Abstract
To investigate the relationship between diabetic foot complications (DFCs) and clinical characteristics, especially the number and types of first-degree family members with diabetes. A total of 8909 type 2 diabetes patients were enrolled. The clinical characteristics of these patients, including DFCs and family history of diabetes (FHD), were collected from medical records. Multiple regression was used to investigate the association between FHD and DFCs after adjusting for confounding factors. The patients with one and more than one first-degree family member with diabetes accounted for 18.7% and 12.8%, respectively. The proportions of the participants with a father with diabetes, a mother with diabetes, both parents with diabetes, siblings with diabetes, father and siblings with diabetes, mother and siblings with diabetes, and both parents and siblings with diabetes were 3.5%, 6.2%, 1.1%, 14.4%, 1.5%, 4%, and 0.7%, respectively. The multiple regression analysis showed that the number of family members with diabetes was positively associated with DFCs. However, among the different types of FHD, only the patients with a mother with diabetes showed a statistical association with DFCs. In addition to FHD, other factors, including gender, body mass index, platelet count, hemoglobin levels, albumin levels, high-density cholesterol levels, diabetic peripheral neuropathy, and the use of lipid-lowering agents, oral hypoglycemic agents, and insulin, were also associated with DFCs. DFCs were associated with different numbers of family members with diabetes and types of FHD. This association reveals the importance of genetic and environmental factors in DFCs and highlights the importance of adding FHD to public health strategies targeting detecting and preventing the disease.
Similar content being viewed by others
Introduction
Globally, the number of people living with diabetes mellitus (DM) has increased fourfold over the past 30 years1. Type 2 diabetes mellitus (T2DM), accounting for 90% of cases of diabetes, leads to diabetes-related complications, such as microvascular and macrovascular complications, which impair patients’ physiological and psychological well-being and impose a considerable burden on the global health-care system2.
Among the diabetes-related complications, diabetic foot complications (DFCs), a condition of chronic ulcer, occur in 25% of diabetic patients3 and cause nontraumatic lower-extremity amputations (LEAs) worldwide4. Although there is a decreasing trend in the annual incidence of LEAs caused by T2DM5, the cost of ulceration and amputations attributable to diabetes reached $10.9 billion in 20016. Several risk factors are correlated with DFCs, such as severe peripheral arterial disease (PAD)7, poor glycemic control and neuropathy8, and foot deformity9. A prospective study with a follow-up period of 10 years observed that the risk of first major amputation for DFC patients with PAD was 35 times higher than the risk for those without PAD7. However, it remains unknown whether other risk factors, including family history of diabetes (FHD), especially the different number and different types of first-degree family members, and other clinical characteristics are associated with DFCs.
FHD, an easily attended and significant medical record in the clinic, has been observed to have a significant association with diabetes10,11,12,13. A previous study observed a fourfold increase in the risk of T2DM in participants with FHD compared with those without FHD14. Additionally, FHD is closely related to diabetes-related complications, such as diabetic retinopathy (DR)15,16 and neuropathy17. A study focused on parental history of diabetes and DR found that the patients with a parental history of diabetes indicated a high prevalence of DR even after adjusting for usual confounders of DR15. However, few studies have concentrated on the relationship between DFCs and FHD, especially of the different number and different types of first-degree family member with diabetes.
Therefore, the current study aimed to investigate the relationship between DFCs and clinical characteristics, especially of the different numbers (such as one or more) and different types (such as mother, father, or siblings) of first-degree family members with diabetes.
Methods
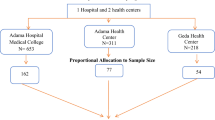
Study population
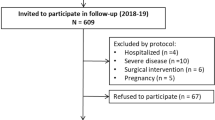
A total of 8909 T2DM patients from the National Clinical Research Center for Metabolic Diseases Diabetes Center, P.R. China, the Department of Endocrinology of the Second Xiangya Hospital of Central South University were recruited for the study from January 2013 to November 2018. All clinical characteristics were collected from the patients’ medical records, including the FHD and DFCs. The inclusion criteria were as follows: (1) type 2 diabetes and (2) age of disease onset ≥ 18 years old. The exclusion criteria were as follows: (1) type 1 diabetes or latent autoimmune diabetes in adults (LADA); (2) pregnancy or lactation; (3) cancer; (4) secondary disease resulting in elevated blood glucose; (5) patients with missing values of FHD and DFCs. A detailed flow chart is shown in supporting information Table 1. The study was approved by the Hunan Research Ethics Committees in the Second Xiangya Hospital of Central South University, China. All participants in this study provided informed consent prior to their inclusion in the study. All methods were carried out in accordance with relevant guidelines and regulations.
