Abstract
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) blood pressure (BP) guidelines lowered the hypertension threshold to ≥ 130/80 mmHg, but the role of diastolic BP remains contested. This two-sample mendelian randomisation study used replicated genetic variants predicting systolic and diastolic BP applied to the UK Biobank and large genetic consortia, including of cardiovascular diseases and parental lifespan, to obtain total and direct effects. Systolic and diastolic BP had positive total effects on CVD (odds ratio (OR) per standard deviation 2.15, 95% confidence interval (CI) 1.95, 2.37 and OR 1.91, 95% CI 1.73, 2.11, respectively). Direct effects were similar for systolic BP (OR 1.83, 95% CI 1.48, 2.25) but completely attenuated for diastolic BP (1.18, 95% CI 0.97, 1.44), although diastolic BP was associated with coronary artery disease (OR 1.24, 95% CI 1.03, 1.50). Systolic and diastolic BP had similarly negative total (− 0.20 parental attained age z-score, 95% CI − 0.22, − 0.17 and − 0.17, 95% CI − 0.20, − 0.15, respectively) and direct negative effects on longevity. Our findings suggest systolic BP has larger direct effects than diastolic BP on CVD, but both have negative effects (total and direct) on longevity, supporting the 2017 ACC/AHA guidelines lowering both BP targets.
Similar content being viewed by others
Introduction
Elevated blood pressure (BP), or hypertension, increases the risk of dying from cardiovascular disease (CVD)1, and is one of the most important factors determining population health worldwide2. The number of adults with hypertension has increased from 594 million in 1975 to 1.13 billion in 2015, driven by increasing prevalence in south Asia and sub-Saharan Africa3, as well as the evolving definition of hypertension4. In 2017 the American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommended reducing the threshold for hypertension from 140/90 to 130/80 mmHg5,6, largely based on results from the Systolic Blood Pressure Intervention Trial (SPRINT). However, the SPRINT trial focused on systolic BP, which raised the questions as to whether lowering the diastolic BP threshold was necessary7, and reignited interest in the importance of BP components, particularly diastolic BP8,9.
Trials of specifically reducing diastolic BP without changing systolic BP are difficult to conduct, meaning the importance of diastolic BP remains to be fully elucidated. Observational studies are open to both confounding and selection bias which may bias estimates. Mendelian randomisation (MR) using genetic variants as instrumental variables10, which are randomly allocated at conception, is much less open to confounding11. Previous MR studies suggested diastolic BP was not associated with CVD overall or by subtype independent of systolic BP12, and was inversely associated with risk of large artery stroke13, suggesting some cerebrovascular-protective effects of diastolic BP. Another MR study suggested diastolic BP was more strongly associated with shorter lifespan than systolic BP14, but did not consider the relative contribution of systolic and diastolic BP together, i.e. direct as well as total effects. From a population health perspective, the overall health benefits of achieving a low diastolic BP is probably more relevant because elevated BP likely has other non-cardiovascular consequences15.
Here, we examined the effects of systolic and diastolic BP on CVD, its subtypes, and lifespan, using multivariable MR, which is an increasingly popular method of considering multiple risk factors simultaneously16,17. Specifically, we used replicated genetic instruments and the largest publicly available genetic studies of CVD and longevity.
Results
Total effects of systolic and diastolic BP
The 272 and 267 strong, independent and replicated SNPs predicting systolic and diastolic BP had mean (range) F-statistic for systolic and diastolic BP of 83.2 (29.3–612.4) and 90.7 (30.0–818.1), indicating bias due to weak instruments is unlikely. These SNPs explained approximately 2.59 and 2.96% of the variance of systolic and diastolic BP, respectively. Of these SNPs, 10 SNPs for systolic BP and 9 SNPs for diastolic BP were not available in the parental lifespan GWAS, nor were their proxies. The I2 statistics were at least 92.5% for systolic, and 93.8% for diastolic BP. Power calculations showed that at 5% alpha, this study has 80% power to detect, in the univariable MR. an odds ratio (OR) of about 1.11 for coronary artery disease, 1.11 for ischaemic stroke (1.19 in the UK Biobank), 1.09 for heart failure, 1.08 for atrial fibrillation and a beta coefficient of 0.04 standardised combined parental attained age. Supplementary Tables S1-S2 show the SNPs used. These SNPs explained a larger proportion of the phenotypic variance of systolic and diastolic BP, than of the outcomes considered, suggesting reverse causality was unlikely.
