Abstract
There is no recognized serum biomarker to predict the recurrence of endometrial carcinoma (EC). We aimed to explore serum human epididymis protein 4 (HE4) and cancer antigen 125 (CA125) as the biomarkers to predict and monitor recurrence of type II EC. 191 patients diagnosed with type II EC were involved for this retrospective study. Comparing recurrent with non-recurrent patients, HE4 levels resulted a statistically significant difference at primary diagnosis and recurrence, respectively (P = 0.002 and P = < 0.001), while CA125 levels resulted statistically significant (P = < 0.001) at recurrence. According to receiver operating characteristic curve analysis, the areas under the curve were significant for HE4 levels at primary diagnosis and recurrence predicting recurrence. Furthermore, CA125 levels at recurrence were significant. And the combination of both markers showed the higher sensitivity and specificity than single one. Patients with higher HE4 levels were associated with worse disease-free survival and overall survival, the opposite was true for patients with lower HE4 levels. The preoperative HE4 levels could be used to evaluate the risk factors of type II EC. Which suggested that HE4 levels might associated with the prognosis of type II EC. And combination of HE4 and CA125 could be applied to monitor recurrence during follow-up.
Similar content being viewed by others
Introduction
Endometrial carcinoma (EC) is the most common malignancy of the female genital tract and the fourth commonest cancer in women1, most of the EC diagnosed at the early stage, having a favorable prognosis with a 5-year overall survival of 74–91%2. However, 13–17% of the EC patients recur within the first 3 years3,4. EC is usually classified into two types: type I include grade 1 and grade 2 endometrioid carcinoma, and type II refers to grade 3 endometrioid carcinoma and special types (such as serous carcinoma, clear cell carcinoma and carcinosarcoma). Type I EC presents a good prognosis, and type II EC is susceptible to distant metastasis, recurrence and poor prognosis5,6.
Traditionally, EC patients followed up by imaging techniques, such as computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET)7. Yet, these approaches were high expenditure and not handy. Up to now, no consensus has been reached on the serological markers of EC. Overexpression in human epididymis protein 4 (HE4) and cancer antigen 125 (CA125) genes were found in EC patients through The Cancer Genome Atlas (TCGA) gene database (https://cancergenome.nih.gov/) and we found the significantly correlated with the overall survival of EC patients, which indicated that HE4 and CA125 were closely correlated with EC. HE4 and CA125 are commonly used in clinical practice. In clinical practice, HE4 and CA125 have been routinely used to diagnose many malignant tumors, especially ovarian cancer8. Despite previous reports, that the serum tumor markers CA125 and HE4, are significantly correlated with recurrence of EC9,10. Yet CA125 is easily affected by inflammation, endometriosis, and pregnancy, but HE4 is not11. In our knowledge, there is little study on the application of serum HE4 in type II EC.
HE4 is a part of the WAP four-disulfide core family of proteins, belongs to the protease inhibitors. It’s a secreted protein that is overexpressed in malignant tumors, especially in ovarian cancer and EC12.
Current guidelines of the National Comprehensive Cancer Network (NCCN) point out, Patients with EC after initial treatment, who experience symptoms such as abnormal bleeding again or imaging suggests recurrence, commonly, tend to distant metastasis however, leading to poor results of treatment, in the literatures13, the early detection and comprehensive individual treatment of local recurrence, will guide a better prognosis.
The aim of this study was to appraise the appropriateness of HE4 as an indicator for the follow-up of type II EC recurrence, and to evaluate the value of HE4 combined with CA125 in monitoring the recurrence of type II EC, to assess the optimal cut-off value of CA125 and HE4 for type II EC recurrence.
