Abstract
The anterior talofibular ligament and the calcaneofibular ligament are the most commonly injured ankle ligaments. This study aimed to investigate if the double fascicular anterior talofibular ligament and the calcaneofibular ligament are associated with the presence of interconnections between those two ligaments and connections with non-ligamentous structures. A retrospective re-evaluation of 198 magnetic resonance imaging examinations of the ankle joint was conducted. The correlation between the double fascicular anterior talofibular ligament and calcaneofibular ligament and connections with the superior peroneal retinaculum, the peroneal tendon sheath, the tibiofibular ligaments, and the inferior extensor retinaculum was studied. The relationships between the anterior talofibular ligament’s and the calcaneofibular ligament’s diameters with the presence of connections were investigated. Most of the connections were visible in a group of double fascicular ligaments. Most often, one was between the anterior talofibular ligament and calcaneofibular ligament (74.7%). Statistically significant differences between groups of single and double fascicular ligaments were visible in groups of connections between the anterior talofibular ligament and the peroneal tendon sheath (p < 0.001) as well as the calcaneofibular ligament and the posterior tibiofibular ligament (p < 0.05), superior peroneal retinaculum (p < 0.001), and peroneal tendon sheath (p < 0.001). Differences between the thickness of the anterior talofibular ligament and the calcaneofibular ligament (p < 0.001), the diameter of the fibular insertion of the anterior talofibular ligament (p < 0.001), the diameter of calcaneal attachment of the calcaneofibular ligament (p < 0.05), and tibiocalcaneal angle (p < 0.01) were statistically significant. The presence of the double fascicular anterior talofibular ligament and the calcaneofibular ligament fascicles correlate with connections to adjacent structures.
Similar content being viewed by others
Introduction
The ATFL is the weakest part of the lateral ankle ligaments, which is usually the first and most common injured ligament in ankle inversions. The anterior talofibular ligament (ATFL) is composed of the superior (S-ATFL) and inferior fascicle (I-ATFL)1,2,3,4,5,6,7. Meanwhile, the calcaneofibular ligament (CFL) is composed of the medial (M-CFL) and lateral (L-CFL)6,8,9. The interconnections between the ATFL, CFL, and the posteriori talofibular ligament (PTFL) provide integration between components making a complex of ligaments to a functional unit1,10. The most prominent interconnection is I-ATFL and the CFL, which is usually arch-formed11. The S-ATFL is considered as an intraarticular structure, while the I-ATFL is an extraarticular part. It is unclear if the S-ATFL is intrasynovial or only intracapsular. If the only S-ATFL is injured, healing potential is lower because of its intraarticular localization, and if the I-ATFL is preserved, a secondary microinstability may appear12. However, during injury propagating via the I-ATFL, forces may also be transmitted to the CFL, causing its injury, and the full instability may appear13.
The diagnostic imaging of the posttraumatic ankle is based mainly on the clinical examination and x-ray. However, MRI is often performed to accurately assess all injuries to bones and soft tissue14. MRI criteria of injury to a ligament also include an assessment of dimensions; however, the cut-off values are not fully established. There is a significant discrepancy in the length, thickness, and width of the normal ATFL (Table 1) and CFL (Table 2). Most of the previously published anatomical research based on dissections focuses on surgically useful measurements as length and width. However, studies on thickness measurement are found less frequently. The mean thickness of the ATFL measured on MRI was 2.19 ± 0.6 mm, and the corresponding value for the CFL was 2.13 ± 0.5 mm15. According to an MRI study, the length of the ATFL was 2.19 mm, and the respective value for CFL was 2.13 mm16. The definition of the normal diameters is essential in the assessment of the ATFL and CFL after trauma and in chronic instability17.
There are also biomechanical differences between fascicles of the ATFL; the S-ATFL is taut in plantarflexion while the I-ATFL in dorsiflexion. Taking into consideration the biomechanical features of the ATFL, a possible two fascicle reconstruction may restore both the structure and function of the ligament. It should be added that such reconstruction is not performed nowadays18. The lateral ligament complex may include an occurring variable, the lateral talocalcaneal ligament, which may support the CFL. Malalignment of the ankle or subtalar joint may cause overuse of the supporting ligaments. Hindfoot valgus may influence the CFL19, which via existing interconnections, may cause dysfunction of the whole lateral ligament complex. Clinical observation indicates that the ATFL and CFL accompany the pathology of adjacent non-ligamentous structures as the superior peroneal retinaculum or the peroneal tendons. Morphological studies of anatomical connections may help in improving diagnostic imaging and surgery of the injured ligaments and non-ligamentous structures by understanding the mechanism of injury and by selecting the best method of reconstruction20. The hypothesis of our study is that there are interconnections between the lateral ligaments and non-ligamentous structures in the area of the lateral malleolus. The aim of the study was to assess the presence of communications between the ATFL and CFL with adjacent structures and correlate it with the ATFL and CFL’s morphology.