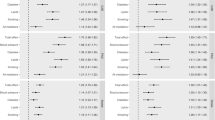
Both systolic and diastolic BP were positively associated with major CVD events, (OR 2.15 [95% confidence interval (CI) 1.95, 2.37] and 1.91 [95% CI 1.73, 2.11], respectively) (Fig. 1 and supplementary Table S3). For CVD subtypes, both systolic and diastolic BP were most strongly associated with coronary artery disease, and least strongly associated with atrial fibrillation, as well as being positively associated with ischaemic stroke and heart failure. The MR-Egger intercepts (minimum P for intercept 0.081) did not suggest these IVW estimates were invalid. Higher systolic (beta coefficient − 0.20 [95% CI − 0.22, − 0.17]) and diastolic (beta coefficient − 0.17 [95% CI − 0.20, − 0.15]) BP were inversely associated with parental lifespan (Fig. 1 and supplementary Table S3), equivalent to 2.9 and 2.6 years lower combined parental attained age per SD of BP. Estimates obtained using the weighted median and MR-PRESSO were generally concordant in direction and magnitude. Using Phenoscanner, we identified 15 and 18 potential pleiotropic SNPs for systolic and diastolic BP that were strongly (P < 5 × 10–8) associated with mostly BMI (supplementary Tables S4A and B). Excluding these SNPs gave similar MR estimates (supplementary Table S5). Higher pulse pressure was positively associated with all CVD outcomes considered, and inversely associated with parental lifespan (supplementary Table S6).
Direct effects of systolic and diastolic BP
Of the 392 SNPs for systolic and diastolic BP, 312 SNPs were independent (r2 < 0.001), rs73033340 or its proxies were not available in the systolic BP GWAS, leaving 311 SNPs (299 for parental lifespan) for the multivariable MR analyses. Of these, 178 SNPs were associated with both systolic (243) and diastolic BP (246) at P < 5 × 10–8. The multivariate F-statistics for the genetic instruments for systolic and diastolic BP, taking into account their phenotypic correlation, were 31.1 and 32.1, respectively, indicating strong instruments for multivariable MR.
Direct effects of systolic and diastolic BP were attenuated compared to the total effects, with stronger associations for systolic than diastolic BP (Fig. 1 and supplementary Table S7). Systolic (OR 1.83 [95% CI 1.48, 2.25]), but not diastolic BP (OR 1.18 [95% CI 0.97, 1.44]) remained positively associated with major CVD events. Systolic BP was positively associated with all CVD subtypes considered. In contrast, diastolic BP remained only nominally associated with coronary artery disease (OR 1.24 [95% CI 1.03, 1.50], p = 0.023), but not with ischaemic stroke (OR 1.12 [95% 0.94, 1.33], heart failure (OR 1.05 [95% CI 0.87, 1.28]) or atrial fibrillation (OR 1.08 [95% CI 0.88, 1.33]). Higher systolic BP (beta coefficient − 0.13 [95% CI − 0.19, − 0.07] and diastolic BP (beta coefficient − 0.07 [95% CI − 0.12, − 0.02]) remained inversely associated with parental lifespan (Fig. 1 and supplementary Table S7), equivalent to − 1.9 and − 1.0 years per SD BP, respectively. There was statistical evidence of pleiotropic effects from the modified Cochran’s Q test, and potential directional pleiotropy based on the multivariable MR-Egger intercepts for systolic BP and the UK Biobank estimates including major CVD events (p for intercept = 0.03) and coronary artery disease (p for intercept = 0.03). However, the MR-Egger estimates suggested similar but larger effect sizes (supplementary Table S7), and estimates from other multivariable MR methods, as well as the sensitivity analysis further adjusting for education, smoking and BMI in the multivariable IVW models, were consistent with the main IVW estimates (supplementary Table S7). Repeating the analysis using genetic associations with BP unadjusted for BMI yielded univariable (supplementary Table S8) and multivariable (supplementary Table S9) results with a similar interpretation.
Discussion
Consistent with previous MR studies18,19,20, and trials21,22, higher systolic and diastolic BP were associated with higher risk of CVD. Multivariable MR showed that higher systolic BP was associated with higher risk of CVD overall and by subtype. Diastolic BP was nominally associated with coronary artery disease, but not with CVD overall and other subtypes independent of systolic BP. However, both systolic and diastolic BP independently contributed to lifespan. Taken together, our results demonstrate that systolic and diastolic BP are both targets of intervention.
Although we used a study design less susceptible to confounding than conventional observational studies, our findings are broadly consistent with observational studies showing that systolic-diastolic and isolated systolic hypertension are associated with higher risk of CVD, with less conclusive findings for isolated diastolic hypertension8,9,23,24. Using genetic variants independently predicting BP which were stringently selected by LD independence and external replicability in this MR study, we found that lifetime exposure to higher diastolic BP was associated with shorter lifespan and possibly higher risk of coronary artery disease, even after accounting for effects via systolic BP, which are less consistent with previous multivariable MR analyses12,13. Here, the multivariate F statistics for the genetic instruments for systolic and diastolic BP were greater than the rule-of-thumb value of 10, circumventing weak instrument bias possibly towards the null in a previous MR12,25. We extensively validated our multivariable MR findings. Other than removing SNPs associated with confounders of BP and CVD/lifespan13, we used other multivariable MR methods, including multivariable weighted median and MR-PRESSO, we also used genetic associations unadjusted for BMI to circumvent selection bias due to conditioning on heritable traits26. Our findings therefore provide additional confirmation of the harmful effects of diastolic BP independent of systolic BP. Notably, effects of diastolic BP on CVD were more substantially attenuated than those of systolic BP when considering systolic and diastolic BP together. However, we observed independent effects of diastolic BP reducing lifespan proxied by parental attained age inclusive of deaths occurring at younger ages. On one hand, these results may suggest that the total effects of diastolic BP can be largely attributed to systolic BP given systolic and diastolic BP are highly correlated phenotypically27 and genetically28. On the other hand, diastolic BP was less consistently associated with CVD by subtype as it was not associated with ischaemic stroke, heart failure or atrial fibrillation. We cannot exclude the possibility of selection bias attenuating estimates for diastolic BP because GWAS are a non-random subset of their underlying birth cohorts who survive long enough to be included29, thus necessitating the inclusion of lifespan phenotypes less affected by this issue. Isolated diastolic hypertension is more common in early life30, so the possibility remains that higher diastolic BP precludes survival to recruitment more strongly than higher systolic BP, meaning that estimates for diastolic BP on the CVDs that occur later in life, such as ischaemic stroke, heart failure and atrial fibrillation31, are more artefactually attenuated than those for systolic BP. Observationally, in a young sample, isolated diastolic and isolated systolic hypertension had similar contributions to major CVD events32. Systolic and diastolic BP had similar total and direct effects on lifespan, consistent with a previous MR study14, which again suggests the possibility that estimates for diastolic BP are artefactually attenuated by diastolic BP having a greater effect than systolic BP on mortality at younger ages from other causes of death33.
