Abstract
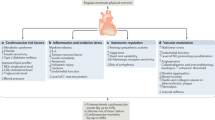
Long-term sports training leads to myocardial adaptations, with remodelling of the heart chambers. However, while myocardial adaptations of the left heart are well described, remodelling of the right heart and its impact on the development of arrhythmias is still debated. To conduct a systematic review on right ventricle (RV) and right atrium (RA) structural and functional changes in athletes who participate in long-term endurance training. Systematic review. A systematic literature search was conducted. All the articles reporting right heart echocardiographic (ECHO) and cardiac magnetic resonance (CMR) parameters evaluated in endurance athletes and sedentary subjects were considered eligible. A multivariate analysis was conducted to investigate whether age, sex, body surface area (BSA), intensity of training are associated with RV ECHO, CMR parameters and RA ECHO parameters. A positive association between age and right atrium area (RAA) (P = 0.01) was found. This is a negative association to RV E/A (P = 0.004), and RV end diastolic diameter (RVED) longitudinal (P = 0.01). A positive association between BSA and RVED middle (P = 0.001), as well between BSA and RAA (P = 0.05) was found, along with a negative association with RV E/A (P = 0.002). A positive association between intensity of training and RV end systolic area (RVESA) (P = 0.03), RV end diastolic volume indexed (RVEDVI) (P = 0.01), RV end systolic volume indexed (RVESVI) (P = 0.01) was found, along with a negative association with ejection fraction (EF %) (P = 0.01). Endurance athletes demonstrated an association between RV remodelling and age, BSA and intensity of training.
Similar content being viewed by others
Introduction
“Athlete’s heart” refers to remodelling of the whole cardiac muscles induced by the high workload of sports training1,2,3,4,5,6,7,8,9,10. Heart remodelling is different following endurance training and resistance training11.
In endurance training, the left ventricle (LV) undergoes eccentric hypertrophy, while resistance training promotes concentric hypertrophy12. A clear classification is not possible as the overall size of cardiomyocytes increases under both remodelling patterns. In general, the thickness of the LV wall prevails in resistance training as a consequence of chronic volume overload; LV dilatation is a prominent characteristic in endurance-trained heart, mainly determined by chronic systolic pressure overload13.
However, exercise-induced changes of the right ventricle (RV) are still debated14. Also, there seems to be an association between RV hypertrophy and Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)15,16,17, one of the major causes of cardiac death in young athletes18,19. Therefore, it would be interesting to define exercise-induced RV adaptation, and its impact on the onset of arrhythmias16. Endurance training causes greater morphological and functional RV changes than any other type of exercise, but the role of variables such as age, sex and BSA has not been established20. Endurance training increases the hemodynamic needs with a consequent chronic pressure elevation in the cardiac chambers21. As a result, long-term exercise leads to permanent RV structural and functional modifications, with large interindividual variability22. It is important to distinguish between acute and chronic adaptations, and to consider exercise loading and intensity23, which induce different functional and clinical consequences22,23. Immediately after an intense exercise, the serum level of troponin and B-type natriuretic peptide increases17,24. A process of micro injuring and healing occurs, mirroring what take place in skeletal muscles, which, eventually, leads to myocardial adaptation22.
This study investigates the structural and functional changes of the right ventricle (RV) and right atrium (RA) in athletes who participate in long-term endurance training, and defines whether the RV ECHO and CMR reference values for the general population are appropriate for endurance athletes.
Methods
Search strategy
The present systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) recomendations25. We followed the PICO protocol for the preliminary search:
-
P (Problem): right heart in endurance athletes;
-
I (Intervention): long-term endurance sport training;
-
C (Comparator): right heart in sedentary individuals;
-
O (Outcomes): morphological and functional ECHO and CMR parameters.
Literature search and selection
Two authors (MP; VC) independently performed the literature search in May 2021. The following databases were used for the search: Medline, Scopus and Cochrane. To conduct a comprehensive systematic literature search, we used both controlled vocabulary and free text terms. For our research, the following MESH terms were used: right ventricle, right atrium, right heart, heart chambers, endurance, athletes, echocardiography, cardiac magnetic resonance, sport, players, remodelling, adaptation, training, work out. Only studies published from 2000 up to May 2021 were accessed. Resulting titles and abstracts of interests were screened by the two authors independently. The full text of the articles of interest were examined. Disagreements about the eligibility of a study were resolved were solved by a third author (FM).