The definition of diabetes was mainly based on the standards of the American Diabetes Association (ADA)18.
Measurements
The measurement of hemoglobin (Hb) and platelet (PLT) levels were performed by the automated hematology analyzer ADVIA 2120 (Siemens Healthcare Diagnostics, Germany). The biochemical parameters, consisting of albumin (Alb), creatinine (Cr), uric acid (UA), fasting blood glucose (FBG), total cholesterol (TC), low-density lipoprotein-cholesterol (LDL-C), and high-density lipoprotein-cholesterol (HDL-C) levels, were evaluated by the Hitachi 912 automated analyzer. The standard methods and automatic high-performance liquid chromatography (VARIANT-II Hemoglobin Testing System; Bio-Rod Laboratories, Hercules, CA) were performed to measure the levels of fasting C-peptide and glycosylated hemoglobin (HbA1C), respectively. Additionally, the immunoturbidimetric method was used to measure proteinuria.
Definitions
The definition of FHD was the presence or absence of diabetes among the first-degree family members, including father, mother, and siblings. According to the different types of first-degree family members with diabetes, all patients were subdivided into seven groups, including fathers with diabetes, mothers with diabetes, parents with diabetes, siblings with diabetes, fathers and siblings with diabetes, mothers and siblings with diabetes, or both parents and siblings with diabetes. The formula of the body mass index (BMI) and waist-hip ratio (WHR) were as follows: weight (kg)/height (m2) and waist/hip, respectively. FBG and fasting c-peptide levels were used to calculate homoeostatic model assessment 2 of β-cell function (HOMA2-B) and insulin resistance (HOMA2-IR). The estimated glomerular filtration rate (eGFR) was calculated based on the Modification of Diet in Renal Disease (MDRD) formula. The definition of drinkers or smokers was a drinking or smoking time ≥ 1 year. The treatment of angiotensin-converting enzyme inhibitor (ACEI), angiotensin receptor blockers (ARB), oral hypoglycemic agents (OHA), or insulin were referred to regular medications taking ≥ 3 months.
The diagnosis of DFCs was based on the following three criteria: (1) diagnosed with diabetes; (2) foot tissue dystrophy (ulcer or gangrene); and (3) accompanied by neuropathy or/and vasculopathy18. Neurologic examination was used to assess the foot dorsum and position in the toes sense and to evaluate the patellar reflexes and deep tendon. DR is an important manifestation of diabetic microvascular disease, which is classified as no proliferative diabetic retinopathy (NPDR) or proliferative diabetic retinopathy (PDR) based on new retinal blood vessel formation. Diabetic peripheral neuropathy (DPN) was diagnosed by clinical symptoms of sensory nerve and autonomic nerve (such as persistent pain and/or sensory disturbance in the extremities or lower extremities; decreased sensation), the examination of neurology and electrophysiologic investigations. Diabetic nephropathy (DN) was defined by a urinary albumin creatinine ratio (UACR) ≥ 30 mg/24 h. Microalbuminuria was defined as UACR ≥ 30 mg/24 h but ≤ 300 mg/24 h, and macroalbuminuria was defined as UACR ≥ 300 mg/24 h. The definition of coronary heart disease (CHD) was impaired myocardium attributable to imbalanced coronary blood flow and myocardial demands, including acute coronary syndrome and chronic coronary syndrome, as described in a previous study19. Cerebrovascular disease (CVD) is mainly caused by intracranial blood circulation disorders caused by brain vessels, such as stoke and cerebral infarction, as previously described20. Hypertension (HTN) was defined as the SBP greater than 130 mmHg or the DBP greater than 80 mmHg.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation, and discrete variables are described as percentages. For continuous variables, one-way ANOVA or the Kruskal–Wallis H test were used to compare the differences among groups. For discrete variables, we used the Chi-square test to compare groups. Multivariate regression analysis was used to estimate the association between DFCs and clinical variables. The variables selected for the multivariate regression analysis were based on the statistical significance of univariate regression analysis, including sex, DBP, durations, smoking, BMI, FHD, Hb levels, PLT levels, LDL-C levels, HDL-C levels, TC levels, Alb levels, HOMA-IR, eGFR, lipid-lowering agents, OHA and insulin (see supporting information Table 3), whereas disease onset age and HbA1c and DPN were forcibly selected for the multivariate regression analysis. All variables in the regression analysis were described as positive or negative based on a cut-off number, which is described in detail in the supplementary materials (see supporting information Table 2). The analysis was performed by SPSS 25.0, and a two-tailed P value < 0.05 was considered statistically significant.
