Abstract
Atopic dermatitis (AD) is associated with allergic comorbidities, such as asthma, allergic rhinitis (AR), and allergic contact dermatitis (ACD). The etiology of keloid is largely unknown; however, AD and keloid share inflammatory pathways characterized by T-helper cell 2 cytokines and increased dermal fibroblast activity. The prevalence of keloids has been reported to increase in patients with AD, but it remains controversial. This study aimed to estimate the prevalence of keloids in patients with AD, and compare it with the prevalence of other comorbidities of AD. We assessed the Korean National Health Information Database and medical records including coexisting asthma, AR, and ACD. Single and multiple logistic regression models were created for keloids and each allergic disease. The prevalence of keloids was higher in the AD group than in the control group. Among patients with AD, adolescents and adults had a higher prevalence of keloids than infants and children. The risk of keloids was high with AD alone, and coexisting asthma significantly increased the risk. Similarly, the risk of keloids was higher in AR associated with AD and ACD associated with AD than in AD alone. Thus, among Koreans, patients with AD have a higher risk of keloid development, with coexisting allergic diseases increasing the risk.
Similar content being viewed by others
Introduction
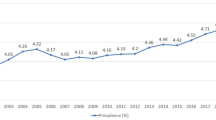
Atopic dermatitis (AD) is a chronic inflammatory skin disease associated with numerous atopic and nonatopic comorbidities1. The prevalence of AD is estimated to be 15–20% in children and 1–3% in adults, and the incidence has increased two- to three-fold during the past few decades in industrialized countries2.
Keloid is a fibroproliferative dermal tumor resulting from skin trauma and subsequent abnormal scar formation3. The mechanism underlying the pathological development of keloids is largely unknown; however, it is mainly characterized by an overproduction of extracellular matrix and high activity of fibroblasts during the inflammatory and remodeling phases of scar formation, resulting in the excessive accumulation of collagen4,5. These processes are also observed in fibroblasts among patients with AD6. Although the association between AD and keloids is still unclear, several possible links have been hypothesized.
AD and keloid share common inflammatory pathways that are characterized by T-helper cell 2 (Th2) cytokines. An impaired inflammatory response of fibrogenesis involving Th2 cytokines secreted by CD4 + T cells such as interleukin (IL)-4, IL-5, IL-10, and IL-13, leads to the imbalance between pro-fibrotic and anti-fibrotic signals7. Additionally, in AD, upregulation of Th2 cytokines is triggered, and IL-4, IL-5, IL-10, and IL-13 are secreted, resulting in epidermal thickening, inflammation, pruritus, and decreased expression of barrier proteins such as filaggrin and loricrin, all of which are clinical characteristics of AD8. The reason why prurigo nodularis is frequently observed in patients with AD, with lichenification being one of the most common clinical manifestations of AD, is presumed to be due to this process9.
It is well established that patients with AD have a higher chance of developing allergic comorbidities such as asthma, allergic rhinitis (AR), and allergic contact dermatitis (ACD)1. Furthermore, the severity of AD was associated with a higher prevalence of comorbid allergic disorders and increased severity of comorbidities10. Based on these facts, the authors hypothesized that the patients with both AD and allergic comorbidities might have a higher prevalence of keloids.
Keloids occur more frequently in dark-skinned individuals, with a higher prevalence in Fitzpatrick skin phototypes III to VI11. African Americans have a 5 to 16 times higher prevalence of keloids than Caucasians12. The annual keloid incidence rate is 0.15% among the general Taiwanese population, but the exact prevalence among Asians is unknown13. In a large-scale retrospective cohort study in Taiwan, the probability of keloid development in patients with AD is 3.19 times higher than in the healthy population14. However, to date, there are no known reports on the prevalence of keloids in AD accompanied by allergic diseases.
To the best of our knowledge, this study first analyzed big data from the Korean National Health Information Database (NHID) and aimed to (1) estimate the prevalence of keloids in patients with AD and (2) compare the prevalence of keloids with those of patients with AD alone and those with both AD and allergic comorbidities.