Some limitations of this study should be mentioned. The validity of MR relies on the three major instrumental variable assumptions. First, the genetic instruments should be associated with the exposure, here we used SNPs strongly predicting BP with external replication to minimise false positives. Second, the genetic variants are not associated with confounders of the exposure and outcome. Third, the genetic variants are associated with the outcome only through the exposure. Although we could not definitively test the second and third assumptions, we used MR-Egger and conducted a sensitivity analysis adjusting for major confounders of BP and CVD, we did not find strong evidence of directional pleiotropy. Multivariable MR additionally requires no perfect collinearity between the genetic associations with the exposures34. We included genetic variants independently predicting systolic and diastolic BP, with the conditional instrument strength well above the rule-of-thumb value, so the multivariable MR estimates are unlikely to be explained by multicollinearity17. Fourth, this was a two-sample MR study using summary statistics, meaning we could only assess linear relations of BP with CVD and lifespan, and our findings could not be used to inform the optimal BP levels given the long-debated J- (or U-) shaped relationship of BP with mortality and morbidity35. However, confounding by poor health may give rise to the J-curve36, which is increasingly refuted37, and could be further tested using individual-level data38. We also could not assess differences by sex, because relevant sex-specific summary statistics are not available. Fifth, the validity of MR maybe influenced by canalisation, where genetic variation can be eliminated by compensatory mechanisms during development39. However, canalisation biases the effect estimates towards the null10, which does not explain the positive associations here. Sixth, the UK Biobank was used for the exposures and some of the outcomes, which might result in bias in the direction of the observational association. However, we used strong genetic instruments for BP so bias due to weak instruments is unlikely40. The SNPs also had high I2 statistics, so bias due to confounding between exposure and outcome in overlapping samples is unlikely for the IVW and weighed median estimates, although some bias inflating the MR-Egger estimates is possible given a higher I2 is desired, so the MR-Egger estimates should be interpreted with caution41. Seventh, we constructed major CVD events by combining summary statistics of several potentially correlated outcomes, which could result in underestimation of the standard error, but at the same time takes into account the effect of a genetic variant on several phenotypes of interest. To correct for this possibility, we inflated the standard error42, we also investigated several common CVD subtypes as validation. Eighth, the BP GWAS adjusted for BMI to control for confounding, which could be a source of selection bias43, resulting in potential reversal of MR estimate direction due to unobserved common causes of BMI and exposure/outcome44, or common causes of survival and outcome45. However, adjusting for potential common causes, such as education, smoking and BMI, did not change the estimates. A previous MR using genetic predictors of BP without adjustment for BMI showed similar univariable MR estimates for BP on stroke19. Our sensitivity analysis provides similar reassurance. Ninth, the association for the direct effect of diastolic BP on coronary artery disease only reached the nominal but not Bonferroni-corrected significance threshold, suggesting insufficient strength of evidence. However, we found strong evidence of a direct effect of diastolic BP on lifespan, future studies using larger sample sizes for coronary artery disease should further elucidate this finding. Finally, although most of the outcome GWASs were conducted in European-descent individuals, the CARDIoGRAMplusC4D consortium consisted of participants from multiple ancestral groups, hence confounding by population structure is possible46. However, most of the participants were of European descent (77%), and some of the non-European studies adjusted for genetic principal components to correct for population structure47, we also included the UK Biobank estimates to increase the precision, the pooled estimate was 93% European so any bias due to population structure is likely to be minimal.
From a population health perspective, the findings in the present study suggest that within the usual population range, the “lower the better” concept for systolic BP is also relevant to diastolic BP48, and our study provides some genetic validation supporting the benefits of a lower diastolic BP threshold for hypertension49, which may perhaps motivate changes in other existing guidelines50. In conjunction with the 2017 ACC/AHA guidelines, the inclusion of more individuals for BP management and a lower BP target, regardless of systolic or diastolic BP, may produce enormous health benefits in the face of population ageing.