Results
The clinical characteristics of the participants
A total of 8909 participants diagnosed with T2DM were recruited for the study. The mean age of all patients was 57.89 ± 12.2 years, and the mean disease onset age was 49.33 ± 11.37 years. Men accounted for 55.4% of the sample. A total of 2804 (31.5%) patients had first-degree family members with diabetes. Among them, the patients with one and more than one first-degree family member with diabetes accounted for 18.7% and 12.8%, respectively. The proportions of the participants with a father with diabetes, a mother with diabetes, both parents with diabetes, siblings with diabetes, a father and siblings with diabetes, a mother and siblings with diabetes, and both parents and siblings with diabetes were 3.5%, 6.2%, 1.1%, 14.4%, 1.5%, 4%, and 0.7%, respectively. The mean concentrations of FBG and HbA1c were 8.60 ± 4.02 mmol/l and 9.06% ± 2.39%, respectively. The patients with HOMA-IR ≥ 1 accounted for 48.4%. Moreover, among the diabetes-related complications, nearly half of the subjects had DPN (50.7%), and only a small proportion of patients had DFCs (7.7%). Additionally, regarding the treatments, a large proportion of people took lipid-lowering agents (71.3%), OHA (70.9%) and insulin (70.2%). Only 17.5% and 23.1% of participants took ACEIs and ARBs, respectively (see Table 1).
Comparison of the clinical characteristics among the groups based on different numbers of first-degree relatives with diabetes
Based on the number of first-degree relatives with diabetes, the study was divided into 3 groups as follows: “No FHD” group referred to patients with no first-degree relatives with diabetes; the “One member with FHD” group referred to patients with only one first-degree relative with diabetes; the “ ≥ 2 members with FHD” group referred to patients with more than 2 first-degree relatives with diabetes. The following clinical characteristics were significantly different across the 3 groups: age, the proportion of men, DBP, the durations of diabetes, disease onset age, smoking and drinking habit, Hb levels, FBG, HbA1c levels, Alb levels, TC levels, proteinuria, eGFR, HOMA2-IR and HOMA2-B, the prevalence of DR, DPN, DF, diabetic ketosis (DK), CHD, CVD, HTN, the use of lipid-lowering agents and OHA (P < 0.05). Other parameters, including BMI, WHR, SBP, PLT levels, LDL-C levels, HDL-C levels, uric acid levels, the prevalence of DN, and the use of ACEI, ARB and insulin, were not significantly different across groups (P ≥ 0.05) (see Table 2).
Comparison of the clinical characteristics among the groups based on different types of first-degree relatives with diabetes
When comparing the clinical characteristics of the 8 groups, we found that the following parameters showed significant differences: age, the proportion of men, SBP, durations of the disease, disease onset age, smoking and drinking, Hb levels, FBG levels, HbA1C levels, Alb levels, TC levels, LDL-C levels, proteinuria, uric acid levels, eGFR, HOMA2-B, DR, DPN, DN, DK, CHD, CVD, HTN, ARB, lipid-lowering agents, OHA, and insulin (P < 0.05). Other variables, including WHR, PLT levels, HDL-C levels, HOMA2-IR, DFCs and the use of ACEI, did not differ significantly across groups (P ≥ 0.05) (see Table 3).
