Abstract
Herein it was evaluated the impact of PD-L1 immunohistochemical expression and stromal tumor-infiltrating lymphocyte (sTIL) counts in pretreatment needle core biopsy on response to neoadjuvant chemotherapy (NACT) for patients with breast carcinomas (BC). In 127 paired pre- and post-NACT BC specimens, immunohistochemical expression of PD-L1 was evaluated in stroma and in neoplastic cells. In the same samples sTILs were semi-quantified in tumor stroma. Post-NACT specimens were histologically rated as having residual cancer burden (RCB of any degree), or with complete pathological response (pCR). PD-L1 expression and higher sTIL counts were associated with histological grade 3 BC. PD-L1 expression was also associated with the non-luminal-HER2+ and triple negative immunohistochemical profiles of BC. Pathological complete response was associated with histological grade 3 tumors, and with the non-luminal-HER2+ and triple negative profiles. Additionally, our results support an association between PD-L1 expression and pCR to NACT. It was also observed that there is a trend to reduction of sTIL counts in the post-NACT specimens of patients with pCR. Of note, PD-L1 was expressed in half of the hormone receptor positive cases, a finding that might expand the potential use of immune checkpoint inhibitors for BC patients.
Similar content being viewed by others
Introduction
Breast cancer is the most common malignancy among women worldwide, excluding non-melanoma skin cancer. This neoplasia accounts for about a third of all cancers and represents the first most frequent cause of death1. In Brazil, breast cancer has an estimated incidence of 66,280 cases for 2020, and a mortality rate of 17,572 patients in 20182. Treatment of breast cancer includes surgery, radiation therapy, chemotherapy, hormone therapy and targeted therapy3,4,5. Breast cancer is a heterogeneous disease classified into different molecular subtypes6,7. An immunohistochemical surrogate panel was proposed to guarantee a wider clinical usage of the molecular typing. This panel includes markers for estrogen (ER) and progesterone receptors (PR), the cell proliferation associated antigen Ki67 and the epidermal growth factor receptor c-erb-B2/Her-2-neu (HER2). A dubious immunohistochemical expression of HER2 implies investigation of gene amplification by fluorescence in situ hybridization8.
Although the classification of breast carcinomas into molecular or immunohistochemical subtypes has contributed to a better stratification of patients for different therapeutic regimens9, a significant number of patients do not benefit from chemotherapy10. The major obstacle in treating any cancer with chemotherapy is the development of chemoresistance, leading to disease progression and metastasis5,11,12,13,14,15. Drug resistance is perhaps the main cause of death associated with cancer and brings significant harm to therapeutic interventions.
This drawback has led to the development of novel therapeutic choices, among which immunotherapy involving the PD-1/PD-L1 axis blockade. Further, PD-L1 expression in breast carcinomas, associated with increased density of stroma tumor-infiltrating lymphocytes (sTILs), shows a plausible predictive value for response to chemotherapy, especially in the context of neoadjuvance16,17,18.
Previous studies have shown expression of PD-L1 in both tumor epithelial cells and sTILs. However, there is still much controversy in defining which pattern of PD-L1 expression is clinically relevant. In positive cases, an irregular distribution pattern, limited to small aggregates of tumoral and/or immune cells predominates19,20. Another challenging issue related to the immunohistochemical evaluation of PD-L1 is the antibody clone and the automated platform in which the reaction is performed. Multiple clones and platforms have been used for different tumor types, as SP-142 and SP-263 (Roche), 22C3 and 28-8 (Dako), ZR3 (Cell Marque), QR1 (Quartett) and others21,22. Finally, subjectivity in scoring the reaction has been verified among pathologists23.
In this scenario, studies in different settings are needed to investigate the clinical value of PD-L1 expression and sTIL counts in breast cancer. The present study was designed to evaluate the relationship between PD-L1 expression and sTIL counts before and after neoadjuvant chemotherapy in women with breast cancer, and their relationship with pathological response.
Materials and methods
Study design, setting and subjects
The present cohort study was conducted at the Women’s Hospital (Hospital da Mulher Professor José Aristodemo Pinotti, Centro de Atenção Integral à Saúde da Mulher—CAISM), State University of Campinas (UNICAMP), São Paulo, Brazil. Women with invasive breast carcinoma who underwent neoadjuvant chemotherapy (NACT) and post-NACT surgery between June 2016 and June 2019 were included. None of them received endocrine therapy in the neoadjuvant scenario. The study was approved by the Research Ethics Committee of Campinas State University (CAAE: 85013718.1.0000.5404). All procedures were carried out according to the Helsinki Declaration and its later amendments. Biological samples were stored at the Biobank number 56 from CAISM. All women signed the informed consent before having their biological samples deposited in the institutional biobank. The diagnosis of breast carcinoma was performed on specimens obtained by percutaneous needle (core) biopsy under ultrasound view. Criteria for indicating NACT included histological subtype, stage and age. NACT followed the institutional clinical protocol, considering the immunohistochemistry based molecular subtype of breast cancer.