In conclusion, this present MR study showed higher systolic and diastolic BP to be independently associated with higher risk of coronary artery disease and shorter lifespan. Our findings provide supporting evidence of lower systolic and diastolic BP targets in the 2017 ACC/AHA guidelines.
Methods
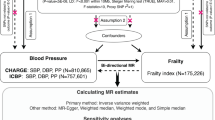
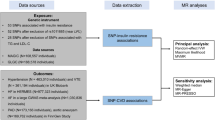
Genetic instruments for blood pressure
We obtained strong (P < 5 × 10–8), independent (r2 < 0.001) and externally replicated single nucleotide polymorphisms (SNPs) from the genome-wide association studies (GWAS) for BP traits by Evangelou et al.28 which provided summary statistics on ~ 757,601 individuals of European ancestry (grasp.nhlbi.nih.gov/FullResults.aspx), with a mean age of 56.0 years, of which 54.7% were women. The summary statistics were generated by fixed-effects inverse-variance weighted (IVW) meta-analysis of the International Consortium for Blood Pressure (ICBP) and the UK Biobank. Both the ICBP and the UK Biobank GWASs adjusted for age, age2, sex and body mass index (BMI), and included study-level genomic control accounting for population structure, as well as correction for observed BP based on hypertension medication status by adding 15 and 10 mmHg for systolic and diastolic BP, respectively. Palindromic SNPs with an effect allele frequency > 0.42 and < 0.58, which are difficult to align, were replaced with proxies (r2 ≥ 0.8 obtained from LDlink51) wherever available. The pooled mean (standard deviation (SD)) systolic and diastolic BP were 138.4 (20.1) and 82.8 (11.2) mmHg, respectively28.
Genetic associations with CVD and its subtypes
CVD was considered as major CVD events defined as a composite of coronary artery disease, stroke (intracranial haemorrhage and ischaemic stroke) and heart failure, similar to SPRINT22. Genetic associations with CVD (Table 1) were obtained from the UK Biobank (pan.ukbb.broadinstitute.org) participants of European ancestry on ~ 420,531 individuals52. To obtain the composite CVD outcome, we combined the summary statistics for each of the four CVD subtypes from the UK Biobank, which reflect their relative proportion in the population, using fixed-effects IVW meta-analysis. Given these subtypes are likely correlated, we applied genomic control by inflating the standard error using the square root of the linkage disequilibrium (LD) score regression intercept (1.337)53,54. LD score regression is a linear regression of SNP association chi-square statistic on SNP LD score, a departure from unity of the intercept indicates bias in the effect sizes due to population structure. We estimated the LD score regression intercept using LD Hub55.
We included major CVD subtypes from the largest and most recent publicly available genetic consortia for validation, including of coronary artery disease56, ischaemic stroke57, heart failure58 and atrial fibrillation59. Where these genetic consortia did not overlap with the UK Biobank, we included the MR estimates from the UK Biobank to improve the precision of our estimates. We did not present the MR estimates for intracranial haemorrhage because no large GWAS was available for meaningful interpretation60, nor has it accrued a substantial number of cases in the UK Biobank. We considered atrial fibrillation for CVD subtype validation because it was studied in a secondary analysis of the SPRINT results61.
Genetic associations with lifespan
We obtained genetic associations with combined parental attained age, as a proxy of longevity, from the UK Biobank participants of British ancestry62. We used parental longevity as a proxy of longevity because it enables use of a larger sample, and parental longevity is correlated with individual longevity phenotypically and genetically63,64. Participants provided the current age, or the age at death of their parents. The mean parental age at death (SD) was 78.6 (9.8) for mothers and 72.2 (11.1) for fathers, and 151.6 (15.0) years for both parents combined62. The attained age was standardised to the sex-specific mean value before being combined to account for the generally longer lifespan of women.
Statistical analysis
We assessed the strength of the genetic instruments using the F-statistic, approximated by the squared SNP-exposure association divided by the variance of this association. An F-statistic < 10 indicates a potentially weak instrument65. We conducted power calculations, based on the approximation that the sample size needed in an MR study is approximately the sample size for an conventional observational study divided by the proportion of variance in exposure explained by the genetic instrument66. SNPs instrumenting BP but unavailable for an outcome were replaced by proxies (r2 ≥ 0.8) wherever available. SNPs were aligned on the same effect allele for exposure and outcome. We used the MR Steiger test of directionality to assess whether the selected SNPs explained a larger proportion of the phenotypic variance of BP, than of the outcomes67.
