Abstract
The myocardial contraction fraction (MCF: stroke volume to myocardial volume) is a novel volumetric measure of left ventricular myocardial shortening. The purpose of the present study was to assess whether MCF could predict adverse outcomes for HCM patients. A retrospective cohort study of 438 HCM patients was conducted. The primary and secondary endpoints were all-cause mortality and HCM-related mortality. The association between MCF and endpoints was analysed. During a follow-up period of 1738.2 person-year, 76 patients (17.2%) reached primary endpoint and 50 patients (65.8%) reached secondary endpoint. Both all-cause mortality rate and HCM-related mortality rate decreased across MCF tertiles (24.7% vs. 17.9% vs. 9.5%, P trend = 0.003 for all-cause mortality; 16.4% vs. 9.7% vs. 6.1%, P trend = 0.021 for HCM-related mortality). Patients in the third tertile had a significantly lower risk of developing adverse outcomes than patients in the first tertile: all-cause mortality (adjusted HR: 0.26, 95% CI: 0.12–0.56, P = 0.001), HCM-related mortality (adjusted HR: 0.17, 95% CI: 0.07–0.42, P < 0.001). At 1-, 3-, and 5-year of follow-up, areas under curve were 0.699, 0.643, 0.618 for all-cause mortality and 0.749, 0.661, 0.613 for HCM-related mortality (all P value < 0.001), respectively. In HCM patients, MCF could independently predict all-cause mortality and HCM-related mortality, which should be considered for overall risk assessment in clinical practice.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetically transmitted disease characterized by a broad spectrum of clinical manifestations, varying from asymptomatic and benign clinical course to adverse outcomes1,2,3. Most of the patients are presented with favorable prognosis and live a normal longevity, while for some other patients, HCM progresses along specific disease pathways and leads to mortality, including sudden cardiac death, refractory heart failure and HCM-related stroke4. Several factors have been identified as prognostic factors of adverse outcomes, including age, New York Heart Association (NYHA) class, family history of sudden death (FHSD), syncope, atrial fibrillation, non-sustained ventricular tachycardia, maximal wall thickness (MWT) and obstruction5. However, the clinical outcomes of HCM are still hard to predict due to clinical heterogeneity.
Recently, a novel volumetric index, myocardial contraction fraction (MCF), defined as ratio of stroke volume (SV) to left ventricular myocardial volume (LVMV)6, has been regarded as a useful predictor for cardiovascular disease events and survival in general populations7, patients with aortic stenosis8, patients with cardiac amyloidosis9,10 and patients with non-ischemic dilated cardiomyopathy11. So far, little is known about its predictive capacity for mortality in HCM patients.
Therefore, the purpose of the present study was to investigate whether MCF could predict all-cause mortality, as well as HCM-related mortality in HCM patients.
Methods
Study population
From December 2008 to May 2016, 499 HCM patients were identified in the study at inpatient department of West China Hospital, Sichuan University, a tertiary referral center. Diagnosis was based on the echocardiographic demonstration of an unexplained increase in wall thickness ≥ 15 mm, in the absence of abnormal load conditions12. Forty-one patients were excluded the study because of loss to follow up after the first evaluation. Another 20 patients without MCF values were also excluded from the study, leaving a final sample size of 438 HCM patients. Detailed information about those participants has been reported elsewhere13. Follow-up was conducted by clinical consultations, medical records review and telephone interviews. The study was approved by the Ethics Committee on Medical Research of West China Hospital of Sichuan University, and performed according to the principles of the Declaration of Helsinki. Due to the retrospective nature of the study, informed consent was waived.
Echocardiographic measurement
The whole cohort underwent a standard two-dimensional transthoracic echocardiography (TTE) during baseline visits. All TTE examinations were performed following the recommendations of the American Society of Echocardiography (ASE)-European Association of Echocardiography (EAE)14. left ventricular mass (LVM) was calculated according to the corrected formula of the ASE-EAE as follows: LVM (g) = 0.8 × 1.04 × {[interventricular septal wall thickness (IVST) + posterior wall thickness (PWT) + left ventricular end-diastolic diameter (LVEDD)]3 − LVEDD3} + 0.6. LVMV was acquired by LVM divided by the mean density of myocardium (1.05 g/ml). Left ventricular end-diastolic volume (LVEDV) and left ventricular end-systolic volume (LVESV) were calculated from two-dimensional echo guided M-mode echocardiographic dimensions using the following formula: LVEDV (ml) = 4.5 × (LVEDD)2, LVESV (ml) = 3.72 × (LVESD)215. SV (ml) = LVEDV-LVESV. Ejection fraction (EF%) was calculated as (LVEDV-LVESV)/LVEDV × 100. In the last, MCF = SV/LVMV. Left ventricular diastolic dysfunction (LVDS) was based on echocardiography diagnosis according to the guideline16. End-stage HCM (ESHCM) was defined by an LVEF < 50% on echocardiography during follow-up. The presence of left ventricular outflow tract obstruction was defined as a gradient > 30 mmHg at rest.