The following regimens are indicated as NACT at our hospital: for luminal BC, four cycles of standard chemotherapy with usual anthracycline plus cyclophosphamide, with 21 days intervals, followed by weekly dose of taxane for 12 weeks, the (ACT) regimen24. For HER2 positive BC, the same ACT regimen is applied, plus four cycles of trastuzumab every 21 days, during NACT; then, trastuzumab is given as adjuvant therapy to complete 17 cycles25. Carboplatin is added to standard NACT for triple negative breast cancer (TNBC), to improve pathological complete response (pCR), although this indication is controversial in the literature26. After NACT all women underwent surgical treatment (mastectomy or quadrantectomy with sentinel lymph node biopsy or axillary lymph node dissection), according to the standard institutional protocol. Patients who abandoned treatment and those without available tumor tissue on pre-treatment archival specimens were excluded.
Among 127 women included in the study, three presented bilateral carcinoma. Clinicopathological data, as age, ethnicity, menopausal status, pregnancy, lactation, hormone replacement, family background of breast or ovarian cancer, smoking, clinical tumor stage, and clinical axillary lymph node status were obtained at medical consultation, registered in the medical records and listed on a data collection form. Clinical staging was performed according to the International Federation of Gynecology and Obstetrics system27. Response to chemotherapy was assessed in the surgical specimen post-NACT, according to the Residual Cancer Burden (RCB) online calculator. This reproducible and clinically validated approach allowed scoring of response to therapy as: complete pathological response (pCR), RCB-I (minimum residual disease), RCB-II (moderate residual disease), and RCB-III (extensive residual disease). The pathological reports provided the final residual tumor dimensions (in mm), the percentage of cancer cell areas in the residual tumor bed, and the proportion of in situ component. In addition, the number of positive lymph nodes and the diameter (mm) of the largest nodal metastasis had been informed28. For statistical analyses, cases were clustered into: (a) cases with complete pathological response (pCR), and (b) cases with residual breast carcinoma (RCB-I to RCB-III).
Histopathology and immunohistochemical evaluation
Tissue samples were collected either by percutaneous needle core biopsy (pre-treatment specimens), or during surgical resection after NACT (post-treatment specimens). All samples were fixed in 10% buffered formalin and paraffin-embedded. Hematoxylin–eosin-stained sections were reviewed to confirm the histological diagnosis in the core needle biopsy and in post-NACT tissues. In every case, histological diagnoses were established according to the World Health Organization (WHO) criteria29. Histological non special and special types were included; tumor grade and the presence of vascular invasion were revised.
Stromal tumor-infiltrating lymphocytes (sTILs) were assessed on hematoxylin–eosin-stained slides from matched pre-treatment core needle biopsies and post-neoadjuvant chemotherapy resection specimens. sTILs were assessed according to the guidelines of the Immuno-Oncology Biomarker Working Group29.Although the guidelines for sTILs evaluation have been established for initial diagnostic specimens of tumors, they were also used for residual disease. Stromal TILs were defined as the percentage of tumor stroma area occupied by mononuclear inflammatory cells in the tissue samples. After NACT, in women with residual cancer, sTILs were evaluated in the residual tumor bed, defined as the largest cross-sectional area of residual invasive tumor cells30. In women with pCR, sTILs were assessed in the tumor bed. The criteria described by Dieci et al.30 were used to group sTILs intensity: absent, mild (> 1% to 10%), moderate (11% to 60%), and intense (> 60%). Only sTILs in association to invasive tumors were considered; areas of ductal carcinoma in situ and normal breast lobules were not addressed for sTILs scoring31.
Conventional manual immunohistochemical technique was performed, as follows: tissue sections were deparaffinized in xylene and rehydrated in alcohol gradient; antigen retrieval was made in citrate buffer (pH 6.0) in a regular microwave at 95º C for 30 min; endogenous peroxidase activity was blocked with 0.3% hydrogen peroxidase; then, slides were incubated overnight with the primary antibodies at 8° C; the next morning, primary antibodies were rinsed away with phosphate buffer saline, and the biotin-free peroxidase-conjugated polymer system was applied for one hour at room temperature; freshly prepared 3–3′-diaminobenzidine tetrahydrochloride was used to reveal peroxidase bound to immunocomplexes for 25 min; counterstain was achieved using Harris hematoxylin, followed by dehydration, clearing, and mounting. Positive and negative controls were run in each batch.
Primary antibodies used for the evaluation of molecular types of breast cancer were: anti-estrogen receptor (ER, clone 1D5, diluted at 1:1000), anti-progesterone receptor (PR, clone PR636, diluted at 1:800), anti-HER2 (polyclonal, code A0485, diluted at 1:1100), and proliferation marker Ki67 (clone MIB1, diluted at 1:500). All antibodies and the detection system Envision Flex were provided by Dako—Agilent, Santa Clara, CA, USA. For the evaluation of PD-L1 expression, an anti-PD-L1 rabbit monoclonal antibody was used (clone ZR3; diluted at 1:75, Cell Marque – Sigma-Aldrich, MO, USA)32; in this case, antigen retrieval was made using Tris–EDTA buffer, pH 9.0.