Materials and methods
Data sources
The data used in this study were obtained from the Korean NHID, in which diseases were coded according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). This database contains nationwide claims data and is linked at an individual level with the Korean registration number assigned to all Korean residents at birth or immigration for practical purposes. This study was approved by the Institutional Review Board of Kyung Hee University (IRB number 2019-07-076) and a waiver of informed consent was approved from IRB due to the retrospective nature of the big datasets. All methods were performed in accordance with the relevant guidelines and regulations.
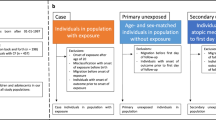
Study design and population
We assessed the Korean NHID from 2017 to 2018 and medical records were analyzed according to the ICD-10-CM codes. From this database, two groups were defined: an AD patient group and a control group. A total of 2,517,401 subjects under the ICD-10 code L20 were included in the AD group. For the control group, we excluded patients with the AD code, L20, for the past 3 years from the database. A random sample of 3% was prepared. In total, 3,132,283 subjects in the control group were matched by age and sex. All subjects in both groups were classified into two subgroups, with or without keloids. A diagnosis of keloids was defined as the condition under ICD-10 code L91.
Demographic information (age and sex) and comorbidities of allergic diseases identified by ICD-10-CM codes were also collected. The associated allergic diseases in this study included asthma (ICD-10 code J304), AR (ICD-10 code L209), and ACD (ICD-10 code L239). All patients and the control group were classified by age: infant and early childhood, 0–5 years; late childhood, 6–10 years; adolescence, 11–20 years; adulthood, 21–60 years; and the elderly, > 61 years.
Statistical analysis
A chi-square test was employed, and the odds ratios (ORs) were analyzed to compare the AD and control groups by age and sex. In the age group, the OR of late childhood, adolescence, adulthood, elderly was compared with infancy and early childhood as a reference. Also, in the sex, the OR of female was compared as male as a reference. In addition, logistic regression was performed to analyze the differences in the effects of variables, including the presence or absence of AD, age, and sex, on the prevalence of keloids. Furthermore, we analyzed the OR of the risk of keloids between the AD patients without asthma (or allergic rhinitis, allergic contact dermatitis) and with asthma (or allergic rhinitis, allergic contact dermatitis), and was compared to the control group through the multiple logistic regression adjusted by age and gender. A p-value of < 0.05 was considered statistically significant. All data processing and statistical analyses were performed using SAS Enterprise Guide 7.1 (SAS Institute Inc., Cary, NC).
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. This research study was conducted retrospectively from data obtained for clinical purposes. An IRB of Kyung hee university hospital officially granted ethical approval.
Results
Baseline characteristics of patients
Baseline characteristics of patients in the AD and control group are shown in Table 1. All personnel in this study were Koreans. A total of 5,649,684 personnel were included in this study, and 44.56% (2,517,401) had AD (see Supplementary Table S1 online). In patients with AD, 26.01% of patients were younger than 5 years, and 51.88% were younger than 20 years of age. The rate of AD tended to decrease with age. Of the patients with AD, 53.01% were females. Among all age groups, the prevalence of AD was the highest among infants and children.
Increased prevalence of keloids in the AD group
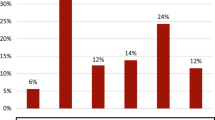
The prevalence of keloids was higher in the AD group than in the control group (Table 2). Keloids exist in 1.43% (36,090 out of 2,517,401) of the patients with AD and in 0.52% (16,216 out of 3,132,283) of the control group. Simple logistic regression was performed, and the prevalence of keloids was significantly higher among the patients with AD than in the control group (OR 2.795, p < 0.001). When comparing the prevalence of keloids according to the age groups of all patients, the prevalence of keloids was higher among adolescents and adults than among those belonging to infancy and early childhood (OR 18.333, and OR 29.289, 95%, p < 0.001). The entire numbers can be found as Supplementary Table S2 online.