Outcomes
The primary and secondary endpoints were all-cause mortality and HCM-related mortality, respectively. HCM-related mortality was comprised of sudden or unexpected death, death resulting from progressive hear failure, death caused by HCM-related stroke, and perioperative death due to ventricular septal myectomy.
Statistical analysis
Continuous variables were expressed as means ± standard deviation (SD) or median (interquartile range) as appropriate. Categorical variables were expressed as frequencies (n) and percentages (%). MCF was categorized into tertiles to evaluate its influence on all-cause mortality and HCM-related mortality, with the lowest tertile (T1) serving as a referent group. Survival curves were presented as Kaplan–Meier curves, and the log-rank test was used for comparison between groups. The association between MCF and all-cause mortality and HCM-related mortality was assessed by univariate and multivariate Cox’s proportional hazard models. Baseline variables that were considered clinically relevant or that showed a univariate relationship with thromboembolism were entered into multivariate cox proportional hazards regression models. The consistency of association between MCF and endpoints in prespecified subgroups was assessed with the use of cox regression with tests for interaction. Receiver operating curve (ROC) as a function of time and the area under curve (AUC)17 was used to illustrate the discriminative ability of MCF for all-cause mortality and HCM-related mortality at follow-up time of 1-, 3-, 5-year. All statistical analyses were performed using Empower (R) (www.empowerstats.com, X&Y solutions, inc. Boston MA), R (https://www.R-project.org) and SPSS (SPSS Inc., Chicago, Illinois, USA). A two-sided P value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics
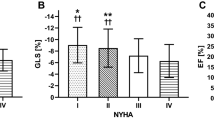
Table 1 shows the baseline characteristics of the sample across MCF tertiles (T1: 3.5% ≤ MCF < 13.9%, T2: 13.9% ≤ MCF < 18.8%, T3:18.8% ≤ MCF < 44.3%). A total of 438 HCM patients was included in the present study. The median age at baseline was 58.0 years old (interquartile range: 46.0–67.0) and 242 patients (55.3%) were male. The average MCF was 16.7 ± 6.4. Prevalence of New York Heart Association (NYHA) III/IV, atrial fibrillation (AF) and ESHCM significantly decreased from T1 to T3. Systolic blood pressure (SBP), left ventricular diameter, EDD, ESV, SV and EF increased significantly across tertiles. In addition, there was a significant tend of decreasing left atria diameter (LA), IVS, LVPW, MWT and LVMV from T1 to T3. Other detailed information about medical histories, medications, clinical procedures and echocardiographic data are shown in Table 1.
Outcomes
During a median follow-up of 3.7 years (range 0.1–9.4) and 1738.2 person-years of observation, 76 patients had all-cause mortality with an incidence rate of 17.4%. There were 50 (65.8%) HCM-related mortality. Detail information is shown in Table 2. The number of primary and secondary endpoint across MCF tertiles is presented in Table 3. Both all-cause mortality rate and HCM-related mortality rate decreased significantly across MCF tertiles (24.7% vs. 17.9% vs. 9.5%, P trend = 0.003 for all-cause mortality; 16.4% vs. 9.7% vs. 6.1%, P trend = 0.021 for HCM-related mortality). A time-to-event analysis also indicated that patients with reduced MCF values had higher risk of all-cause mortality and HCM-related mortality (Fig. 1).
Survival analysis
Univariate Cox’s proportional hazard analysis revealed that patients in the third MCF tertile showed a 66% decrease of all-cause mortality and 67% decrease of HCM-related mortality when compared to that of patients in the first tertile. Other significant predictors of endpoints for HCM patients are shown in Table 2. Among them, baseline SBP and EF were protective factors. Baseline heart rate, AF, NYHA class II/IV, LA, LVPW and ESHCM were risk factors.
Five models were constructed to examine the effect of comorbidity, medication and echocardiographic parameters on the association between MCF and mortality risk. The association remained consistent and stable after adjusting different potential confounders (Table 4). After adjusting age, gender, FHSD, syncope, NYHA class III/IV, MWT and LVOTO in model 5, in comparison of the top tertile versus the bottom tertile of MCF, HRs for all-cause mortality and HCM-related mortality were 0.26 (95% CI: 0.12–0.56, P = 0.001) and 0.17 (95% CI: 0.07–0.42, P < 0.001), respectively. What’s more, no significant observations between MCF and other variables were observed during subgroup analysis (supplementary Table 1). Again, the strength and direction of the associations did not change materially.