Evaluation of ER and PR was performed according to Allison et al.33, on the diagnostic (pre-treatment) specimens. Cases were considered positive if 1% or more tumor cells were positive. For Ki67, results were represented by the percentage of positive tumor cells in hot spots34. Human epidermal growth factor receptor 2 (HER2) staining was scored as 0 + /1 + (negative), 2 + (equivocal), or 3 + (positive). Equivocal (2 +) cases were further submitted to fluorescence in situ hybridization (FISH) to detect gene amplification in a reference Laboratory, according to the recommendations of the American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP)35. To address tumor heterogeneity, in cases negative for hormone receptors and/or HER2 in immunohistochemistry performed on the pre-treatment tissue sample, immunohistochemistry was remade on the surgical specimens with residual disease for subtype confirmation36.
Cases were grouped according to the reactivity with these markers in four groups: luminal-like (hormone receptor positive/HER2 negative); luminal-HER2 (hormone receptor positive/HER2 positive); non-luminal-HER2 (hormone receptors negative/HER2 positive); triple negative (hormone receptors negative/HER2 negative)8.
PD-L1 assessment was visually estimated on both pre- and post-NACT tissue specimens. Membranous and cytoplasmic staining of epithelial tumor cells and stroma cells were evaluated. A case was considered positive if more than 1% of positive cells were present, in one or both components37,38. In the presence of residual tumor, comparison of PD-L1 expression between pre- and post-NACT specimens was made in tumor and stromal cells. In patients with pCR, only stromal components were compared between pre and post NACT specimens.
As evaluation of PD-L1 immunostaining is not part of the pathologist’s customary routine, it was independently carried out by two pathologists for all 127 matched specimens (LH and KA). After a period of co-observation training, both pathologists estimated the expression of this marker individually. Then, the interobserver agreement was calculated. For discordant cases, a consensus of both pathologists was reached at the coobservation microscope. The same routine was adopted for post-NACT specimens. All other microscopical evaluations were made as standardized in pathology practice.
Statistical analysis
Data were analyzed using the R Environment for Statistical Computing Software39. Significance was set at p < 0.05, with 95% confidence intervals (CIs). First, we assessed the relationship between key clinical and pathological features and PD-L1, sTILs, pathological response status, using a bivariate binomial model; odds ratios and p-values for the associations were calculated. Next, we compared the pre-treatment status (biopsy fragment) and post-neoadjuvant chemotherapy, paired with the sTIL counts (evaluating in both cases with residual disease and with complete pathological response to treatment) and PD-L1 expression (evaluating in both cases with expression only in the lymphoplasmocytic infiltrate, and with expression in histiocytes), using the McNemar's paired chi-squared test.
Four scenarios were possible in relation to sTIL counts: (1) Increased, when sTIL counts were low/negative before and moderate/intense after NACT; (2) Positive stable, when sTILs were moderate/intense before and after NACT; (3) Negative stable, when sTILs were low/negative before and after NACT, and (4) Decreased, when sTILs were moderate/intense before NACT and turned out to be low/negative after NACT. Likewise, four scenarios were possible in relation to PD-L1 expression: (1) Increased, when PD-L1 was negative before and positive after NACT; (2) Positive stable, when PD-L1 was positive before and after NACT; (3) Negative stable, when PD-L1 was negative before and after NACT, and (4) Decreased, when PD-L1 was positive before NACT and turned out to be negative after NACT. Then, we fit a logistic regression model for the association of these four scenarios (using “Increased” as reference) with pathological response. Finally, we produced Box plots for pre- and post-NACT PD-L1 expression according to sTILs rates, including the PD-L1 expression with or without histiocytes and sTIL counts with or without pCR. T-tests were used to compare the mean values of PD-L1 expression according to sTILs status.
Ethics statement
The study follows the recommendations of the Guiding Medical Doctors in Biomedical Research Involving Human Subjects, the Declaration of Helsinki (Declaration of Helsinki III, 1997) and Resolution 441/2012 of the National Health Council.
Results
Clinicopathological findings
Fifty-six patients were under 50 years of age, 107 were caucasian, and 67 were in menopause. Initial biopsy specimens showed predominance of histological non-special type (102 patients, 80.3%); Nottingham grade was 1 or 2 in 62 cases and 3 in 65; vascular invasion was present in 22 cases (16.9%). Ninety-one (71.6%) patients were positive for HR and 51 (40.2%) were positive for HER2. The minority presented Ki67 counts lower than 30% (21 patients, 16.5%) (Tables 1, 2).
HER2 immunohistochemical evaluation resulted in 71 negative cases (scores 0/1 +); 54 equivocal (score 2 +) and two positive (score 3 +) cases. From the 54 equivocal cases, FISH analysis resulted with gene amplification in 38 cases; 15 cases did not present gene amplification. In one case, FISH remained inconclusive (Table 2).
Complete pathological response was achieved in 25 tumors (19.7%), while in 102 there was residual disease (Table 3).
Among the 127 core needle biopsies collected before NACT, 75 (59.0%) expressed PD-L1 either in epithelial or stromal cells. High sTIL counts were present in 55 tumors. None of the clinical characteristics was related to both parameters (Fig. 1, Table 1).
