Abstract
Serology is essential for Q fever diagnostics, a disease caused by the bacterial pathogen Coxiella burnetii. The gold standard test is an immunofluorescence assay utilizing whole cell antigens, which are both dangerous and laborious to produce. Complexities of the antigen coupled with the subjective nature of the assay lead to decreased uniformity of test results and underscore the need for improved methodologies. Thirty-three C. burnetii proteins, previously identified as immunoreactive, were screened for reactivity to naturally infected goat serum. Based on reactivity, 10 proteins were analyzed in a secondary screen against human serum from healthy donors. Assay sensitivity and specificity ranged from 21 to 71% and 90 to 100%, respectively. Three promising antigens were identified based on receiver operating characteristic curve analysis (CBU_1718, CBU_0307, and CBU_1398). Five multiplex assays failed to outperform the individual proteins, with sensitivities and specificities ranging from 29 to 57% and 90 to 100%, respectively. Truncating the top antigen, CBU_1718, had no effect on specificity (90%); yet sensitivity decreased dramatically (71% to 21%). Through this study, we have expanded the subset of C. burnetii immunoreactive proteins validated by enzyme-linked immunosorbent assay and demonstrate the effect of novel antigen combinations and protein truncations on assay performance.
Similar content being viewed by others
Introduction
Diagnostic testing for Q fever, caused by the bacterial pathogen, Coxiella burnetii, is largely dependent on serology1,2. During the early stages of infection, a diagnosis can be made through detection of bacterial DNA by PCR from samples of whole blood or serum; however, the window of effectiveness is usually limited to the first two weeks of symptom onset2. Symptoms of acute Q fever are often nonspecific with fever, fatigue, chills and myalgia being the most frequently reported2. This often leads to a low clinical suspicion, which limits the ability to effectively utilize PCR-based assays. Due to the persistence of IgG antibodies to C. burnetii for months to years after infection, serological diagnosis of acute Q fever relies on paired acute and convalescent samples taken 3–6 weeks apart2. In less than 5% of acute cases, chronic Q fever can develop with symptoms ranging from endocarditis to chronic hepatitis or chronic vascular infections2. The success of PCR in diagnosis of chronic Q fever cases ranges from 33 to 64%; as a result, serology is essential for Q fever diagnostics. Persistent IgG antibodies can also influence serological testing for chronic Q fever; therefore, serology is not reliable in the absence of clinical findings. The performance of serology-based testing methods can vary based on the source of the antigen, background titers of the population being tested, as well as the type of test being utilized3.
Methods for serological testing include complement fixation, radioimmunoassay, enzyme-linked immunosorbent assay (ELISA), Western blotting and the immunofluorescence assay (IFA). IFA is the gold standard serologic assay for Q fever, and in the United States, more than 12,800 serum samples are tested annually by this method2,4. The assay utilizes antigen coated onto slides to detect the presence of anti-C. burnetii IgG antibodies from serum resulting in fluorescence that is visualized under a microscope, which can be subjective. The antigens used are inactivated cells from the Nine Mile Phase I and Nine Mile Phase II isolates of C. burnetii. Nine Mile phase I is the C. burnetii reference strain and IgG antibodies against this strain typically develop in higher abundance in chronic Q fever patients2. The phase II strain of C. burnetii is an avirulent form of the Nine Mile strain and IgG antibodies against it typically develop to higher levels during acute Q fever2. Production of the phase I antigen is hazardous owing to the need to culture large amounts of pathogenic bacteria, which requires specialized equipment in a BSL3 facility2,5. C. burnetii has a low infectious dose of 1–10 organisms, is naturally stable in the environment for long periods, is able to spread via aerosols, and has been previously weaponized6,7. These characteristics led to its classification as a potential bioweapon and a select agent, which further restricts antigen preparation to select facilities8. The slow growth kinetics of the bacteria coupled with its specialized growth requirements are additional barriers to large-scale production. Furthermore, the inherent complexities of the whole cell antigen as well as the subjective nature of the IFA lead to inconsistencies in test results.