Materials and methods
Patients
191 patients with type II EC (median age 60 years, range 35–89 years), all accepted surgery treatment at the Department of Gynecology, The First Affiliated Hospital of Chongqing Medical University, between May 2011 and August 2019 were included in this retrospective analysis. The stage of the patients was assessed according to the International Federation of Gynecology and Obstetrics (FIGO) staging system14. Patients with progressive disease were excluded from the study. All of the patients accepted surgery at least included total hysterectomy and bilateral salpingo-oophorectomy, advanced-staged patients were also treated for cytoreductive procedures. Most of the patients accepted adjuvant treatment (chemotherapy and/or radiotherapy). Patients Follow-up implemented was from primary diagnosis until the last registered visit or death. Interval time was about 3–6 months for the first 3 years and twice or once a year till 5 years. The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University and was performed in accordance with the tenets of the Declaration of Helsinki, and informed consents were obtained from all patients. Clinical information was collected from the Electronic Medical Record System of The First Affiliated Hospital of Chongqing Medical University.
Quantitative determination of HE4 and CA125 in human serum
3 mL serum specimen was collected before surgery or during follow-up from each patient to detect serum HE4 and CA125 levels by chemiluminescence approach (Abbott Laboratories, US) on the fully automated Architect instrument. Sampling for patients at 3–6 month intervals for first 3 years followed by every 6–12 months thereafter during follow-up. The normal reference value was as follows: pre-menopausal HE4 ≤ 70 pmol/L, post-menopausal HE4 ≤ 140 pmol/L. CA125 < 35U/mL.
Statistical analysis
All statistical calculations were performed with SPSS software (version 25.0; IBM SPSS). A probability of 0.05 was considered to indicate statistical significance. We used the Wilcoxon signed-rank test to estimate the association between serum HE4, CA125 and recurrence. We used receiver operator curves (ROC) were to evaluate the ability of serum biomarker to identify patients with recurrent disease. The optimal cut-off value of serum HE4 and CA125 levels were determined using the maximum Youden index (YI = Sensitivity + Specificity − 1). For survival analysis, disease-free survival (DFS) was defined as the time interval between the date of surgery and the date of recurrence or death/last follow-up, while overall survival (OS) was defined as the time interval between the date of diagnosis and the date of death or last follow-up. Survival models were fitted using the Cox proportional hazard models, while survival curves were drawn based on the Kaplan–Meier methods. All the models assumptions were tested.
Results
A total of 232 patients were diagnosed as type II EC between 2011 and 2019, but 30 patients were lost at follow-up, 11 patients did not undergo surgery only chemotherapy treatment. Consequently, only 191 patients were involved in this retrospective study, Median follow-up was 27 months (range 2–94 months). 42 patients developed recurrent disease, and 42 patients died of the disease. The characteristics of patients are demonstrated in Table 1.
Table 2 shows the correlation between serological markers and pathological factors of type II EC in each group. According to Wilcoxon test, serum CA125 and HE4 are significantly related to clinical pathological risk factors at primary diagnosis, such as depth of myometrial invasion, lymph node status and FIGO stage. The levels of serum HE4 and CA125 elevated significantly in the high-risk groups. In the process of analysis, we found a statistically significant difference between HE4 at initial diagnosis and at recurrence (P = 0.002, P = < 0.001), respectively, comparing recurrent and non-recurrent patients. Otherwise we found a statistically significant difference between CA125 at recurrence (P = < 0.001) comparing recurrent and non-recurrent patients.
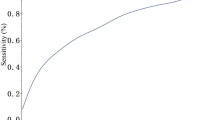
At primary diagnosis time point, in our study, HE4 levels above 89.50 pmol/L demonstrated sensitivity of 61.1% and a specificity of 72.1% in predicting EC recurrence. Furthermore, we found that a HE4 cut-off value of 92.50 pmol/L at recurrence time point is able to monitor patients at recurrence or not, with a sensitivity of 61.3% and a specificity of 96.2%, and a CA125 cut-off value of 32.45 U/mL, with a sensitivity of 71.0% and a specificity of 93.4%. The areas under the curve (AUCs) were not significant for CA125 at primary diagnosis. The combination of both biomarkers was higher associated with recurrence, with a sensitivity of 80.6% and a specificity of 91.5% (Table 3 and Fig. 1).