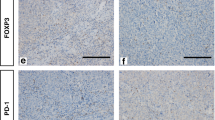
(A) triple negative breast carcinoma: scattered tumor infiltrating lymphocytes (core biopsy, H&E, original magnification 400 ×). (B) triple negative breast carcinoma: aggregates of tumor infiltrating lymphocytes (core biopsy, H&E, original magnification 400 ×). (C) luminal-like, HER2 negative breast carcinoma: PD-L1 positive tumor infiltrating lymphocytes (core biopsy, immunohistochemistry, original magnification 400 ×). (D) luminal-like, HER2 positive breast carcinoma: PD-L1 positive tumor cells (core biopsy, immunohistochemistry, original magnification 400 ×).
Agreement between the two observers for the evaluation of PD-L1 status in pre-treatment biopsy was reached in 63 positive cases, and in 37 negative cases, resulting in an overall agreement (Cohen’s Kappa) of 0.54. For post-NACT specimens, agreement for positive PD-L1 status was reached in 65 cases, and in 36 negative cases, resulting in an overall agreement (Cohen´s Kappa) of 0.55. Discordant cases were mostly represented by those in which the degree of positivity was borderline.
Patients were followed up for at least 26 months, up to 56 months: 94 are alive, disease free; 11 are alive with disease and 22 died of disease. Survival analyses according to PD-L1 expression and sTIL counts in pretreatment core biopsy did not reach significant results (data not shown).
Statistical analyses
In univariate analysis, we observed correlation between higher histological grade (Nottingham) with PD-L1 expression and high sTIL counts. The variables with significant association with PD-L1 in univariate analysis were selected to enter a multivariate regression model; after multivariate adjustment, triple negative BC remained significantly associated with PD-L1 (Table 2).
Twenty-five tumors (19.7%) of the entire cohort evolved with pCR and 102 (80.3%), with residual disease after NACT. In univariate analysis, high histological grade, and PD-L1 overall expression in core needle specimens were associated with complete response rate. After multivariate adjustment, non-luminal-HER2+ and triple negative cases were significantly associated with pCR (Table 3).
Stromal TIL counts in the core needle biopsy did not show significant change in relation to the post-NACT sTIL counts in the surgical specimen; this was valid for both, women with or without residual disease (McNemar test for paired sample p = 0.17 and p = 0.20; Table 4).
Table 5 shows that in patients with residual tumor, 64% remained with low sTIL counts or decreased sTIL numbers and 36% remained with high sTIL counts or increased. Although not statistically significant, there was a trend to decrease in sTIL counts among patients with pCR (p = 0.07).
Comparing PD- L1 status between core needle biopsy and post-NACT surgical specimens, expression status was significantly maintained: positive cases remained mostly positive and negative cases remained mostly negative. This was valid for both evaluations, considering the expression in histiocytes or disregarding these cells (McNemar test for paired sample, p < 0.01; Table 6).
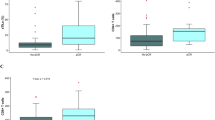
There was a significant association between stromal and epithelial PD-L1 expression with sTIL counts in pre-treatment specimens (Fig. 2A: p = 0.02; Fig. 2B: p < 0.01). In the post-NACT scenario this association also existed when all cases, with or without pCR, were included (Fig. 2E: p = 0.04; Fig. 2F: p = 0.02). No association between the expression of stromal and epithelial PD-L1 with sTIL counts was observed in the post-NACT cenario, when pCR cases were excluded (Fig. 2C: p = 0.40; Fig. 2D: p = 0.12).
In the y-axis, PD-L1 expression is shown as the linear percentage of stained epithelial or stromal cells. In the x-axis, sTIL counts are indicated. (A, C, E) correspond to the values in stromal cells. (B, D, F) correspond to epithelial values. In core needle biopsies (pre-treatment) PD-L1 expression is correlated with sTILs, for both epithelial and stromal compartments (A, B, p = 0.02 and p < 0.01, respectively). The same happened in post-NACT specimens when all cases (with residual disease and pCR) were included (Figures E and F, p = 0.04 and p = 0.02, respectively). However, when only cases with residual disease are considered, this relation was not present (C, D, p = 0.40 and p = 0.12, respectively).
When expression of PD-L1 is considered only on epithelial cells and when it is evaluated in epithelial + stromal components of core needle biopsies, it is associated with pCR (p = 0.02 and p = 0.03, respectively; Table 7).
Table 8 shows that there was no significant change of PD-L1 expression on core needle biopsy versus post-NACT surgical specimens, comparing women with residual cancer or pCR. This is valid either considering PD-L1 expression on histiocytes in the total score, or disregarding them.
Discussion
In the present study PD-L1 expression evaluated in initial biopsies correlated with pathological complete response after NACT. Significance was found either when both neoplastic and stromal cells or when just epithelial cells were considered. Similar results were reached in most studies enrolled in a systematic review by Miglietta et al.40. Only rare studies associated PD-L1 positive expression with the presence of residual disease after NACT41. According to the review by Stovgaard et al.42, all six studies addressed for PD-L1 expression in the NACT setting found significant association between pre-treatment PD-L1 expression and higher pCR. In this review, one of the studies showed association of PD-L1 expression in tumor cells and pCR but did not establish this marker as predictive for complete response in individual subtypes of breast carcinoma43. Another one found association between PD-L1 expression and pCR only in univariate, but not in multivariate analysis44.
