Abstract
Hematuria, either glomerular or extraglomerular, is defined as 3 or more red blood cells (RBCs)/high power field. Currently, urinalyses are commonly performed using automated urine sediment analyzers. To assess whether RBC counting by automated urine sediment analyzers is reliable for defining hematuria in glomerular disease, random specimen urinalyses of men with nephritic glomerular disease (7674 urinalyses) and bladder cancer (12,510 urinalyses) were retrospectively reviewed. Urine RBCs were counted by an automated urine sediment analyzer based on flow cytometry (UF-1000i, Sysmex Corporation) or digital image analysis (Cobas 6500, Roche Diagnostics GmbH). In about 20% of urine specimens, the specific gravity was less than 1.010, making the RBC counts unreliable. In the urine specimens with specific gravity ≥ 1.010, RBC counts measured using either UF-1000i or Cobas 6500 were well correlated with the positive grades in the dipstick blood test. However, at a trace, 1+, or higher positive dipstick tests for blood, RBC counts were graded significantly lower in glomerular disease than in bladder cancer. The findings suggest that RBC counting by UF-1000i or Cobas 6500 underestimates the severity of hematuria in glomerular disease, possibly because dysmorphic RBCs in glomerular disease are susceptible to hemolysis and/or fail to be properly recognized.
Similar content being viewed by others
Introduction
Hematuria can occur in glomerular diseases as well as extraglomerular diseases, including urologic malignancies. It is detected in the urinalysis by either a dipstick test or microscopic examination of urine sediment. The urinary dipstick test detects the peroxidase-like activity of heme in red blood cells (RBCs) and is very sensitive for hematuria, but may not be specific1,2. Thus, hematuria is defined by the number of RBCs in the urine sediment, i.e., 3 or more RBCs/high power field (HPF)3,4.
In the past, RBCs in the urine were counted by manual microscopic examination, but it is time-consuming and labor-intensive. For rapid and efficient urinalysis, automated urine sediment analyzers were introduced more than 20 years ago and have taken over this task in clinical laboratories5,6.
The current automated urine sediment analyzers identify RBCs by flow cytometry (for example, UF-1000i urine analyzer, Sysmex Corporation, Kobe, Japan) or analysis of digitalized images of the urine sediment (for example, Cobas 6500 urine analyzer, Roche Diagnostics GmbH, Mannheim, Germany)7,8. The analyzers have good performance for the identification of isomorphic RBCs as in extraglomerular hematuria9.
In glomerular disease, the presence of hematuria is a key factor in differentiating nephritic disease from nephrotic disease. Recently, more attention has been paid to hematuria in glomerular disease because hematuria was shown to have a negative prognostic impact10.
Glomerular hematuria is different from extraglomerular hematuria in terms of the RBC morphology. RBCs from extraglomerular hematuria have an isomorphic appearance as seen in peripheral blood smears, whereas RBCs of glomerular origin are small and have a dysmorphic appearance with marked variability in size and shape11. The morphologic alterations of RBCs occur due to mechanical trauma taking place while they pass through the glomerular basement membrane or the osmotic stress due to high or low osmolarity within the renal tubules12.
Glomerular hematuria is also defined as the presence of ≥ 3 or 5 RBCs/HPF13,14,15,16,17,18,19,20,21. To assess whether RBC counting by automated urine sediment analyzers is reliable for defining hematuria in glomerular disease, this study compared urine RBC counts of patients with nephritic glomerular disease and those with bladder cancer at each positive grade in a dipstick blood test in the urinalyses performed using two automated urine sediment analyzers (UF-1000i urine analyzer and Cobas 6500 urine analyzer).