Eligibility criteria
According to the authors’ language capabilities, articles in English, Italian, French, German, Portuguese and Spanish were considered. Studies with level of evidence I to III, according to the Oxford Centre for Evidence-Based Medicine (OCEBM), were considered26. Data from national registries were excluded, as well as reviews, letters, expert opinions, case reports, editorials, animal, computational and cadaveric studies. As the aim was to investigate the remodelling of the right heart in endurance athletes, only study which investigated athletes who regularly played sports listed on the Mitchel Category class C27 were examined. Only studies reporting right heart ECHO and/or CMR parameters of endurance athletes and a sedentary group as controls were eligible. To evaluate chronic adaptations, only CMR or an ECHO evaluation performed at rest were considered. The exclusions criteria were represented by all the variables which could alter the physiological parameters: the presence of diseases, a family history of pulmonary or cardiac diseases, chronic use of drugs.
Data extraction
Data were extracted by two different authors (MP; VC). Data from the following end-points were collected:
-
generalities displayed author and publication year and general characteristics of our population: number of athletes, number of sedentary individuals, sex, age, body mass index (BMI), body surface area (BSA), heart rate (HR), training hours and years of training.
-
ECHO data to assess the morphological and functional parameters of the right heart: basal, middle, longitudinal right ventricle end diastolic diameter (RVED) and their values BSA indexed, right ventricle end diastolic area (RVEDA), end systolic area (RVESA) and their values BSA indexed, right ventricle wall thickness (RVWT), right ventricle E/A (RV E/A), fractional area change (FAC %), ejection fraction (EF %) tricuspid annular plane excursion (TAPSE), right ventricle outflow tract (RVOT1,RVOT2,RVOT3) and their values BSA indexed, right atrial area (RAA), right atrial volume (RAV) and their value BSA indexed.
-
CMR data to assess the morphological and functional parameters of the right heart: right ventricle end diastolic volume (RVEDV), right ventricle end systolic volume (RVESV), right ventricle stroke volume (RVSV), mass and their value BSA indexed and ejection fraction (EF %).
Outcomes of interest
The primary outcome of interest was to investigate the association between right heart remodelling and age, sex, BSA and intensity of training. The second outcome of interest was to compare the mean values of endurance athletes morphological and functional parameters. To underline the different adaptation of RV in male and female among CMR studies, five studies were selected, in which parameters referred to male athletes, male sedentary, female athletes, female sedentary were reported separately. In these studies, the difference of the means between male athletes-male sedentary subjects and female athletes-female sedentary subjects were compared.
Methodological quality assessment
The same two reviewers who extracted data (MP; VC) assessed the risk of bias of the included studies using the Newcastle Ottawa Scale (NOS)28. The NOS evaluates three parameters, namely selection, comparability and exposure. The parameter selection domain includes 4 items useful to check definition and representativeness of cases and controls; the comparability domain includes 1 item to compare cases and controls based on the study design or analysis; the exposure domain includes 3 items to evaluate methods adopted in the study to ascertain exposure for cases and controls28. The maximum score for each study is nine points, and a study with lesser than five points is considered at high risk of bias. The NOS has been described as a reliable tool to assess the quality of case control studies and cohort studies29.
Statistical analysis
For the multivariate analyses, the STATA/MP 16.1 (StataCorp, College Station, TX) was used, with a multiple linear model regression diagnostic. For pairwise correlation, the Pearson Product-Moment Correlation Coefficient (r) was used. The final effect was evaluated according to the Cauchy–Schwarz inequality: + 1 (positive linear correlation) and − 1 (negative linear correlation). Values of 0.1 <| r |< 0.3, 0.3 <| r |< 0.5, and | r |> 0.5 were considered to have small, medium, and strong correlation, respectively. The test of overall significance was performed through the χ2 test, with values of P < 0.05 considered statistically significant. For continuous variable, mean and standard deviation was evaluated. The T test was performed, with P < 0.05 considered statistically significant.
