reporting rates of under 30%. The decrease in 1-year mortality rate could reflect an improvement and development in operative technique, and post-operative care of hip fracture patients, thereby improving the prognosis.
Most studies included in this study have been deemed to have low levels of bias. However, those papers which have been identified to have potential issues with bias are commonly due to confounding variables, which most commonly are due to a significant difference between the ages of the short and long CMD groups. The studies which had these differences postulated that the difference could be attributed to shorter operative time which would be favourable in older age groups12,25,26.
In light of our analysis, we postulate that the use of short CMDs may be better suited for high-risk patients who may not be able to tolerate longer operating times. This includes those who have multiple medical comorbidities, and the elderly. The decrease in the amount of time under anaesthesia could be advantageous for these patients as it may decrease the risk of perioperative complications13,40. However, this should also be weighed against benefit in long-term outcomes that have been shown with the use of a long CMD.
While the study has presented several findings that could help guide the decision between the use of a short or long CMD, the strength of this study is in the volume of patients included in the analysis. This is the largest meta-analysis on the topic thus far, with the inclusion of large multi-centre data in the pooled analysis. Limitations of the paper would include the lack of RCTs included. While there were 3 included in the analysis, a larger pool of RCTs would be helpful in ascertaining the differences between short and long CMDs. Additionally, there was limited data available for some of the outcomes of interest, including 1-year post-operative HHS and transfusion rate, preventing a pooled analysis on these outcomes. Furthermore, the mean follow-up period of the included studies was varied (10.2–40.6 months), making a cross sectional study of the outcomes of interest difficult. While a key point of interest would be to investigate incidence and timeline of peri-implant fracture rates, few studies reported the time to the incidence of peri-implant fracture. This precluded further analysis on this subject, and the current study is only able to draw a conclusion to the overall rate of complications and peri-implant fractures. Other potentially interesting areas of further research on this topic would include a comparison between the peri-implant fracture rate in different periods post-operatively, including short- and long-term studies on the topic.
Conclusion
Short CMDs offer advantages of shorter operative time and lesser blood loss. However long CMDs could offer longer-term protection against peri-implant fractures. Therefore, in planning for the operation, a patient specific approach may be necessary to make a decision according to the individual risk profile of the patient.
References
Cooper, C., Campion, G. & Melton, L. J. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 2(6), 285–289 (1992).
Cenzer, I. S. et al. One-year mortality after hip fracture: Development and validation of a prognostic index. J. Am. Geriatr. Soc. 64(9), 1863–1868 (2016).
Hu, F., Jiang, C., Shen, J., Tang, P. & Wang, Y. Preoperative predictors for mortality following hip fracture surgery: A systematic review and meta-analysis. Injury 43(6), 676–685 (2012).
Ahn, J. & Bernstein, J. Fractures in brief: Intertrochanteric hip fractures. Clin. Orthop. Relat. Res. 468(5), 1450–1452 (2010).
Page, P. R. J. et al. Changing trends in the management of intertrochanteric hip fractures—A single centre experience. Injury 47(7), 1525–1529 (2016).
Seo, J.-S., Min, H.-J., Kim, D. M., Oh, S.-M. & Kim, S.-M. Surgical results of the cephalomedullary nail for the femoral intertrochanteric fracture: Comparison between non-experienced surgeons and experienced surgeon. Hip Pelvis. 28(4), 225–231 (2016).
Fairag, R., Abduljabbar, F. H., Page, A. & Dimentberg, R. Are cephalomedullary nail guides accurate? A case report of an unexpected complication after nailing an intertrochanteric femoral fracture. Geriatr. Orthop. Surg. Rehabil. 9, 2151458518757797 (2018).
Yuan, X., Yao, Q., Ni, J., Peng, L. & Yu, D. Proximal femoral nail antirotation versus dynamic hip screw for intertrochanteric fracture in elders: A meta-analysis. Zhonghua Yi Xue Za Zhi 94(11), 836–839 (2014).
Jha, V. & Ahmed, T. Modified short proximal femoral nail for intertrochanteric fractures of femur in Indian patients—Our experience. Malays Orthop. J. 14(2), 72–82 (2020).
Blum, L. E., Yee, M. A., Mauffrey, C., Goulet, J. A., Perdue, A. M. & Hake, M. E. Comparison of reamed long and short intramedullary nail constructs in unstable intertrochanteric femur fractures: A biomechanical study. OTA Int. 3(2), e075 (2020).
Marmor, M. et al. Biomechanical comparison of long, short, and extended-short nail construct for femoral intertrochanteric fractures. Injury 46(6), 963–969 (2015).
Vaughn, J. et al. Complications of short versus long cephalomedullary nail for intertrochanteric femur fractures, minimum 1 year follow-up. Eur. J. Orthop. Surg. Traumatol. 25, 665–670 (2014).
Dunn, J. et al. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review. J Orthop Traumatol. 17(4), 361–367 (2016).
Zhang, Y. et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 103(5), 685–690 (2017).
Lindskog, D. M. & Baumgaertner, M. R. Unstable intertrochanteric hip fractures in the elderly. JAAOS. 12(3), 179–190 (2004).