To estimate the total effects of systolic and diastolic BP (per SD increment) we used univariable MR, specifically IVW with multiplicative random effects to combine the SNP-specific Wald estimates, obtained by dividing the SNP-outcome association by the SNP-exposure association. Given, the IVW estimates with multiplicative random effects assumes balanced pleiotropy68, we conducted sensitivity analyses using the weighted median, MR-Egger and MR pleiotropy residual sum and outlier (MR-PRESSO). The weighted median estimates are robust to directional genetic pleiotropy as long as more than 50% of the weight comes from valid SNPs69. The MR-Egger estimates are robust to directional genetic pleiotropy even if all SNPs are invalid instruments, provided the Instrument Strength Independent of Direct Effect (InSIDE) assumption is satisfied. A non-zero MR-Egger intercept indicates potential directional pleiotropy and possible bias in the IVW estimates70. We assessed the variability of instrument strength using the I2 statistic. An I2 < 90% suggests violation of the no measurement error (NOME) assumption and an invalid MR-Egger estimate65. An I2 ≥ 97% suggests bias due to overlapping samples for exposure and outcome is minimal41. MR-PRESSO statistically detects horizontal genetic pleiotropy and produces corrected estimates after removal of outliers71. We conducted a supplementary analysis using pulse pressure as the exposure given a widening pulse pressure reflects increasing difference between systolic and diastolic BP. We used Phenoscanner to identify which of the SNPs predicting BP was also strongly (P < 5 × 10–8) associated with education, smoking or BMI72, and we conducted a sensitivity analysis excluding such SNPs.
To estimate direct effect of systolic and diastolic BP we used multivariable MR of independent (r2 < 0.001) SNPs instrumenting systolic or diastolic BP obtained using the “clump_data” function of the “TwoSampleMR” R package, based on the European 1000 Genomes catalog, and the strength of their associations with systolic or diastolic BP, retaining the lower P-value when a SNP instrumented both BPs. We used multivariable IVW16, weighted median73, MR-Egger74 and MR-PRESSO71 to estimate the direct effect. We estimated the Sanderson–Windmeijer multivariate F-statistic to assess the conditional instrument strength, as well as the modified Q statistic as a measure of instrument pleiotropy17, taking into account the phenotypic correlation between systolic and diastolic BP (Pearson correlation 0.69 in the UK Biobank) to estimate the covariance of SNP-exposure associations25,75. To assess whether the multivariable MR results were robust to horizontal pleiotropy45, we included a sensitivity analysis which further adjusted for major confounders of BP and CVD, namely education (number of years)76, smoking (ever or never)42 and BMI77 by including their genetic associations in the multivariable IVW model. We included BMI in the multivariable MR model because genetic associations with the outcomes were independently estimated and did not account for the pleiotropic effects via BMI, despite the BP GWAS having already adjusted for BMI.
As the BP GWAS adjusted for BMI, potentially resulting in selection bias of the genetic associations with BP via common causes of BP and BMI26, we repeated the univariable and multivariable analyses using genetic associations with BP unadjusted for BMI extracted from the UK Biobank. We presented the estimates as per SD increment in the main text for direct comparison of systolic and diastolic BP, and, for interpretability, as per 10 (systolic BP) and 5 (diastolic BP) mmHg in the supplementary materials. With consideration of multiple testing and the similar aetiology of the CVDs included in the present study, a Bonferroni-corrected p-value of 0.0125 (0.05/2 BP traits*2 outcome groups) was considered strong evidence whereas a nominal p-value < 0.05 but > 0.0125 was considered suggestive evidence34, which adequately controls for multiple testing while avoiding false negatives. We used the R packages “TwoSampleMR” to obtain univariable MR estimates, the “MendelianRandomization” package to obtain multivariable MR estimates, and the “MVMR” package to obtain the Sanderson–Windmeijer multivariate F-statistic and the modified Q statistic. All statistical analyses were conducted using R (version 4.0.1, The R Foundation for Statistical Computing Platform, Vienna, Austria).
Ethics
This study only used publicly available data. No original data were collected. Ethical approval for each of the studies included in the investigation can be found in the original publications.
References
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913. https://doi.org/10.1016/s0140-6736(02)11911-8 (2002).
Gakidou, E. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422. https://doi.org/10.1016/S0140-6736(17)32366-8 (2017).
Collaboration, N. C. D. R. F. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 389, 37–55. https://doi.org/10.1016/S0140-6736(16)31919-5 (2017).
Kotchen, T. A. Developing hypertension guidelines: An evolving process. Am. J. Hypertens. 27, 765–772. https://doi.org/10.1093/ajh/hpt298 (2014).
James, P. A. et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA 311, 507–520. https://doi.org/10.1001/jama.2013.284427 (2014).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, e13–e115. https://doi.org/10.1161/HYP.0000000000000065 (2018).
McGrath, B. P. & McEvoy, J. W. Did the 2017 ACC/AHA blood pressure guideline get it wrong in reducing the diastolic threshold to define hypertension from 90 to 80 mmHg?. J. Clin. Hypertens. https://doi.org/10.1111/jch.13899 (2021).
Flint, A. C. et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N. Engl. J. Med. 381, 243–251. https://doi.org/10.1056/NEJMoa1803180 (2019).
McEvoy, J. W. et al. Association of isolated diastolic hypertension as defined by the 2017 ACC/AHA blood pressure guideline with incident cardiovascular outcomes. JAMA 323, 329–338. https://doi.org/10.1001/jama.2019.21402 (2020).
Davey Smith, G. & Ebrahim, S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease?. Int. J. Epidemiol. 32, 1–22. https://doi.org/10.1093/ije/dyg070 (2003).