Methods
Patients
This study included adult patients (≥ 18 years) who were diagnosed with nephritic glomerular disease via a kidney biopsy and diagnosed with bladder cancer via a bladder biopsy or transurethral resection of bladder tumor at Asan Medical Center (Seoul, Korea), a tertiary hospital; the patients’ medical records were retrospectively reviewed. Between January 2011 and November 10, 2016, urine sediment examinations were carried out using the UF-1000i urine analyzer (Sysmex Corporation). Thereafter, the instrument for urinalysis was changed to the Cobas 6500 urine analyzer (Roche Diagnostics GmbH). For the analysis of the UF-1000i urine analyzer data, the urinalyses of the patients with glomerular disease performed between January 2011 and October 2016 and the urinalyses of the patients with bladder cancer performed between January 2013 and December 2015 were collected. For the analysis of the Cobas 6500 urine analyzer data, the urinalyses of the patients with glomerular disease performed between December 2016 and December 2020 and the urinalyses of the patients with bladder cancer performed between January 2017 and December 2019 were collected.
For the patients with glomerular disease, some urinalyses were conducted the day after the kidney biopsy, which may have caused extraglomerular hematuria. Thus, only urinalyses from outpatients, and not inpatients, were included. In young women with glomerular disease, extraglomerular hematuria derived from menstrual blood may contaminate the glomerular hematuria; thus, only men were included. For the same reason, patients with both bladder cancer and glomerular disease were also excluded. In the case of patients with bladder cancer who had undergone radical cystectomy with formation of an ileal conduit or neobladder during the study period, only those urinalysis data obtained prior to the cystectomy were included. Finally, the urinalyses of gross hematuria, identified via the red, reddish, or orange hue of the urine, were excluded.
This study was approved by the Institutional Review Board (IRB) of Asan Medical Center (IRB No. S2021-0242-0001); the requirement of obtaining informed consent was waived owing to the retrospective study design. All methods were performed in accordance with the Declaration of Helsinki.
Laboratory parameters
Urine specimens were randomly obtained at the outpatient clinic and transported to the clinical laboratory without preservatives. The laboratory aimed to report the urinalysis results within 1 h of sampling.
Urinary RBCs counted via either the UF-1000i urine analyzer or the Cobas 6500 urine analyzer were reported as follows: grade 1 (0–2 RBCs/HPF), grade 2 (3–5 RBCs/HPF), grade 3 (6–10 RBCs/HPF), grade 4 (11–20 RBCs/HPF), grade 5 (21–30 RBCs/HPF), grade 6 (31–100 RBCs/HPF) and grade 7 (> 100 RBCs/HPF).
The presence of blood and the pH of the urine were measured via a dipstick test. The urine color and the dipstick test results were read via an automatic reader. The Urisys 2400 automated urine test strip analyzer (Roche Diagnostics GmbH) was used to read the dipstick tests of the urine specimens examined using the UF-1000i urine analyzer, whereas the Cobas 6500 urine analyzer was used to conduct the urine dipstick test as well as the urine RBC counting using two modules, the Cobas u 601 for the urine dipstick and the Cobas u 701 for urine microscopy. Test strips in the Urisys 2400 cassettes and the cobas u packs were used with the Urisys 2400 analyzer and the Cobas u 601 analyzer, respectively. In both analyzers, dipstick hematuria was graded as −, ±, 1+, 2+, 3+, and 4+. The pH of the urine was categorized as follows; 5, 6, 6.5, 7, 8 and 9.
The Urisys 2400 and Cobas u 601 urine analyzers both contain a built-in refractometer, and the specific gravity (SG) was measured via refractometry. The scale of urine SG ranged from 1.000 to 1.050. In dilute urine, the RBCs absorb water, swell, and may rupture. In concentrated urine, the RBCs tend to shrink and become crenated. A urine SG of 1.010 corresponds to approximately 300 mOsm/kg, similar to the osmolarity of plasma22, and a urine SG > 1.020 often indicates dehydration23. In this study, therefore, urine samples with SG < 1.010 and > 1.020 were considered dilute and concentrated urine, respectively.