Wimberly et al.16 favored a predictive value of PD-L1 expression for pCR applying a particular method, that is, quantitative immunofluorescence evaluation by image analysis and signal amplification with thyramide. As the values were continuous, the cut point to consider PD-L1 positive was statistically set. Cerbelli et al.45 showed association of PD-L1 expression in triple negative breast cancers with pCR, when cut off was set at ≥ 25% positive tumor cells. This controversy shows that studies on PD-L1 expression in breast cancer patients submitted to NACT are still needed, with special emphasis on methodological standardization of immunohistochemical evaluation and correlation with other interfering clinicopathological features. In this respect, the analyses performed in the present study, associating multiple clinical and pathological parameters with PD-L1 expression, were not homogeneously addressed in previous investigations. According to the systematic review from Stovgaard et al.42, PD-L1 expression in breast carcinomas variated between 0 to 83% in all different intrinsic subtypes, and most studies included in the review presented values around 50%, a figure similar to that evidenced in the present study (59%).
Comparison of IHC evaluation of PD-L1 in cancer has been problematic, as different studies use diverse anti-PD-L1 antibodies or platforms. To circumvent this issue there are currently three diagnostics automated IHC assays approved by the Food and Drug Administration (FDA), one using the SP142 clone, the other, the 22C3 clone, and the third, the SP263 clone. Not only the anti-PD-L1 antibody and the platform used are different, but also the scoring systems, with three variations: scoring on tumor cells, on stromal cells and a combination of both, tumor and stromal cells46. The platform using the SP142 clone is scored by ICa (percentage of tumor area covered by PD-L1 positive immune cells)47, and the platform using the 22C3 clone, by CPS (positive tumor or immune cells as percentage of all tumor cells), without possibility of interchange between both scoring systems48. For breast cancer, the ICa score has been suggested, but in a recent evaluation of the three scoring systems, Guo et al.38 advocated the cutoff 1% using the combined score, in tumor and immune cells.
For our study, we performed manual IHC detection of PD-L1 using the ZR3 rabbit monoclonal antibody. The ZR3 clone has been indicated as one of the biosimilar diagnostic antibodies used in clinical practice (Sorokin et al.32; Gonzales-Ericsson et al.49). Scoring was performed by a consensus of two pathologists assessing tumor epithelial cells and stromal immune cells in the tumor microenvironment by visual analysis. The scoring method used in this study for PD-L1 expression is somewhat similar to that of the SP142 assay, using a 1% cutoff, but herein this cutoff was applied to staining of both epithelial and stromal cells in combination38,48.
The predominant association of PD-L1 expression with non-luminal breast carcinomas (27 out of 36, or 75%) and high histological grade (51 out of 65, or 78%) found in our patients is in accordance with previous reports16,40,42,43. PD-L1 expression is particularly frequent in triple negative breast carcinomas, a subtype that most benefits from immunotherapy. Interestingly, among our cases of hormone positive carcinomas PD-L1 was expressed in about half of the cases (48 out of 94, or 52%). This figure is higher than the frequency reported earlier, around 20%42. This figure suggests that immunotherapy might also be appropriate for luminal and PD-L1 positive breast cancers, a proposition which warrants further studies.
Among pathological parameters, complete pathological response (20% of the cases) was associated with grade 3 and absent expression of hormonal receptors, results already reported before45. sTIL counts on initial diagnostic biopsy did not influence pathological response, in opposition with previous reports16,18,50,51. This discrepancy could be attributed to the different proportion of molecular subtypes of breast carcinoma in our study, or to factors related to patient’s biological characteristics. Comparing the initial biopsy with post-NACT specimens in patients with both residual tumor and complete pathological response, we observed a considerable number of cases with pCR which presented a reduction of sTILs after neoadjuvant chemotherapy. This difference, however, did not reach statistical significance (p = 0.07). In a report on 59 paired samples, a significant reduction in sTILs was seen in post-chemotherapy specimens in comparison with baseline samples; PD-L1 expression remained similar in the paired samples18. In this study the greatest decrease in sTILs was associated with pCR. In more recent studies, reduction in sTILs was also detected in post-NACT samples50,51. This decrease could reflect the removal of antigenic stimuli exerted by neoplastic cells, which would be followed by reduction of lymphocyte infiltrates in patients with pCR. An inverse relation, that is, an increase in sTILs in post-NACT surgical specimens, was observed by others52,53, who interpreted their observation as an attractant effect on lymphocytes exerted by chemotherapy. In regard to the maintenance of PD-L1 expression in residual carcinomas, it is possible that such patients could also benefit from inclusion of immune checkpoint inhibitors to conventional therapy18.
Our study presents some limitations, as the relatively small number of the different immunohistochemically defined subtypes of breast carcinoma; the evaluation of more patients with hormone receptor expression, HER2 positive and triple negative would allow the analysis of the clinical impact of PD-L1 expression and sTIL counts within each group. Second, the evaluation of sTILs can be made using markers for different lymphoid subtypes, allowing the determination of which could exert impact on clinical outcomes. In the present report, we used exclusively H&E, according to the guidelines of the International Immuno-Oncology Biomarker Working Group27,28. Finally, long term follow up could allow the evaluation of the influence of such parameters in disease free and overall survivals. However, the patients were enrolled prospectively and had a standardized treatment and evaluation.