Lawlor, D. A., Harbord, R. M., Sterne, J. A. C., Timpson, N. & Davey Smith, G. Mendelian randomization: Using genes as instruments for making causal inferences in epidemiology. Stat. Med. 27, 1133–1163. https://doi.org/10.1002/sim.3034 (2008).
Wan, E. Y. F. et al. Blood pressure and risk of cardiovascular disease in UK biobank: A mendelian randomization study. Hypertension 77, 367–375. https://doi.org/10.1161/hypertensionaha.120.16138 (2021).
Surendran, P. et al. Discovery of rare variants associated with blood pressure regulation through meta-analysis of 1.3 million individuals. Nat. Genet. 52, 1314–1332. https://doi.org/10.1038/s41588-020-00713-x (2020).
Sakaue, S. et al. Trans-biobank analysis with 676,000 individuals elucidates the association of polygenic risk scores of complex traits with human lifespan. Nat. Med. 26, 542–548. https://doi.org/10.1038/s41591-020-0785-8 (2020).
Stocks, T. et al. Blood pressure and risk of cancer incidence and mortality in the metabolic syndrome and cancer project. Hypertension 59, 802–810. https://doi.org/10.1161/hypertensionaha.111.189258 (2012).
Burgess, S. & Thompson, S. G. Multivariable mendelian randomization: The use of pleiotropic genetic variants to estimate causal effects. Am. J. Epidemiol. 181, 251–260. https://doi.org/10.1093/aje/kwu283 (2015).
Sanderson, E., Davey Smith, G., Windmeijer, F. & Bowden, J. An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int. J. Epidemiol. 48, 713–727. https://doi.org/10.1093/ije/dyy262 (2018).
Lieb, W. et al. Genetic predisposition to higher blood pressure increases coronary artery disease risk. Hypertension 61, 995–1001. https://doi.org/10.1161/HYPERTENSIONAHA.111.00275 (2013).
Georgakis, M. K. et al. Genetically determined blood pressure, antihypertensive drug classes, and risk of stroke subtypes. Neurology 95, e353–e361. https://doi.org/10.1212/wnl.0000000000009814 (2020).
Gill, D. et al. Genetically predicted midlife blood pressure and coronary artery disease risk: Mendelian randomization analysis. J. Am. Heart Assoc. 9, e016773. https://doi.org/10.1161/JAHA.120.016773 (2020).
Benavente, O. R. et al. Blood-pressure targets in patients with recent lacunar stroke: The SPS3 randomised trial. Lancet 382, 507–515. https://doi.org/10.1016/s0140-6736(13)60852-1 (2013).
Group et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116. https://doi.org/10.1056/NEJMoa1511939 (2015).
German, C. A. et al. Implications of the 2017 American College of Cardiology/American Heart association hypertension guideline in a modern primary prevention multi-ethnic prospective cohort (multi-ethnic study of atherosclerosis). Am. J. Cardiol. 123, 1076–1082. https://doi.org/10.1016/j.amjcard.2018.12.040 (2019).
McGrath, B. P. et al. Isolated diastolic hypertension in the UK biobank: Comparison of ACC/AHA and ESC/NICE guideline definitions. Hypertension https://doi.org/10.1161/HYPERTENSIONAHA.120.15286 (2020).
Sanderson, E., Spiller, W. & Bowden, J. Testing and correcting for weak and pleiotropic instruments in two-sample multivariable mendelian randomisation. BioRxiv https://doi.org/10.1101/2020.04.02.021980 (2020).
Hartwig, F. P., Tilling, K., Davey Smith, G., Lawlor, D. A. & Borges, M. C. Bias in two-sample Mendelian randomization when using heritable covariable-adjusted summary associations. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyaa266 (2021).
Gavish, B., Ben-Dov, I. Z. & Bursztyn, M. Linear relationship between systolic and diastolic blood pressure monitored over 24 h: Assessment and correlates. J. Hypertens. 26, 199–209. https://doi.org/10.1097/HJH.0b013e3282f25b5a (2008).
Evangelou, E. et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat. Genet. 50, 1412–1425. https://doi.org/10.1038/s41588-018-0205-x (2018).
Schooling, C. M. et al. Use of Multivariable Mendelian Randomization to Address Biases Due to Competing Risk Before Recruitment. 11. https://doi.org/10.3389/fgene.2020.610852 (2021).
Rutan, G. H. et al. Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the multiple risk factor intervention trial. Circulation 77, 504–514. https://doi.org/10.1161/01.cir.77.3.504 (1988).
Kuan, V. et al. A chronological map of 308 physical and mental health conditions from 4 million individuals in the English National Health Service. Lancet Digit. Health 1, e63–e77. https://doi.org/10.1016/S2589-7500(19)30012-3 (2019).
Lee, H. et al. Cardiovascular risk of isolated systolic or diastolic hypertension in young adults. Circulation 141, 1778–1786. https://doi.org/10.1161/circulationaha.119.044838 (2020).
Klarin, D. et al. Genetic architecture of abdominal aortic aneurysm in the million veteran program. Circulation https://doi.org/10.1161/circulationaha.120.047544 (2020).
Burgess, S. et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. https://doi.org/10.12688/wellcomeopenres.15555.2 (2019).