The effect of allergic comorbidities associated with AD on keloids
The effect of having allergic comorbidities associated with AD on the risk of developing keloids (Table 3) was evaluated using multiple logistic regression. Patients with AD alone were at a higher risk of keloids (OR 2.97, p < 0.001), and asthma coexisting with AD increased the risk of keloids significantly (OR 3.17, p < 0.001). This effect was also observed in AR and ACD. In patients with AR associated with AD, the risk of keloids increased compared with that in AD alone (OR 3.2, vs. OR 2.61, p < 0.001). In patients with ACD associated with AD, the risk of keloids increased compared with that in AD alone (OR 3.81, vs. OR 2.32, p < 0.001). The entire numbers can be found as Supplementary Table S2 online.
Discussion
This is the first study demonstrating that the risk of keloids is strongly associated with AD in the Korean population. Our results also demonstrate that the prevalence of keloids increases with coexisting allergic diseases, such as asthma, AR, and ACD. Previous data on the prevalence of keloids is based mainly on Caucasians and Taiwanese in Asia13,14. In Korea, where all citizens are obligated to subscribe to national medical insurance, large cohort study using electronic medical information is feasible. For the first time, our findings show that the prevalence of keloids increased in patients with AD in the Korean population. Hajdarbegovic et al. also suggested that keloids may be strongly associated with atopic asthma in European, African, and Asian populations15. The findings in this study are consistent with those of previous studies wherein the risk of keloids is higher in AD patients with allergic comorbidities.
The molecular pathophysiology of keloid formation and progression is poorly understood. However, fibroblasts, one of the main cells responsible for most of the collagen and extracellular matrix deposition in both normal and abnormal wound healing, have been identified to contribute to keloid formation and dermal structural changes in AD skin lesions16. Recently, Shin et al. reported that the expression of thymic stromal lymphopoietin (TSLP), an IL-7-like cytokine, was increased in keloid tissue compared to the normal skin. In addition, keloidal fibroblasts treated with TSLP produced higher levels of collagen I, collagen III, and transforming growth factor β compared to normal fibroblasts, which explains the pivotal role of TSLP in keloid development17. Increased serum TSLP has also been observed in AD patients18.
Another molecule that contributes to the collagen production of dermal fibroblasts in AD is Oncostatin M (OSM), a T lymphocyte/macrophage-derived proinflammatory signaling molecule similar to the IL-6 cytokine family19. Fibroblasts are target cells for OSM. OSM stimulates collagen and glycosaminoglycan production in dermal fibroblasts, and this process can be observed in both keloidal formation and prurigo nodularis in patients with AD20.
Other than upregulation of Th2 cytokines, effector memory CD8 + T cells and CD103 + CD8 + resident memory T (TRM) cells are increased in keloid tissue. Therefore, increased CD8 + TRM in keloid tissues might contribute to local inflammation21. TRM cells have been shown to contribute to the recurrence of AD; however, the exact roles of skin TRM are still unclear22.
There have been a few reports on the association between allergic diseases and keloid development; however, these results are still debated. Hajdarbegovic et al., for example, revealed no association between AD and keloids in the adjusted model of a case–control study. Additionally, they suggested that asthma was significantly, consistently, and strongly associated with keloids. However, there were no consistent associations found on keloids with atopic eczema or hay fever15. In contrast, Lu et al. demonstrated that patients with AD had a greater possibility of developing keloids in a nationwide retrospective cohort study in Taiwan. According to this study, the AD cohort had significantly higher percentages of patients with asthma (25.41 vs. 12.91, p < 0.001), AR (54.78 vs. 35.92, p < 0.001), and allergic conjunctivitis (57.22 vs. 42.08, p < 0.001) compared with the non-AD cohort14. In our study, AD patients with ACD also had an increased prevalence of keloid risk, which is different from previous studies, suggesting that ACD may have the characteristic of AD-associated comorbidity. In the past, the higher permeation of contact allergens through the disrupted skin barrier was the main factor of ACD in patients with AD. Recently, potential shared immune pathways have been demonstrated for subsets of AD and ACD, including Th1, Th2, Th9, and/or Th1723,24.