Time-dependent AUC
The all-cause mortality rates were 7.1%, 12.1% and 15.8% at 1-, 3-, 5-year of follow-up, respectively. HCM-related mortality rates were 5.0%, 7.8% and 10.5%. Figure 2 depicts time-dependent ROC for MCF associated with endpoints at different follow-up time. At 1-, 3-, and 5-year, the AUCs were 0.699, 0.643 and 0.618 for all-cause mortality and 0.749, 0.661 and 0.613 for HCM-related mortality (all P value < 0.001). The corresponding cut-off value, youden index, sensitivity and specificity of MCF for each outcome at different timepoints are shown in supplementary Table 2.
Discussion
In this relatively large study cohort of HCM patients, MCF was a significant and independent predictor of all-cause mortality and HCM-related mortality. The association was not changed materially after adjusting potential risk factors in multivariate Cox’s proportional hazard analysis or subgroup analysis. However, the discriminative ability showed a decreasing trend along with the extension of follow-up time.
MCF was firstly proposed by King et al. as an index of myocardial shortening which could be able to distinguish pathologic hypertensive hypertrophy and physiological hypertrophy of athletes6. Then a number of studies have begun to examine the relationship between MCF and cardiovascular disease (CVD) events and mortality or survival in different populations of participants. Chuang et al. analyzed data from the Framingham Heart Study cohort and concluded that patients in the lowest-quartile was 7 times more likely to develop a hard CVD event, which was consisted of cardiovascular death, myocardial infarction, stroke or new heart failure, when compared to patients in remaining quartiles7. In another major study cohort, the Multi-Ethnic Study of Atherosclerosis, Abdalla et al. also reported that the lowest MCF quartiles was associated with an increased risk for incident CVD (myocardial infarction, resuscitated cardiac arrest, stroke, coronary heart disease and stroke death) (HR: 2.42, 95%CI: 1.58–3.72)18. In patients with cardiomyopathy, including cardiac amyloidosis and non-ischemic cardiomyopathy, historical studies consistently confirmed the prognostic capacity for adverse outcomes9,10,11. Few data have evaluated the role of MCF played in patients with HCM. As far as we know, only one study ever conducted to fill this knowledge gap. In this study, Shimada et al.revealed that MCF independently predicted the composite endpoint of embolic stroke, heart transplant and cardiac death for HCM patients (HR: 0.5 per 10% increase, 95%CI: 0.28–0.90, P = 0.02)19. However, this study was largely limited by its small sample size (n = 137). The results of our study collaborated with the historical ones and mainly delineated the predictive capacity of MCF for mortality in HCM patients. The strength of results was enhanced by a relatively large number of participants (n = 438). In addition, our study is the first study to evaluate the predictive ability of MCF at different timepoints.
It is noteworthy that MCF values in our study cohort were lower than that of previous study19, which could be explained by the fact that this HCM cohort was enrolled at the inpatient department of a tertial referral center, patients were more exacerbated than general HCM populations. Consequently, the survival rate was apparently lower at certain timepoint when compare to the reported 1-,3-,5-year survival rates of 98.0%, 94.3%,82.2% in a recent heavy-weighted meta-analysis4. The predictive ability of MCF for HCM-related mortality at 1-year of follow-up was quite considerable with AUC as high as 0.75. Unfortunately, there was a decreasing trend with increasing follow-up periods which might be explained by the change of MCF itself and other risk factors and cohorts as time went by. Therefore, a dynamic evaluation based on the change of MCF may improve the predictive ability since echocardiography was a noninvasive, easily accessible routine examination for HCM patients.
Several limitations of the present study should be addressed. Firstly, this is a retrospective study with relatively small sample size and did not include a control group. Secondly, M-mode echocardiography was used for patients in our study, which might lead to LVM underestimation. However, most epidemiological reports use this imaging modality based on its technical feasibility and availability at the time when most studies were performed. So is in our retrospective study. Thirdly, patients in this study were from the inpatient department of a tertiary referral center, who tended to be sicker than the general HCM population with lower MCF values. Therefore, the strength of results may be limited when apply it to the whole HCM patients. Fourthly, it was underpowered to examine different types of cardiovascular endpoints due to small number of events, and thus we did not perform the analysis. Lastly this population was located in Chengdu, China, lack of region diversification and race comparison, the results may not be generalized to other specific patient groups or ethnicities. Large prospective studies are warranted.