The association between DFCs and clinical characteristics based on different numbers and types of first-degree relatives with diabetes
The multivariable regression analysis showed DFCs was positively associated with sex (OR = 1.596, 95%CI 1.249–2.039), having one first-degree family member with diabetes (OR = 1.377, 95%CI 1.087–1.744), having more than one family first-degree member with diabetes (OR = 1.402, 95%CI 1.079–1.822), PLT levels higher than 300 * 109/L (OR = 3.158, 95%CI 1.800–5.540), DPN (OR = 2.696, 95%CI 2.159–3.366), the using of lipid-lowering agents (OR = 1.721, 95%CI 1.369–2.164) and the use of insulin (OR = 1.650, 95%CI 1.248–2.182). BMI (OR = 0.787, 95%CI 0.647–0.956), Hb levels (OR = 0.416, 95%CI 0.332–0.522), HDL-C levels (OR = 0.660, 95%CI:0.537–0.811), Alb levels (OR = 0.585, 95%CI 0.420–0.816), and OHA (OR = 0.529, 95%CI 0.431–0.649) were negatively associated with DFCs. Other variables, including DBP, duration, disease onset age, smoking, HbA1c levels eGFR, and HOMA2-IR, were not significantly associated with DFCs (P ≥ 0.05).
When the different types of first-degree relatives with diabetes was entered into the analysis instead of the number of first-degree relatives with diabetes, the results revealed that only having a mother with a history diabetes was positively associated with diabetes (OR = 1.484, 95%CI 1.022–2.154); other types, including a father, siblings, siblings and a mother, siblings and a father, both parents and siblings, both parents, displayed no significance (P > 0.05). Regarding other variables, such as BMI, Hb levels, PLT levels, DPN, and OHA, similar results were observed with the abovementioned variables in Table 4 (see Table 5).
Discussion
In this study, we found that DFCs among T2DM patients were associated with FHD, including both the number and type of first-degree family members with diabetes. However, among the different types of first-degree family members with diabetes, only the patients with a mother with a history of diabetes showed a statistical association with DFCs. In addition to FHD, other factors, including gender, BMI, PLT levels, Hb levels, Alb levels, HDL-C levels, DPN, and the use of lipid-lowering agents, OHA, and insulin, were also associated with DFCs.
The management of diabetes is an important part of public health policy. However, it is not going well, especially the management of diabetic complications, such as DFCs21,22. A previous study reported that the overall number of amputations is still high21. Thus, identifying the risk factors for DFCs among diabetes patients is important. Previous studies have revealed that many factors are associated with DFCs, such as smoking, sex, FBS, and HbA1c levels23,24,25. In our study, we observed a strong relationship between FHD and DFCs, especially of the different numbers of relatives with diabetes, in which the number of patients with one and more than 1 relative with diabetes led to 1.377- and 1.402-fold increases in the risk of DFCs, respectively, compared with those without FHD.
FHD has been considered a reflection of both genetic effects and environmental effects26. Regarding the genetic effects, with the rapid advancement in currently emerging genetic methods, such as genome-wide association studies (GWAS), a wide variety of candidate genes associated with T2DM have been identified27. The genetic risk score (GRS) has been reported to be associated with FHD28,29. A study investigated whether the GRS value was associated with parental numbers with FHD, indicating an important role of genes and FHD28. Similarly, genetic factors may be vital in DFCs, and diabetes-related complications have been reported to have a phenomenon of family clustering in type 1 diabetes30 and type 2 diabetes31. Genetic and ethnic factors play an important role in not only DPN but also DFCs32. Several studies have identified that some genetic variants may be potential risk factors for DFCs, such as the polymorphisms of MAPK1433, TNFRSF11B34, MCP135, VEGF36,37, TNF-α38, and osteoprotegerin gene39. In addition, one genome-wide association study conducted by Meng et al.33, which included 699 diabetic foot ulcers and 2695 controls, indicated that the single‐nucleotide polymorphism rs80028505 of MAPK14 was a risk factor for diabetic foot ulcers. Another study aimed to investigate the relationship between VEGF gene polymorphisms and DFCs in a Chinese population showed that the VEGF gene could be a susceptible gene of DFCs36. Another study found that polymorphisms in cytokine/chemokine genes had a close association with amputation and severe infection in individuals with DFCs38. Therefore, we conjectured from the abovementioned studies that the higher prevalence of DFCs in patients with FHD may be due to genetic impact.