Results
Search results
The search resulted in 2280 articles. After removing duplicates (N = 696), a total of 1584 articles were screened. A further 1166 articles were excluded because of: the type of the study (N = 508), the absence of sedentary controls (N = 193), sports not listed on the Mitchel Category class C (N = 131), language limitations (N = 7), evaluation after an acute stress (N = 118), presence of diseases (N = 209). Another 364 studies were excluded because they did not match the topic of interest or did not report quantitative data on outcome of interest. Finally, 54 articles were included in the analysis: 32 articles reporting ECHO parameters, 20 reporting CMR parameters, 2 reporting both. The flowchart of the literature search is shown in Fig. 1.
Methodological quality assessment
The NOS scale evidenced an overall high quality of the included studies. Studies eligibility criteria and sports category were well described, as were the selection criteria of control groups. The intensity of training was seldom reported. Demographic characteristics were often exhaustively described. The procedure to assess outcomes was overall clearly described. The description of ECHO and CMR results was also comprehensive. A NOS scale score > 8 was achieved by all the included studies.
Population demographic
In ECHO studies, data from 2102 athletes and 1311 sedentary practice were collected. The mean age of athletes and sedentary was 26.6 ± 8.6 and 26.6 ± 7.6, respectively. The BSA was 1.86 ± 0.2 and 1.82 ± 0.15, respectively. The BMI of athletes was 24.8 ± 2.01 and BMI of sedentary was 22.89 ± 1.32. HR was 57.3 ± 7.06 and 69.6 ± 5.26, respectively. In CMR studies, data from 1257 athletes and 909 sedentary subjects were collected. The mean age of athletes and sedentary was 31.5 ± 9.8 and 31.9 ± 8.8, respectively. The BSA was 1.89 ± 0.19 and 1.87 ± 0.15, respectively. The BMI of athletes was 22.4 ± 0.5, and that of sedentary participants was 24.4 ± 1.1. HR was 57.3 ± 7.06 and 63.4 ± 6.9, respectively. Population demographics is shown in Table 1 and in Table 2.
Outcome of interest
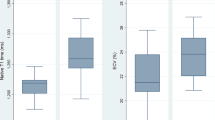
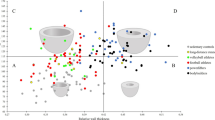
Age showed evidence of statistically significant moderate negative association to RV E/A in athletes (P = 0.009, r = − 0.63). Age showed also a statistically significant negative and strong association to RVED longitudinal in athletes (P = 0.01, r = − 0.7). Age showed evidence of statistically significant strong positive association with an increased rate of progression to RAA both in the athletes and sedentary controls (P = 0.04, r = 0.77, P = 0.02, r = 0.85, respectively). BSA showed statistically significant strong positive association with an increased rate of progression to RVED middle in athletes (P = 0.001, r = 0.71), while in sedentary subject there was evidence of statistically significant moderate positive association with an increased rate of progression (P = 0.05, r = 0.54). Also, BSA showed statistically significant strong positive association with an increased rate of progression to RAA both in athletes and sedentary controls (P = 0.05, r = 0.82, P = 0.04, r = 0.83, respectively). Notably, BSA showed statistically significant strong negative association to ratio RV E/A in athletes (P = 0.002, r = − 0.72). With regard to ECHO data, intensity of training showed evidence of statistically significant strong positive association with an increased rate of progression to RVESA (P = 0.03, r = 0.85). Considering CMR data, the intensity of training presented statistically significant positive and, respectively, strong moderate association to RVEDVI and RVESVI (P = 0.01, r = 0.65, P = 0.01, r = 0.70, respectively). Moreover, evidence of a statistically significant moderate negative association was found between the intensity of training and EF % (P = 0.01, r = − 0.60). The multivariate analysis is shown in Table 3 and supplemental Table 1 (ECHO data) and in Table 4 (CMR data).
A statistically significant difference was observed between RVEDVI means difference values in male and RVEDVI means difference values in female (P = 0.001), as shown in Table 5.
A statistically significant difference was found between all RV ECHO and CMR means in endurance athletes and RV reference means. Results are shown in Table 6 and in Table 7.
In athletes, EF % showed evidence of a statistically significant strong negative association to RVEDV and RVESV (P = 0.01, r = − 0.70, P = 0.0003, r = − 0.89, respectively). Data are reported in Table 8.