A recombinant protein based diagnostic assay would eliminate the need for the dangerous and labor-intensive generation of whole cell antigen and improve test uniformity. A number of studies have identified C. burnetii immunogenic proteins using a variety of methodologies including 2-dimensional gel electrophoresis (2D-GE), protein microarrays and even immunocapturing9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. Only ~ 20% of the identified C. burnetii immunoreactive proteins have been validated in an ELISA; none of which are as sensitive and specific as the whole cell antigen13,14,16,20,27. This suggests a need for further exploration of the utility of these antigens in a multiplexed assay, which has not been developed. This study aims to expand the subset of C. burnetii immunoreactive proteins that have been validated by ELISA and assess the top candidates for use in a multiplexed assay. Furthermore, truncated fragments of the best antigen (CBU_1718) were generated in an effort to improve antibody detection.
Methods
Bacterial strains, plasmids and growth conditions
The Coxiella burnetii strain used in this study was Nine Mile phase I (NMI)28. This strain, isolated from a tick in 19351, can cause Q fever in humans29, and it is the reference strain used as whole cell antigen in current diagnostic tests. The strain was grown in ACCM-2 and DNA was extracted as previously described30. The Escherichia coli strain used in this study was K12 JM109 (New England Biolabs). Plasmid pIVEX2.4d was utilized as the over-expression vector (Biotechrabbit). The recombinant C. burnetii constructs used in this study are listed in Supplemental Table 1. E. coli was grown in Luria–Bertani medium at 37 °C. When required, carbenicillin was used at 100 mg l−1.
Over-expression and purification of recombinant proteins
Coding regions of each of the 33 proteins and 4 truncations were amplified from the C. burnetii NMI template by PCR using gene specific primers (Table S1). PCR reactions were carried out using Phusion High-Fidelity DNA Polymerase (Thermo Fisher Scientific) per the manufacturer’s instructions. Resulting PCR products were cloned into the over-expression vector pIVEX2.4d, introducing an N-terminal 6 histidine tag. The recombinant C. burnetii constructs were purified using the HiSpeed Plasmid Midi Kit (Qiagen) per the manufacturer’s instructions and confirmed by sequencing. Cell-free expression of the recombinant proteins was performed using the RTS 100 E. coli HY kit (Biotechrabbit) according to the manufacturer’s protocol. Proteins for the primary screen were purified using Ni–NTA magnetic agarose beads (Qiagen) under native conditions and stored in 25% glycerol at − 80 °C. Large scale expressions were performed for the secondary screen using the RTS 500 ProteoMaster E. coli HY Kit (Biotechrabbit) and purified using Ni–NTA agarose (Qiagen) via the column method under native conditions. Post purification buffer exchange and concentration was performed using Amicon Ultra-15 Centrifugal Filter Units (Millipore Sigma) per manufacturer’s instructions. Purified proteins were stored at − 20 °C in PBS containing 1 × protein stabilization cocktail (Thermo Fisher Scientific). Protein expression was verified by SDS-PAGE analysis.
Serum sample procurement
Goat serum samples for the primary screen were from stored stocks obtained during a 2011 Q fever outbreak31. For the secondary screen, we utilized de-identified and banked human serum samples that were originally derived from routine blood donations in the United States. Serum samples were considered positive for anti-C. burnetii antibodies against either phase I or phase II Coxiella based on IFA (titer ≥ 16) and/or ELISA (absorbance ≥ twofold relative to BSA controls). Samples were stored at − 80 °C. This study does not involve human subjects under 45 CFR 46.102(f) and was approved by the Human Research Protection Office of the Centers for Disease Control and Prevention.