Material and methods
The MRI examinations were done from January 2017 to April 2019, and no traumatic indications were reviewed. Exclusion criteria were trauma in the anamnesis, obvious abnormality in the lateral region of the ankle, the presence of the orthopedic hardware due to the possible artifacts (23 cases excluded), a history of previous fracture (19 cases excluded), and obvious abnormality in relation to the lateral malleolus (8 cases excluded). In total, 198 MRI examinations of the ankle fulfilled the inclusion and exclusion criteria. All examinations were reviewed twice, and the final results were made by consensus.
The MRI protocol may vary between cases, but inclusion criteria were the presence at least proton density (PD) or T2-weighted sequences without fat saturation in sagittal, axial, and coronal plane to assess ligaments structure. The other sequences, like T1-weighted turbo spin-echo (T1-TSE), PD with fat suppression, or short-T1 inversion recovery (STIR), were used to detect pathology, which might be the exclusion criterion. All MRI examinations were performed using the MRI machine Ingenia 3.0 T MR system (Philips Healthcare) with a dedicated ankle coil.
Our study included 110 females and 80 males with an age range of 18–58 years, and a mean age of 31 years. The right ankle was examined in 107 cases, and the left one in 91.
The statistical correlations between of presence of connection to adjacent structures, the morphometry, side, gender, and presence of the interconnections between the ATFL and CFL in the groups of single and double fascicular ATFL and CFL were analyzed. The other lateral structures included in our study were the PTFL, the superior peroneal retinaculum (SPR), the peroneal tendon sheath (PTS), the fibulotalocalcaneal ligament (FTCL), the anterior inferior tibio-fibular ligament (AITFL), and the inferior extensor retinaculum (IER). The measurement of the tibiocalcaneal angle (TCA), according to Buck et al.24 was performed and correlated with CFL morphology and morphometry.
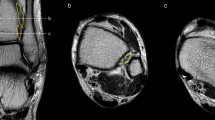
The protocol and some of the measurements are presented in Fig. 1. The length and thickness of the midportion of the ATFL was measured on the axial sequence (Fig. 1a). The length of the fibular insertion of the ATFL was evaluated on the sagittal sequence (Fig. 1b), while the coronal sequence was used to assess the biggest diameter of the talar insertion (Fig. 1c). The length, the width, and the diameter of the fibular insertion of the CFL were assessed on the consecutive sagittal slides (Fig. 1d). The coronal sequences were used to measure the length of the calcaneal insertion (Fig. 1e), while the thickness of the midportion was measured on the axial sequence in the middle part of the ligament (Fig. 1f). In the two-fascicular ligaments, the width was measured for both bundles together, and the ratio size between the fascicles was noted. The CFL angle and the TCA were measured as in a previous study24.
The Local Swedish Ethics Committee and Institutional Ethics Committee at the Medical University of Warsaw approved the study and waived the need for informed consent (Numbers 06177 and AKBE/258/2019) due to the retrospective and non-invasive nature of the study. The study was conducted in accordance with the Declaration of Helsinki. The anonymization of patient data in the research process ensured data protection in accordance with the European General Data Protection Regulation. The authors declare that this work has not received any funding before or during research. There are no relationships with any companies whose products or services may be related to the subject matter of the article.
Results
Our MRI study revealed the presence of interconnections between the ATFL and CFL and with other lateral ankle structures included in the study (Figs. 2 and 3). We noticed several statistically significant differences in the incidence of these connections and diameters between the groups of single and double fascicular ATFL and CFL (Tables 3 and 4). There were no significant differences regarding gender and side (p > 0.05).
A 33-yeard-old patient with suspicion of an osteochondral lesion of the talus, which was not confirmed on the MRI. The communications present in relation to the lateral malleolus. The CFL (straight arrow), the ATFL (dashed arrow), the SPR (curved arrow), the IER (curved dashed arrow), and the PTFL (*). On figure (b, c, f, g and h) two fascicles of the CFL are visible: L- the L-CFL and M- the M-CFL. Levels of cross-sections are labeled on figures (e) and (f).