Discussion
Endurance athletes demonstrated a statistically significant association between RV remodelling and age, BSA and intensity of training. 2-D ECHO is the easiest way to assess morphological and functional parameters of the right heart, and CMR became fundamental to evaluate the RV morphology23. In fact, it is currently used to diagnose ARVC, although normal range values of both ECHO and CMR parameters in endurance athletes have not been established yet30. Right cardiac chambers remodelling depends on many factors. To analyse the differences between male and female RV adaptation to exercise training, five CMR studies in which data were separated for sex were selected. Changes in morphological and functional parameter both in males (athletes versus sedentary) and in females (athletes versus sedentary) were analysed. There are no differences in the kinetics of trend of adaptation between males and females, with the exception of RVEDV, and all the other parameters showed a similar trend of adaptation both in female and male endurance athletes. Age and increased BSA in athletes are linked to a decrease in diastolic function with a reduction in RV E/A. The intensity of exercise training is associated with heart morphological remodelling. The studies show that 6–8 h/w are sufficient to induce remodelling evident on ECHO and CMR31,32,33. Another goal of this systematic review was to discuss whether the normal RV reference values fitted the RV characteristics in endurance athletes. Athletes involved in endurance sport have different ECHO parameters from those of the general population20. Comparing the studies’ results with the reference values, the mean values of all considered parameters in endurance athletes are higher than those of the general population indicated by the American Society of Echocardiography and the European Association of Cardiovascular Imaging34. Furthermore, there is a difference between the reference mean values adopted for CMR parameters and the mean values in endurance athletes35. This is in accordance with an earlier systematic review, which underlines how endurance sport induces the most significant modification in the right heart, with eccentric hypertrophy12. Such structural changes could lead to incorrectly diagnose ARVC. The ARVC is a group of cardiomyopathies with a similar phenotype and tendency to ventricular arrhythmias. Mutations encoding desmosomal genes are associated to ARVC. In some individuals the phenotypical expression can be triggered by endurance exercise training15. The mean values of RVEDVI are 132.25 ± 9.63 mL/m2 and 109.5 ± 9.35 mL/m2 respectively for males and females, and they are both over the limit of the major criteria for diagnosis of ARVC (≥ 110 mL/m2 for males and ≥ 100 mL/m2 for females)30. The value of 30.24 ± 1.11 mm for RVOT1 is below the limit of major criteria (≥ 32 mm) but it is included in the minor criteria limit (≥ 29 to ≤ 32 mm), while the BSA indexed value (20.18 ± 4 mm/m2) is just above the major criteria limit (≥ 19 mm/m2). The value of 31.83 ± 2.34 mm for RVOT2 is above the limit of the minor criteria (> 32 mm), and the RVOT2/BSA (22.3 ± 3.15 mm/m2) is beyond the limit of the major criteria (> 21 mm/m2). Functional parameters (FAC % and EF %) are not over the limit for diagnosis of ARVC (> 33% to ≤ 40% and > 40% to ≤ 45%, respectively)28. A low value of RV E/A is a sign of diastolic disfunction36. As highlighted in previous studies, age affects diastolic function, with proliferation of extracellular matrix and crosslinking of collagen fibres4. The present study shows that a negative association is evident among athletes, but not among sedentary subjects. Some chronic cardiac microinjuries can emphasise the physiological mechanisms of extracellular matrix rearrangement and fibrotic alteration that normally occur with aging. This leads to a decrease in right heart wall compliance with a reduction in diastolic function. Low values in EF % are related to ventricular chamber dilatation, as shown in Table 8, with a negative association with EDV and ESV. EF % exhibits a negative association with the intensity of training. The more an athlete trains, the more the EF % decreases. Actually, in the case of ventricle dilatation, a lower EF % is necessary to obtain the same SV22.Although EF% decreases, this is not sufficient to justify a systolic disfunction or any other pathological condition, and it should be regarded as a physiological adaptation to the increase in EDV and ESV. To make a correct diagnosis of ARVC, it is important to examine the family history, and to fulfil the other Task Force criteria30. Pathology should be suspected when ECHO shows akinesia, dyskinesia, or an aneurysm, because they are not features of athlete’s heart37. Indeed, the remodelling induced by endurance sport could resemble a cardiomyopathy, but the real impact on future morbidity is still unknown. However, if a subject has a latent ARVC, sport-induced adaptation could deteriorate this condition15,16.