A study to investigate the association between different relatives with diabetes and the prevalence of T1DM, LADA and T2DM found that any first-degree member with diabetes, such as a father with diabetes, a mother with diabetes, or siblings with diabetes, would increase the prevalence of LADA and T2DM14. When we explored the relationship between different types of FHD and DFCs, the results suggested that only having a mother with a history of diabetes was associated with DFCs after adjusting for some usual confounders of DFCs; other types of diabetes showed no statistical association. The mechanism remains unknown. Some studies observed maternal transmission in T2DM40,41. The hypotheses attributed the maternal transmission to the distinctly maternal genetic and environmental impact42. Thus, we speculated that maternal transmission likely existed in DFC individuals and that the high prevalence of DFCs in patients with a mother history of diabetes may be caused by maternal transmission. Another possible explanation was that environmental factors, such as smoking and drinking23,43,44 and BMI45, also contributed to DFCs. In our study, participants in mother history seemingly had unhealthy lifestyles with worse weight management and glycemic control and a higher percentage of smokers and drinkers (Table 3). Additionally, family lifestyles, including eating habits, are mainly derived from mothers, and mothers’ history of diabetes may be easily inclined to live with unhealthy lifestyles, leading to a higher prevalence of DFCs.
Our study found that male gender was a risk factor for DFCs. A study aimed to investigate 88 potential risk factors for amputation in DFC patients implied that male gender increased the likelihood of amputation by eightfold compared to female gender46. On the one hand, males tend to have higher foot pressure and a higher prevalence of peripheral insensate neuropathy, which may contribute to DFCs47,48. On the other hand, females may be inclined to be more self-managed and self-caring and show an active attitude towards foot care; however, males are more likely to express fear, inactive attitudes and an uncooperative manner in behavior49,50.
PLT levels were also a risk factor for DFCs. Similarly, a study observed a positive association between amputation and PLT levels in diabetic forefoot ulcers46. PLT hyperreactivity, mainly caused by hyperglycemia, metabolic disturbance and insulin resistance, plays an important role in the prothrombotic state of diabetes51. A prothrombotic state may result in atherogenesis attributable to the impaired endothelium or ruptured plaque by abnormal adhesion and aggregation of PLT levels52. Furthermore, inflammation has an association with endothelial injury and regulates platelet action-associated proteins53. Atherogenesis and inflammation may contribute to the occurrence of PAD, which has been demonstrated to be a risk factor for DFCs7,54.
The relationship between BMI and DFCs remains controversial23,46,55. On the one hand, a study investigated whether BMI had no association with diabetic foot ulcers23. On the other hand, another study showed a positive association between BMI and DFCs8, contrary to our results. This may be caused by racial differences. Dyslipidemia, such as the decreased level of HDL and increased level of triglycerides, has been proven to be related to DFCs44,56, consistent with our study. Due to the negative association between DFCs and HDL, it was easy to comprehend the higher percentage of lipid-lowering agent use in DFC patients. Moreover, one multicentric cross-sectional study revealed that insulin was positively associated with DFCs57, consistent with our findings that DFC patients had a higher proportion of insulin.
Several limitations were observed in the study. First, it was not clear whether the first-degree family members with diabetes had type 1 diabetes or type 2 diabetes. Second, this was a cross-sectional and single-center observation, and more prospective and multicenter studies should be conducted.
In conclusion, DFCs were associated with different numbers and types of family members with diabetes. This association reveals the importance of genetic and environmental factors in DFCs and highlights the importance of adding FHD to public health strategies targeting detecting and preventing the disease.
Data availability
The data included in the manuscript are available.
References
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98 (2018).
Chatterjee, S., Khunti, K. & Davies, M. J. Type 2 diabetes. Lancet 389, 2239–2251 (2017).