Statistical analysis
The data are expressed as the median (interquartile range). The values obtained for the two groups were compared using the Mann–Whitney U test. To measure the strength of association between the positive degree on the dipstick blood test and the urine RBC count, Spearman’s rank-order correlation was used. The prevalence of categorical variables was compared between the two groups using the chi-squared test or Fisher’s exact test. Statistical analyses were performed using SPSS version 21 (IBM Co., Armonk, NY, USA). p values less than 0.05 were considered statistically significant.
Results
Patient characteristics
In the data obtained via the UF-1000i urine analyzer, 330 patients were diagnosed with nephritic glomerular disease (235, IgA nephropathy; 39, pauci-immune crescentic glomerulonephritis; 35, lupus nephritis; 13, membranoproliferative glomerulonephritis; 6, Henoch-Schönlein purpura; and 2, postinfectious glomerulonephritis). The median age at diagnosis was 47 (28–58) years. The control group consisted of 967 patients who were diagnosed with bladder cancer (958, transitional cell carcinoma; 4, bladder invasion of prostate carcinoma; 3, urachal carcinoma; 1, spindle cell neoplasm; and 1, metastatic sigmoid colon carcinoma). The median age at diagnosis was 67 (59–74) years (p < 0.001 compared with glomerular disease). The number of urinalyses was 9 (3–17) among the patients with glomerular disease and 5 (3–7) among the patients with bladder cancer.
In the data obtained via the Cobas 6500 urine analyzer, 385 patients were diagnosed with glomerular disease (266, IgA nephropathy; 57, pauci-immune crescentic glomerulonephritis; 36, lupus nephritis; 13, Henoch-Schönlein purpura; 11, membranoproliferative glomerulonephritis; and 2, postinfectious glomerulonephritis). The median age at diagnosis was 46 (30–58) years. The control group consisted of 1087 patients who were diagnosed with bladder cancer (1064, transitional cell carcinoma; 7, urachal carcinoma; 7, neuroendocrine small cell carcinoma; 6, bladder invasion of prostate carcinoma; 1, mucinous adenocarcinoma; 1, pleomorphic undifferentiated sarcoma; and 1, invasive poorly differentiated carcinoma). The median age at diagnosis was 69 (60–75) years (p < 0.001 compared with glomerular disease). The number of urinalyses was 9 (4–13) among the patients with glomerular disease and 6 (4–9) among the patients with bladder cancer.
Distributions of urine SG and pH
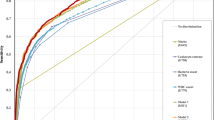
The SG of urine affects the morphology of RBCs and may thus alter the identification of RBCs via automated urine sediment analyzers. The distribution of the urine SG in each group is shown in Fig. 1.
In the data obtained via the UF-1000i urine analyzer, the SG of urine from patients with bladder cancer and glomerular disease was 1.015 (1.010–1.020) and 1.014 (1.010–1.019) (p < 0.001), respectively. The frequency of a dilute urine specimen with SG < 1.010 was 21.8% (1148/5271) among patients with bladder cancer and 22.3% (866/3892) among patients with glomerular disease. In contrast, the frequency of a concentrated urine specimen with SG > 1.020 was 21.7% (1142/5271) among patients with bladder cancer and 18.9% (737/3892) among patients with glomerular disease (p < 0.001).
In the data obtained via the Cobas 6500 urine analyzer, the SG of urine from patients with bladder cancer and glomerular disease was 1.016 (1.011–1.020) and 1.015 (1.011–1.020) (p < 0.001), respectively. The frequency of a dilute urine specimen with SG < 1.010 was 18.1% (1310/7239) among patients with bladder cancer and 18.4% (696/3782) among patients with glomerular disease. In contrast, the frequency of a concentrated urine specimen with SG > 1.020 was 24.9% (1806/7239) among patients with bladder cancer and 21.6% (816/3782) among patients with glomerular disease (p < 0.001).