Cardiac remodelling is evident in both sexes, but the lack of studies investigating separately ECHO parameters in male and female athletes does not allow to thoroughly assess similarity and differences. Also, atrial adaptations should be considered, but there are still few studies which analyse atrial chamber remodelling in athletes. A positive association was shown between RAA and age, and between RAA and BSA, but the data available on RA were fewer than data on RV: other studies should be conducted to assess the impact of RA remodelling in endurance athletes. Similarly, years of training were not taken into account because of the lack of relevant data, and further investigations could be conducted to ascertain how many years of training induce permanent RV modifications. The impact of systolic and diastolic disfunction should be analysed considering a longer follow-up period to estimate the incidence of cardiovascular diseases in endurance athletes. Future studies should overcome these limitations to offer a more complete overview.
Conclusion
Endurance athletes exhibit an association between RV remodelling and age, BSA and intensity of training. In particular, RV E/A is an age-related functional parameter, and it should be carefully evaluated because it is a marker of diastolic dysfunction. The systolic function of the RV is decreased in endurance athletes. This is a normal adaptation to exercise, induced by structural changes, and it is within the normal limits. RV ECHO and CMR values in endurance athletes are slightly different from the reference values established in the general population. This could lead to an incorrect diagnosis of ARVC.
References
Bernheim, A. M. et al. Structural and functional cardiac alterations in Ironman athletes: New insights into athlete’s heart remodeling. Int. J. Cardiol. 164, 251–253 (2013).
Koç, M., Bozkurt, A., Akpinar, O., Ergen, N. & Acartürk, E. Right and left ventricular adaptation to training determined by conventional echocardiography and tissue Doppler imaging in young endurance athletes. Acta Cardiol. 62, 13–18 (2007).
D’Andrea, A. et al. Range of right heart measurements in top-level athletes: The training impact. Int. J. Cardiol. 164, 48–57 (2013).
Teske, A. J. et al. Effect of Long term and intensive endurance training in athletes on the age related decline in left and right ventricular diastolic function as assessed by doppler echocardiography. Am. J. Cardiol. 104, 1145–1151 (2009).
Major, Z. et al. Comparison of left and right ventricular adaptation in endurance-trained male athletes. Acta Physiol. Hung. 102, 23–33 (2015).
Bernardino, G. et al. Three-dimensional regional bi-ventricular shape remodeling is associated with exercise capacity in endurance athletes. Eur. J. Appl. Physiol. https://doi.org/10.1007/s00421-020-04335-3 (2020).
Arvidsson, P. M. et al. Left and right ventricular hemodynamic forces in healthy volunteers and elite athletes assessed with 4D flow magnetic resonance imaging. Am. J. Physiol. Hear. Circ. Physiol. 312, H314–H328 (2017).
Bohm, P. et al. Right and left ventricular function and mass in male elite master athletes: A controlled contrast-enhanced cardiovascular magnetic resonance study. Circulation 133, 1927–1935 (2016).
Perseghin, G. et al. Effect of the sporting discipline on the right and left ventricular morphology and function of elite male track runners: A magnetic resonance imaging and phosphorus 31 spectroscopy study. Am. Heart J. 154, 937–942 (2007).
Pelà, G., Bruschi, G., Montagna, L., Manara, M. & Manca, C. Left and right ventricular adaptation assessed by doppler tissue echocardiography in athletes. J. Am. Soc. Echocardiogr. 17, 205–211 (2004).
Morganroth, J., Maron, B. J., Henry, W. L. & Epstein, S. E. Comparative left ventricular dimensions in trained athletes. Ann. Intern. Med. 82, 521–524 (1975).
Utomi, V. et al. Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete’s heart. Heart 99, 1727–1733 (2013).
Gaasch, W. H. & Zile, M. R. Left ventricular structural remodeling in health and disease: With special emphasis on volume, mass, and geometry. J. Am. Coll. Cardiol. 58, 1733–1740 (2011).
