Abstract
The repeatability of the 20-min pad test has not been reported. The aim of this study was to evaluate the test–retest reliability of the 20-min pad test in women with urodynamic stress incontinence. Among 89 enrolled women, 67 (75%) women were diagnosed with urodynamic stress incontinence and were examined in this study. The mean strong-desire volume of all the women was 306.7 ± 115.7 mL. The pad weights of the test versus retest were 28.3 ± 41.2 g versus 28.4 ± 38.6 g, p = 0.29, respectively. The test and retest pad weight results had a Spearman’s rho of 0.788 (p < 0.0001). The intraclass correlation coefficient was 0.793 (95% confidence interval, 0.704–0.882; p < 0.0001). The Bland–Altman plots all revealed good agreement between the test and the retest in the pad weights. In conclusion, the 20-min pad test infused with a strong-desired volume has good test–retest reliability to assess the severity of urine leakage for women with urodynamic stress incontinence.
Similar content being viewed by others
Introduction
The pad test was initially proposed by Sutherst et al. in 19811 and modified by the Standardization Committee of the International Continence Society (ICS)2,3. It is a noninvasive method of quantifying the volume of urine leakage in patients with urinary incontinence4. There are two versions: the short-term pad test, which is performed in the clinic over a period of one hour, and the long-term pad test, which is usually performed at home over a period of 24 h4,5. The most commonly used protocol of the pad test is the standardized ICS one-hour pad test protocol, starting with 500 mL drinking water without voiding3. Thus, the doctors cannot know the exact urine volume in the bladder when the test begins.
The20-min pad test was proposed by Hahn and Fall6 and modified by Sand and Ostergard since 20057. The 20-min pad test is performed with artificial water infusion into the bladder rather than by natural diuresis as in a 1-h pad test7. The 20-min pad test was reported to have a better sensitivity than the one-hour pad test for women with stress urinary incontinence (SUI)8. In addition, the strong-desired (SD) volume was reported to have a better sensitivity than 250 mL as the volume of water infusion before the initiation of the 20-min pad testing9.
A significant variation between the test and the retest and inadequate repeatability of the one-hour pad test has been reported10,11. As mentioned above, the 20-min pad test has been reported to have a better sensitivity than the 1-h pad test8. However, the repeatability of the 20-min pad test has not been reported. We were interested in whether the 20-min pad test had adequate repeatability. Thus, the aim of this study was to elucidate the test–retest reliability of the 20-min pad test.
Results
After urodynamic studies, 67/89 (75%) of women with SUI were diagnosed as having urodynamic stress incontinence (USI) and received a retest of the 20-min pad testing. According to the presence of detrusor overactivity (DO), these 67 women with USI were divided into the USI only group (n = 53) and the USI and DO group (n = 14). The USI with DO group had a lower volume at first desire, normal desire and SD to void compared with the USI only group (Table 1).
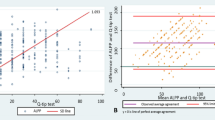
The pad weights of the test and the retest in all 67 women, the USI only group and the USI and DO group are shown in Table 2. The distribution of pad weights of the test and the retest in all women and both subgroups are shown in Fig. 1.
The Wilcoxon signed rank test revealed no difference in pad weights between the test and the retest in all women (p = 0.29), the USI only group (p = 0.40), and the USI and DO group (p = 0.66). In addition, the Spearman correlation of pad weights between the test and the retest was 0.788 (p < 0.0001) in the 67 women (Fig. 1a). The Bland–Altman plot revealed a mean difference of − 0.125 (confidence interval [CI]: − 6.420 to 6.179) for the test vs. retest results (limits of agreements: − 50.786 to 50.536) (Fig. 2a). There was no difference in variances (Pitman’s test, r = 0.106, p = 0.393).
In addition, the subgroup analysis also revealed a good rest and retest correlation in the pad weight of the USI only group (rho = 0.761, p < 0.0001, Fig. 1b). The Bland–Altman plot revealed a mean difference of 0.881 (CI: − 5.772 to 7.534) for the test vs. retest results (limits of agreements: − 48.188 to 46.426) (Fig. 2b); and there was no difference in variances (Pitman’s test, r = 0.172, p = 0.219).
The subgroup analysis also showed a good rest and retest correlation in the pad weight of the USI and DO group (rho = 0.848, p = 0.0001) (Fig. 1c, Table 2). The Bland–Altman plot revealed a mean difference of − 3.936 (CI: − 22.572 to 14.701) for the test vs. retest results (limits of agreements: − 67.199 to 59.328) (Fig. 2c); and there was no difference in variances (Pitman’s test, r = − 0.007, p = 0.981). The intraclass correlation coefficients of the pad weights between the test and the retest were 0.793 (95% CI 0.704–0.882; p < 0.0001) in all 67 women with USI, 0.797 (95% CI 0.698–0.896; p < 0.0001) in the USI only group, and 0.785 (95% CI 0.581–0.990; p = 0.0002) in the USI and DO group (Table 2).