The connection between the ATFL and CFL
The connection of the ATFL with the CFL was the most common one and was found in 148 cases (74.7%), Figs. 2, 3, 4, 5. The majority of the interconnections between the ATFL and CFL were observed in the groups of double fascicular ATFL (125 cases, 63.1%) and the double fascicular CFL (105 cases, 53%; Table 3). However, those differences were not statistically significant (Table 1). These interconnections were seen in the proximity to the fibular insertion of the ATFL and the CFL. This structure is often arciform and connecting the I-ATFL and the L-CFL (Figs. 2 and 3g).
A 45-yeard-old patient with suspicion of a soft tissue tumor, which was not confirmed on the MRI. The double fascicular ATFL, two fascicles with the same diameter. Sagittal section (a,b) and transverse section (c). The S-ATFL (straight arrow), the I-ATFL (curved arrow), the PTFL (dashed arrow), and the CFL (curved dashed arrow). Levels of cross-sections are labeled on figures (b,c).
A 20-yeard-old patient with suspicion of ganglion originating from the talonavicular joint, which was not confirmed on the MRI. The presence of the os subfibulare does not change the anatomical relations of the ligaments. ATFL (curved arrow) and CFL (straight arrow). The M-CFL (M) runs anterior to communicate with the ATFL, while the L-CFL (L) attaches to the fibula.
The connections of the ATFL and CFL with other structures
The most connections with non-ligamentous structures were seen in groups of double fascicular ligaments (Figs. 4, 5, 6). In the group of the ATFL, the other most common connections were noticed with the SPR (26.8%), IER (24.2%), and PTS (14.6%), Table 3. Among the ATFL’s connections, only the connection with the PTS differed significantly between the single and double fascicular ligament (Table 3).
A 34-yeard-old patient with suspicion of the soft tissue tumor, which was not confirmed on the MRI. The double fascicular ATFL, two asymmetrical fascicles. Sagittal section (a,b) and transverse section (c). The S-ATFL (straight arrow), the I-ATFL (curved arrow), the PTFL (dashed arrow), and the CFL (curved dashed arrow). Levels of cross-sections are labeled on figures b and c.
In the group of the CFL, the other most common connections were with the PTFL (68.7%), the SPR (67.2%), and the FTCL (64.1%), Figs. 7 and 8. Among the CFL’s connections, only the connections with the PTFL, SPR, and PTS differed significantly between the single and double fascicular ligament (Table 3). We did not identify connections of the CFL with the AITFL and IER.
A 43-yeard-old patient with suspicion of a tumor. The MRI did not reveal a tumor in the soft tissue. The oblique sections (a–d) and the axial cross-section (e). Levels of cross-sections are labeled on figures (d,e). Connections of the CFL (curved arrow) with the FTCL (straight arrow), the PTS (dashed arrow), the superior peroneal retinaculum (dashed curved arrow), the PTFL (*), and the ATFL (**).
A 19-yeard-old patient with suspicion of the rheumatoid arthritis. No changes which correspond to this were found. The MRI did not reveal a tumor in the soft tissue. The communication between the CFL and the SPR. The axial section (a) and the corona section (b). Levels of cross-sections are labeled on both figures with lines and letters a and b. Connections of the CFL (curved arrow) with the superior peroneal retinaculum (dashed curved arrow), the peroneus brevis (*), and the peroneus longus (**).
The incidence of occurrence double fascicular ATFL and CFL
The presence of the double fascicular ATFL was identified in 148 cases (74.7%), of which in 101 cases (76.3%), two fascicles were completely separated while in 47 cases (23.7%) were incompletely separated. The single fascicular ATFL was identified in 50 cases (25.3%). The double fascicular CFL was recognized in 131 cases (66.2%), whereas a single fascicular CFL was seen in 67 cases (33.8%). In 84 cases (42.4%), the LTCL was present and branched from the CFL in 69 cases (34.8%), while in 15 cases (7.6%), it originated from the calcaneus as a separate structure.
The possibility to distinguish the medial (M-CFL) and the lateral (L-CFL) CFL fascicle was from the midportion and proximal to that. The L-CFL was always thicker than the M-CFL and had insertion on the inferoanterior outline of the apex of the lateral malleolus. We identified two variations of attachment of the M-CFL. The most often, one was seen on the fibula medial of the L-CFL in 84 cases (64.1%). The other one was found on the talus in 47 cases (23.7%) of which united with LTCL before it reaches the talus in 28 cases (14.1%) or ran directly to the talus in 19 cases (9.6%) (Fig. 9).