Conclusion
The present study supports the role of PD-L1 immunohistochemical expression evaluated in initial biopsies in predicting pCR after NACT. This is valid when only epithelial cells are considered and when both epithelial and stromal cells are included. The value of sTILs in predicting pCR was not confirmed by our data. However, we could support the notion that, in general, post-NACT specimens present decreased numbers of sTILs in patients with pCR. PD-L1 associated with higher histological grade (Nottingham) at diagnosis, with non-luminal-HER2+ and triple negative BC, and with sTIL counts. Besides, our data also support the association of pathological complete response rate with high histological grade, non-luminal-HER2+ and triple negative subtypes of BC. Of note, the higher number of patients with HR + subtype in our study might indicate a potential use of immunotherapy in this group of women. Finally, the methods used herein are applicable in most routine pathology laboratories, supported by consensus studies on scoring of sTILs and PD-L1 expression.
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68(6), 394–424. https://doi.org/10.3322/caac.21492 (2018).
INCA, Instituto Nacional do Câncer. Tipos de cancer: cancer de mama, [Internet], [cited 19 September 2020]. Available from https://www.inca.gov.br/tipos-de-cancer/cancer-de-mama (2020).
Esserman, L. et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: Results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 30(26), 3242–3249. https://doi.org/10.1200/JCO.2011.39.2779 (2012).
Steding, C. E. Creating chemotherapeutic-resistant breast cancer cell lines: Advances and future perspectives. Future Oncol. 12(12), 1517–1527. https://doi.org/10.2217/fon-2016-0059 (2016).
Haque, W. et al. Response rates and pathologic complete response by breast cancer molecular subtype following neoadjuvant chemotherapy. Breast Cancer Res. Treat. 170(3), 559–567. https://doi.org/10.1007/s10549-018-4801-3 (2018).
Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406(6797), 747–752. https://doi.org/10.1038/35021093 (2000).
Haukaas, T. et al. Metabolic clusters of breast cancer in relation to gene- and protein expression subtypes. Cancer Metabol. 4, 12. https://doi.org/10.1186/s40170-016-0152-x (2016).
Kos, Z. & Dabbs, D. J. Biomarker assessment and molecular testing for prognostication in breast cancer. Histopathology 68(1), 70–85. https://doi.org/10.1111/his.12795 (2016).
Cipolla, C. et al. The prognostic value of sentinel lymph node micrometastases in patients with invasive breast carcinoma. Ann. Ital. Chir. 86, 497–502 (2015).
Sparano, J. A. et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N. Engl. J. Med. 379(2), 111–121. https://doi.org/10.1056/NEJMoa1804710 (2018).
Yardley, D. A. Drug resistance and the role of combination chemotherapy in improving patient outcomes. Int. J. Breast Cancer 2013, 137414. https://doi.org/10.1155/2013/137414 (2013).
Majidinia, M. & Yousefi, B. Breast tumor stroma: A driving force in the development of resistance to therapies. Chem. Biol. Drug Des. 89(3), 309–318. https://doi.org/10.1111/cbdd.12893 (2017).
Hong, B., Zhang, J. & Yang, W. Activation of the LKB1-SIK1 signaling pathway inhibits the TGF-β-mediated epithelial-mesenchymal transition and apoptosis resistance of ovarian carcinoma cells. Mol. Med. Rep. 17(2), 2837–2844 (2018).
Lee, A. & Djamgoz, M. Triple negative breast cancer: Emerging therapeutic modalities and novel combination therapies. Cancer Treat. Rev. 62, 110–122. https://doi.org/10.1016/j.ctrv.2017.11.003 (2018).
Santos, J. C. et al. Exosome-mediated breast cancer chemoresistance via miR-155 transfer. Sci. Rep. 8(1), 829. https://doi.org/10.1038/s41598-018-19339-5 (2018).
Wimberly, H. et al. PD-L1 expression correlates with tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy in breast cancer. Cancer Immunol. Res. 3(4), 326–332. https://doi.org/10.1158/2326-6066.CIR-14-0133 (2015).
Du, Q. et al. PD-L1 acts as a promising immune marker to predict the response to neoadjuvant chemotherapy in breast cancer patients. Clin. Breast Cancer 20(1), e99–e111. https://doi.org/10.1016/j.clbc.2019.06.014 (2020).
Pelekanou, V. et al. Tumor-infiltrating lymphocytes and PD-L1 expression in pre- and posttreatment breast cancers in the SWOG S0800 phase II neoadjuvant chemotherapy trial. Mol. Cancer Ther. 17(6), 1324–1331. https://doi.org/10.1158/1535-7163.MCT-17-1005 (2018).
Barrett, M. T. et al. The association of genomic lesions and PD-1/PD-L1 expression in resected triple-negative breast cancers. Breast Cancer Res. BCR 20(1), 71. https://doi.org/10.1186/s13058-018-1004-0 (2018).
Dill, E. A. et al. PD-L1 expression and intratumoral heterogeneity across breast cancer subtypes and stages: An assessment of 245 primary and 40 metastatic tumors. Am. J. Surg. Pathol. 41(3), 334–342. https://doi.org/10.1097/PAS.0000000000000780 (2017).