Armstrong, D. G., Wrobel, J. & Robbins, J. M. Guest Editorial: Are diabetes-related wounds and amputations worse than cancer?. Int. Wound J. 4, 286–287 (2007).
Harding, J. L., Pavkov, M. E., Gregg, E. W. & Burrows, N. R. Trends of nontraumatic lower-extremity amputation in end-stage renal disease and diabetes: United States, 2000–2015. Diabetes Care 42, 1430–1435 (2019).
Lin, C. W. et al. Nationwide trends in the epidemiology of diabetic foot complications and lower-extremity amputation over an 8-year period. BMJ Open Diabetes Res. Care. 7, e000795 (2019).
Boulton, A. J., Vileikyte, L., Ragnarson-Tennvall, G. & Apelqvist, J. The global burden of diabetic foot disease. Lancet 366, 1719–1724 (2005).
Morbach, S. et al. Long-term prognosis of diabetic foot patients and their limbs: Amputation and death over the course of a decade. Diabetes Care 35, 2021–2027 (2012).
Bekele, F., Chelkeba, L., Fekadu, G. & Bekele, K. Risk factors and outcomes of diabetic foot ulcer among diabetes mellitus patients admitted to Nekemte referral hospital, western Ethiopia: Prospective observational study. Ann. Med. Surg. 51, 17–23 (2020).
Prompers, L. et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 50, 18–25 (2007).
Wagner, R. et al. Family history of diabetes is associated with higher risk for prediabetes: A multicentre analysis from the German Center for Diabetes Research. Diabetologia 56, 2176–2180 (2013).
Zhang, Y. et al. Prevalence and risk of diabetes based on family history in the Shanghai High-Risk Diabetic Screen (SHiDS) study. Diabet Med. 33, 1705–1711 (2016).
Alharithy, M. K., Alobaylan, M. M., Alsugair, Z. O. & Alswat, K. A. Impact of family history of diabetes on diabetes control and complications. Endocr. Pract. 24, 773–779 (2018).
Bennet, L., Franks, P. W., Zoller, B. & Groop, L. Family history of diabetes and its relationship with insulin secretion and insulin sensitivity in Iraqi immigrants and native Swedes: A population-based cohort study. Acta Diabetol. 55, 233–242 (2018).
Carlsson, S., Midthjell, K. & Grill, V. Influence of family history of diabetes on incidence and prevalence of latent autoimmune diabetes of the adult: Results from the Nord-Trondelag Health Study. Diabetes Care 30, 3040–3045 (2007).
Lapeyre, G. et al. A parental history of diabetes is associated with a high risk of retinopathy in patients with type 2 diabetes. Diabetes Metab. 43, 557–559 (2017).
Maghbooli, Z., Pasalar, P., Keshtkar, A., Farzadfar, F. & Larijani, B. Predictive factors of diabetic complications: A possible link between family history of diabetes and diabetic retinopathy. J. Diabetes Metab. Disord. 13, 55 (2014).
Cheema, S. et al. Risk factors for microvascular complications of diabetes in a high-risk middle east population. J. Diabetes Res. 2018, 8964027 (2018).
American Diabetes, A. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2020. Diabetes Care 43, S14–S31 (2020).
Dalen, J. E., Alpert, J. S., Goldberg, R. J. & Weinstein, R. S. The epidemic of the 20(th) century: Coronary heart disease. Am. J. Med. 127, 807–812 (2014).
Sacco, R. L. & Rundek, T. Cerebrovascular disease. Curr. Opin. Neurol. 25, 1–4 (2012).
Gregg, E. W. et al. Changes in diabetes-related complications in the United States, 1990–2010. N. Engl. J. Med. 370, 1514–1523 (2014).
Mishra, S. C., Chhatbar, K. C., Kashikar, A. & Mehndiratta, A. Diabetic foot. BMJ 359, j5064 (2017).
Altenburg, N. et al. Alcohol consumption and other psycho-social conditions as important factors in the development of diabetic foot ulcers. Diabet. Med. 28, 168–174 (2011).
Sharma, S., Schaper, N. & Rayman, G. Microangiopathy: Is it relevant to wound healing in diabetic foot disease?. Diabetes Metab. Res. Rev. 36(Suppl 1), e3244 (2020).