Enzyme-linked immunosorbent assay (ELISA)
Proteins were coated onto immulon 2 high bind 96-well microtiter EIA plates (Thermo Fisher Scientific) at 2 µg ml−1 by incubating at 4 °C in 100 µl per well of coating buffer (50 mM Na2CO3, 50 mM NaHCO3, pH 9.6) overnight. Empty well controls contained coating buffer only. Plates were washed in 300 µl per well of PBS containing 0.05% Tween-20 (PBST). Wells were blocked with 200 µl for 2 h at 37 °C in a humidified atmosphere. Assays using goat serum were blocked in PBST containing 5% bovine milk; assays using human serum were blocked in 50% PBST/50% SEA block buffer (Thermo Fisher Scientific). Following the blocking step, plates were incubated with 100 µl per well of serum (1:100) in PBST for 1 h at 37 °C in a humidified atmosphere. Plates were washed and incubated with 100 µl per well of a biotin-labeled, species-specific primary antibody against IgG (KPL) at 1:50,000. Plates were washed and incubated with 100 µl per well of peroxidase-labeled streptavidin (KPL) at 1:2000 for 1 h each at 37 °C in a humidified atmosphere. Detection was achieved through addition of 100 µl per well of ABTS substrate (KPL). Reactions were stopped with 100 µl per well of 1% SDS and absorbance measured at 405 nm using an ELx800 microplate reader (BioTek).
Statistical analysis
Sensitivity and specificity were determined by receiver operating characteristic (ROC) curve analysis. A 5% confidence limit was used to determine statistical significance. All analyses were performed using GraphPad Prism version 7.01 (GraphPad Software Inc., La Jolla, California).
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC.
Results
Selection and primary screening of immunoreactive proteins
A meta-analysis was performed to find studies between 2005 and 2015 that identified candidate C. burnetii immunoreactive proteins. A total of 16 publications were found with methodologies for seropositive identification including 2-dimensional gel electrophoresis, Western blot and protein microarrays11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. Proteins selected for inclusion in this study fall into three categories. Category I includes 13 proteins based on seroreactivity in ≥ 4 publications. Category II includes three proteins, which demonstrated seroreactivity against human serum in ≥ 3 studies. Finally, category III consists of 17 proteins all of which were identified in ≥ 2 immunoproteomic studies, with at least one of those studies using human serum.
A total of 33 proteins were used as antigens in ELISAs to assess reactivity to goat serum positive for antibodies against phase I and/or phase II C. burnetii. Goat serum was utilized in the initial screen in order to preserve limited stocks of anti-C. burnetii antibody positive human serum. Positive reactions were defined as an absorbance reading (405 nm) ≥ mean + 3 × the standard deviation of BSA negative controls and demonstrated statistical significance (p-value < 0.05) based on a Student’s t-test. A total of nine proteins were selected for further analysis based on the ability to detect antibodies against C. burnetii in ≥ 50% of the serum samples tested (Fig. 1). Although, CBU_1065 was only able to detect antibodies in 12.5% of the serum samples tested, the intensity of the reaction was much greater than other antigens. Therefore, it was also included in additional screening as it might be useful in improving sensitivity of a multiplexed assay. The remaining proteins were considered weakly reactive (< 50% positive) or nonreactive (0% positive) and were excluded from further analysis.
Primary screen of recombinant protein antigens. Recombinant proteins were used as antigens in enzyme-linked immunosorbent assays (ELISA) against 8 goat serum samples that were positive for antibodies against phase I and/or phase II whole cell C. burnetii. Positive reactions were defined as an absorbance reading (405 nm) ≥ mean + 3 × the standard deviation of BSA negative controls and demonstrated statistical significance (p-value < 0.05) based on a Student’s t-test. Data is presented as the percentage of positive serum samples for each antigen. Grey bars represent recombinant protein antigens that were selected for further assay development.