According to the cut-off level for preoperative serum HE4, we found that patients with higher HE4 levels were associated with worse DFS and OS, while patients with lower HE4 levels were associated with better DFS and OS. (Fig. 2) The univariate cox analysis was used to analyze the clinicopathological factors may affect the prognosis of EC. (Table 4) In addition, we found that the serum HE4 levels exceed 92.50 pmol/L, CA125 levels greater than 32.45 U/mL at recurrence were independent factor for DFS and OS (Table 5).
Discussion
In our study, we found that the preoperative serum HE4 levels of patients without recurrence were significantly lower than those with recurrence. The higher the preoperative serum HE4 levels, the worse the DFS and OS, which suggested that the preoperative serum HE4 levels could be applied to predict the prognosis of patients. There was no statistically significant difference in their preoperative serum CA125 levels. Otherwise, we could monitor the recurrence though the combination of HE4 and CA125 during the follow-up. And in multivariate analysis, patients with higher serum HE4 levels during follow-up had 15.565 times risk for recurrence, 4.493 times risk for death as much as patients with lower serum HE4 levels. Patients with higher CA125 levels during follow-up had 7.864 times risk for recurrence, 8.835 times risk for death as much as patients with lower serum HE4 levels.
HE4 is related to the occurrence and development of EC. The prognosis of patients with EC is poor with the gene mutation. The expression levels of HE4 in EC tissue is significantly higher than those in normal endometrium or benign endometrial lesions. The same is true for serum HE4 levels. Moreover, serum HE4 levels are associated with the tumor load, which is significantly higher before primary treatment than that after primary treatment, and it will elevate with the recurrence10,15.
Previous studies had shown that HE4 and CA125 could be used as biomarkers to distinguish patients with EC from benign lesions, with good sensitivity and specificity, especially the cut-off value for HE4 between 60 and 70 pmol/L. Yilmaz et al. found that the cut-off level for preoperative serum HE4 of 60.95 pmol/L was associated with a sensitivity and specificity of 72.7% and 84.4% for the diagnosis of EC, respectively16. Dewan et al. reported that a sensitivity and specificity of 86.7% and 100% for preoperative serum HE4 of 69.72 pmol/L to identify EC17. The HE4 and CA125 levels were related to tumor heterogeneity. In the previous studies, patients with later stage, poorer differentiation, deep myometrial invasion and lymph node metastasis had higher HE4 and CA125 levels9,18,19,20. Our results were in agreement with them.
However, there were relatively few studies on type II EC. Type II EC has a worse prognosis, and is more prone to recurrence. Early diagnosis and monitoring of recurrence, and timely intervention are essential. In the present study, we showed that the preoperative serum HE4 levels could be used to predict recurrence of patients. For the high-risk patients, postoperative follow-up should be enhanced. In addition, HE4 and CA125 levels during the follow-up could dynamically reflect the tumor load to monitor the recurrence10. HE4 and CA125 have been used as biomarkers for ovarian cancer for decades. Recently, many studies have proposed that HE4 and CA125 could be applied to early diagnosis and monitor the recurrence for EC. A previous study reported that in the multivariate analysis, preoperative serum HE4 levels exceed 81 pmol/L is an independent factor for recurrence21. In our study, a preoperative serum HE4 levels greater than 89.50 pmol/L was associated with a sensitivity and specificity of 61.1% and 72.1% for predicting recurrence, respectively. However, few studies proposed that the role of HE4 and CA125 in monitor recurrence during follow-up after treatment. A study showed that HE4 levels increased during follow-up greater than 70 pmol/L, with a sensitivity and specificity of 81% and 64% for predicting recurrence, respectively10. Our study showed that CA125 levels rose again exceed 32.45 U/mL may indicate recurrence, with a sensitivity and specificity of 71.0% and 93.4%, respectively. For HE4 levels, it was greater than 92.50 pmol/L, with a sensitivity and specificity of 61.3% and 96.2%, respectively.