Huang, Z. H. et al. Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: A meta-analysis. Int Wound J. 16, 1373–1382 (2019).
Cornelis, M. C., Zaitlen, N., Hu, F. B., Kraft, P. & Price, A. L. Genetic and environmental components of family history in type 2 diabetes. Hum Genet. 134, 259–267 (2015).
Langenberg, C. & Lotta, L. A. Genomic insights into the causes of type 2 diabetes. Lancet 391, 2463–2474 (2018).
Vassy, J. L. et al. Association between parental history of diabetes and type 2 diabetes genetic risk scores in the PPP-Botnia and Framingham Offspring Studies. Diabetes Res. Clin. Pract. 93, e76–e79 (2011).
t Hart, L. M. et al. Combined risk allele score of eight type 2 diabetes genes is associated with reduced first-phase glucose-stimulated insulin secretion during hyperglycemic clamps. Diabetes 59, 287–292 (2010).
The Diabetes Control and Complications Trial Research Group. Clustering of long-term complications in families with diabetes in the diabetes control and complications trial. Diabetes 46, 1829–1839 (1997).
Abbott, C. A. et al. The North-West Diabetes Foot Care Study: Incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet. Med. 19, 377–384 (2002).
Lamont, P., Franklyn, K., Rayman, G. & Boulton, A. J. Update on the diabetic foot 2012: The 14th biennial Malvern Diabetic Foot Conference, May 9–11, 2012. Int. J. Low Extrem. Wounds. 12, 71–75 (2013).
Meng, W. et al. A genome-wide association study suggests that MAPK14 is associated with diabetic foot ulcers. Br. J. Dermatol. 177, 1664–1670 (2017).
Mrozikiewicz-Rakowska, B. et al. Selected RANKL/RANK/OPG system genetic variants in diabetic foot patients. J. Diabetes Metab. Disord. 17, 287–296 (2018).
Su, N. et al. Association of MCP-1 rs1024611 polymorphism with diabetic foot ulcers. Medicine 97, e11232 (2018).
Li, X., Lu, Y. & Wei, P. Association between VEGF genetic variants and diabetic foot ulcer in Chinese Han population: A case-control study. Medicine 97, e10672 (2018).
Erdogan, M. et al. The relationship of the endothelial nitric oxide synthase (eNOS) and vascular endothelial growth factor (VEGF) gene polymorphism in Turkish type 2 diabetic patients with and without diabetic foot ulcers. Foot 37, 5–10 (2018).
Viswanathan, V., Dhamodharan, U., Srinivasan, V., Rajaram, R. & Aravindhan, V. Single nucleotide polymorphisms in cytokine/chemokine genes are associated with severe infection, ulcer grade and amputation in diabetic foot ulcer. Int. J. Biol. Macromol. 118, 1995–2000 (2018).
Nehring, P. et al. Osteoprotegerin gene rs2073617 and rs3134069 polymorphisms in type 2 diabetes patients and sexspecific rs2073618 polymorphism as a risk factor for diabetic foot. Pol. Arch. Med. Wewn. 123, 176–182 (2013).
Meigs, J. B., Cupples, L. A. & Wilson, P. W. Parental transmission of type 2 diabetes: The Framingham Offspring Study. Diabetes 49, 2201–2207 (2000).
Kim, D. J. et al. Lack of excess maternal transmission of type 2 diabetes in a Korean population. Diabetes Res. Clin. Pract. 65, 117–124 (2004).
McCarthy, M. et al. Evaluation of the importance of maternal history of diabetes and of mitochondrial variation in the development of NIDDM. Diabet. Med. 13, 420–428 (1996).
Liu, X. L. et al. Analysis on the risk factors of diabetic foot ulcer in diabetic patients of Uyghur nationality and Han nationality in the Xinjiang Uygur Autonomous Region. Zhonghua Shao Shang Za Zhi. 33, 486–490 (2017).
Chellan, G. et al. Foot care practice—The key to prevent diabetic foot ulcers in India. Foot 22, 298–302 (2012).
Boyko, E. J. et al. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care 22, 1036–1042 (1999).
