Abstract
Prone positioning for whole-breast irradiation (WBI) reduces dose to organs at risk, but reduces set-up speed, precision, and comfort. We aimed to improve these problems by placing patients in prone crawl position on a newly developed crawl couch (CrC). A group of 10 right-sided breast cancer patients requiring WBI were randomized in this cross-over trial, comparing the CrC to a standard prone breastboard (BB). Laterolateral (LL), craniocaudal (CC) and anterioposterior (AP) set-up errors were evaluated with cone beam CT. Comfort, preference and set-up time (SUT) were assessed. Forty left and right-sided breast cancer patients served as a validation group. For BB versus CrC, AP, LL and CC mean patient shifts were − 0.8 ± 2.8, 0.2 ± 11.7 and − 0.6 ± 4.4 versus − 0.2 ± 3.3, − 0.8 ± 2.5 and − 1.9 ± 5.7 mm. LL shift spread was reduced significantly. Nine out of 10 patients preferred the CrC. SUT did not differ significantly. The validation group had mean patient shifts of 1.7 ± 2.9 (AP), 0.2 ± 3.6 (LL) and − 0.2 ± 3.3 (CC) mm. Mean SUT in the validation group was 1 min longer (P < 0.05) than the comparative group. Median SUT was 3 min in all groups. The CrC improved precision and comfort compared to BB. Set-up errors compare favourably to other prone-WBI trials and rival supine positioning.
Similar content being viewed by others
Introduction
Breast cancer is the second most frequent cancer in women worldwide1. Early stage patients undergo breast conserving surgery. Additional whole-breast irradiation (WBI) leads to a 15.7% absolute reduction of relapse risk at 10 years and an absolute breast cancer mortality reduction of 3.3% at 15 years2. WBI implicates irradiation of surrounding organs at risk (OAR), which may cause side-effects like pneumonitis, fibrosis, ischemic heart disease, hypothyroidism, skin changes, and radiation-induced cancers3,4,5,6,7.
Intensity-modulated radiotherapy and volumetric-modulated arc therapy made radiation more conformal. Image guided radiotherapy (IGRT) made treatments more accurate and precise, decreasing OAR doses8,9,10. OAR doses are further improved by breath hold techniques11,12, a contralateral breast-holder, or changing the treatment position. Prone positioning minimizes target movement, reducing anterior thoracic expansion during breathing13,14,15. As the breast falls away from the thoracic wall, OARs can be more easily spared16,17. Prone positioning, however, is reported to suffer from reduced set-up precision, increased set-up time and reduced patient comfort14,15,18.
In case of regional nodal irradiation (RNI), prone breastboards often obstruct optimal beam paths. Their placement on top of the treatment couch hinders sagittal positioning of the laser on the target. Therefore, reference lines on the patient’s back are used, causing latero-lateral inaccuracies. This is aggravated by a tilted wedge in many breastboards, causing some patients to slide down from it. Furthermore, many patients have difficulties raising their arms above the head after surgery. We developed a support couch that addresses the problems of inaccuracy, discomfort and restricted beam access in classic prone breastboards. We named it the prone crawl breast couch (further called crawl couch), because patients take a position resembling a phase of prone crawl swimming19. Dosimetric studies show reduced OAR doses with the crawl couch over supine setup in WBI + RNI20,21. However, there are no data available on set-up precision and comfort of the crawl couch.
In this study, we compare the crawl couch to our standard breastboard in a group of 10 patients refered for WBI, with regard to set-up precision, set-up time, and patient comfort. A second cohort of forty patients served as a validation group. The novelty of this trial is the use of the crawl couch, specifically designed to improve upon the limitations of “standard” prone positioning.
Materials and methods
Study design
Ten patients referred for hypofractionated WBI in 15 fractions were randomized 1:1 to start radiotherapy on either of the two available support devices. After 8 fractions, they crossed over the other device, serving as their own control. We further refer to this group as the comparative group. The trial was approved by the Ghent Universitary Hospital Ethics Board (reference number: EC-UZ-2014/1250, Belgian Registration Number: B670201422932). A second group of 40 patients was treated solely on the crawl couch and consented for their data to be used as internal validation of the results for the first patient group (reference number: EC-UZ-2016/0351, Belgian Registration Number: B670201628048). This group is further referred to as the validation group. All patients in our research voluntarily joined the study and informed consent was obtained from all participants before inclusion. The research was performed in accordance with relevant guidelines and regulations.
Support devices
Currently, in WBI-only treatments, we use a modified AIO prone breastboard (Orfit, Wijnegem, Belgium), described previously22,23 and further called standard breastboard. The crawl couch was designed for RNI in prone position. The contralateral arm is extended forward on an arm support, and the ipsilateral arm is held along the torso, leaving the ipsilateral shoulder and clavicular region unsupported by the couch. Stability is provided by the anhedral slope design of the contralateral arm support, an ipsilateral lateral pelvic support and an ipsilateral arm support blade along the patient’s waist and thoracic wall, which supports the arm up to the region below the axilla24. The caudal part of the crawl couch—supporting the patient’s legs hips and waist—rests on the treatment couch and the cranial part—supporting the torso breast and head—extends into the air, allowing sagittal projection of a floor laser on the treated breast19 (Fig. 1).