Baldwin, P. C. I., Lavender, R. C., Sanders, R. & Koval, K. J. Controversies in intramedullary fixation for intertrochanteric hip fractures. J. Orthop. Trauma 30(12), 635–641 (2016).
Horwitz, D. S., Tawari, A. & Suk, M. Nail length in the management of intertrochanteric fracture of the femur. JAAOS 24(6), e50–e58 (2016).
Hou, Z. et al. Treatment of pertrochanteric fractures (OTA 31–A1 and A2): Long versus short cephalomedullary nailing. J. Orthop. Trauma. 27(6), 318–324 (2013).
Dunn, J. et al. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review. J. Orthop. Traumatol. 17(4), 361–367 (2016).
Sadeghi, C., Prentice, H. A., Okike, K. M. & Paxton, E. W. Treatment of intertrochanteric femur fractures with long versus short cephalomedullary nails. Perm. J. 24, 19 (2020).
Hulet, D. A. et al. Short versus long cephalomedullary nails for fixation of stable versus unstable intertrochanteric femur fractures at a level 1 trauma center. Orthopedics 42(2), e202–e209 (2019).
Krigbaum, H., Takemoto, S., Kim, H. T. & Kuo, A. C. Costs and complications of short versus long cephalomedullary nailing of OTA 31–A2 proximal femur fractures in U.S. veterans. J. Orthop. Trauma 30(3), 125–9 (2016).
Kleweno, C. et al. Short versus long cephalomedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. J. Orthop. Trauma 28(7), 391–397 (2014).
Frisch, N. B. et al. Short versus long cephalomedullary nails for pertrochanteric hip fracture. Orthopedics 40(2), 83–88 (2017).
Boone, C. et al. Short versus long intramedullary nails for treatment of intertrochanteric femur fractures (OTA 31–A1 and A2). J. Orthop. Trauma 28(5), e96–e100 (2014).
Guo, X. F., Zhang, K. M., Fu, H. B., Cao, W. & Dong, Q. A comparative study of the therapeutic effect between long and short intramedullary nails in the treatment of intertrochanteric femur fractures in the elderly. Chin. J. Traumatol. 18(6), 332–335 (2015).
Sellan, M. et al. Short versus long intertan fixation for geriatric intertrochanteric hip fractures: A multicentre head-to-head comparison. J. Orthop. Trauma 33(4), 169–174 (2019).
Okcu, G., Ozkayin, N., Okta, C., Topcu, I. & Aktuglu, K. Which implant is better for treating reverse obliquity fractures of the proximal femur: A standard or long nail?. Clin. Orthop. Relat. Res. 471(9), 2768–75 (2013).
Hong, C. C. et al. The long and short of cephalomedullary nails in the treatment of osteoporotic pertrochanteric fracture. Singapore Med J. 58(2), 85–91 (2017).
Li, Z., Liu, Y., Liang, Y., Zhao, C. & Zhang, Y. Short versus long intramedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. Int. J. Clin. Exp. Med. 8(4), 6299–6302 (2015).
Raval, P., Ramasamy, A., Raza, H., Khan, K. & Awan, N. Comparison of short vs long anti-rotation in treating trochanteric fractures. Malays. Orthop. J. 10(1), 22–28 (2016).
Bovbjerg, P. E., Larsen, M. S., Madsen, C. F. & Schønnemann, J. Failure of short versus long cephalomedullary nail after intertrochanteric fractures. J. Orthop. 18, 209–212 (2020).
Shannon, S. F. et al. Short versus long cephalomedullary nails for pertrochanteric hip fractures: A randomized prospective study. J. Orthop. Trauma. 33(10), 480 (2019).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 366, l4898 (2019).
Sterne, J. A. et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 355, i4919 (2016).
Page, P. R. J., Poole, W. E. C., Shah, K. & Upadhyay, P. K. Short or long intramedullary devices for hip fracture? A systematic review of the evidence. J. Orthop. 22, 377–382 (2020).
Zhang, Y. et al. Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31–A1, A2 and A3): A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 103(5), 685–690 (2017).
Sohatee, M. & Bennet, J. A systematic review of short versus long intramedullary fixation in the management of pertrochanteric fractures. Trauma 20(3), 161–168 (2018).
Rapp, K., Becker, C., Lamb, S. E., Icks, A. & Klenk, J. Hip fractures in institutionalized elderly people: Incidence rates and excess mortality. J. Bone Miner. Res. 23(11), 1825–1831 (2008).
Cinque, M. E. et al. Short versus long cephalomedullary nailing of intertrochanteric fractures: A meta-analysis of 3208 patients. Arch. Orthop. Trauma Surg. https://doi.org/10.1007/s00402-021-03752-z (2021).
Author information
Authors and Affiliations
Contributions
H.R.B.A.R conceptualized and refined the research idea. He was also involved in the interpretation of the statistical analyses and drafting of the manuscript. G.K.Y.T and C.S.C were involved in the literature search, selecting and performing the statistical analysis and drafting of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tan, G.K.Y., Chong, C.S. & Bin Abd Razak, H.R. Clinical outcomes following long versus short cephalomedullary devices for fixation of extracapsular hip fractures: a systematic review and meta-analysis. Sci Rep 11, 23997 (2021). https://doi.org/10.1038/s41598-021-03210-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-03210-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.