Leischik, R. et al. Progress in Cardiovascular Diseases Exercise-induced right ventricular injury or arrhythmogenic cardiomyopathy (ACM): The bright side and the dark side of the moon. Prog. Cardiovasc. Dis. https://doi.org/10.1016/j.pcad.2020.03.015 (2020).
Prior, D. & Gerche, A. La. Exercise and Arrhythmogenic Right Ventricular Cardiomyopathy. Hear. Lung Circ. (2019). https://doi.org/10.1016/j.hlc.2019.12.007.
La Gerche, A. et al. Exercise-induced right ventricular dysfunction is associated with ventricular arrhythmias in endurance athletes. Eur. Heart J. 36, 1998–2010 (2015).
Sharma, S. & Zaidi, A. Exercise-induced arrhythmogenic right ventricular cardiomyopathy: Fact or fallacy?. Eur. Heart J. 33, 938–940 (2012).
Sheffle, N. & Bowden, T. Pre-participation screening for hypertrophic cardiomyopathy in young athletes. Br. J. Card. Nurs. 9, 551–559 (2014).
Heidbüchel, H. et al. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias: Role of an electrophysiologic study in risk stratification. Eur. Heart J. 24, 1473–1480 (2003).
D’Ascenzi, F. et al. Normative reference values of right heart in competitive athletes: A systematic review and meta-analysis. J. Am. Soc. Echocardiogr. 30, 845-858.e2 (2017).
La Gerche, A. et al. Disproportionate exercise load and remodeling of the athlete’s right ventricle. Med. Sci. Sports Exerc. 43, 974–981 (2011).
D’Andrea, A. et al. Physiologische und pathophysiologische Auswirkungen auf das rechte Herz bei Leistungssportlern. Herz 40, 369–378 (2015).
D’Andrea, A. et al. Right heart structural and functional remodeling in athletes. Echocardiography 32, 11–22 (2015).
Shave, R. et al. Exercise-induced cardiac troponin elevation: Evidence, mechanisms, and implications. J. Am. Coll. Cardiol. 56, 169–176 (2010).
Shamseer, L. et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 349, 1–25 (2015).
The 2011 Oxford CEBM Levels of Evidence: Introductory Document. 1–3 (2011).
Mitchell, J. H., Haskell, W., Snell, P. & Van Camp, S. P. Task force 8: Classification of sports. J. Am. Coll. Cardiol. 45, 1364–1367 (2005).
Studies, C. C. Selection 1). 2–4.
Zeng, X. et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 8, 2–10 (2015).
Marcus, F. I. et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the task force criteria. Circulation 121, 1533–1541 (2010).
Bauce, B. et al. Differences and similarities between arrhythmogenic right ventricular cardiomyopathy and athlete’s heart adaptations. Br. J. Sports Med. 44, 148–154 (2010).
Barczuk-Falęcka, M., Małek, ŁA., Krysztofiak, H., Roik, D. & Brzewski, M. Cardiac magnetic resonance assessment of the structural and functional cardiac adaptations to soccer training in school-aged male children. Pediatr. Cardiol. 39, 948–954 (2018).
Scharf, M. et al. Cardiac magnetic resonance assessment of left and right ventricular morphologic and functional adaptations in professional soccer players. Am. Heart J. 159, 911–918 (2010).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 16, 233–271 (2015).
Kawel-Boehm, N. et al. Normal values for cardiovascular magnetic resonance in adults and children. J. Cardiovasc. Magn. Reson. 17, 1–33 (2015).
Zaidi, A. et al. Echocardiographic assessment of the right heart in adults: A practical guideline from the British Society of Echocardiography. Echo Res. Pract. 7, G19–G41 (2020).
D’Ascenzi, F., Solari, M., Corrado, D., Zorzi, A. & Mondillo, S. Diagnostic differentiation between arrhythmogenic cardiomyopathy and athlete’s heart by using imaging. JACC Cardiovasc. Imaging 11, 1327–1339 (2018).
Baggish, A. L. et al. Differences in cardiac parameters among elite rowers and subelite rowers. Med. Sci. Sports Exerc. 42, 1215–1220 (2010).
Bjerring, A. W. et al. Morphological changes and myocardial function assessed by traditional and novel echocardiographic methods in preadolescent athlete’s heart. Eur. J. Prev. Cardiol. 25, 1000–1007 (2018).
