Abstract
Data regarding the status of physical activity or understanding of the importance of exercise, such as barriers of exercise or enablers of exercise, in dialysis patients were insufficient. This study aimed to evaluate the status of physical activity and the understanding of the importance of exercise in Korean dialysis patients. The study participants were recruited from 27 hospitals or dialysis centers (n = 1611). Physical activity was evaluated using the Korean version of the International Physical Activity Questionnaire-Short Form. High physical activity was defined as ≥ 600 metabolic equivalent of task (MET). Knowledge about the importance of exercise, enabler for regular exercise, benefits of exercise, and barrier to exercise was evaluated. Health-related quality of life (HRQoL) was assessed by the Kidney Disease Quality of Life version 1.3. The number of participants in the hemodialysis (HD) and peritoneal dialysis (PD) groups was 1247 and 364, respectively. The intensity of physical activity did not differ between the two modalities. The time of physical activity was longer in HD patients than in PD patients, which resulted in greater MET values and the number of high physical activity. There were 762 (61.1%) HD patients and 281 (77.2%) PD patients who heard of the importance of exercise (P < 0.001). In both HD and PD patients, dialysis staff played the most significant role as educators on the importance of exercise and enablers of exercise. The most important barriers to exercise were poor motivation and fatigue in both modalities. HD patients exhibited greater differences in HRQoL scales across two physical activity levels, compared to PD patients. Our study showed that the barrier to exercise and the enablers of exercise were poor motivation/fatigue and encouragement from dialysis staff, respectively.
Similar content being viewed by others
Introduction
End-stage renal disease is an advanced stage of chronic kidney disease requiring renal replacement therapies such as hemodialysis (HD), peritoneal dialysis (PD), or kidney transplantation1, 2. Most end-stage renal disease patients have undergone dialysis because of organ shortage1, 2. High mortality and morbidity rates are observed in dialysis patients3. Advances in dialysis technologies can lead to improved long-term survival in dialysis patients. However, a uremic condition in dialysis patients is a well-known premature aging process4. Improvement in the long-term survival of dialysis patients increases exposure duration to a uremic condition, leading to an increased prevalence of physical disability5. This may result to another medical care burden.
It is well known that the prevalence of physical disability in dialysis patients is higher than that in the general population6. Therefore, knowledge about the importance of exercise to attenuate this problem has been addressed. Previous studies have evaluated knowledge about the importance of exercise in dialysis patients. A recent meta-analysis evaluated 21 randomized trials, and merged data showed that exercise improved the muscle mass and/or muscle strength7. However, all studies showed inconsistent results. Data regarding the current status of physical activity or understanding of the importance of exercise, such as barriers of exercise or enablers of exercise, in dialysis patients were insufficient. In addition, dialysis modality, region, or ethnicity can affect these associations, but there were insufficient data regarding dialysis modality and few data on Korean dialysis patients. This study aimed to evaluate the status of physical activity and the understanding of the importance of exercise in Korean dialysis patients.
Patients and methods
Study population
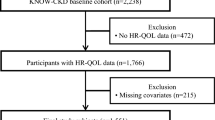
The study participants were initially enrolled in a previous study8. Briefly, the study participants were recruited from 27 hospitals or dialysis centers in Daegu/Kyungsangpook-do between July and December 2012. In total, 2737 participants who received dialysis were included. Participants were excluded if they met the following criteria: age < 20 years (n = 12), history of hospitalization during the past 3 months except for vascular access problems (n = 351), dialysis duration < 6 months (n = 164), unable to walk with or without an assistive device (n = 79), lack of laboratory findings (n = 117), refusal to participate (n = 254), or unable to communicate with interviewer (n = 149). Finally, 1611 participants were ultimately included. This study was approved by the institutional review board of a tertiary medical center (Approval number: 2016-06-022). Informed consent was obtained from all participants. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Study variables
The study variables have been previously described8. Briefly, demographic and laboratory data collected upon enrollment included the following: age, sex, body mass index (BMI; kg/m2), diabetes mellitus (DM), coronary artery disease (CAD), cerebrovascular disease (CVD), dialysis vintage (years), education level, and hemoglobin (mg/dL), blood urea nitrogen (BUN; mg/dL), creatinine (mg/dL), calcium (mg/dL), phosphorus (mg/dL), total cholesterol (mg/dL), serum potassium (mEq/L), intact parathyroid hormone (i-PTH; pg/mL), and high-sensitivity C-reactive protein (hs-CRP; mg/dL) levels, dialysis modality (HD or PD), and type of dialysis or access (arteriovenous fistula [AVF] or arteriovenous graft [AVG] in HD patients and continuous ambulatory PD [CAPD] or automated PD [APD] in PD patients).