To examine the effects of high and low urine SG values on RBC counting via automated urine sediment analyzers, the RBC counts at each positive grade in the dipstick blood test were compared according to the SG. In most cases, the RBC counts were graded significantly lower in urine specimens with SG < 1.010 than in those with SG 1.010–1.020. High urine SG (> 1.020) did not seem to alter the RBC counting via the UF-1000i urine analyzer, but tended to decrease the RBC counts in patients with glomerular disease when the urinalyses were performed using the Cobas 6500 urine analyzer (Supplementary Tables S1–S4, Supplementary Figs. S1–S4).
Urine pH is another factor that affects the morphology of RBCs. In highly alkaline urine (pH > 9), RBCs may undergo lysis due to swelling of the outer membrane layers24. In the data obtained via the UF-1000i urine analyzer, the pH of urine from bladder cancer and glomerular disease was 6 (5–6.5) and 5 (5–6.5) (p < 0.001), respectively. There were 7/5271 (0.13%) urine specimens with pH ≥ 9 among the patients with bladder cancer and 2/3892 (0.05%) among the patients with glomerular disease. In the data obtained via the Cobas 6500 urine analyzer, the pH of urine from bladder cancer and glomerular disease was 6 (5–7) and 5 (5–6) (p < 0.001), respectively. There were 16/7239 (0.22%) urine specimens with pH ≥ 9 among the patients with bladder cancer and 6/3782 (0.16%) among the patients with glomerular disease.
Correlation between the urinary dipstick blood test and urinary RBC counts
The relation between positive grades in the dipstick test and urinary RBC counts was assessed in urine samples with SG ≥ 1.010 and pH < 9.0.
In the data obtained via the UF-1000i urine analyzer, the Spearman’s correlation coefficient for the correlation between the positive grades in the dipstick test and urine RBC counts was 0.900 (n = 4117, p < 0.001) in bladder cancer and 0.829 (n = 3024, p < 0.001) in glomerular disease, respectively.
In the data obtained via the Cobas 6500 urine analyzer, the Spearman’s correlation coefficient for the correlation between the positive grades in the dipstick test and urine RBC counts was 0.911 (n = 5914, p < 0.001) in bladder cancer and 0.834 (n = 3081, p < 0.001) in glomerular disease, respectively.
RBC counts at each positive degree of the dipstick blood test
The RBC counts at each positive grade of the dipstick blood test were compared between glomerular disease and bladder cancer in urine samples with SG ≥ 1.010 and pH < 9.0.
In both bladder cancer and glomerular disease, the RBC counts were widely distributed at each degree of positivity in the dipstick test, suggesting that some RBCs undergo lysis before urinalysis or are not recognized (Tables 1, 2).
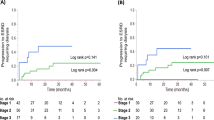
However, at a trace, 1+, or higher positive dipstick tests for blood, RBC counts were graded significantly lower in glomerular disease than in bladder cancer. In the data obtained via the UF-1000i urine analyzer, the grades of RBC counts/positivity in the dipstick test were 1 (1–1)/−, 1 (1–2)/±, 2 (1–2)/1+, 3 (2–4)/2+, 5 (3–6)/3+, and 7 (6–7)/4+ in bladder cancer, and 1 (1–1)/−, 1 (1–1)/±, 1 (1–2)/1+, 2 (1–3)/2+, 3 (2–4)/3+, and 5 (4–6)/4+ in glomerular disease, with the magnitude of difference bigger as the positive grade increased (Fig. 2).
Comparison of hematuria grades measured using the UF-1000i urine analyzer between bladder cancer and glomerular disease at each positive dipstick grade. Vertical boxes, error bars, and dots represent the median with interquartile range, minimum and maximum values, and outliers, respectively (***p < 0.001).
The difference was greater in the data obtained via the Cobas 6500 urine analyzer at 1+ or higher positive dipstick tests for blood; 1 (1–1)/−, 2 (1–3)/±, 3 (3–4)/1+, 4 (2–4)/2+, 5 (4–6)/3+, and 7 (6–7)/4+ in bladder cancer, and 1 (1–1)/−, 1 (1–1)/±, 1 (1–2)/1+, 1 (1–2)/2+, 3 (1–4)/3+, and 5 (4–6)/4+ in glomerular disease (Fig. 3).