Secondary screening of immunoreactive proteins
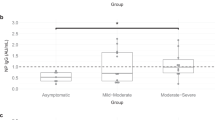
The top 10 immunoreactive proteins selected from the primary screen were utilized as antigens in ELISAs to assess their ability to correctly differentiate human serum positive for anti-C. burnetii antibodies against negative controls. The recombinant proteins were compared to whole cell phase I and phase II C. burnetii using a panel of 24 human serum samples (14 positives by IFA for either phase I or phase II anti-C. burnetii antibodies; 10 samples negative by IFA). ROC curve analysis was performed using the resulting absorbance readings to determine the accuracy of each protein as a diagnostic antigen (Fig. 2). The area under the ROC curve (AUC) determines how well the diagnostic test can classify serum as containing anti-C. burnetii antibodies. An AUC of 1 indicates an accurate test; whereas, a test with an AUC of ≤ 0.5 is unable to distinguish the positive samples from the negative controls. The best antigens, CBU_1718 and CBU_0307, were able to correctly classify the same number of serum samples (71.43% sensitivity and 90% specificity) (Table 1). CBU_1718 had a slightly better discriminative ability (AUC 0.8786, p = 0.0019) compared to CBU_0307 (AUC 0.7929, p = 0.0164). Additionally, CBU_1398 had an AUC of 0.75 and showed significant discriminative ability (p < 0.05); however, the sensitivity was only 57%. No other recombinant protein antigens tested had significant discriminative ability. The whole cell antigens, which are the gold standard for diagnostic testing and were the antigens used in the IFA to define the true positive samples in this study, outperformed all of the tested proteins with a sensitivity of 85.71% and 100% specificity for PhI (AUC 0.95, p = 0.0002) and 92.86% sensitivity, 100% specificity for PhII (AUC 0.9786, p < 0.0001). The most inaccurate protein was CBU_0718 with a sensitivity of 28.57% and a specificity of 90% (AUC 0.5786, p = 0.5195).
ROC curve analysis of recombinant protein antigens. Recombinant proteins were used as antigens in enzyme-linked immunosorbent assays (ELISA) against 24 human serum samples. Fourteen were positive for antibodies against phase I and/or phase II; 10 were negative. The AUC for each antigen is displayed as black dots, bars represent the 95% confidence interval.
Analysis of multiplexed antigens on assay accuracy
Multiplexed assays were performed using combinations of protein antigens to improve assay sensitivity. We tested five combinations based on predicted sensitivity and specificity from the singleplex ROC curve analysis. As demonstrated in Table 1, combination 1 equally combined five different proteins (CBU_1718, CBU_0307, CBU_1398, CBU_1065 and CBU_0891) and performed the best with a sensitivity of 57.14% and specificity of 100%. The AUC of combination 1 was 0.85, p = 0.0041, while still significant, it was worse than the top performing single antigen, CBU_1718 (Fig. 2). Combinations 3 (AUC 0.8286, p = 0.0071) and 4 (AUC 0.7786, p = 0.0224) both had significant discriminative ability with sensitivities/specificities of 50%/100% and 42.86%/90%, respectively. Combinations 2 (AUC 0.7286, p = 0.0610) and 5 (AUC 0.7, p = 0.1011) demonstrated sensitivity/specificity of 50%/90% and 28.57%/90%, respectively. For each of the five combinations none was more accurate than the individual proteins.