DM was evaluated using three indicators: (1) a patient-reported history of DM, (2) the medical record of DM diagnosis or medication, and (3) a fasting glucose level ≥ 126 mg/dL. We evaluated all three indicators for all the patients and DM was diagnosed if one or more indicators among the three were positive. CAD was evaluated using two indicators: (1) a patient-reported history of angina, myocardial infarction, or congestive heart failure, and (2) the medical record for the presence of angina, myocardial infarction, or congestive heart failure. CVD was evaluated using two indicators: (1) a patient-reported history of stroke, and (2) the medical record for the presence of stroke. We evaluated all two sources of evidence for all patients and CAD or CVD were diagnosed if one or more among two indicators were positive.
Assessment for status of physical activity and understanding of the importance of exercise
Physical activity was evaluated using the Korean version of the International Physical Activity Questionnaire-Short Form9. Briefly, physical activity was evaluated regardless if it was leisure or working. Total physical activity was calculated by metabolic equivalent of task (MET) values using the intensity and time of the physical activity. A 3.3 MET was identified for low-intensity physical activity such as walking, 4.0 MET for moderate-intensity physical activity such as moving lightweight materials or cycling in moderate speed, and 8.0 MET for vigorous-intensity physical activity such as aerobics, running, or cycling in high speed. Total MET values were calculated as the sum of MET values × time of physical activity (minutes/week). High physical activity was defined as ≥ 600 MET regardless of intensity or time of physical activity.
All participants were provided with the following questions: “Has the participant ever heard the importance of exercise?” The answer was either “yes” or “no.” If the participant answered “yes,” the next question was “Who told you of the importance of exercise?” The answers were physician, nurse, other dialysis patients, social or mass media, family, friend, nutritionist, social worker, or others. For all participants, the next question was “What is the enabler for regular exercise?” The answers were encouragement from physician; encouragement from nurse; encouragement from family, relatives, or friends; participation in a specialized exercise program; encouragement from other dialysis patients; or presence of an exercise facility.
Further questions were evaluated according to the performance of exercise. If the participant exercised, the question was “What are the benefits of exercise?” The answers were mood, strength, overall vitality (VT), sleeping, confidence, blood pressure, doing the things that the patient wants for himself/herself, muscle cramping, intradialytic hypotension, or others. If the participant did not exercise, the question was “What is the barrier to exercise?” The answers were poor motivation, fatigue, lack of time to exercise, pain, uncertain on how to exercise, depressive mood, fear of injury, lack of equipment or place to exercise, or unsure about the importance of exercise. The answers were in multiple choices.
Definitions
We evaluated disability using four questions with regard to the activities of daily living to assess whether the participants currently needed help from another person to have a meal, dress/undress, get in or out of bed, or take a bath or shower. For each question, they answered one of three responses: “No help needed”; “Some help needed”; “Complete help needed”. Disability was defined as the inability to perform at least one of the four activities of daily living domains without help10.
Exhaustion was measured using two questions from the Center for Epidemiological Studies Depression (CES-D) Scale11: (1) I felt that everything I did was an effort and (2) I could not get going. Then the following question was asked: “How often did you feel this way?” The answer was rarely or none of the time, some or a little of the time, a moderate amount of the time, or most of the time. The participants answering moderate or most of the time to either or both of the two questions were identified as those experiencing exhaustion. A fall was defined as an event that resulted in a participant coming to rest unintentionally on the ground or a lower level with or without losing consciousness during the last 12 months12.