Haapaniemi, T., Luhtala, S., Tani, T. & Isola, J. Immunohistochemical fluoro-chromogenic triple staining for accurate detection of PD-L1 and PD-1 in NSCLC. In 3rd NordiQC Conference on Applied Immunohistochemistry. Aalborg, Denmark. June 6th–9th, [Internet]. Available from http://nordiqc2017.dk/posters/haapaniemi-et-al/ (2017).
Gaule, P. et al. A quantitative comparison of antibodies to programmed cell death 1 ligand 1. JAMA Oncol. 3(2), 256–259. https://doi.org/10.1001/jamaoncol.2016.3015 (2017).
Reisenbichler, E. S. et al. Prospective multi-institutional evaluation of pathologist assessment of PD-L1 assays for patient selection in triple negative breast cancer. Mod. Pathol. Off. J. U. S. Can. Acad. Pathol. Inc. 33(9), 1746–1752. https://doi.org/10.1038/s41379-020-0544-x (2020).
Sparano, J. A. et al. Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J Med 358(16), 1663–1671. https://doi.org/10.1056/NEJMoa0707056 (2018).
Perez, E. A. et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2-positive breast cancer: Planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 32(33), 3744–3752. https://doi.org/10.1200/JCO.2014.55.5730 (2014).
Lee, J. S. et al. Neoadjuvant treatment for triple negative breast cancer: Recent progresses and challenges. Cancers 12(6), 1404. https://doi.org/10.3390/cancers12061404 (2020).
Lokuhetty, D., White, V. A., Watanabe, R. & Cree, I. A. Breast Tumours 5th edn. (International Agency for Research on Cancer, 2019).
Provenzano, E. et al. Standardization of pathologic evaluation and reporting of postneoadjuvant specimens in clinical trials of breast cancer: recommendations from an international working group. Mod. Pathol. Off. J. U. S. Can. Acad. Pathol. Inc. 28(9), 1185–1201. https://doi.org/10.1038/modpathol.2015.74 (2015).
Denkert, C. et al. Standardized evaluation of tumor-infiltrating lymphocytes in breast cancer: Results of the ring studies of the international immuno-oncology biomarker working group. Mod. Pathol. Off. J. U. S. Can. Acad. Pathol. Inc. 29(10), 1155–1164. https://doi.org/10.1038/modpathol.2016.109 (2016).
Dieci, M. V. et al. International Immuno-Oncology Biomarker Working Group on Breast Cancer (2018). Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: A report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin. Cancer Biol. 52(Pt 2), 16–25. https://doi.org/10.1016/j.semcancer.2017.10.003 (2018).
Hendry, S. et al. Assessing tumor-infiltrating lymphocytes in solid tumors: A practical review for pathologists and proposal for a standardized method from the international immunooncology biomarkers working group: Part 1: Assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv. Anat. Pathol. 24(5), 235–251. https://doi.org/10.1097/PAP.0000000000000162 (2017).
Sorokin, M. et al. RNA sequencing in comparison to immunohistochemistry for measuring cancer biomarkers in breast cancer and lung cancer specimens. Biomedicines 8(5), 114. https://doi.org/10.3390/biomedicines8050114 (2020).
Allison, K. H. et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 38(12), 1346–1366. https://doi.org/10.1200/JCO.19.02309 (2020).
Dowsett, M. et al. International Ki-67 in Breast Cancer Working Group. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J. Natl. Cancer Inst. 103(22), 1656–1664. https://doi.org/10.1093/jnci/djr393 (2011).
Wolff, A. C. et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. Arch. Pathol. Lab. Med. 142(11), 1364–1382. https://doi.org/10.5858/arpa.2018-0902-SA (2018).
Coates, A. S. et al. Tailoring therapies–improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 26(8), 1533–1546. https://doi.org/10.1093/annonc/mdv221 (2015).
Nanda, R. et al. Effect of pembrolizumab plus neoadjuvant chemotherapy on pathologic complete response in women with early-stage breast cancer: An analysis of the ongoing phase 2 adaptively randomized I-SPY2 trial. JAMA Oncol. 6(5), 676–684. https://doi.org/10.1001/jamaoncol.2019.6650 (2020).
Guo, H. et al. Comparison of three scoring methods using the FDA-approved 22C3 immunohistochemistry assay to evaluate PD-L1 expression in breast cancer and their association with clinicopathologic factors. Breast Cancer Res. BCR 22(1), 69. https://doi.org/10.1186/s13058-020-01303-9 (2020).
R Core Team. R: A language and environment for statistical computing. [Internet]. R Foundation for Statistical Computing: Vienna, Austria. Available from http://www.R-project.org/ (2014).
Miglietta, F., Griguolo, G., Guarneri, V. & Dieci, M. V. Programmed cell death ligand 1 in breast cancer: technical aspects, prognostic implications, and predictive value. Oncologist 24(11), e1055–e1069. https://doi.org/10.1634/theoncologist.2019-0197 (2019).
Frank, G. A. et al. PD-L1-status raka molochnoĭ zhelezy [PD-L1 status in breast cancer]. Arkhiv patologii 81(2), 3–9. https://doi.org/10.17116/patol2019810213 (2019).