D’Ascenzi, F. et al. Characterization of right atrial function and dimension in top-level athletes: A speckle tracking study. Int. J. Cardiovasc. Imaging 29, 87–94 (2013).
D’Ascenzi, F. et al. Electrocardiographic changes induced by endurance training and pubertal development in male children. Am. J. Cardiol. 119, 795–801 (2017).
De Luca, A., Stefani, L. & Galanti, G. Right ventricle chamber of young trained athletes: Morphology and function. Asian J. Sports Med. 4, 281–288 (2013).
Esposito, R. et al. Nonsymmetric myocardial contribution to supranormal right ventricular function in the athlete’s heart: Combined assessment by speckle tracking and real time three-dimensional echocardiography. Echocardiography 31, 996–1004 (2014).
Eun, L. Y. & Chae, H. W. Assessment of myocardial function in elite athlete’s heart at rest—2D speckle tracking echocardiography in Korean elite soccer players. Sci. Rep. 6, 2–7 (2016).
Hedman, K. et al. Female athlete’s heart: Systolic and diastolic function related to circulatory dimensions. Scand. J. Med. Sci. Sport. 25, 372–381 (2015).
King, G. et al. Reduced right ventricular myocardial strain in the elite athlete may not be a consequence of myocardial damage. ‘Cream masquerades as skimmed milk’. Echocardiography 30, 929–935 (2013).
Kooreman, Z. et al. Athletic remodeling in female college athletes: The ‘morganroth hypothesis’ revisited. Clin. J. Sport Med. 29, 224–231 (2019).
Lakatos, B. K. et al. Exercise-induced shift in right ventricular contraction pattern: Novel marker of athlete’s heart?. Am J. Physiol. Hear. Circ. Physiol. 315, H1640–H1648 (2018).
Leischik, R., Foshag, P., Strauss, M. & Spelsberg, N. Left ventricular function and physiological performance in female ironman athletes and female police officers. Percept. Mot. Skills 122, 1002–1022 (2016).
Mirea, O. et al. Multidirectional left ventricle and longitudinal right ventricle deformation analysis by two-dimensional speckle tracking echocardiography in young elite athletes. Acta Cardiol. 71, 395–402 (2016).
Moro, A. S., Okoshi, M. P., Padovani, C. R. & Okoshi, K. Doppler echocardiography in athletes from different sports. Med. Sci. Monit. 19, 187–193 (2013).
Pagourelias, E. D. et al. Right atrial and ventricular adaptations to training in male Caucasian athletes: An echocardiographic study. J. Am. Soc. Echocardiogr. 26, 1344–1352 (2013).
Popple, E. et al. Right ventricular structure and function in senior and academy elite footballers. Scand. J. Med. Sci. Sport. 28, 2617–2624 (2018).
Rimensberger, C., Carlen, F., Brugger, N., Seiler, C. & Wilhelm, M. Right ventricular adaptations and arrhythmias in amateur ultra-endurance athletes. Br. J. Sports Med. 48, 1179–1184 (2014).
Rundqvist, L., Engvall, J., Faresjo, M., Carlsson, E. & Blomstrand, P. Regular endurance training in adolescents impacts atrial and ventricular size and function. Eur. Heart J. Cardiovasc. Imaging 18, 681–687 (2017).
Sanchis-gomar, F. et al. No evidence of adverse cardiac remodeling in former elite endurance athletes. Int. J. Cardiol. 222, 171–177 (2016).
Sanz-de la Garza, M. et al. Influence of gender on right ventricle adaptation to endurance exercise: An ultrasound two-dimensional speckle-tracking stress study. Eur. J. Appl. Physiol. 117, 389–396 (2017).
Simsek, Z., Tas, M. H., Gunay, E. & Degirmenci, H. Speckle-tracking echocardiographic imaging of the right ventricular systolic and diastolic parameters in chronic exercise. Int. J. Cardiovasc. Imaging 29, 1265–1271 (2013).
Sitges, M. et al. Characterizing the spectrum of right ventricular remodelling in response to chronic training. Int. J. Cardiovasc. Imaging 33, 331–339 (2017).
Utomi, V. et al. The impact of chronic endurance and resistance training upon the right ventricular phenotype in male athletes. Eur. J. Appl. Physiol. 115, 1673–1682 (2015).