Frailty was defined using the modified criteria previously described elsewhere10, 13,14,15. Components included slowness, poor endurance, physical inactivity, and unintentional weight loss. Slowness and poor endurance were determined by the physical functioning (PF) scale of the Short-Form-36 (SF-36) (2 points for PF scale < 75) and the VT scale of the SF-36 (1 point for VT scale < 55), respectively. Participants who were physically inactive were defined as inactive group (1 point for physical inactivity). Unintentional weight loss was defined as unintentional body weight loss > 4.5 kg or 5% of the baseline value over the past year (1 point for weight loss). All points of scoring of each frailty component were summed. Those participants who scored with ≥ 3 points were defined as having frailty. Cut-off values for PF, VT, or weight loss were defined from the Cardiovascular Health Study, Women’s Health Initiative Observational Study, and the Dialysis Morbidity and Mortality Study Wave 213,14,15. These studies diagnosed frailty using items on the SF-36. Previous studies used a cut-off value dichotomized at the 25th percentile of PF or VT. The cut-off of PF was highly associated with slow walking speed and that of VT was associated with poor endurance. Therefore, 75 < PF and 55 < VT were used to identify slowness and poor endurance, respectively. In addition, the Cardiovascular Health Study and Women’s Health Initiative Observational Study defined unintentional weight loss as the loss of > 10 pound (4.5 kg) over the past year, or more than 5% of the body weight in the previous 2 years. Therefore, we used a similar cut-off value for unintentional weight loss.
Assessment of health-related quality of life scale scores
Health-related quality of life (HRQoL) was assessed by the Kidney Disease Quality of Life (KDQOL) version 1.3 Korean version16. KDQOL version 1.3 includes the SF-36 scale (36 items) and kidney disease-specific scale (11 items). The SF-36 scale includes the following eight domains: PF, role limitations due to physical health problems (RP), body pain, general health, VT, social functioning, role limitations due to emotional problems (RE), mental health (MH), and overall health rating. A total score of 0–100 is calculated for each domain. A low score means a low HRQoL. These scales have been used to calculate the physical component scale (PCS) and mental component scale (MCS)17, 18. The 11-item kidney disease-specific scale consists of symptoms/problems, kidney disease effects, kidney disease burden, work status, cognitive function, quality of social interaction (QSI), sexual function, sleep, social support, patient satisfaction, and dialysis staff encouragement.
Statistical analyses
Data were analyzed using the statistical software SPSS version 25 (Chicago, IL, USA). Categorical variables were expressed as both counts and percentages. Continuous variables were evaluated for the distributional assumption of normality using Kolmogorov–Smirnov test. Continuous variables are expressed as mean ± standard deviation for those with normal distribution and median (interquartile range) for those with non-normal distribution. For continuous variables with normal distribution, means were compared using Student’s t-test. For continuous variables with non-normal distribution, values were compared using Kolmogorov–Smirnov z test. Categorical data was expressed as numbers (percentage) and Pearson’s χ2 or Fisher’s exact test was used to analyze categorical variables. Logistic regression analysis was performed to identify the impact of the dialysis modality for high physical activity. Multivariate analysis was performed using the analysis of covariance or logistic regression analysis and adjusted for age; sex; BMI; DM; CAD; CVD; serum albumin, BUN, creatinine, total cholesterol, i-PTH, and hs-CRP levels; and dialysis modality (PD or HD) or type of dialysis or access (AVF, AVG, or PD). The level of statistical significance was set at P < 0.05.
Results
Participants’ characteristics
The number of participants in the HD and PD groups was 1247 and 364, respectively (Table 1). The mean age in the HD and PD groups was 56.4 ± 13.2 and 54.1 ± 11.9 years, respectively. HD patients were older than PD patients. BMI was greater in PD patients than in HD patients. The proportion of patients with DM, CAD, or CVD was greater in HD patients than in PD patients. The levels of albumin, BUN, or hs-CRP were greater in HD patients than in PD patients, while those of creatinine, total cholesterol, or i-PTH were greater in PD patients than in HD patients.
Current status of physical activity according to dialysis modality
The number of patients with no, low-, moderate-, or vigorous-intensity physical activity was 567 (45.5%), 427 (34.2%), 219 (17.6%), and 34 (2.7%) in HD patients and 161 (44.2%), 135 (37.1%), 63 (17.3%), and 5 (1.4%) in PD patients, respectively (P = 0.409). The time of physical activity was 30 (120) minutes in HD and 30 (87.5) minutes in PD patients, respectively (P = 0.014). The MET value was 90 (360) in HD and 90 (270) in PD patients, respectively (P = 0.021). The two groups had different distributions in time of physical activity and MET. The number of HD or PD patients with high physical activity was 140 (11.2%) and 20 (5.5%), respectively (P = 0.001). The proportion of patients with high MET was greater in HD patients than in PD patients. Multivariate analysis-adjusted covariates showed that MET values in HD and PD patients were 325.1 ± 1.1 and 241.8 ± 1.1, respectively (P = 0.002). Multivariate linear regression analyses showed that old age, female sex, and high BMI levels were inversely associated with MET levels (Table S1). High BUN levels and HD modality were positively associated with MET level.