Pad weight > 1 g was defined as the positive result, and there was no significant difference in the results between the test and retest pad tests (n = 67, McNemar’s test, p = 0.48). The agreement rate was 88.1%. The kappa statistic showed a substantial agreement (kappa value = 0.62, 95% CI 0.38–0.86).
Similarly, in the USI only group, there was no significant difference in the results between the test and retest pad tests (n = 53, McNemar’s test, p = 0.26). The agreement rate was 86.8%. The kappa statistic showed a moderate agreement (kappa value = 0.59, 95% CI 0.31–0.86).
In the USI and DO group, there was no significant difference in the results between the test and retest pad tests (n = 14, McNemar’s test, p = 0.32). The agreement rate was 92.9%. The kappa statistic showed a substantial agreement (kappa value = 0.76, 95% CI 0.32–1.00).
Discussion
Significant variation between the test and retest and inadequate repeatability of the one-hour pad test have been reported10,11. Nonetheless, in our study, pad weights in the test and retest of the 20-min pad testing revealed a significant Spearman’s correlation (Table 2), good agreement in the Bland–Altman plot (Fig. 2), a good intraclass correlation (Table 2), and no difference in the Wilcoxon signed rank test (Table 2). Thus, our study revealed that the 20-min pad test should have a good test–retest reliability for the quantification of urine leakage for female patients with USI.
In Table 1, women in the USI and DO group tended to have a smaller bladder capacity with a mean infused volume of less than 250 mL (mean: 238.7 mL), while the USI only group had a mean infused volume of more than 250 mL (mean 324.7 mL, Table 1). It has been reported that bladder infusion with an SD volume of water has better sensitivity than bladder infusion with 250 mL before the beginning of the 20-min pad testing9. Our study confirmed that if we infused 250 mL into the bladder for pad testing in each USI woman, some women would have bladder overdistension or inadequate distension, resulting in excessive or decreased urine leakage during pad testing, leading to overestimation or underestimation of the SUI severity. The above findings may support the findings of better sensitivity of bladder infusion with the SD volume of water for a 20-min pad test compared with 250 mL9.
Pad testing is used to assess SUI severity4. In this study, the determination of the SD volume was derived from filling cystometry, which is an invasive examination. However, we can estimate the SD volume from the bladder diary without the need for filling cystometry. It had been reported that excluding the first morning void, the days 1 to 3 average maximum daytime voided volumes in the bladder diary had good correlation with the SD volume12. In addition, on day 1, the maximum daytime voided volumes have been shown to be well correlated with the SD volume12. Thus, we can request that our patient record the bladder diary for at least one day before the 20-min pad testing, and then we can derive the maximum daytime voided volume as a surrogate for the SD volume. Therefore, we can use the maximum daytime voided volume as the volume for bladder infusion before the initiation of pad testing. In addition, simply infusing distilled water until one feels that one must go to the restroom might be another alternative. Furthermore, a soft, thin, lubricated catheter is suggested to minimize the irritation to the urothelium of the urethra, which may induce more urine leakage or urethral contractility13.
Common female lower urinary tract disorders include SUI, overactive bladder syndrome (OAB), bladder outlet obstruction, bladder dysfunction and interstitial cystitis/painful bladder syndrome (IC/PBS)14. SUI is the complaint of involuntary loss of urine on effort or physical exertion, or on sneezing or coughing15, and is generally treated by surgery16. OAB is defined by the presence of urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, and in the absence of urinary tract infection or other obvious pathology15. OAB is frequently treated by pharmacology, such as antimuscarinics and beta-3 agonists17. Refractory OAB can be treated by sacral neuromodulation, transvaginal electrical stimulation or intravesical botox injection18,19. Based on the finding of good test–retest reliability of the 20-min pad test for women with USI with or without DO, the 20-min pad test seems to be a good tool to assess the severity of SUI with or without OAB.
IC/PBS is a complex pathology, which is often associated with vulvodynia, endometriosis and pelvic floor dysfunction in women20, and may present with urinary urgency, urgency incontinence, recurrent urinary tract infection, vaginal dryness or dyspareunia21. Thus, IC/PBS should be considered in the differential diagnosis for women with overactive bladder symptoms with pelvic organ discomfort/pain21. Pad tests have been used to assess the therapeutic effect in women with OAB22,23. Steps for performing a 20-min pad test include hand-washing7. Hand-washing may induce involuntary detrusor contraction, resulting in urgency incontinence24. Thus, the 20-min pad test might be used to assess urgency incontinence in women with IC/PBS.