A 41-yeard-old patient with suspicion of a stress fracture of the distal tibia. No fractures were revealed on the MRI. The variably occurring accessory fascicle of the CFL inserts on the talus (curved dashed arrow). The CFL (straight arrow) in the distal part is not divided, and the proximal part (P) attaches to the lateral malleolus. The PTS (dashed arrow) and the PTFL (*).
We revealed a statistically significant negative correlation between the CFL angle and TCA r(198) = − 0.25, p < 0.001. The differences in TCA were statistically significant, Table 5. In 52 cases (26.3%), the CFL angle was lower than 119 grades, which is the recommended cut-off for hindfoot19.
The differences in diameters between groups of single and double fascicular ATFL and CFL.
The average length of the ATFL was 24.2 ± 3.4 mm, the thickness in the midportion was 2.1 ± 0.3 mm, while the corresponding values for the CFL were 32.6 ± 4 mm and 2 ± 0.2 mm (Tables 4 and 5). Statistically significant differences between the single and double fascicular ATFL and CFL were noticed in thickness (Table 4). The superior fascicle of the ATFL (S-ATFL) was bigger in 122 cases (82.4%) than the I-ATFL, while in 26 cases (17.6%), the S-ATFL and the I-ATFL were at the same diameter. We did not notice any case where the I-ATFL was bigger.
The average breadth of the midportion of the ATLF was 5.1 ± 0.7 mm, and the corresponding value for the CFL was 6.5 ± 1.4 mm; however, without statistically significant differences (Tables 4 and 5). The average CFL angle was 117.2 ± 11.4 grades, while the TCA was 11.0 ± 4.4 grades, which was statistically significant (Table 5).
Bony attachments of the two fascicules of the ATFL, the talus and the fibula, were the same. The average craniocaudal length of the fibular insertions of the ATFL was 5.8 ± 0.9 mm, and the CFL was 5.2 ± 1 mm (Tables 4 and 5). However, statistically significant differences were noticed only between groups of the ATFL (Table 4). The average craniocaudal diameters of the talar insertion of the ATFL was 4.3 ± 0.6 mm, and the respective diameter of the calcaneal insertion of the CFL was 7.4 ± 1.4 mm, which was statistically significant (Tables 4 and 5).
Discussion
The first contribution of the present study is that the connections with the non-ligamentous structures occur more often in groups of double fascicular ATFL or CFL. The second is that there are differences in diameter between single and double fascicular ligaments.
The nomenclature of the internal structure of a ligament is not clear and somewhat ambiguous. After other authors1,10,25, we implemented the term fascicule; however, there are no papers systematizing the nomenclature similar to the nomenclature of tendons26.
The occurrence of interconnections between the ATFL, CFL, and PTFL causes the formation of an anatomical and functional lateral fibulotalocalcaneal ligament complex11. It is located in the space between the medial side of the distal part of the lateral malleolus and the lateral outline of the talus10,11. Moreover, the footprint of the CFL and the ATFL is more confluent on the anterior border of the lateral malleolus18, also integrating bony attachments. The arciform fibers between the I-ATFL and the CFL1 may play a mechanical role in stabilizing the ankle when tension shifts between these two ligaments. After the S-ATFL is torn, the tearing continues via the arciform connection to the CFL, and the patient may develop ankle instability11. The extensive surgical dissection inferior to the lateral malleolus may cause injury to the arciform communication if it is preserved during trauma. Therefore, that should be considered during the surgery.
The connections between the ligament complex and adjacent non-ligamentous structures were revealed in our study, but to our knowledge, not studied previously in-depth. Furthermore, we revealed a significant correlation between the double fascicular structure of the ATLF and CFL with a higher occurrence of connections between the ATFL and CFL with non-ligamentous structures. The higher occurrence of communication in a group of double fascicular ligaments1 may, therefore, be due to development27. Moreover, anatomical studies show a relationship between the shape of the medial articular surface of the lateral malleolus and the connection between ATFL and PTFL, which may also indicate a developmental context.
Previously proven connections between the lateral ligament complex of the ankle with ligaments in the Kager’s fat pat may indicate the existence of some functional ligamentous-fascial units28 where the ligament complex is one part of the entirety. The presence of interconnections between the lateral ankle ligaments explain the concomitant nature of lateral ankle ligament injuries, making them like the deltoid ligament or spring ligament complex; despite having parts, it is challenging to separate them from each other10,29.