Analysis of protein truncations on assay accuracy
We examined the efficacy of truncated proteins as antigens in an effort to eliminate potential non-specific epitopes and improve assay specificity. We selected the best antigen based on the results of the secondary screen, CBU_1718, for this analysis and created four fragments by eliminating portions of either amino-or carboxy-termini at random (Table 2). Fragment A is 27 kDa and lacks the amino-terminal. The carboxy-terminal was eliminated from truncations B, C and D, which are 32 kDa, 49 kDa and 53 kDa, respectively. Protein fragments were analyzed against six serum samples selected based on results from the full-length CBU_1718 protein antigen in the secondary ELISA screen (Table 2). Three serum samples were used that were negative on the IFA against the PhI and/or PhII whole cell antigen. The true negative was also negative using the full-length CBU_1718 antigen, borderline negative was close to the cut-off value in an ELISA with the full-length CBU_1718, and false positive was positive using the full-length CBU_1718 antigen due to non-specific binding. Three serum samples were tested that were positive against the PhI and/or PhII whole cell antigen by IFA. The false negative was negative by ELISA using the full-length CBU_1718 antigen, borderline positive was close to the cut-off, and the last was a strong positive based on results of the full-length CBU_1718 protein in the secondary ELISA screen. Fragments B and C lost reactivity to the borderline positive and strong positive serum samples; however, the false positive serum sample was still recognized by these fragments. The third C-terminal truncation, fragment D did not lose reactivity to any of the tested serum samples. Interestingly, fragment A lost reactivity to the false and borderline positives; yet, the strong positive was still recognized. Therefore, we analyzed fragment A against all 24 serum samples in order to determine how it performs as an antigen relative to the full-length protein (Table 1 and Fig. 2). Although specificity of the fragmented antigen did not change (90%), assay sensitivity fell to 21.43% with an AUC of 0.5714 (p = 0.5582).
Discussion
A total of 33 C. burnetii recombinant proteins were analyzed for use as antigens in singleplex and multiplex ELISAs in an effort to improve Q fever diagnostic testing. All tested proteins had previously been identified as immunoreactive, 17 of which had never been validated by ELISA11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. In a primary screen against sera from naturally infected goats, 9 proteins displayed reactivity to greater than 50% of the samples tested and were selected for further assay development. In a secondary screen against human sera from healthy donors, assay sensitivity ranged from 21 to 71% for the individual proteins with specificities ranging from 90 to 100%. Three of the tested recombinant proteins were good candidates based on ROC curve analysis.
Eleven of the tested proteins had no reactivity in the initial screen while 13 were considered weakly reactive. One protein found to be weakly reactive in the present study was the highly published antigen, CBU_1910 (Com1)32. Com1 had previously been identified as seroreactive against human and rodent sera with sensitivity and specificity ranging from 37.5% to 100% and 71% to 100%, respectively13,33,34. Interestingly, this antigen performed poorly in this study when tested against serum from naturally infected goats. These findings suggest that the antigenicity of Com1 and possibly other antigens may be species-specific. Similarly, the three proteins selected for inclusion based on category II criteria (≥ 3 human serum studies) were weakly reactive (CBU_1719) or non-reactive (CBU_1143 and CBU_0545) against goat serum in the initial screen. The latter proteins have only been identified in screens using human serum; whereas CBU_1719 was identified in screens using either human or rodent serum. In a comprehensive review of C. burnetii immunoreactive proteins, it was demonstrated that 65% of antigens identified with human serum do not overlap with antigens identified in screens using rodent serum32. The findings highlight an important limitation to the study herein, which may have missed useful human diagnostic antigens as a result of using caprine serum for the initial screen. Unfortunately, the use of goat serum was necessary to conserve the limited stocks of human serum while screening a large number of recombinant antigens for functionality.
Combinations of the top performing antigens were attempted by equally pooling from two to five proteins. In each case, the top performing antigen of the mix functioned better independently (Table 1 and Fig. 2). A previous report noted that a C. burnetii recombinant protein-based multiplexed assay had been attempted; however, details of the assay, including the antigens used, were not published. In the study, the use of multiple proteins increased assay sensitivity albeit at the expense of assay specificity13. In the study herein, assay sensitivity was compromised by combining multiple antigens. This is likely a result of the different analysis performed to determine cut-off values. Herein ROC curves were utilized to assign cut-off values, which allows for the highest true-positive rate while maintaining the lowest false positive rate. In each case, assay sensitivity could be improved by adjusting the cut-off; however, as assay sensitivity increases it does so at the expense of assay specificity. Regardless of the type of analysis used, in the absence of improved antigen specificity, it is unlikely that a multiplexed antigen will surpass whole cell bacteria as the favored diagnostic antigen.