Vitarelli, A. et al. Comprehensive assessment of biventricular function and aortic stiffness in athletes with different forms of training by three-dimensional echocardiography and strain imaging. Eur. Heart J. Cardiovasc. Imaging 14, 1010–1020 (2013).
Brosnan, M. J., Claessen, G., Heidbuchel, H., Prior, D. L. & La Gerche, A. Right precordial T-wave inversion in healthy endurance athletes can be explained by lateral displacement of the cardiac apex. JACC Clin. Electrophysiol. 1, 84–91 (2015).
Domenech-Ximenos, B. et al. Exercise-induced cardio-pulmonary remodelling in endurance athletes: Not only the heart adapts. Eur. J. Prev. Cardiol. 27, 651–659 (2020).
Dupont, A. C. et al. Aortic compliance variation in long male distance triathletes: A new insight into the athlete’s artery?. J. Sci. Med. Sport 20, 539–542 (2017).
Esch, B. T. et al. Changes in ventricular twist and untwisting with orthostatic stress: Endurance athletes versus normally active individuals. J. Appl. Physiol. 108, 1259–1266 (2010).
Luijkx, T. et al. Sport category is an important determinant of cardiac adaptation: An MRI study. Br. J. Sports Med. 46, 1119–1124 (2012).
Małek, ŁA. et al. Cardiovascular magnetic resonance with parametric mapping in long-term ultra-marathon runners. Eur. J. Radiol. 117, 89–94 (2019).
Prakken, N. H. et al. Cardiac MRI reference values for athletes and nonathletes corrected for body surface area, training hours/week and sex. Eur. J. Cardiovasc. Prev. Rehabil. 17, 198–203 (2010).
Prakken, N. H. et al. The effect of age in the cardiac MRI evaluation of the athlete’s heart. Int. J. Cardiol. 149, 68–73 (2011).
Fagard, R. Athlete’s heart. J. Am. Coll. Cardiol. 40, 634–640 (2002).
Schiros, C. G. et al. Importance of three-dimensional geometric analysis in the assessment of the Athlete’s heart. https://doi.org/10.1016/j.amjcard.2012.12.027 (2013).
Steding-Ehrenborg, K., Boushel, R. C., Calbet, J. A., Åkeson, P. & Mortensen, S. P. Left ventricular atrioventricular plane displacement is preserved with lifelong endurance training and is the main determinant of maximal cardiac output. J. Physiol. 593, 5157–5166 (2015).
Swoboda, P. P. et al. Relationship between cardiac deformation parameters measured by cardiovascular magnetic resonance and aerobic fitness in endurance athletes. J. Cardiovasc. Magn. Reson. 18, 1–8 (2016).
Szelid, Z. et al. Right ventricular adaptation is associated with the Glu298Asp variant of the NOS3 gene in elite athletes. PLoS ONE 10, 1–12 (2015).
Acknowledgements
This study was undertaken in the University of Salerno in collaboration with Universidad Politécnica de Madrid and Universidad Complutense de Madrid. No source of funding was used to assist in design, collection, analysis and interpretation of data or in writing of this study.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
M.P.: collection, analysis, interpretation of the data, writing of the paper; F.M.: analysis, interpretation of the data, writing of the paper; V.C.: collection, interpretation of the data, writing of the paper; M.I.B.: conceptualisation, interpretation of the data, writing of the paper; J.J.R.-Á.: conceptualisation, interpretation of the data, critical revision; F.J.C.M.: conceptualisation, interpretation of the data, writing of the paper; N.M.: conceptualisation, interpretation of the data, writing of the paper, critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Conti, V., Migliorini, F., Pilone, M. et al. Right heart exercise-training-adaptation and remodelling in endurance athletes. Sci Rep 11, 22532 (2021). https://doi.org/10.1038/s41598-021-02028-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02028-1
This article is cited by
-
Lack of cardiac remodelling in elite endurance athletes: an unexpected and not so rare finding
European Journal of Applied Physiology (2024)
-
The athlete’s heart: insights from echocardiography
Echo Research & Practice (2023)
-
Normative values of non-invasively assessed RV function and pulmonary circulation coupling for pre-participation screening derived from 497 male elite athletes
Clinical Research in Cardiology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.