The AITFL connects with the ATFL stabilizing the position of the talus. The continuity of communication between the ATFL and AITFL preserves the anterior protrusion of the talus, which may cause friction with the inferior fascicle of the AITFL in patients with posttraumatic anterolateral hyperlaxity of the injured ATFL25. We noticed approximately a ten times lower occurrence of connections of the AITFL with ATFL when compared to the previous study, which was conducted on cadavers25. The wide differences between the anatomical studies based on dissections and research based on MRI30 were also noticed before in other ankle ligaments, which may be related to the method.
The presence of the connections of the CFL and the ATFL with the SPR and PTS may explain the posttraumatic instability of the peroneal tendons. It may be important for developing surgical techniques. Failure to recognize SPR injury may cause instability of the peroneal tendons and result in its rupture31. The existence of interconnections that lead to dysfunction of one structure may affect the function of the other. This clinical observation also confirms the significance of the described connections and their relationship with the double fascicular ATFL or CFL.
The fascicular feature of the ATFL was shown in anatomical studies1,11 and one anatomical-radiological study by Delfaut et al.32. Despite the amount of research, significant discrepancies in the frequency of the double fascicular ATFL from 25%18 to 100%9 are noticed. It is difficult to clearly define where such large discrepancies in the literature come from. It may be because some of these studies were done on small materials (Tables 1 and 2). In our study, the incidence of a single ATFL fascicle was comparable to most anatomical studies on larger material1,3,8,33. MRI is an appropriate method to detect abnormality and the presence of the fascicular structure of the ATFL32. We did not identify the tri- or multifascicular ligaments9,20,33. The third fascicle, if it is present, is the smallest of the ATFL fascicles and was reported in no more than 2%-12%, while some studies do not confirm its presence at all3,22. We believe that the absence of this rare variation in our result may be due to the MRI protocol or was a consequence of overdissection, which can be noticed when some of the anatomical studies are reviewed. The high occurrence of the double-fascicular structure of ATFL and CFL, together with the variability of connections, requires an update of the anatomical classification like it was done in other structures in the locomotor system34.
The presence of connections revealed in our study is also important for radiologists during the assessment of an ankle using an MRI after injury and for orthopedists in planning the reconstruction of ruptured ligaments35. The double fascicular structure of ATFL can be a diagnostic pitfall in MRI because the thin layers of connective tissue separating the bundles of the ligament have a slightly higher signal, imitating ligament abnormality32. Therefore, awareness of its occurrence is important for radiologists. The magic-angle effect may increase the intraligamentous signal, which may be seen on short echo time (TE) MRI sequences when a collagen structure is oriented at 55 grades to the main magnetic field36. Our study revealed the fascicular structure of the ATFL also on long-TE MRI sequences, which negates the presence of this artifact. No absence of the ATFL was detected, which was reported previously in 5%3,22.
The LTCL is a variable structure located in direct relation to the CFL. Most of the cases found in our study branched directly from the CFL, while in others, authors reported that it was never found as a separate structure11. The close relation to the CFL indicates that the LTCL, if present, is part of the lateral ankle ligament complex.
A ligament's fascicular structure allows different fiber orientations, functional differentiation, and better alignment of a joint. Due to interconnections, single smaller ligaments connect to form the larger anatomical-functional units resembling, for example, a cuff rotator in the shoulder. Functionally, this possibly results in better biomechanical joint stabilization1. We believe that the presence of the connections described by us is also crucial in training and preventing sports injuries. Strengthening one structure by the presence of connections may improve the function of others. However, further research is needed to confirm our hypothesis. We believe that our results provide sufficient anatomical background for further functional studies.
Differences between the diameters of the ligaments between the single and double fascicular were noticed. To our knowledge, there is no anatomic or radiologic paper about the correlation of the length, the width, and the thickness of the ATFL and the CFL with its fascicular nature. The length of the ATFL reported previously seemed to be circa 10 mm shorter when compared to studies on smaller materials2,3,6,9,20, whereas when compared to other authors who used larger material, our results were similar1,22 (Tables 1 and 2). Differences are probably related to the number of cases and methods of measurement with or without bony attachments9,37. It was reported that the wider and longer ligament’s fascicles are more prone to the pathological process than thinner ones38. Therefore, the diameters may have a clinical significance.
The thickness of the CFL shown in our study was consistent with what was previously reported16,17. The ATFL, in clubfeet, was reported to be much wider than in the two normal feet, which indicates a developmental background12,27. The width of the midportion assessed in our study is slightly smaller than reported previously9,22,33.