Han et al. demonstrated the relationship between a disintegrin and metalloprotease 33 (ADAM33) polymorphism and keloid scars in an East Asian population. Q-1 SNPs in blood were significantly associated with keloid scars. ADAM33 protein is a zinc-dependent endopeptidase, characterized by a pro-domain, metalloprotease domain, and disintegrin domain25. The ADAM33 gene was found to be associated with asthma and airway hyperresponsiveness26. It is thought that this may explain the increased keloid risk in AD associated with asthma. Considering the literature mentioned above, AD and keloid share various genetic and pathologic mechanisms.
One of the strengths of this study is the use of a large population-based claims dataset consisting of one ethnic group, which enabled the analysis of all cases of AD, keloids, and comorbid allergic diseases. Moreover, since the Korean NHID is one of the largest claims datasets including all age groups and the entire region, the possibility of selection bias is reduced to compare the relationships between the AD patients and control group. Second, it is the first time that a large cohort analysis has demonstrated the result of an increase in the prevalence of keloids in AD patients with allergic diseases. However, this study has several limitations. First, due to the characteristics of the nationwide database of the NHID, the possibility of false negatives exists in both groups. All participants were patients who visited the hospital for any purpose. Therefore, it cannot be ruled out that both groups have a slightly higher likelihood of keloid diagnosis compared to the actual healthy group, which increases the possibility of underestimation compared to the actual prevalence of keloid. Second, there may be a relative underestimation of the prevalence of keloids in the control group, the general patient population. Compared to patients with AD who visit a dermatologist, the control patients who visit other departments are likely to be unaware of their keloid scars and have no need for medical services. However, considering the accessibility and affordability of medical specialists in the Republic of Korea, this statistical difference is thought to be small compared to other countries. Third, since the data are large-scale cohort data collected for insurance purposes rather than research purposes, several important confounding factors including family history, occupation and level of education were not provided. Thus, further prospective studies with accurate inclusion criteria are needed to clarify the exact relationship between allergic diseases and keloids.
In conclusion, this study demonstrated that in the Korean population, patients with AD have a higher risk of keloid development, and the risk is even higher with coexisting allergic diseases. Nevertheless, further exploration of this association is needed to confirm these relationships and the pathophysiological mechanisms common to AD and keloids.
Data availability
All databases are available as Supplementary Information files.
References
Silverberg, J. I. Comorbidities and the impact of atopic dermatitis. Ann. Allergy. Asthma. Immunol. 123, 144–151 (2019).
Nutten, S. Atopic dermatitis: Global epidemiology and risk factors. Ann. Nutr. Metab. 66(Suppl 1), 8–16 (2015).
Bran, G. M., Goessler, U. R., Hormann, K., Riedel, F. & Sadick, H. Keloids: Current concepts of pathogenesis (review). Int. J. Mol. Med. 24, 283–293 (2009).
Fujiwara, M., Muragaki, Y. & Ooshima, A. Keloid-derived fibroblasts show increased secretion of factors involved in collagen turnover and depend on matrix metalloproteinase for migration. Br. J. Dermatol. 153, 295–300 (2005).
Nakaoka, H., Miyauchi, S. & Miki, Y. Proliferating activity of dermal fibroblasts in keloids and hypertrophic scars. Acta. Derm. Venereol. 75, 102–104 (1995).
Berroth, A. et al. Role of fibroblasts in the pathogenesis of atopic dermatitis. J. Allergy. Clin. Immunol. 131, 1547–1554 (2013).
Tripathi, S. et al. Hypertrophic scars and keloids: A review and current treatment modalities. Biomed. Dermatol. 4, 1 (2020).
Brandt, E. B. & Sivaprasad, U. Th2 cytokines and atopic dermatitis. J. Clin. Cell. Immunol. 2, 110 (2011).
Iking, A. et al. Prurigo as a symptom of atopic and non-atopic diseases: Aetiological survey in a consecutive cohort of 108 patients. J. Eur. Acad. Dermatol. Venereol. 27, 550–557 (2013).