Comparison of hematuria grades measured using the Cobas 6500 urine analyzer between bladder cancer and glomerular disease at each positive dipstick grade. Vertical boxes, error bars, and dots represent the median with interquartile range, minimum and maximum values, and outliers, respectively (***p < 0.001).
A dipstick positive result, but a negative microscopic result (RBC 0–2/HPF) was also more frequent in glomerular disease than in bladder cancer: 13.5% in bladder cancer and 26.7% in glomerular disease in the data obtained via the UF-1000i urine analyzer (p < 0.001), and 3.7% in bladder cancer and 18.9% in glomerular disease in the data obtained via the Cobas 6500 urine analyzer (p < 0.001).
Among the urine samples with a negative result in the dipstick test, the frequency of 3 or more RBCs/HPF was similar between bladder cancer (1.4%) and glomerular disease (1.8%) in the data obtained via the UF-1000i urine analyzer, but it was higher in bladder cancer (8.7%, p < 0.001) than in glomerular disease (1.9%) in the data obtained via the Cobas 6500 urine analyzer.
Discussion
The urine dipstick test is very sensitive for the detection of hematuria (sensitivity 91–100%), but it may not be specific (specificity 65–99%) because it also yields positive results for hemoglobinuria or myoglobinuria25. In the present study, the participating subjects showed no clinical evidence of intravascular hemolysis or rhabdomyolysis, and a positive urine dipstick blood test was strongly indicative of hematuria considering that bladder cancer and glomerular disease had been pathologically proven. For both bladder cancer and glomerular disease, the grades of hematuria measured using the dipstick were well correlated with urine RBC counts measured via the automated urine sediment analyzers. In dilute or highly alkaline urine, RBCs may undergo lysis. Even after dilute or alkaline urine specimens were excluded, however, there were urinalyses with a positive dipstick test for blood but negative or relatively few RBCs, suggesting that some RBCs are degraded before urinalysis or are not detected. Such urinalyses were more frequent in cases of glomerular disease than in cases of bladder cancer, and at a trace, 1+, or higher positive dipstick tests for blood, the RBC counts were significantly lower in glomerular disease than in bladder cancer.
In glomerular hematuria, RBCs pass through the glomerular filtration barrier and the convoluted tubules, which may distort the RBC morphology. RBCs may undergo lysis during this passage, or the morphologically altered RBCs can be more vulnerable to hemolysis26. If RBCs are degraded, they are not detected by microscopic examination, but the hemoglobin released from the RBCs is still detected by the dipstick test27. Besides, automated urine sediment analyzers detect isomorphic RBCs well but may not be good at detecting dysmorphic RBCs8,28,29.
The UF-1000i urine analyzer counts RBCs by flow cytometry, whereas the Cobas 6500 urine analyzer identifies RBCs by the analysis of digital images of the urine sediment. Though the two urine sediment analyzers counted fewer RBCs in patients with glomerular disease than in patients with bladder cancer for each positive dipstick blood test, the differences in RBC numbers between patients with bladder cancer and patients with glomerular disease were greater with the Cobas 6500 urine analyzer than with the UF-1000i urine analyzer. This may be in part because the Cobas 6500 urine analyzer tended to count fewer RBCs in the concentrated urine of patients with glomerular disease. The Cobas 6500 urine analyzer may also give some false positive results for RBCs in patients with bladder cancer because 3 or more RBCs/HPF despite a negative result in the dipstick test was more frequent in patients with bladder cancer than in those with glomerular disease.