The protein CBU_1718 (GroEL or HtpB), is a heat shock protein and was the best performing antigen among the 33 tested. It was previously identified as an immunodominant C. burnetii protein in more than 16 publications against human, goat, mouse and guinea pig sera27,32. As one of the most highly published antigens, it is not surprising that a sensitivity of 71% and 90% specificity was identified for the antigen. The usefulness of GroEL as a diagnostic antigen for detecting C. burnetii infection in goats was demonstrated previously against both primary and recurrent infections27. GroEL has been identified as both immunoreactive and a useful diagnostic antigen in many other organisms including Burkholderia mallei, Burkholderia pseudomallei and Helicobacter pylori among others35,36,37. A previous study utilizing protein microarray demonstrated that GroEL of C. burnetii displayed some cross-reactivity as it recognized 20% of sera from persons with rickettsial spotted fever and 10% from persons with Legionella pneumonia23. Similarly, recombinant GroEL displayed reactivity against 10% of the Q fever negative human serum in the present study. In an effort to reduce this non-specific reactivity, we created truncations of the GroEL protein which has proved useful in other organisms such as PstS1 of Mycobacterium tuberculosis or the multi-fragment antigen of infectious bronchitis virus38,39. Evaluation of truncated GroEL proteins herein identified a putative C. burnetii specific-epitope located between the amino acids 467 to 496 in the C-terminal region. Although sensitivity was vastly decreased herein, the ability to utilize truncated proteins as part of a multiplexed antigen may be a useful tool for further assay development.
Through this study, the subset of C. burnetii immunoreactive proteins that have been validated by ELISA has been expanded. Furthermore, the effect of novel antigen combinations and protein truncations on assay performance has been examined. Limitations of the current study include small numbers of serum samples used to screen the antigens. Furthermore, the use of human serum derived from healthy donors limits the ability to determine how these antigens perform against serum from persons with active acute and chronic Q fever.
References
Maurin, M. & Raoult, D. Q fever. Clin. Microbiol. Rev. 12, 518–553 (1999).
Anderson, A. et al. Diagnosis and management of Q fever–United States, 2013: Recommendations from CDC and the Q Fever Working Group. MMWR Recomm. Rep. 62, 1–30 (2013).
Fournier, P. E., Marrie, T. J. & Raoult, D. Diagnosis of Q fever. J. Clin. Microbiol. 36, 1823–1834 (1998).
Miller, H. K. et al. Trends in Q fever serologic testing by immunofluorescence from four large reference laboratories in the United States, 2012–2016. Sci. Rep. 8, 16670. https://doi.org/10.1038/s41598-018-34702-2 (2018).
Johnson, J. E. & Kadull, P. J. Laboratory-acquired Q fever. A report of fifty cases. Am. J. Med. 41, 391–403. https://doi.org/10.1016/0002-9343(66)90085-4 (1966).
Tigertt, W. D., Benenson, A. S. & Gochenour, W. S. Airborne Q fever. Bacteriol. Rev. 25, 285–293 (1961).
Welsh, H. H., Lennette, E. H., Abinanti, F. R. & Winn, J. F. Air-borne transmission of Q fever: The role of parturition in the generation of infective aerosols. Ann. N. Y. Acad. Sci. 70, 528–540. https://doi.org/10.1111/j.1749-6632.1958.tb35409.x (1958).
Rotz, L. D., Khan, A. S., Lillibridge, S. R., Ostroff, S. M. & Hughes, J. M. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 8, 225–230. https://doi.org/10.3201/eid0802.010164 (2002).
Zhang, G., Kiss, K., Seshadri, R., Hendrix, L. R. & Samuel, J. E. Identification and cloning of immunodominant antigens of Coxiella burnetii. Infect. Immun. 72, 844–852. https://doi.org/10.1128/iai.72.2.844-852.2004 (2004).