CA125 is highly susceptible to other factors, such as menstruation, pregnancy, endometriosis and peritonitis22. HE4 is relatively stable, but also affected by smoking, renal failure and so on11,23,24. We found that the combination of the two had a better effect in monitoring recurrence, with a sensitivity and specificity as high as 80.6% and 91.5%, respectively. In addition, we also found that the cut-off value obtained from ROC curve could be used to predict DFS and OS of patients, suggesting that HE4 could be used as a biomarker to predict the prognosis of patients of EC.
As expected, this retrospective study attempts to use HE4 and CA125 for early detection of recurrence, which could precede clinical and imaging manifestation, so that we could diagnose and treat it in time.
A large-scale multi-institutional prospective future research is required to support the value of HE4 and CA125 for the monitoring recurrence of EC.
Conclusion
The preoperative serum HE4 levels could be used to evaluate the risk factors of type II EC, such as later stage, poorer differentiation, deep myometrial invasion and lymph node metastasis, and higher HE4 levels were relative to worse DFS and OS. Which suggested pretreatment HE4 levels might associated with the prognosis of type II EC. What’s more, the combination of HE4 and CA125 could be used to monitor recurrence during follow-up, which contributes to earlier detection and intervention treatment without delay.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 68, 7–30. https://doi.org/10.3322/caac.21442 (2018).
Creasman, W. T. et al. Carcinoma of the corpus uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int. J. Gynaecol. Obstet. 95(Suppl 1), S105-143. https://doi.org/10.1016/S0020-7292(06)60031-3 (2006).
Fung-Kee-Fung, M. et al. Follow-up after primary therapy for endometrial cancer: A systematic review. Gynecol. Oncol. 101, 520–529. https://doi.org/10.1016/j.ygyno.2006.02.011 (2006).
Testa, A. C. et al. Which imaging technique should we use in the follow up of gynaecological cancer?. Best Pract. Res. Clin. Obstet. 28, 769–791. https://doi.org/10.1016/j.bpobgyn.2014.04.008 (2014).
Suarez, A. A., Felix, A. S. & Cohn, D. E. Bokhman redux: Endometrial cancer “types” in the 21st century. Gynecol. Oncol. 144, 243–249. https://doi.org/10.1016/j.ygyno.2016.12.010 (2017).
Bhatla, N. & Denny, L. FIGO cancer report 2018. Int. J. Gynecol. Obstet. 143, 2–3. https://doi.org/10.1002/ijgo.12608 (2018).
Boruta, D. M., Gehrig, P. A., Fader, A. N. & Olawaiye, A. B. Management of women with uterine papillary serous cancer: A Society of Gynecologic Oncology (SGO) review. Gynecol. Oncol. 115, 142–153. https://doi.org/10.1016/j.ygyno.2009.06.011 (2009).
Paunovic, V., Protrka, Z., Ardalic, D. & Paunovic, T. Usefulness of human epididymis protein 4 in predicting optimal cytoreductive therapy in patients with advanced ovarian cancer. J. Buon 22, 29–33 (2017).
Abbink, K. et al. He4 is superior to Ca125 in the detection of recurrent disease in the follow-up of high risk endometrial cancer patients. Int. J. Gynecol. Cancer 27, 1010–1010 (2017).
Brennan, D. J. et al. Serum HE4 detects recurrent endometrial cancer in patients undergoing routine clinical surveillance. BMC Cancer https://doi.org/10.1186/s12885-015-1028-0 (2015).
Huhtinen, K. et al. Serum HE4 concentration differentiates malignant ovarian tumours from ovarian endometriotic cysts. Br. J. Cancer 100, 1315–1319. https://doi.org/10.1038/sj.bjc.6605011 (2009).