Conclusion
In conclusion, our results indicated that reduced MCF was significantly associated with increased risk for all-cause mortality and HCM-related mortality in HCM patients. MCF showed certain discriminative ability at different timepoints of follow-up, which should be considered as a useful clinical tool for mortality risk assessment among HCM patients.
References
Spirito, P. et al. Clinical course and prognosis of hypertrophic cardiomyopathy in an outpatient population. N. Engl. J. Med. 320(12), 749–755 (1989).
Maron, B. J. et al. Clinical course of hypertrophiccardiomyopathy with survival to advanced age. J. Am. Coll. Cardiol. 42(5), 882–888 (2003).
Kubo, T. et al. Patients’ characteristics and clinical course of hypertrophic cardiomyopathy in a regional Japanese Cohort―results from Kochi RYOMA study. Circul. J. CJ-17-0845 (2018)
Maron, B. J. et al. Epidemiology of hypertrophic cardiomyopathy–related death: revisited in a large non–referral-based patient population. Circulation 102(8), 858–864 (2010).
Liu, Q. et al. Survival and prognostic factors in hypertrophic cardiomyopathy: a meta-analysis. Sci. Rep. 7(1), 1–10 (2017).
King, D. L., Coffin, L. E. & Maurer, M. S. Myocardial contraction fraction: a volumetric index of myocardial shortening by freehand three-dimensional echocardiography. J. Am. Coll. Cardiol. 40(2), 325–329 (2002).
Chuang, M. L. et al. Usefulness of the left ventricular myocardial contraction fraction in healthy men and women to predict cardiovascular morbidity and mortality. Am. J. Cardiol. 109(10), 1454–1458 (2012).
Romeo, F. J. et al. Prognostic impact of myocardial contraction fraction in patients undergoing transcatheter aortic valve replacement for aortic stenosis. Cardiovasc. Diagn. Ther. 10(1), 12 (2020).
Rubin, J. et al. Myocardial contraction fraction by M-mode echocardiography is superior to ejection fraction in predicting mortality in transthyretin amyloidosis. J. Cardiac Fai. 24(8), 504–511 (2018).
Tendler, A. et al. The myocardial contraction fraction is superior to ejection fraction in predicting survival in patients with AL cardiac amyloidosis. Amyloid 22(1), 61–66 (2015).
Arenja, N. et al. Diagnostic and prognostic value of long-axis strain and myocardial contraction fraction using standard cardiovascular MR imaging in patients with nonischemic dilated cardiomyopathies. Radiology 283(3), 681–691 (2017).
Authors/Task Force Members. et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 35(39), 2733–2779 (2014).
He, S. et al. External validation of the model of thromboembolic risk in hypertrophic cardiomyopathy patients. Can. J. Cardiol. 35(12), 1800–1806 (2019).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16(3), 233–271 (2015).
de Simone, G. et al. Estimation of left ventricular chamber and stroke volume by limited M-mode echocardiography and validation by two-dimensional and Doppler echocardiography. Am. J. Cardiol. 78(7), 801–807 (1996).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. J. Echocardiogr. 17(12), 1321–1360 (2016).
Kamarudin, A. N., Cox, T. & Kolamunnage-Dona, R. Time-dependent ROC curve analysis in medical research: current methods and applications. BMC Med. Res. Methodol. 17(1), 53 (2017).
Abdalla, M. et al. Association between reduced myocardial contraction fraction and cardiovascular disease outcomes: the multi-ethnic study of atherosclerosis. Int. J. Cardiol. 293, 10–16 (2019).
Shimada, Y. J. et al. Myocardial contraction fraction predicts cardiovascular events in patients with hypertrophic cardiomyopathy and normal ejection fraction. J. Cardiac Fail. 25(6), 450–456 (2019).
Funding
This study was supported by the National Natural Science Foundation of China (grant number: 81600299) and Key research project of Sichuan health planning committee in 2019, Project (NO.19ZD018).
Author information
Authors and Affiliations
Contributions
H.L:designed this study, analyzed data and Drafted the article. Z.Q.-W. and L.M.-Z. prepared figures and tables. X.P.-C. revision of article. S.H: Approval of article .All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, H., Wang, Z., Zhao, L. et al. Myocardial contraction fraction predicts mortality for patients with hypertrophic cardiomyopathy. Sci Rep 10, 17026 (2020). https://doi.org/10.1038/s41598-020-72712-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72712-1
This article is cited by
-
Prognostic value of albumin to fibrinogen ratio for mortality in patients with hypertrophic cardiomyopathy
BMC Cardiovascular Disorders (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.