Xiong, X. et al. Identification of Coxiella burnetii CD8+ T-cell epitopes and delivery by attenuated Listeria monocytogenes as a vaccine vector in a C57BL/6 mouse model. J. Infect. Dis. 215, 1580–1589. https://doi.org/10.1093/infdis/jiw470 (2017).
Chao, C. C. et al. Identification, cloning, and expression of potential diagnostic markers for Q fever. Ann. N. Y. Acad. Sci. 1063, 76–78. https://doi.org/10.1196/annals.1355.010 (2005).
Coleman, S. A. et al. Proteome and antigen profiling of Coxiella burnetii developmental forms. Infect. Immun. 75, 290–298. https://doi.org/10.1128/IAI.00883-06 (2007).
Beare, P. A. et al. Candidate antigens for Q fever serodiagnosis revealed by immunoscreening of a Coxiella burnetii protein microarray. Clin. Vaccine Immunol. 15, 1771–1779. https://doi.org/10.1128/CVI.00300-08 (2008).
Chen, C. et al. A systematic approach to evaluate humoral and cellular immune responses to Coxiella burnetii immunoreactive antigens. Clin. Microbiol. Infect. 15(Suppl 2), 156–157. https://doi.org/10.1111/j.1469-0691.2008.02206.x (2009).
Sekeyova, Z. et al. Identification of protein candidates for the serodiagnosis of Q fever endocarditis by an immunoproteomic approach. Eur. J. Clin. Microbiol. Infect. Dis. 28, 287–295. https://doi.org/10.1007/s10096-008-0621-4 (2009).
Sekeyova, Z. et al. Characterization of antigens for Q fever serodiagnostics. Acta Virol. 54, 173–180. https://doi.org/10.4149/av_2010_03_173 (2010).
Vigil, A. et al. Genome-wide profiling of humoral immune response to Coxiella burnetii infection by protein microarray. Proteomics 10, 2259–2269. https://doi.org/10.1002/pmic.201000064 (2010).
Vigil, A. et al. Profiling the humoral immune response of acute and chronic Q fever by protein microarray. Mol. Cell. Proteomics 10, M110 006304. https://doi.org/10.1074/mcp.M110.006304 (2011).
Papadioti, A. et al. A proteomic approach to investigate the differential antigenic profile of two Coxiella burnetii strains. J. Proteomics 74, 1150–1159. https://doi.org/10.1016/j.jprot.2011.04.016 (2011).
Kowalczewska, M., Nappez, C., Vincentelli, R., La Scola, B. & Raoult, D. Protein candidates for Q fever serodiagnosis. FEMS Immunol. Med. Microbiol. 64, 140–142. https://doi.org/10.1111/j.1574-695X.2011.00912.x (2012).
Chen, C. et al. Identification of CD4+ T cell epitopes in C. burnetii antigens targeted by antibody responses. PLoS ONE 6, e17712. https://doi.org/10.1371/journal.pone.0017712 (2011).
Xiong, X. et al. Exploratory study on Th1 epitope-induced protective immunity against Coxiella burnetii infection. PLoS ONE 9, e87206. https://doi.org/10.1371/journal.pone.0087206 (2014).
Xiong, X., Wang, X., Wen, B., Graves, S. & Stenos, J. Potential serodiagnostic markers for Q fever identified in Coxiella burnetii by immunoproteomic and protein microarray approaches. BMC Microbiol. 12, 35. https://doi.org/10.1186/1471-2180-12-35 (2012).
Wang, X., Xiong, X., Graves, S., Stenos, J. & Wen, B. Protein array of Coxiella burnetii probed with Q fever sera. Sci. China Life Sci. 56, 453–459. https://doi.org/10.1007/s11427-013-4472-6 (2013).
Jiao, J. et al. Serological characterization of surface-exposed proteins of Coxiella burnetii. Microbiology 160, 2718–2731. https://doi.org/10.1099/mic.0.082131-0 (2014).