Logistic regression analysis showed that the odds ratio for high physical activity in HD patients was 2.18 (1.34–3.53) compared to that in PD patients (Table S2, P = 0.002). The odds ratio for high physical activity in HD patients was 3.01 (1.64–5.54) compared to that in PD patients on multivariate analysis (P < 0.001). In addition, multivariate logistic regression analysis showed that those are old in age was associated with lower odds ratio for high physical activity. Those that have high serum albumin, creatinine, or total cholesterol, and undergo HD, were associated with higher odds ratio for high physical activity.
The numbers of patients with disability, frailty, fall, or exhaustion were 195 (15.6%) in HD and 109 (29.9%) in PD (P < 0.001), 421 (33.8%) in HD and 136 (37.4%) in PD (P = 0.204), 225 (18.0%) in HD and 60 (16.5%) in PD (P = 0.493), and 347 (27.8%) in HD and 124 (34.1%) in PD (P = 0.021), respectively. Table S3 show the proportions of patients with disability, frailty, fall, or exhaustion according to physical activity. The participants without high physical activity had significantly higher prevalence of disability, faulty, or exhaustion in HD patients and frailty in PD patients compared to those with high physical activity. Although statistical significance was not obtained in fall in HD patients and disability, fall, or exhaustion in PD patients, the trends were similar.
The numbers of PD patients who had undergone CAPD or APD were 196 (53.8%) and 89 (24.5%), respectively. There were no data for PD modality in 79 patients (21.7%). The numbers with CAPD or APD performing high physical activity were 9 (4.6%) and 6 (6.7%), respectively (P = 0.451). MET values in CAPD or APD patients were 90 (270) and 90 (310), respectively (P = 0.385). There was no significant difference in the proportion of high physical activity and MET values between CAPD and APD.
Patients’ understanding of the importance of exercise according to dialysis modality
There were 762 (61.1%) HD patients and 281 (77.2%) PD patients who heard of the importance of exercise (P < 0.001). In both HD and PD patients, dialysis staff (physician and/or nurse) played the most significant role as educators on the importance of exercise and enablers of exercise (Table 2). The most commonly selected benefits from exercise were mood, strength, and overall VT in both HD and PD patients. Poor motivation and fatigue were the most common barriers to exercise in both HD and PD patients.
With regard to individuals providing education on the importance of exercise, the proportion of nurses was greater in PD patients than in HD patients. The proportion of other dialysis patients was greater in HD patients than in PD patients. For benefits from exercise, the proportion of sleep was greater in PD patients than in HD patients. There were no significant differences in the number of enablers of exercise or barriers to exercise between the two dialysis modalities.
Comparison of HRQoL scale scores according to physical activity
In HD patients, all SF-36 scales and symptoms/problems, cognitive function, and QSI scores among kidney disease-specific scales were greater in patients with high physical activity than in those without high physical activity (Table 3). In PD patients, PF, BP, and PCS in SF-6 scales were greater in patients with high physical activity than in those without high physical activity. Overall improvement of HRQoL scale scores according to physical activity was more prominent in HD patients than in PD patients.
Discussion
Our multicenter cohort study enrolled only relatively stable dialysis patients. We divided patients into two groups according to the dialysis modality. First, the modality per se can be an inherent confounding factor for physical activity or understanding of the importance of exercise. Second, we want to evaluate the association between dialysis modality and physical activity or exercise-related factors. The intensity of physical activity did not differ between the two modalities. Most patients performed low- to moderate-intensity physical activities. The time of physical activity was longer in HD patients than in PD patients, which resulted in greater MET values and the number of high physical activity. Dialysis staff were significantly important for the improvement of exercise in both HD and PD patients, but the importance of dialysis staff was considerably greater in PD patients. The most important barriers to exercise were poor motivation and fatigue in both modalities. HD patients exhibited greater differences in HRQoL scales across the two physical activity levels, compared to PD patients.