Drapkin, R. et al. Human epididymis protein 4 (HE4) is a secreted glycoprotein that is overexpressed by serous and endometriold ovarian carcinomas. Cancer Res. 65, 2162–2169. https://doi.org/10.1158/0008-5472.Can-04-3924 (2005).
Koh, W. J. et al. Uterine neoplasms, Version 1.2018, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 16, 170–199 (2018).
Pecorelli, S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynaecol. Obstet. 105, 103–104. https://doi.org/10.1016/j.ijgo.2009.02.012 (2009).
Angioli, R. et al. The role of HE4 in endometrial cancer recurrence: How to choose the optimal follow-up program. Tumor Biol. 37, 4973–4978. https://doi.org/10.1007/s13277-015-4324-z (2016).
Yilmaz, S. A. et al. The role of human epididymis secretory protein E4 in patients with endometrial cancer and premalignant endometrial lesions. J. Obstet. Gynaecol. 37, 58–63. https://doi.org/10.3109/01443615.2016.1174199 (2017).
Dewan, R., Dewan, A., Hare, S., Bhardwaj, M. & Mehrotra, K. Diagnostic performance of serum human epididymis protein 4 in endometrial carcinoma: A Pilot Study. J. Clin. Diagn. Res. 11, XC01–XC05. https://doi.org/10.7860/JCDR/2017/28926.10285 (2017).
Wang, Y. et al. Predictive value of serum HE4 and CA125 concentrations for lymphatic metastasis of endometrial cancer. Int. J. Gynaecol. Obstet. 136, 58–63. https://doi.org/10.1002/ijgo.12010 (2017).
Brennan, D. J. et al. Serum HE4 as a prognostic marker in endometrial cancer—A population based study. Gynecol. Oncol. 132, 159–165. https://doi.org/10.1016/j.ygyno.2013.10.036 (2014).
Antonsen, S. L. et al. HE4 and CA125 levels in the preoperative assessment of endometrial cancer patients: A prospective multicenter study (ENDOMET). Acta Obstet. Gynecol. Scand. 92, 1313–1322. https://doi.org/10.1111/aogs.12235 (2013).
Mutz-Dehbalaie, I. et al. HE4 is an independent prognostic marker in endometrial cancer patients. Gynecol. Oncol. 126, 186–191. https://doi.org/10.1016/j.ygyno.2012.04.022 (2012).
Buamah, P. Benign conditions associated with raised serum CA-125 concentration. J. Surg. Oncol. 75, 264–265. https://doi.org/10.1002/1096-9098(200012)75:4%3c264::Aid-Jso7%3e3.0.Co;2-Q (2000).
Qu, W. L. et al. Physiopathological factors affecting the diagnostic value of serum HE4-test for gynecologic malignancies. Expert Rev. Mol. Diagn. 16, 1271–1282. https://doi.org/10.1080/14737159.2016.1251317 (2016).
Dochez, V. et al. Efficacy of HE4, CA125, risk of malignancy index and risk of ovarian malignancy index to detect ovarian cancer in women with presumed benign ovarian tumours: A prospective, multicentre trial. J. Clin. Med. https://doi.org/10.3390/jcm8111784 (2019).
Author information
Authors and Affiliations
Contributions
Q.Q., Q.L. and X.M. designed the study, Q.Q. and Q.L. drafted the manuscript, W.Y. and S.Z. conducted the statistical analysis. S.Z. and S.G. collected the data, W.Y. and S.G. were responsible for follow-up. X.M. revised the manuscript. All authors have read and approved the final study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Quan, Q., Liao, Q., Yin, W. et al. Serum HE4 and CA125 combined to predict and monitor recurrence of type II endometrial carcinoma. Sci Rep 11, 21694 (2021). https://doi.org/10.1038/s41598-021-01263-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01263-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.