The thickness of the ligaments is one of the most important measurements for the radiologists because the ligamentous thickening and thinning is an MRI criteria for tears32. We reveled that ligaments’ dimensions are related to their fascicular structure. We used 3 T MRI because it allows for good resolution and excellent tissue differentiation39. To our knowledge, there is no cut-off value of the normal variants of the ATFL. The average thickness of the midportion of the ATFL revealed by us corresponds to the values reported before22,40,41 thus, we recommend using 2 mm as a cut-off value of the normal ligament. It is difficult to find studies on all dimensions of the ATFL and CFL on the same material, which makes comparison difficult (Tables 1 and 2).
To our knowledge, there have been no previous large-scale MRI studies regarding measurements of bony insertions. MRI examinations were performed for clinical purposes, so the assessment of the two dimensions of the insertion was somewhat difficult. Therefore, we included the largest diameter of the attachment-based on the known shape of the attachment9,18,21,42. Most of the previous studies provide the value of the area of insertion, which makes it harder to compare. However, some reference can be made. There is a discrepancy in the size ratio of the attachments reported in the literature. Some authors report that size of the talar insertion of the ATFL is bigger than the fibular one9, while the other reported exactly the opposite18. It is difficult to solve this problem based on our measurements. However, the craniocaudal diameter revealed in our study was larger in the fibula, where the attachment is more elongated, while the talar attachment is more oval1,3,18.
An unrecognized hindfoot valgus may cause a chronic deformity and secondary osteoarthritis. Initially, the patient experiences only the pain associated with overuse, and an MRI is often performed. Early identification of a valgus malalignment on an MRI may be crucial for the patient’s outcome. The CFL angle and the tension of the CFL change during movements and deformation. The cut-off value for the suspicion for a valgus hindfoot, ≤ 119 grades19, may be used with great sensitivity and specificity. The increased TCA is associated with a reduced CFL angle and may indicate a hindfoot19. Taking into consideration the presence of the connections between ligaments and non-ligamentous structures, fluctuations in tension in CFL translates to other structures causing changes in their function.
We acknowledge several limitations in our present study. Only one dimension of the bony attachments was measured. We believe that the full assessment of the bony attachments area and more accurate measurements may be possible when a special protocol with ultra-thin layers or with 3D sequences can be used. However, we believe that the MRI assessment of the fibular attachment may be difficult due to the multiple connections described1,3,18. The measurement errors may be related to the cutting angle and the measurement point of the single slice image. The retrospective character may also be a limitation of the study.
The presence of the double fascicular structure of the ATFL and CFL is related, more often, with the occurrence of interconnections between these two ligaments as well as with the adjacent structures.
Abbreviations
- AITFL:
-
The anterior inferior tibio-fibular ligament
- ATFL:
-
The anterior talofibular ligament
- CFL:
-
The calcaneofibular ligament
- FTCL:
-
The fibulotalocalcaneal ligament
- I-ATFL:
-
The interior fascicle of the ATFL
- IER:
-
The inferior extensor retinaculum
- L-CFL:
-
The lateral fascicle of the CFL
- LTCL:
-
The lateral talocalcaneal ligament
- M-CFL:
-
The medial fascicle of the CFL
- PTFL:
-
The posteriori talofibular ligament
- PTS:
-
The peroneal tendon sheath
- S-ATFL:
-
Superior fascicle of the ATFL
- SD:
-
Standard deviation
- SPR:
-
The superior peroneal retinaculum
- TCA:
-
The tibiocalcaneal angle
- TE:
-
Echo time
References
Edama, M. et al. Morphological features of the anterior talofibular ligament by the number of fiber bundles. Ann. Anat. 216, 69–74 (2018).
Milner, C. E. & Soames, R. W. Anatomical variations of the anterior talofibular ligament of the human ankle joint. J. Anat. 191(Pt 3), 457–458 (1997).
Raheem, O. A. & O’Brien, M. Anatomical review of the lateral collateral ligaments of the ankle: a cadaveric study. Anat. Sci. Int. 86, 189–193 (2011).
Siegler, S., Block, J. & Schneck, C. D. The mechanical characteristics of the collateral ligaments of the human ankle joint. Foot Ankle 8, 234–242 (1988).
Uğurlu, M. et al. Anatomy of the lateral complex of the ankle joint in relation to peroneal tendons, distal fibula and talus: a cadaveric study. Joint Dis. Related Surg. 21(3), 153–158 (2010).
Yildiz, S. & Yalcin, B. The anterior talofibular and calcaneofibular ligaments: an anatomic study. Surg. Radiol. Anat. 35, 511–516 (2013).