In our study, more PD patients recognized the importance of exercise than HD patients. However, HD patients had more time for physical activity than PD patients, but the intensity of physical activity was similar in both modalities. Clinical practitioners or patients may misunderstand that HD patients consume more time for dialysis than PD patients. However, in Korea, most HD patients have undergone HD in a dialysis facility adjacent to their home or workplace, and a number of PD patients have selected the PD modality due to limitation of access to a dialysis facility such as a distant HD facility19. Regarding the time for dialysate exchanges or movement to a PD facility, HD patients may not spend much time for dialysis compared to PD patients. Therefore, lack of time as a barrier to exercise was similar in both modalities at approximately 15%, and lack of an exercise facility or program was not considered an important barrier. The most important barriers to exercise and enablers of exercise were poor motivation and encouragement from dialysis staff, respectively. These findings reveal that frequent visits to a dialysis facility or communication with dialysis staff would be of merit to HD patients, which led to a greater proportion of high physical activities or MET values in HD patients than in PD patients. In addition, poor motivation for exercise in PD patients can be improved by proper and sustained education by dialysis staff on the importance of exercise. The association between physical activity and traveling method or distance to the HD facility is a very interesting issue. Traveling method (walking or car) or distance to the HD facility can be associated with physical activity, and physical activity can also influence the selection of dialysis modality, HD facility, or the traveling method. However, our study did not include the data regarding traveling method or interval between home or workplace and HD facility. Additional studies using these data would be useful in identifying the association between these variables.
Delgado et al. investigated the recognition to exercise in 100 HD patients20. They compared two groups, one with low and the other with high physical activity. Although the most commonly reported barrier to exercise was fatigue, statistical significance was not achieved using multivariate analysis. Lack of motivation, many medical problems, and not having enough time, a safe place to exercise, or an exercise partner were significantly associated with low physical activity. An integrative review study was performed using data from 14 studies regarding data for barriers to exercise in chronic kidney disease21. Although questionnaires regarding barrier to exercise were inconsistent and the patients’ reports on barriers were complex and diverse, the most frequently identified barrier was fatigue or lack of energy. Further, studies evaluated barriers to exercise or physical activity, but certain limitations remained. First, most of the studies had a relatively small sample size between 22 and 269 (the median sample size from 14 studies was 88). Second, most studies focused on HD patients alone. The 12 of 13 studies using dialysis patients were performed using HD patients alone and a total sample size of 1 study using both HD and PD patients consisted of only 78 responses (including 19 from PD patients). Third, 7 of 14 studies were carried out on multiple ethnicities, 2 studies evaluated only a single ethnicity, and 5 studies did not present ethinicity as a variable. Although multiple ethnicities might be useful in studies in terms of generalizability, this may be confounding element in small sample size studies. Our study enrolled both HD and PD patients and had both a large sample size and a single ethnicity (only Asian dialysis patients, including 1,247 HD and 364 PD patients). Our results showed that poor motivation and fatigue were most common barriers to exercise in HD patients (similar results compared to previous results) and same trends were also observed from PD patients.
Although there are few high-quality studies regarding the association between exercise and HRQoL scales in dialysis patients, many clinical practitioners suggest that exercise can improve both physical health and MH22,23,24,25. In our study, almost all scales associated with physical health and MH were greater in HD patients with high physical activity than in those without high physical activity. Dialysis patients also understood the impact of exercise on mood, strength, or VT. For the kidney disease-specific scale, symptoms/problems, cognitive function, and QSI were greater in HD patients with high physical activity than in those without high physical activity. However, there were no statistically significant differences in PD patients with high physical activity compared to in those without high physical activity (except body pain). Two issues may be associated with this non-difference. Sustained peritoneal dialysate in the abdomen can attenuate the impact of physical activity on some physical health/MH scales or the kidney disease-specific scales, and a small number of PD patients on high physical activity also led to statistical non-significance. In addition, disability, frailty, fall, or exhaustion was greater in HD patients without high physical activity than in those with high physical activity. Moreover, in PD patients, frailty alone differed between the two groups. However, trends for disability, fall, or exhaustion were similar with the results from HD patients.
In our study, clinical symptom was not an important barrier to exercise. Moorman et al. showed that the barrier to exercise was excessive tiredness or weakness or shortness of breath26. In our study, all dialysis patients were ambulatory and medically stable. Therefore, only a few patients had difficulty in exercising due to a medical problem such as shortness of breath, except pain.