Stovgaard, E. S., Dyhl-Polk, A., Roslind, A., Balslev, E. & Nielsen, D. PD-L1 expression in breast cancer: Expression in subtypes and prognostic significance: A systematic review. Breast Cancer Res. Treat. 174(3), 571–584. https://doi.org/10.1007/s10549-019-05130-1 (2019).
Kitano, A. et al. Tumour-infiltrating lymphocytes are correlated with higher expression levels of PD-1 and PD-L1 in early breast cancer. ESMO Open 2(2), e000150. https://doi.org/10.1136/esmoopen-2016-000150 (2017).
Wang, Y. et al. Lymphocyte-activation gene-3 expression and prognostic value in neoadjuvant-treated triple-negative breast cancer. J. Breast Cancer 21(2), 124–133. https://doi.org/10.4048/jbc.2018.21.2.124 (2018).
Cerbelli, B. et al. PD-L1 expression in TNBC: A predictive biomarker of response to neoadjuvant chemotherapy?. Biomed. Res. Int. 2017, 1750925. https://doi.org/10.1155/2017/1750925 (2017).
Davis, A. A. & Patel, V. G. The role of PD-L1 expression as a predictive biomarker: An analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors. J. Immunother. Cancer 7(1), 278. https://doi.org/10.1186/s40425-019-0768-9 (2019).
Schmid, P. et al. Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): Updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 21(1), 44–59. https://doi.org/10.1016/S1470-2045(19)30689-8 (2020).
Nanda, R. et al. Pembrolizumab in patients with advanced triple-negative breast cancer: Phase Ib KEYNOTE-012 study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 34(21), 2460–2467. https://doi.org/10.1200/JCO.2015.64.8931 (2016).
Gonzalez-Ericsson, P. I. et al. The path to a better biomarker: application of a risk management framework for the implementation of PD-L1 and TILs as immuno-oncology biomarkers in breast cancer clinical trials and daily practice. J. Pathol. 250(5), 667–684. https://doi.org/10.1002/path.5406 (2020).
Hamy, A. S. et al. Interaction between molecular subtypes and stromal immune infiltration before and after treatment in breast cancer patients treated with neoadjuvant chemotherapy. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 25(22), 6731–6741. https://doi.org/10.1158/1078-0432.CCR-18-3017 (2019).
Lee, H., Lee, M., Seo, J. H., Gong, G. & Lee, H. J. Changes in tumor-infiltrating lymphocytes after neoadjuvant chemotherapy and clinical significance in triple negative breast cancer. Anticancer Res. 40(4), 1883–1890. https://doi.org/10.21873/anticanres.14142 (2020).
Demaria, S. et al. Development of tumor-infiltrating lymphocytes in breast cancer after neoadjuvant paclitaxel chemotherapy. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 7(10), 3025–3030 (2001).
Ladoire, S. et al. Pathologic complete response to neoadjuvant chemotherapy of breast carcinoma is associated with the disappearance of tumor-infiltrating foxp3+ regulatory T cells. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 14(8), 2413–2420. https://doi.org/10.1158/1078-0432.CCR-07-4491 (2008).
Acknowledgements
We thank all the members at Specialized Pathology Laboratory (LAPE-CAISM/UNICAMP) and in the Pathology Research Laboratory/Molecular Pathology of the Pediatric Research Center (CIPED-UNICAMP).
Funding
This study was partially sponsored by Brazilian National Research Council (CNPq No. 303742/2018-6) Brazil, Coordination of Improvement of Higher Education Personnel - Brazil (Capes), São Paulo Research Foundation (FAPESP; No. 2016/07822-4 and 2018/07913-5), and Support to Teaching, Research and Outreach Activities (FEAPEX No 3050/19). This article is part of the master degree of Lucas Grecco Hoffmann under the tutorial of Sophie Derchain, and presented to the Postgraduate Program on Obstetrics and Gynecology from the School of Medical Sciences, the University of Campinas in Brazil, on 2020.
Author information
Authors and Affiliations
Contributions
L.G.H., L.O.S., S.D., and J.V. equally contributed to study design, data evaluation and writing of the final manuscript. G.R.P.S., and K.S.A. contributed with histopathological and immunohistochemistry analysis. D.E.F., and A.C.F. contributed with data collection, analysis and review. S.O.B.R., and R.M.J. contributes with diagnosis, treatment and review protocols.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoffmann, L.G., Sarian, L.O., Vassallo, J. et al. Evaluation of PD-L1 and tumor infiltrating lymphocytes in paired pretreatment biopsies and post neoadjuvant chemotherapy surgical specimens of breast carcinoma. Sci Rep 11, 22478 (2021). https://doi.org/10.1038/s41598-021-00944-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00944-w
This article is cited by
-
Predictive significance of HIF-1α, Snail, and PD-L1 expression in breast cancer
Clinical and Experimental Medicine (2023)
-
Tumor immune microenvironment components and the other markers can predict the efficacy of neoadjuvant chemotherapy for breast cancer
Clinical and Translational Oncology (2023)
-
PD-L1 protein expression in relation to recurrence score values in early-stage ER + breast cancer
Breast Cancer Research and Treatment (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.