Yıldız, S. & Yalcın, B. The anterior talofibular and calcaneofibular ligaments: an anatomic study. Surg. Radiol. Anat. 35, 511–516 (2013).
Kobayashi, T. et al. Morphological characteristics of the lateral ankle ligament complex. Surg. Radiol. Anat. 42, 1153–1159 (2020).
Wenny, R., Duscher, D., Meytap, E., Weninger, P. & Hirtler, L. Dimensions and attachments of the ankle ligaments: evaluation for ligament reconstruction. Anat. Sci. Int. 90, 161–171 (2015).
Dalmau-Pastor, M., Malagelada, F., Calder, J., Manzanares, M. C. & Vega, J. The lateral ankle ligaments are interconnected: the medial connecting fibres between the anterior talofibular, calcaneofibular and posterior talofibular ligaments. Knee Surg. Sports Traumatol. Arthrosc. 28, 34–39 (2020).
Vega, J., Malagelada, F., Céspedes, M. C. & Dalmau-Pastor, M. The lateral fibulotalocalcaneal ligament complex: an ankle stabilizing isometric structure. Knee Surg Sports Traumatol. Arthrosc. 28, 8–17 (2020).
Windisch, G., Anderhuber, F., Haldi-Brandle, V. & Exner, G. U. Anatomical study for an updated comprehension of clubfoot. Part II: Ligaments, tendons and muscles. J Child Orthop 1, 79–85 (2007).
Golano, P. et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg. Sports Traumatol. Arthrosc. 24, 944–956 (2016).
Szaro, P., Geijer, M. & Solidakis, N. Traumatic and non-traumatic bone marrow edema in ankle MRI: a pictorial essay. Insights Imaging 11, 97 (2020).
Dimmick, S., Kennedy, D. & Daunt, N. Evaluation of thickness and appearance of anterior talofibular and calcaneofibular ligaments in normal versus abnormal ankles with MRI. J. Med. Imag. Radiat. Oncol. 52(6), 559–563 (2008).
Ahmad, M. A., Pandey, U. C., Crerand, J. J., Al-Shareef, Z. & Lapinsuo, M. Magnetic resonance imaging of the normal and injured lateral collateral ligaments of the ankle. Ann. Chir. Gynaecol. 87(4), 311–6 (1998).
Dimmick, S., Kennedy, D. & Daunt, N. Evaluation of thickness and appearance of anterior talofibular and calcaneofibular ligaments in normal versus abnormal ankles with MRI. J. Med. Imaging Radiat. Oncol. 52, 559–563 (2008).
Neuschwander, T. B., Indresano, A. A., Hughes, T. H. & Smith, B. W. Footprint of the lateral ligament complex of the ankle. Foot. Ankle Int. 34, 582–586 (2013).
Lee, S., Oliveira, I., Pressney, I., Welck, M. & Saifuddin, A. The horizontal calcaneofibular ligament: a sign of hindfoot valgus on ankle MRI. Skeletal. Radiol. 49, 739–746 (2020).
Khawaji, B. & Soames, R. The anterior talofibular ligament: A detailed morphological study. Foot (Edinb) 25, 141–147 (2015).
Clanton, T. O. et al. Qualitative and quantitative anatomic investigation of the lateral ankle ligaments for surgical reconstruction procedures. J. Bone Joint Surg. Am. 96, e98 (2014).
Taser, F., Shafiq, Q. & Ebraheim, N. A. Anatomy of lateral ankle ligaments and their relationship to bony landmarks. Surg. Radiol. Anat. 28, 391–397 (2006).
Sindel, M., Demir, S., Yildirim, A. & Ucar, Y. Anatomy of the lateral ankle ligaments. Turk. J. Med. Sci. 28(1), 53–6 (1998).
Buck, F. M. et al. Diagnostic performance of MRI measurements to assess hindfoot malalignment: an assessment of four measurement techniques. Eur. Radiol. 23, 2594–2601 (2013).
Edama, M. et al. Morphological features of the inferior fascicle of the anterior inferior tibiofibular ligament. Sci. Rep. 9, 10472 (2019).
Handsfield, G. G., Slane, L. C. & Screen, H. R. C. Nomenclature of the tendon hierarchy: An overview of inconsistent terminology and a proposed size-based naming scheme with terminology for multi-muscle tendons. J. Biomech. 49, 3122–3124 (2016).
Uchiyama, E. et al. Fetal development of ligaments around the tarsal bones with special reference to contribution of muscles. Clin. Anat. 27, 389–398 (2014).