The present study had a few limitations. First, it had a retrospective design and used data on participants enrolled in a previous study8. In addition, our study was analyzed using data collected at approximately 10 years ago. Many factors, including patients’ characteristics, social, or environmental conditions at onset of data would be different compared to those using recent patients, which may lead to different results. In addition, social, educational, cultural, and environmental factors can influence outcomes related to physical activity, quality of life, and awareness of the need for exercise. However, we did not perform analyses using these data. Second, the present study did not include data from physical performance measurements as an accurate indicator, and the presence of physical activity and understanding of the importance of exercise were evaluated using questionnaires alone. In addition, our data did not include the data regarding bicarbonate, Kt/Vurea, and dialysis treatment adherence and we did not perform a multivariate analysis including these variables. Our results were evaluated without adjusting these variables as possible confounding factors. Current guidelines recommend Kt/Vurea ≥ 1.2 for HD and weekly Kt/Vurea ≥ 1.7 for PD27, 28. Previous data from a representative sample of Koreans showed that the proportion of patients with inadequate HD was 8.5%29. Mean weekly Kt/Vurea for PD was 1.9 ± 0.8 in Korea and a significant portion of PD would be adequate2. Most of the patients from our study may be undergoing adequate dialysis and these may attenuate the effects on physical disability or activity resulting from significantly inadequate dialysis. Third, our study, as a cross-sectional analysis, did not evaluate the causal relationship between physical activity and outcome measurements such as HRQoL scales, disability, frailty, fall, or exhaustion. Fourth, high physical activity was defined as participants ≥ 600 MET, and the number of participants with MET values ≥ 3000, which was classified as a high amount of physical activity, was only 5 (0.4%) in HD patients and 0 in PD patients. Therefore, we did not evaluate the impact of the amount of physical activity. Fifth, exhaustion in our study was defined using two of 20 questions from the CES-D scale for the diagnosis of depression. These 2 questions were classified as indicators of somatic activity30. Evaluation of exhaustion using two questions saves time and is simple. These are originally derived from a questionnaire for the diagnosis of a depressive mood and may not accurately reflect an experience of physical exhaustion. However, Vestergaard et al. evaluated the presence of exhaustion using two questions and observations of physical functioning31. They demonstrated that there was a positive association between the presence of exhaustion and physical activities, including handgrip strength, gait speed, disability, and a short physical performance battery. In addition, Fried et al. used these two questions as a component in their diagnosis of frailty14. A prospective study including additional parameters such as physical performance measurements and interventions for exercise is warranted to overcome these limitations.
In conclusion, our study showed that the barrier to exercise and the enablers of exercise were poor motivation/fatigue and encouragement from dialysis staff, respectively. The frequent contact with medical staff in a HD facility may be associated with a greater amount of high physical activity in HD patients than in PD patients.
References
US Renal Data System. USRDS 2020 Annual Data Report: Atlas of Chronic Kidney Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2020. Available at: https://adr.usrds.org/2020/. Accessed: 23 July 2021.
ESRD Registry Committee: Korean Society of Nephrology. Current Renal Replacement Therapy in Korea, 2020. Available at: http://www.ksn.or.kr/rang_board/list.html?code=sinchart. Accessed: 23 July 2021.
Australia and New Zealand Dialysis and Transplant Registry. 43rd annual ANZDATA report. Available at: https://www.anzdata.org.au/report/anzdata-43rd-annual-report-2020-data-to-2019/. Accessed: 23 July 2021.
Kooman, J. P. et al. Out of control: Accelerated aging in uremia. Nephrol. Dial. Transplant. 28, 48–54 (2013).
Ren, H., Gong, D., Jia, F., Xu, B. & Liu, Z. Sarcopenia in patients undergoing maintenance hemodialysis: Incidence rate, risk factors and its effect on survival risk. Ren. Fail. 38, 364–371 (2016).
Singer, M. A., Hopman, W. M. & MacKenzie, T. A. Physical functioning and mental health in patients with chronic medical conditions. Qual. Life Res. 8, 687–691 (1999).
Lu, Y., Wang, Y. & Lu, Q. Effects of exercise on muscle fitness in dialysis patients: A systematic review and meta-analysis. Am. J. Nephrol. 50, 291–302 (2019).
Lee, S. Y. et al. The prevalence, association, and clinical outcomes of frailty in maintenance dialysis patients. J. Ren. Nutr. 27, 106–112 (2017).
The International Physical Activity Questionnaire, 2005. Available at https://sites.google.com/site/theipaq/. Accessed 6 January 2021.