Cruickshank, J. M., Thorp, J. M. & Zacharias, F. J. Benefits and potential harm of lowering high blood pressure. Lancet 1, 581–584. https://doi.org/10.1016/s0140-6736(87)90231-5 (1987).
Masoli, J. A. H., Delgado, J., Pilling, L., Strain, D. & Melzer, D. Blood pressure in frail older adults: Associations with cardiovascular outcomes and all-cause mortality. Age Ageing https://doi.org/10.1093/ageing/afaa028 (2020).
Kjeldsen, S. E., Oparil, S., Narkiewicz, K. & Hedner, T. The J-curve phenomenon revisited again: SPRINT outcomes favor target systolic blood pressure below 120 mmHg. Blood Press 25, 1–3. https://doi.org/10.3109/08037051.2016.1096564 (2016).
Burgess, S., Davies, N. M. & Thompson, S. G. Instrumental variable analysis with a nonlinear exposure-outcome relationship. Epidemiology 25, 877–885. https://doi.org/10.1097/ede.0000000000000161 (2014).
Waddington, C. H. Canalization of development and the inheritance of acquired characters. Nature 150, 563–565. https://doi.org/10.1038/150563a0 (1942).
Burgess, S., Davies, N. M. & Thompson, S. G. Bias due to participant overlap in two-sample Mendelian randomization. Genet. Epidemiol. 40, 597–608. https://doi.org/10.1002/gepi.21998 (2016).
Minelli, C. et al. The use of two-sample methods for Mendelian randomization analyses on single large datasets. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyab084 (2021).
Karlsson Linnér, R. et al. Genome-wide association analyses of risk tolerance and risky behaviors in over 1 million individuals identify hundreds of loci and shared genetic influences. Nat. Genet. 51, 245–257. https://doi.org/10.1038/s41588-018-0309-3 (2019).
Aschard, H., Vilhjálmsson, B. J., Joshi, A. D., Price, A. L. & Kraft, P. Adjusting for heritable covariates can bias effect estimates in genome-wide association studies. Am. J. Hum. Genet. 96, 329–339. https://doi.org/10.1016/j.ajhg.2014.12.021 (2015).
Hartwig, F. P., Tilling, K., Davey Smith, G., Lawlor, D. A. & Borges, M. C. Bias in two-sample Mendelian randomization by using covariable-adjusted summary associations. BioRxiv https://doi.org/10.1101/816363 (2019).
Schooling, C. M. et al. Use of multivariable mendelian randomization to address biases due to competing risk before recruitment. F Gene https://doi.org/10.3389/fgene.2020.610852 (2021).
Wacholder, S., Rothman, N. & Caporaso, N. Population stratification in epidemiologic studies of common genetic variants and cancer: Quantification of bias. J. Natl. Cancer Inst. 92, 1151–1158. https://doi.org/10.1093/jnci/92.14.1151 (2000).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909. https://doi.org/10.1038/ng1847 (2006).
Bangalore, S. et al. Optimal systolic blood pressure target after SPRINT: Insights from a network meta-analysis of randomized trials. Am. J. Med. 130, 707-719.e708. https://doi.org/10.1016/j.amjmed.2017.01.004 (2017).
Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 30, 427–432. https://doi.org/10.1093/ije/30.3.427%JInternationalJournalofEpidemiology (2001).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 39, 3021–3104. https://doi.org/10.1093/eurheartj/ehy339%JEuropeanHeartJournal (2018).
Machiela, M. J. & Chanock, S. J. LDlink: A web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31, 3555–3557. https://doi.org/10.1093/bioinformatics/btv402 (2015).
Pan-UKB team. (2020).
Devlin, B. & Roeder, K. Genomic control for association studies. Biometrics 55, 997–1004. https://doi.org/10.1111/j.0006-341x.1999.00997.x (1999).
Bulik-Sullivan, B. K. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295. https://doi.org/10.1038/ng.3211 (2015).
Zheng, J. et al. LD Hub: A centralized database and web interface to perform LD score regression that maximizes the potential of summary level GWAS data for SNP heritability and genetic correlation analysis. Bioinformatics 33, 272–279. https://doi.org/10.1093/bioinformatics/btw613 (2017).
Nikpay, M. et al. A comprehensive 1,000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat. Genet. 47, 1121–1130. https://doi.org/10.1038/ng.3396 (2015).
Malik, R. et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 50, 524–537. https://doi.org/10.1038/s41588-018-0058-3 (2018).
Shah, S. et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat. Commun. 11, 163. https://doi.org/10.1038/s41467-019-13690-5 (2020).
Nielsen, J. B. et al. Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat Genet. 50, 1234–1239. https://doi.org/10.1038/s41588-018-0171-3 (2018).
Woo, D. et al. Meta-analysis of genome-wide association studies identifies 1q22 as a susceptibility locus for intracerebral hemorrhage. Am. J. Hum. Genet. 94, 511–521. https://doi.org/10.1016/j.ajhg.2014.02.012 (2014).
Soliman, E. Z. et al. Effect of intensive blood pressure lowering on the risk of atrial fibrillation. Hypertension 75, 1491–1496. https://doi.org/10.1161/HYPERTENSIONAHA.120.14766 (2020).