Silverberg, J. I. et al. Association of atopic dermatitis with allergic, autoimmune, and cardiovascular comorbidities in US adults. Ann. Allergy Asthma Immunol. 121, 604–612 (2018).
Kang, S., Amagai, A., Bruckner, A. L., Enk, A. H., Margolis, D. J., McMichael, A.J., et al. Fitzpatrhick’s Dermatology, 9th edition. (ed. Kang, S.) 3723 (McGraw Hill, 2019)
Kelly, A. P. Update on the management of keloids. Semin. Cutan. Med. Surg. 28, 71–76 (2009).
Sun, L. M., Wang, K. H. & Lee, Y. C. Keloid incidence in Asian people and its comorbidity with other fibrosis-related diseases: A nationwide population-based study. Arch. Dermatol. Res. 306, 803–808 (2014).
Lu, Y. Y. et al. Keloid risk in patients with atopic dermatitis: A nationwide retrospective cohort study in Taiwan. BMJ Open 8, e022865 (2018).
Hajdarbegovic, E. & Bloem, A. The association between atopic disorders and keloids: A case-control study. Indian. J. Dermatol. 60, 635 (2015).
Andrews, J. P., Marttala, J., Macarak, E., Rosenbloom, J. & Uitto, J. Keloids: The paradigm of skin fibrosis: Pathomechanisms and treatment. Matrix Biol. 51, 37–46 (2016).
Shin, J. U. et al. TSLP is a potential initiator of collagen synthesis and an activator of CXCR4/SDF-1 axis in keloid pathogenesis. J. Invest. Dermatol. 136, 507–515 (2016).
Lee, E. B. et al. Increased serum thymic stromal lymphopoietin in children with atopic dermatitis. Pediatr. Allergy. Immunol. 21, e457–e460 (2010).
Williams, K. A., Huang, A. H., Belzberg, M. & Kwatra, S. G. Prurigo nodularis: Pathogenesis and management. J. Am. Acad. Dermatol. 83, 1567–1575 (2020).
Duncan, M. R., Hasan, A. & Berman, B. Oncostatin M stimulates collagen and glycosaminoglycan production by cultured normal dermal fibroblasts: Insensitivity of sclerodermal and keloidal fibroblasts. J. Invest. Dermatol. 104, 128–133 (1995).
Chen, Z. et al. Characterization of CD45RO+ memory T lymphocytes in keloid disease. Br. J. Dermatol. 178, 940–950 (2018).
Xu, Q. N. & Zhu, H. Q. The roles of skin-resident memory T cells in dermatoses. Int. J. Dermatol. Venereol. 2, 29–32 (2019).
Owen, J. L., Vakharia, P. P. & Silverberg, J. I. The role and diagnosis of allergic contact dermatitis in patients with atopic dermatitis. Am. J. Clin. Dermatol. 19, 293–302 (2018).
Thyssen, J. P., McFadden, J. P. & Kimber, I. The multiple factors affecting the association between atopic dermatitis and contact sensitization. Allergy 69, 28–36 (2014).
Han, J. et al. Association of ADAM33 gene polymorphisms with keloid scars in a northeastern Chinese population. Cell. Physiol. Biochem. 34, 981–987 (2014).
Van Eerdewegh, P. et al. Association of the ADAM33 gene with asthma and bronchial hyperresponsiveness. Nature 418, 426–430 (2002).
Acknowledgements
We would like to thank Kang, D.H. for supporting this work.
Funding
This work was supported by a Grant from the Kyung Hee University in 2018 (KHU-20181041).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Conceptualization, funding acquisition, and supervision were performed by M.K.S. and H.J.A. Data collection and analysis were performed by H.E.K. and S.J.J. The first draft and the revision of the manuscript was written by H.E.K. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwon, HE., Ahn, HJ., Jeong, S.J. et al. The increased prevalence of keloids in atopic dermatitis patients with allergic comorbidities: a nationwide retrospective cohort study. Sci Rep 11, 23669 (2021). https://doi.org/10.1038/s41598-021-03164-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-03164-4
This article is cited by
-
Scars
Nature Reviews Disease Primers (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.