Woods, N. F. et al. Frailty: Emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. J. Am. Geriatr. Soc. 53, 1321–1330 (2005).
Orme, J., Reis, J. & Herz, E. Factorial and discriminate validity of the Center for Epidemiological Studies Depression (CES-D) Scale. J. Clin. Psychol. 42, 28–33 (1986).
Buchner, D. M. et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc. 41, 297–308 (1993).
Johansen, K. L., Chertow, G. M., Jin, C. & Kutner, N. G. Significance of frailty among dialysis patients. J. Am. Soc. Nephrol. 18, 2960–2697 (2007).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56A, M146–M156 (2001).
O’Hare, A. M., Tawney, K., Bacchetti, P. & Johansen, K. L. Decreased survival among sedentary patients undergoing dialysis: Results from the dialysis morbidity and mortality study wave 2. Am. J. Kidney Dis. 41, 447–454 (2003).
Park, H. J. et al. Reliability and validity of the Korean version of Kidney Disease Quality of Life instrument (KDQOL-SF). Tohoku J. Exp. Med. 211, 321–329 (2007).
Ware, J. E., Jr, & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 30, 473–483 (1992).
McHorney, C. A., Ware, J. E., Jr, Raczek, A. E. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 31, 247–263 (1993).
Wang, V. et al. Impacts of geographic distance on peritoneal dialysis utilization: Refining models of treatment selection. Health Serv. Res. 52, 35–55 (2017).
Delgado, C. & Johansen, K. L. Barriers to exercise participation among dialysis patients. Nephrol. Dial. Transplant. 37, 1152–1157 (2012).
Hannan, M. & Bronas, U. G. Barriers to exercise for patients with renal disease: An integrative review. J. Nephrol. 30, 729–741 (2017).
Lopes, A. A. et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: The DOPPS. Clin. J. Am. Soc. Nephrol. 9, 1702–1712 (2014).
Gonçalves, F. A. et al. Quality of life in chronic renal patients on hemodialysis or peritoneal dialysis: a comparative study in a referral service of Curitiba—PR. J. Bras. Nefrol. 37, 467–474 (2015).
Thangarasa, T., Imtiaz, R., Hiremath, S., Zimmerman, D. Physical activity in patients treated with peritoneal dialysis: A systematic review and meta-analysis. Can. J. Kidney Health Dis. 5, 2054358118779821. https://doi.org/10.1177/2054358118779821 (2018).
Manfredini, F. et al. Exercise in patients on dialysis: A multicenter, randomized clinical trial. J. Am. Soc. Nephrol. 28, 1259–1268 (2017).
Moorman, D. et al. Benefits and barriers to and desired outcomes with exercise in patients with ESKD. Clin. J. Am. Soc. Nephrol. 14, 268–276 (2019).
Hemodialysis Adequacy 2006 Work Group. Clinical practice guidelines for hemodialysis adequacy, update 2006. Am J Kidney Dis. 48(Suppl 1), S2–S90 (2006).
Peritoneal Dialysis Adequacy Work Group. Clinical practice guidelines for peritoneal dialysis adequacy. Am. J. Kidney Dis. 48(Suppl 1), S98–S129 (2006).
Kim, S. H., Kim, Y. K. & Yang, C. W. The efficacy of dialysis adequacy. J. Korean Med. Assoc. 56, 583–591 (2013).
Poresky, R. H., Clark, K. & Daniels, A. M. Longitudinal characteristics of the Center for Epidemiologic Studies-Depression Scale. Psychol. Rep. 86, 819–826 (2000).
Vestergaard, S. et al. Fatigue in a representative population of older persons and its association with functional impairment, functional limitation, and disability. J. Gerontol. A Biol. Sci. Med. Sci. 64, 76–82 (2009).
Funding
This work was supported by the Medical Research Center Program (2015R1A5A2009124) through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
S.H.K. conceptualized and designed the study, performed the analysis and interpretation of data, and wrote the manuscript. S.H.K., J.Y.D., and J.C.K. generated and collected the data. J.Y.D. and J.C.K. drafted and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, J.C., Young Do, J. & Kang, S.H. Comparisons of physical activity and understanding of the importance of exercise according to dialysis modality in maintenance dialysis patients. Sci Rep 11, 21487 (2021). https://doi.org/10.1038/s41598-021-00924-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00924-0
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.