In urologic malignancies, hematuria is intermittent, and the level of microscopic hematuria does not indicate the seriousness of the disease30, and it is important to determine the presence or absence of hematuria. If adults older than 40 years test positive for hematuria, a urologic investigation is required to exclude malignancy. Because the dipstick test detects heme from hemoglobinuria, myoglobinuria, and glomerular hematuria as well as extraglomerular hematuria, there is a high probability of the result being a false positive for the diagnosis of urologic malignancy. Thus, hematuria is defined as ≥ 3 RBCs/HPF and this is the widely accepted definition across urologic societies3,4; furthermore, the dipstick hematuria test is not considered sufficient to mandate an evaluation.
In glomerular disease, however, the amount of hematuria may be more important than the presence or absence of hematuria because high-grade hematuria suggests a nephritic glomerular disease in the differential diagnosis and may also indicate a worse renal prognosis.
In a recent study31, urine dipstick hematuria was shown to be useful in differentiating proliferative glomerulonephritis from other causes of kidney diseases, with higher positive grades in the dipstick blood test associated with higher positive predictive values.
The association of hematuria with adverse renal outcomes has also been reported in glomerular diseases. IgA nephropathy is one of the representative glomerular diseases presenting with hematuria. The persistence of hematuria in IgA nephropathy was related to a greater probability of developing end-stage kidney disease (ESKD)14,17. Similarly, hematuria in chronic kidney disease was associated with a faster decline in kidney function or an increased risk of developing ESKD15,16. In diabetic nephropathy, hematuria is usually absent, but its presence was associated with an increased risk of ESKD18,21. High-grade hematuria in glomerular disease indicates severe inflammation of glomeruli, and hematuria itself also may increase the injury to the kidney parenchyma by releasing the toxic molecules such as free hemoglobin and heme if RBCs are ruptured while passing through glomeruli and tubules26.
In the above studies, hematuria was defined by the RBC numbers. In a few studies where RBC counts were not available, the dipstick test was used to define hematuria. Dipstick hematuria was also shown to be a risk factor for deterioration of glomerular filtration in chronic kidney disease32,33 and diabetic nephropathy34; however, the grading of hematuria severity was not included in the analysis.
Considering the significance of hematuria in glomerular disease, the severity of hematuria needs to be assessed accurately. However, the current study suggests that automated urine sediment analyzers do not reliably detect RBCs of glomerular origin, and the defining hematuria based on RBC numbers may result in hematuria not being detected or in the severity of hematuria being underestimated in glomerular disease.
Besides the urinalysis method being used, the collection of an adequate urine specimen is a prerequisite for accurate urine sediment examination. To avoid collecting dilute urine, it is recommended that urinalysis be performed using the first-morning specimen. However, randomly voided urine is the most commonly used specimen for urinalysis because it is easiest to obtain, as it was in this study. With the randomly voided urine, 18–22% of the urine specimens had SG < 1.010, which made the assessment of hematuria by RBC counting unreliable due to hypotonic lysis of RBCs.
Even in urine specimens with SG ≥ 1.010, the RBC counts can be affected by the level of urine concentration, with a higher number of RBCs in more concentrated urine. However, the RBC counts are reported without a correction for the degree of urine concentration, and thus do not allow quantitative assessment of hematuria. The same is true for the dipstick blood test.
As compared with urine RBC counting, the urine dipstick blood test may have more advantages for the follow-up of hematuria in cases of glomerular disease, as the results can be positive due to dysmorphic RBCs as well as isomorphic RBCs; further, hematuria can be detected in dilute urine specimens by the presence of heme released from lysed RBCs27.
This study has some limitations. First, automated urinary sediment examination was not compared with the manual microscopic examination, which is recommended in the evaluation of urine sediments in patients with glomerular disease. The latter, however, should be performed by experts under standard conditions and is not feasible where a large number of samples need to be processed quickly. Furthermore, RBC counting under the manual microscopic examination is also not accurate and is subject to wide interobserver variability35. Second, the dipstick blood test may also give false positives and false negatives. Bacterial peroxidase, for example, can produce false-positive results36. However, bacterial peroxidase does not seem to account for the lower numbers of urinary RBCs in glomerular disease because urinary tract infection was not documented in the patients with glomerular disease during the study period. In contrast, ascorbic acid or ascorbic acid-containing soft drinks may cause false-negative results37; however, the patients included in this study were not questioned about this before obtaining urinalysis specimens.