Limitations of this study include the small sample size and the fact that the work was undertaken more than a decade ago. A larger prospective study may be proposed in the future.
In conclusion, the 20-min pad test infused with the SD volume of water has good test–retest reliability to assess the severity of urine leakage for women with USI.
Methods
Between August 2007 and December 2010, all consecutive women with SUI who visited the urogynaecology outpatient clinics of a tertiary referral centre were invited to participate in this study. The exclusion criteria included urinary tract infection and chronic pelvic inflammation and without USI. Only women with USI were included in this study. This study was approved by the Research Ethics Committee of National Taiwan University Hospital. Informed consent was obtained from all participants. All methods in this study were performed in accordance with the relevant guidelines and regulations.
Each enrolled woman underwent a urodynamic study, including uroflowmetry, filling (with a rate of 60 mL H2O/min of 35 °C distilled water) and voiding cystometry, and stress urethral pressure profile. The SD volume for each patient was derived from the filling cystometry.
The 20-min pad test was first proposed by Hahn and Fall6 and modified by Sand and Ostergard7. The detailed steps are as follows. Each patient's bladder was emptied with a transurethral catheter and refilled with the SD volume of distilled water. The catheter was then removed, and the patient returned to a standing position with a preweighed perineal pad placed on the underwear. Thereafter, the patient was asked to cough 10 times, bear down 10 times, do 10 deep knee bends, jump up and down on the spot 10 times, wash her hands under cold water for 1 min, walk up and down five stairs 10 times, walk in the hall for 10 min, and then remove the perineal pad. The perineal pad was weighed, and the weight gain was derived by subtracting the original dry pad weight from the current pad weight. The positive pad weight result was defined as more than 1 g of weight gain7,25.
Because the main purpose of this study was to evaluate the test–retest reliability of the 20-min pad test for patients with USI, only patients with USI were requested to receive a retest of the 20-min pad test within one week after the previous pad test. The physical activities were the same in the test and retest of the 20-min pad testing.
In this study, USI was diagnosed if involuntary urine leakage was noted during filling cystometry, associated with increased intra-abdominal pressure and an absence of detrusor contraction. DO was diagnosed if involuntary detrusor contraction occurred during filling cystometry.
Multichannel urodynamic equipment (Life-Tech, Houston, TX, USA) with computer analysis and Urovision (Urolab Janus System V, Houston, TX, USA) was used. All terminology conformed to the standards recommended by the ICS3. All procedures were performed by an experienced technician, and the data were interpreted by a single observer to avoid interobserver variability.
STATA software (Version 11.0; Stata Corp, College Station, TX, USA) was used for the statistical analyses. The Spearman rank-correlation coefficient and intraclass correlation coefficient were tested for correlation and reliability of the test and retest results. The Wilcoxon signed rank test was tested for the difference of the test and retest. A p value of less than 0.05 was considered statistically significant. A Bland–Altman plot was plotted as the mean difference between the test and retest results against the average of the test and retest results to assess agreement between the two tests26. The limits of agreement were defined as the mean difference ± 1.96 X standard deviation. Pitman’s test was used to test the difference in variances27. Cohen’s kappa statistic is used to measure interrater reliability for categorical items28. Kappa statistic < 0.00 indicates poor agreement, 0–0.20 indicates slight agreement, 0.21–0.40 indicates fair agreement, 0.41–0.60 indicates moderate agreement, 0.61–0.80 indicates substantial agreement, and 0.81–1 indicates almost perfect agreement29.
References
Sutherst, J., Brown, M. & Shawer, M. Assessing the severity of urinary incontinence in women by weighing perineal pads. Lancet 1, 1128–1130 (1981).
Abrams, P., Blaivas, J. G., Stanton, S. L. & Andersen, J. T. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand. J. Urol. Nephrol. Suppl. 114, 5–19 (1988).
Abrams, P. et al. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the International Continence Society. Neurourol. Urodyn. 21, 167–178 (2002).
Krhut, J. et al. Pad weight testing in the evaluation of urinary incontinence. Neurourol. Urodyn. 33, 507–510 (2014).
Ferreira, C. H. & Bø, K. The pad test for urinary incontinence in women. J. Physiother. 61, 98 (2015).
Hahn, I. & Fall, M. Objective quantification of stress urinary incontinence: A short, reproducible, provocative pad-test. Neurourol. Urodyn. 10, 475–481 (1991).
Sand, P. K. & Ostergard, D. R. Pad testing. In Urodynamics and The Evaluation of Female Incontinence: A Practical Guide (eds Sand, P. K. & Ostergard, D. R.) 20–26 (Springer, Berlin, 1995).