Moon, K. C., Kim, S. B., Han, S. K., Jeong, S. H. & Dhong, E. S. Risk factors for major amputation in hospitalized diabetic patients with forefoot ulcers. Diabetes Res. Clin. Pract. 158, 107905 (2019).
Larsson, L. G., Baum, J. & Mudholkar, G. S. Hypermobility: Features and differential incidence between the sexes. Arthritis Rheum. 30, 1426–1430 (1987).
Cheng, Y. J. et al. Peripheral insensate neuropathy—a tall problem for US adults?. Am. J. Epidemiol. 164, 873–880 (2006).
Hjelm, K., Nyberg, P. & Apelqvist, J. Gender influences beliefs about health and illness in diabetic subjects with severe foot lesions. J. Adv. Nurs. 40, 673–684 (2002).
Moura Neto, A., Zantut-Wittmann, D. E., Fernandes, T. D., Nery, M. & Parisi, M. C. Risk factors for ulceration and amputation in diabetic foot: Study in a cohort of 496 patients. Endocrine 44, 119–124 (2013).
Vinik, A. I., Erbas, T., Park, T. S., Nolan, R. & Pittenger, G. L. Platelet dysfunction in type 2 diabetes. Diabetes Care 24, 1476–1485 (2001).
Ferreiro, J. L., Gomez-Hospital, J. A. & Angiolillo, D. J. Platelet abnormalities in diabetes mellitus. Diab. Vasc. Dis. Res. 7, 251–259 (2010).
Kakouros, N., Rade, J. J., Kourliouros, A. & Resar, J. R. Platelet function in patients with diabetes mellitus: From a theoretical to a practical perspective. Int. J. Endocrinol. 2011, 742719 (2011).
Behroozian, A. & Beckman, J. A. Microvascular disease increases amputation in patients with peripheral artery disease. Arterioscler. Thromb. Vasc. Biol. 40, 534–540 (2020).
Assadamongkol, R. et al. Prevalence, risk factors, and type of organism in fungal foot infection and toenail onychomycosis in Thai diabetic patients. J. Med. Assoc. Thai. 99, 659–664 (2016).
Zou, S. Y. et al. Identifying at-risk foot among hospitalized patients with type 2 diabetes: A cross-sectional study in one Chinese tertiary hospital. Chronic Dis. Transl. Med. 1, 210–216 (2015).
Banik, P. C. et al. Risk of diabetic foot ulcer and its associated factors among Bangladeshi subjects: A multicentric cross-sectional study. BMJ Open. 10, e034058 (2020).
Acknowledgements
The study was conducted based on the support of the National Key R&D Program of China (2018YFC1314002; 2016YFC1305501) and the National Natural Science Foundation of China (81730018). Sincere acknowledgement would be expressed to the help and support of the National Clinical Research Center for Metabolic Diseases Diabetes Center.
Author information
Authors and Affiliations
Contributions
The data were collected by X.X., L.W., Y.X. and the manuscript was written by X.X., L.W., Y.X., Y.H., J.Y., H.Z., M.Y. L.S. was responsible for data integrity and accuracy.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiong, Xf., Wei, L., Xiao, Y. et al. Family history of diabetes is associated with diabetic foot complications in type 2 diabetes. Sci Rep 10, 17056 (2020). https://doi.org/10.1038/s41598-020-74071-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-74071-3
This article is cited by
-
The interaction of perfluoroalkyl acids and a family history of diabetes on arthritis: analyses of 2011–2018 NHANES
BMC Public Health (2024)
-
Large-scale causal analysis of gut microbiota and six common complications of diabetes: a mendelian randomization study
Diabetology & Metabolic Syndrome (2024)
-
A prediction model for worsening diabetic retinopathy after panretinal photocoagulation
Diabetology & Metabolic Syndrome (2022)
-
Interaction analysis of lipid accumulation product and family history of diabetes on impaired fasting glucose and diabetes risk in population with normotension in Eastern China: a community-based cross-sectional survey
Archives of Public Health (2022)
-
Machine learning algorithm to evaluate risk factors of diabetic foot ulcers and its severity
Medical & Biological Engineering & Computing (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.