Deringer, J. R., Chen, C., Samuel, J. E. & Brown, W. C. Immunoreactive Coxiella burnetii Nine Mile proteins separated by 2D electrophoresis and identified by tandem mass spectrometry. Microbiology 157, 526–542. https://doi.org/10.1099/mic.0.043513-0 (2011).
Fernandes, I. et al. Evaluation of the recombinant Heat shock protein B (HspB) of Coxiella burnetii as a potential antigen for immunodiagnostic of Q fever in goats. Vet. Microbiol. 134, 300–304. https://doi.org/10.1016/j.vetmic.2008.08.024 (2009).
Stoker, M. G. & Fiset, P. Phase variation of the Nine Mile and other strains of Rickettsia burneti. Can. J. Microbiol. 2, 310–321 (1956).
Benenson, A. S. & Tigertt, W. D. Studies on Q fever in man. Trans. Assoc. Am. Physicians 69, 98–104 (1956).
Kersh, G. J. et al. Genotyping and axenic growth of Coxiella burnetii isolates found in the United States environment. Vector Borne Zoonotic Dis. 16, 588–594. https://doi.org/10.1089/vbz.2016.1972 (2016).
Bjork, A. et al. First reported multistate human Q fever outbreak in the United States, 2011. Vector Borne Zoonotic Dis. 14, 111–117. https://doi.org/10.1089/vbz.2012.1202 (2014).
Gerlach, C., Skultety, L., Henning, K., Neubauer, H. & Mertens, K. Coxiella burnetii immunogenic proteins as a basis for new Q fever diagnostic and vaccine development. Acta Virol. 61, 377–390. https://doi.org/10.4149/av_2017_320 (2017).
Bizzini, A. et al. Evaluation of a new serological test for the detection of anti-Coxiella and anti-Rickettsia antibodies. Microbes Infect. 17, 811–816. https://doi.org/10.1016/j.micinf.2015.09.015 (2015).
Zhang, G. Q. et al. Evaluation of a recombinant 27-kDa outer membrane protein of Coxiella burnetii as an immunodiagnostic reagent. Microbiol. Immunol. 42, 423–428. https://doi.org/10.1111/j.1348-0421.1998.tb02305.x (1998).
Dohre, S. K., Kamthan, A., Singh, S., Alam, S. I. & Kumar, S. Identification of a new diagnostic antigen for glanders using immunoproteome analysis. Comp. Immunol. Microbiol. Infect. Dis. 53, 26–32. https://doi.org/10.1016/j.cimid.2017.06.007 (2017).
Woo, P. C., Leung, P. K., Wong, S. S., Ho, P. L. & Yuen, K. Y. groEL encodes a highly antigenic protein in Burkholderia pseudomallei. Clin. Diagn. Lab. Immunol. 8, 832–836. https://doi.org/10.1128/CDLI.8.4.832-836.2001 (2001).
Formichella, L. et al. A novel line immunoassay based on recombinant virulence factors enables highly specific and sensitive serologic diagnosis of Helicobacter pylori infection. Clin. Vaccine Immunol. 20, 1703–1710. https://doi.org/10.1128/CVI.00433-13 (2013).
Khurshid, S., Khalid, R., Afzal, M. & Waheed Akhtar, M. Truncation of PstS1 antigen of Mycobacterium tuberculosis improves diagnostic efficiency. Tuberculosis 93, 654–659. https://doi.org/10.1016/j.tube.2013.07.005 (2013).
Ding, M. D. et al. Development of an ELISA based on a multi-fragment antigen of infectious bronchitis virus for antibodies detection. Biotechnol Lett 37, 2453–2459. https://doi.org/10.1007/s10529-015-1935-9 (2015).
Author information
Authors and Affiliations
Contributions
H.M. and G.K. designed the study, analyzed the data, and wrote the manuscript. H.M. performed the experiments.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miller, H.K., Kersh, G.J. Analysis of recombinant proteins for Q fever diagnostics. Sci Rep 10, 20934 (2020). https://doi.org/10.1038/s41598-020-77343-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77343-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.