In conclusion, our data suggest that urine RBC counting by the UF-1000i urine analyzer or the Cobas 6500 urine analyzer underestimates the severity of hematuria in glomerular disease, possibly because dysmorphic RBCs are susceptible to hemolysis and/or are not properly recognized.
References
Roberts, J. R. Urine dipstick testing: Everything you need to know. Emerg. Med. News 29, 24–27 (2007).
Willis, G. C. & Tewelde, S. Z. The approach to the patient with hematuria. Emerg. Med. Clin. N. Am. 37, 755–769 (2019).
Davis, R. et al. American Urological Association. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults: AUA guideline. J. Urol. 188(6 Suppl), 2473–2481 (2012).
Wollin, T., Laroche, B. & Psooy, K. Canadian guidelines for the management of asymptomatic microscopic hematuria in adults. Can. Urol. Assoc. J. 3, 77–80 (2009).
Chien, T. I. et al. Urine sediment examination: A comparison of automated urinalysis systems and manual microscopy. Clin. Chim. Acta 384, 28–34 (2007).
Cavanaugh, C. & Perazella, M. A. Urine sediment examination in the diagnosis and management of kidney disease: Core curriculum 2019. Am. J. Kidney Dis. 73, 258–272 (2019).
Becker, G. J., Garigali, G. & Fogazzi, G. B. Advances in urine microscopy. Am. J. Kidney Dis. 67, 954–964 (2016).
Oyaert, M. & Delanghe, J. Progress in automated urinalysis. Ann. Lab. Med. 39, 15–22 (2019).
Lee, W., Ha, J. S. & Ryoo, N. H. Comparison of the automated cobas u 701 urine microscopy and UF-1000i flow cytometry systems and manual microscopy in the examination of urine sediments. J. Clin. Lab. Anal. 30, 663–671 (2016).
Moreno, J. A. et al. Glomerular hematuria: Cause or consequence of renal inflammation? Int. J. Mol. Sci. 20, 2205 (2019).
Kincaid-Smith, P. & Fairley, K. The investigation of hematuria. Semin. Nephrol. 25, 127–135 (2005).
Schramek, P., Moritsch, A., Haschkowitz, H., Binder, B. R. & Maier, M. In vitro generation of dysmorphic erythrocytes. Kidney Int. 36, 72–77 (1989).
Kido, R. et al. Persistent glomerular hematuria in living kidney donors confers a risk of progressive kidney disease in donors after heminephrectomy. Am. J. Transplant. 10, 1597–1604 (2010).
Goto, M. et al. A scoring system to predict renal outcome in IgA nephropathy: A nationwide 10-year prospective cohort study. Nephrol. Dial. Transplant. 24, 3068–3074 (2009).
You-Hsien Lin, H. et al. Microscopic haematuria and clinical outcomes in patients with stage 3–5 nondiabetic chronic kidney disease. Sci. Rep. 5, 15242 (2015).
Yuste, C. et al. Haematuria increases progression of advanced proteinuric kidney disease. PLoS ONE 10, e0128575 (2015).
Sevillano, A. M. et al. Remission of hematuria improves renal survival in IgA nephropathy. J. Am. Soc. Nephrol. 28, 3089–3099 (2017).
Lin, H. Y. et al. Hematuria and renal outcomes in patients with diabetic chronic kidney disease. Am. J. Med. Sci. 356, 268–276 (2018).
Rhee, R. L. et al. The utility of urinalysis in determining the risk of renal relapse in ANCA-associated vasculitis. Clin. J. Am. Soc. Nephrol. 13, 251–257 (2018).
Yu, G. Z. et al. Persistent hematuria and kidney disease progression in IgA nephropathy: A cohort study. Am. J. Kidney Dis. 76, 90–99 (2020).