Szaro, P., Polaczek, M. & Ciszek, B. The Kager’s fat pad radiological anatomy revised. Surg Radiol Anat https://doi.org/10.1007/s00276-020-02552-1 (2020).
Hintermann, B. & Golanó, P. The anatomy and function of the deltoid ligament. Tech. Foot Ankle Surg. 13, 67–72 (2014).
Subhas, N. et al. MRI appearance of surgically proven abnormal accessory anterior-inferior tibiofibular ligament (Bassett’s ligament). Skeletal. Radiol. 37, 27–33 (2008).
Rosenberg, Z. S. et al. MRI features of chronic injuries of the superior peroneal retinaculum. AJR Am. J. Roentgenol. 181, 1551–1557 (2003).
Delfaut, E. M. et al. Multi-fasciculated anterior talo-fibular ligament: reassessment of normal findings. Eur. Radiol. 13, 1836–1842 (2003).
Milner, C. E. & Soames, R. W. Anatomy of the collateral ligaments of the human ankle joint. Foot Ankle Int. 19, 757–760 (1998).
Olewnik, L. et al. Proposal for a new classification of plantaris muscle origin and its potential effect on the knee joint. Ann. Anat. 231, 151506 (2020).
Roemer, F. W. et al. Ligamentous injuries and the risk of associated tissue damage in acute ankle sprains in athletes: a cross-sectional MRI study. Am. J. Sports Med. 42, 1549–1557 (2014).
Richardson, M. L., Amini, B. & Richards, T. L. Some new angles on the magic angle: what MSK radiologists know and don’t know about this phenomenon. Skeletal. Radiol. 47, 1673–1681 (2018).
Kristen, K. H., Seilern Und Aspang, J., Wiedemann, J., Hartenbach, F. & Platzgummer, H. Reliability of ultrasonography measurement of the anterior talofibular ligament (ATFL) length in healthy subjects (in vivo), based on examiner experience and patient positioning. J. Exp. Orthop. 6, 30 (2019).
Akseki, D., Pinar, H., Yaldiz, K., Akseki, N. G. & Arman, C. The anterior inferior tibiofibular ligament and talar impingement: a cadaveric study. Knee Surg. Sports Traumatol. Arthrosc. 10, 321–326 (2002).
Couppe, C. et al. Accuracy of MRI technique in measuring tendon cross-sectional area. Clin. Physiol. Funct. Imaging 34, 237–241 (2014).
Kanamoto, T., Shiozaki, Y., Tanaka, Y., Yonetani, Y. & Horibe, S. The use of MRI in pre-operative evaluation of anterior talofibular ligament in chronic ankle instability. Bone Joint Res. 3, 241–245 (2014).
Burks, R. T. & Morgan, J. Anatomy of the lateral ankle ligaments. Am. J. Sports Med. 22, 72–77 (1994).
Edama, M. et al. Morphological characteristics of the lateral talocalcaneal ligament: a large-scale anatomical study. Surg. Radiol. Anat. 41, 25–28 (2019).
Funding
Open Access funding provided by Gothenburg University Library.
Author information
Authors and Affiliations
Contributions
P.S and M.P. wrote the main manuscript text and K.G.G. prepared all figures. Calculating statistics P.S., M.P, and B.C. Study design P.S. All authors reviewed and accepted the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szaro, P., Ghali Gataa, K., Polaczek, M. et al. The double fascicular variations of the anterior talofibular ligament and the calcaneofibular ligament correlate with interconnections between lateral ankle structures revealed on magnetic resonance imaging. Sci Rep 10, 20801 (2020). https://doi.org/10.1038/s41598-020-77856-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77856-8
This article is cited by
-
Biomechanical improvement of anterior talofibular ligament by augmentation repair of ligament advance reinforcement system: a cadaver study
BMC Surgery (2023)
-
The increased anterior talofibular ligament–posterior talofibular ligament angle on MRI may help evaluate chronic ankle instability
Surgical and Radiologic Anatomy (2023)
-
Individual fascicles of the ankle lateral ligaments and the lateral fibulotalocalcaneal ligament complex can be identified on 3D volumetric MRI
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
-
Difference in the fibular attachment structure between the superior and inferior fascicles of the anterior talofibular ligament using ultrasonography and histological examinations
Surgical and Radiologic Anatomy (2022)
-
Anatomical variants of the medioplantar oblique ligament and inferoplantar longitudinal ligament: an MRI study
Surgical and Radiologic Anatomy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.