Pilling, L. C. et al. Human longevity: 25 genetic loci associated in 389,166 UK biobank participants. Aging (Albany NY) 9, 2504–2520. https://doi.org/10.18632/aging.101334 (2017).
Dutta, A. et al. Longer lived parents: Protective associations with cancer incidence and overall mortality. J. Gerontol. A Biol. Sci. Med. Sci. 68, 1409–1418. https://doi.org/10.1093/gerona/glt061 (2013).
Timmers, P., Wilson, J. F., Joshi, P. K. & Deelen, J. Multivariate genomic scan implicates novel loci and haem metabolism in human ageing. Nat. Commun. 11, 3570. https://doi.org/10.1038/s41467-020-17312-3 (2020).
Bowden, J. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: The role of the I2 statistic. Int. J. Epidemiol. 45, 1961–1974. https://doi.org/10.1093/ije/dyw220 (2016).
Freeman, G., Cowling, B. J. & Schooling, C. M. Power and sample size calculations for Mendelian randomization studies using one genetic instrument. Int. J. Epidemiol. 42, 1157–1163. https://doi.org/10.1093/ije/dyt110 (2013).
Hemani, G., Tilling, K. & Davey Smith, G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 13, e1007081. https://doi.org/10.1371/journal.pgen.1007081 (2017).
Bowden, J. et al. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat. Med. 36, 1783–1802. https://doi.org/10.1002/sim.7221 (2017).
Bowden, J., Davey Smith, G., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40, 304–314. https://doi.org/10.1002/gepi.21965 (2016).
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525. https://doi.org/10.1093/ije/dyv080 (2015).
Verbanck, M., Chen, C. Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50, 693–698. https://doi.org/10.1038/s41588-018-0099-7 (2018).
Staley, J. R. et al. PhenoScanner: A database of human genotype-phenotype associations. Bioinformatics 32, 3207–3209. https://doi.org/10.1093/bioinformatics/btw373 (2016).
Grant, A. J. & Burgess, S. J. a. p. a. Pleiotropy robust methods for multivariable Mendelian randomization. (2020).
Rees, J. M. B., Wood, A. M. & Burgess, S. Extending the MR-Egger method for multivariable Mendelian randomization to correct for both measured and unmeasured pleiotropy. Stat. Med. 36, 4705–4718. https://doi.org/10.1002/sim.7492 (2017).
Zheng, J. et al. PhenoSpD: An integrated toolkit for phenotypic correlation estimation and multiple testing correction using GWAS summary statistics. Gigascience https://doi.org/10.1093/gigascience/giy090 (2018).
Okbay, A. et al. Genome-wide association study identifies 74 loci associated with educational attainment. Nature 533, 539–542. https://doi.org/10.1038/nature17671 (2016).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in ∼700000 individuals of European ancestry. Hum. Mol. Genet. 27, 3641–3649. https://doi.org/10.1093/hmg/ddy271 (2018).
Acknowledgements
We thank the participants and investigators for providing the publicly available summary statistics. Data on blood pressure have been downloaded from the National Heart, Lung, and Blood Institute (grasp.nhlbi.nih.gov/FullResults.aspx). Data on coronary artery disease have been contributed by CARDIoGRAMplusC4D investigators and have been downloaded from www.CARDIOGRAMPLUSC4D.ORG. The MEGASTROKE project received funding from sources specified at http://www.megastroke.org/acknowledgments.html. The list of MEGASTROKE authors is available from https://www.megastroke.org/authors.html. Data on heart failure have been downloaded from Cardiovascular Disease Knowledge Portal (www.broadcvdi.org/). Data on atrial fibrillation have been downloaded from The University of Michigan Center for Statistical Genetics (csg.sph.umich.edu/willer/public/afib2018). Data on parental lifespan have been downloaded from GWAS Catalog (www.ebi.ac.uk/gwas/). Data on the relevant CVD phenotypes in the UK Biobank have been downloaded from the Pan UKBB Team (pan.ukbb.broadinstitute.org). Data on education and smoking initiation have been downloaded from the Social Science Genetic Association Consortium (www.thessgac.org/data). Data on BMI have been downloaded from the Broad Institute (portals.broadinstitute.org/collaboration/giant/index.php/GIANT_consortium_data_files).
Author information
Authors and Affiliations
Contributions
I.I.C., M.K.K. and C.M.S. designed the study and interpreted the results. I.I.C. conducted data analysis and wrote the first draft of the manuscript, with critical feedback from M.K.K. and C.M.S. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chan, I.I., Kwok, M.K. & Schooling, C.M. The total and direct effects of systolic and diastolic blood pressure on cardiovascular disease and longevity using Mendelian randomisation. Sci Rep 11, 21799 (2021). https://doi.org/10.1038/s41598-021-00895-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00895-2
This article is cited by
-
Insights into Causal Cardiovascular Risk Factors from Mendelian Randomization
Current Cardiology Reports (2023)
-
The Interplay between Systolic Blood Pressure, Sauna Bathing, and Cardiovascular Mortality in Middle-Aged and Older Finnish Men: A Cohort Study
The Journal of nutrition, health and aging (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.