Wu, Y. et al. The association of hematuria on kidney clinicopathologic features and renal outcome in patients with diabetic nephropathy: A biopsy-based study. J. Endocrinol. Investig. 43, 1213–1220 (2020).
Imran, S., Eva, G., Christopher, S., Flynn, E. & Henner, D. Is specific gravity a good estimate of urine osmolality? J. Clin. Lab. Anal. 24, 426–430 (2010).
Sawka, M. N. et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 39, 377–390 (2007).
Sharp, V. J., Barnes, K. T. & Erickson, B. A. Assessment of asymptomatic microscopic hematuria in adults. Am. Fam. Phys. 88, 747–754 (2013).
Grossfeld, G. D. et al. Evaluation of asymptomatic microscopic hematuria in adults: The American Urological Association best practice policy—Part I: Definition, detection, prevalence, and etiology. Urology 57, 599–603 (2001).
Yuste, C. et al. Pathogenesis of glomerular haematuria. World J. Nephrol. 4, 185–195 (2015).
Bataille, A. et al. Evidence of dipstick superiority over urine microscopy analysis for detection of hematuria. BMC Res. Notes 9, 435 (2016).
Shayanfar, N., Tobler, U., von Eckardstein, A. & Bestmann, L. Automated urinalysis: First experiences and a comparison between the Iris iQ200 urine microscopy system, the Sysmex UF-100 flow cytometer and manual microscopic particle counting. Clin. Chem. Lab. Med. 45, 1251–1256 (2007).
Cobbaert, C. M. et al. Automated urinalysis combining physicochemical analysis, on-board centrifugation, and digital imaging in one system: A multicenter performance evaluation of the cobas 6500 urine work area. Pract. Lab. Med. 17, e00139 (2019).
Thaller, T. R. & Wang, L. P. Evaluation of asymptomatic microscopic hematuria in adults. Am. Fam. Phys. 60, 1143–1152 (1999).
Palsson, R., Srivastava, A. & Waikar, S. S. Performance of the automated urinalysis in diagnosis of proliferative glomerulonephritis. Kidney Int. Rep. 4, 723–727 (2019).
Orlandi, P. F. et al. Hematuria as a risk factor for progression of chronic kidney disease and death: Findings from the chronic renal insufficiency cohort (CRIC) study. BMC Nephrol. 19, 150 (2018).
Schulman, G. et al. Risk factors for progression of chronic kidney disease in the EPPIC trials and the effect of AST-120. Clin. Exp. Nephrol. 22, 299–308 (2018).
Mashitani, T. et al. Association between dipstick hematuria and decline in estimated glomerular filtration rate among Japanese patients with type 2 diabetes: A prospective cohort study (diabetes distress and care registry at Tenri (DDCRT 14)). J. Diabetes Complicat. 31, 1079–1084 (2017).
Cho, E. J. et al. The efficient workflow to decrease the manual microscopic examination of urine sediment using on-screen review of images. Clin. Biochem. 56, 70–74 (2018).
Lam, M. H. False ‘hematuria’ due to bacteriuria. Arch. Pathol. Lab. Med. 119, 717–721 (1995).
Matsuo, C. et al. Influence of commercial soft drinks or green tea intake to occult blood and sugar tests with urinalysis reagent strips. Rinsho Byori 57, 834–841 (2009).
Author information
Authors and Affiliations
Contributions
W.S.Y. collected and analyzed the data, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, W.S. Automated urine sediment analyzers underestimate the severity of hematuria in glomerular diseases. Sci Rep 11, 20981 (2021). https://doi.org/10.1038/s41598-021-00457-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00457-6
This article is cited by
-
The application of new complex indicators in the detection of urine
BMC Nephrology (2023)
-
Leukocyturia and hematuria enable non-invasive differentiation of Bowman’s capsule rupture severity in PR3-ANCA glomerulonephritis
Journal of Nephrology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.