Wu, W. Y., Sheu, B. C. & Lin, H. H. Comparison of 20-minute pad test versus 1-hour pad test in women with stress urinary incontinence. Urology 68, 764–768 (2006).
Wu, W. Y., Sheu, B. C. & Lin, H. H. Twenty-minute pad test: Comparison of infusion of 250 ml of water with strong-desire volume in the bladder in women with stress urinary incontinence. Eur. J. Obstet. Gynecol. Reprod. Biol. 136, 121–125 (2008).
Lose, G., Rosenkilde, P., Gammelgaard, J. & Schroeder, T. Pad-weighing test performed with standardized bladder volume. Urology 32, 78–80 (1988).
Simons, A. M., Yoong, W. C., Buckland, S. & Moore, K. H. Inadequate repeatability of the one-hour pad test: The need for a new incontinence outcome measure. BJOG 108, 315–319 (2001).
Sand, P. The evaluation of the incontinent female. Curr. Probl. Obstet. Gynecol. Fertil. 15, 109–151 (1992).
Hsiao, S. M. et al. Evaluation of bladder diary parameters based on correlation with the volume at strong-desire to void in filling cystometry. PLoS ONE 8, e69946. https://doi.org/10.1371/journal.pone.0069946 (2013).
Hsiao, S. M., Lin, H. H. & Kuo, H. C. Videourodynamic studies of women with voiding dysfunction. Sci Rep 7, 6845. https://doi.org/10.1038/s41598-017-07163-2 (2017).
Haylen, B. T. et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int. Urogynecol. J. 21, 5–26 (2010).
La Rosa, V. L. et al. Multidisciplinary management of women with pelvic organ prolapse, urinary incontinence and lower urinary tract symptoms. A clinical and psychological overview. Prz. Menopauzalny 18, 184–190 (2019).
Hsiao, S. M. & Lin, H. H. Medical treatment of female overactive bladder syndrome and treatment-related effects. J. Formos. Med. Assoc. 117, 871–878 (2018).
La Rosa, V. L. et al. A comparison of sacral neuromodulation vs. transvaginal electrical stimulation for the treatment of refractory overactive bladder: The impact on quality of life, body image, sexual function, and emotional well-being. Prz. Menopauzalny 18, 89–93 (2019).
Hsiao, S. M., Lin, H. H. & Kuo, H. C. Urodynamic prognostic factors for large post-void residual urine volume after intravesical injection of onabotulinumtoxinA for overactive bladder. Sci. Rep. 7, 43753. https://doi.org/10.1038/srep43753 (2017).
Cervigni, M. & Natale, F. Gynecological disorders in bladder pain syndrome/interstitial cystitis patients. Int. J. Urol. 21(Suppl 1), 85–88 (2014).
Patnaik, S. S. et al. Etiology, pathophysiology and biomarkers of interstitial cystitis/painful bladder syndrome. Arch. Gynecol. Obstet. 295, 1341–1359 (2017).
Yüce, T., Dökmeci, F. & Çetinkaya, ŞE. A prospective randomized trial comparing the use of tolterodine or weighted vaginal cones in women with overactive bladder syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 197, 91–97 (2016).
Brière, R., Versi, E., Richard, P. O., Gratton, M. & Tu, L. M. A preliminary study on the impact of detrusor overactivity on the efficacy of selective bladder denervation for the treatment of female refractory overactive bladder. Urology 136, 88–94 (2020).
Kondo, A. et al. Prevalence of hand-washing urinary incontinence in healthy subjects in relation to stress and urge incontinence. Neurourol. Urodyn. 11, 319–523 (1992).
Soroka, D., Drutz, H. P., Glazener, C. M., Hay-Smith, E. J. & Ross, S. Perineal pad test in evaluating outcome of treatments for female incontinence: A systematic review. Int. Urogynecol. J. 13, 165–175 (2002).
Bland, J. M. & Altman, D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1, 307–310 (1986).
Pitman, E. J. G. A note on normal correlation. Biometrika 31, 9–12 (1939).
Cohen, J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 20, 37–46 (1960).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Author information
Authors and Affiliations
Contributions
W.-Y.W. collected the data. S.-M.H. and P.-C.W. wrote the main manuscript. W.-Y.W. and S.-M.H. performed statistical analysis. S.-M.H. prepared all figures. H.-H.L. developed the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, WY., Hsiao, SM., Wu, PC. et al. Test–retest reliability of the 20-min pad test with infusion of strong-desired volume in the bladder for female urodynamic stress incontinence. Sci Rep 10, 18472 (2020). https://doi.org/10.1038/s41598-020-75567-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-75567-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.