Patient set-up on a crawl couch prototype. (A) The prototype allows unobstructed anterior access to the ipsilateral lymphatic drainage areas. The projection of a red floor laser is seen along the sagital plane. (B) The contralateral side resembles current prone breastboards, overhanging design allows projection of a floor laser to decrease lateral positioning errors, while the patient is wearing a custom made unilateral bra, which retracts the contralateral breast away from the target volume.
Patient groups
Ten consecutive breast cancer patients referred for WBI were included in the comparative group. To avoid two extra CT-scans for breathhold planning (one on each treatment device), we allowed only right-sided WBI breast cancer patients for the control group. For the validation group of 40 patients, left- and right-sided breast cancers were included, as they were only treated using the crawl couch. For all patients, WBI was planned with a median prescription dose of 40.05 Gy in 15 fractions. Left-sided breast cancer patients were treated using a breath hold technique only if the planning constraints to the heart were not met (mean heart dose < 2 Gy and D02 < 10 Gy) in free breathing and were superior using the breath hold technique.
Simulation
In the comparative group, patients underwent a CT-simulation on both support devices on the same day. Slice thickness was 5 mm. The contralateral breast was pulled laterally, by means of a unilateral bra [Tricolast, Deinze, Belgium]. A radio-opaque wire was placed around the ipsilateral breast. The isocenter was located on the acquired images and projected onto the patient using a laser co-ordinate system. The projected lines were marked on the patient’s skin with semi-permanent markers using different colours for each device. As the patient is lying on a solid blade couch, there is no floor laser projection available directly on the treated breast. This is an issue for the laterolateral positioning line, which is marked on the back of the patient. At the first treatment fraction, the patient is positioned using this laterolateral skin marking, and after positioning and CBCT correction, skin markings are added, using additional lasers. We use a floor laser for the crawl couch, and lasers at |40°| angles to the sagittal plane for the standard breastboard22. In this way, both devices had the same set-up protocol on our simulator. The validation group only underwent simulation using the crawl couch. All left-sided breast cancer patients underwent CT simulation including breathhold CT and free breathing CT. The free breathing CT was used for marking the isocenter in all patients.
Endpoints
The primary endpoint was patient positioning accuracy & precision. Secondary endpoints were set-up time and patient comfort.
Positioning was assessed by daily CBCT after positioning on skin markings. Online matching of CBCT and simulation CT images allowed evaluation of position shifts in 3 axes: laterolateral (LL), craniocaudal (CC) and anteroposterior (AP). These were used to compare set-up accuracy & precision on the two support devices. Our treatment couches do not permit rotational corrections. Because additional set-up lines are marked on the patient at the time of the first fraction, couch shifts and set-up time at the first fraction of both devices were not used in the analysis.
We calculated systematic and random errors in accordance with van Herk25. The group systematic error, M, is defined as the mean of the mean individual patient shifts. Σ, defined as the standard deviation (SD) from M, is an estimator for the SD of group systematic errors. Finally, σ, an estimator of the SD of random error, is defined by the root mean square (RMS) of SD from the mean individual patient shift. We report these parameters and an estimated required planning target volume (PTV) margin using his formula, \(2.5\sum + 0.7\sigma \) to compare our results to historical results.
Positioning time was registered in minutes by a radiotherapy technician (RTT) from the moment the patient climbed the treatment couch, until the CBCT was initiated. There was about 22% missing data because the treating RTT forgot to register either the start or stop time. Therefore, a Mann–Whitney U test was used to compare mean positioning time per device in the comparative group and also between the validation group and the comparative crawl group. We compared the means per patient per device using a paired Wilcoxon signed rank test in the comparative group.
Comfort and preference were assessed using patient reported outcome measures questionnaires (PROMs). Patients were asked 3 yes/no questions: if there were difficulties taking the treatment position, if they felt like they were sliding of the wedge, and if they felt tense while maintaining position. This was complemented with a visual analogue scale for pressure, tension, or pain sensation on multiple localisations (see supplementary information Figs. 1 and 2). PROMs were filled in at simulation and after each of the 2 treatment parts. After completing treatment, patients were asked which device they preferred. The validation group reported their PROMs after simulation, day 5 of treatment and at the end of treatment.
Data were analysed using R 3.3.2 with paired comparisons where possible. Tests were performed 2-sided with an α-value of < 0.05. One patient did not return a questionnaire form after the first treatment part, and one patient failed to answer the yes/no question asking about tension. In both cases the questions pertained to the crawl couch and were categorized as missing.
Results
Set-up accuracy & precision
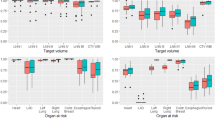
Table 1 shows descriptive statistics for the comparative group on the 3 axes. Figure 2 shows the shifts along the 3 axes acquired during the treatment per patient in this group. A paired T-test was performed to compare M for positioning data along the same axis on both support devices, and an F-test was performed for difference between variances of patient means for the 3 axes on both support devices. There was no significant difference between mean shifts on the 2 support devices, but the SD was significantly smaller for the LL axis for the crawl couch compared to the standard breastboard (P < 0.001). No significant differences in SD for the other axes were observed. The RMS as an estimator for SD of random error is based on individual patient SDs. The individual patient SDs, when treated as a separate measurement, had a statistically significant different mean (P < 0.05) and SD (P < 0.001) along the LL axis only, with smaller values for the crawl couch compared to the standard breastboard.
Distribution of individual patient shifts registered on 3 axes for the standard and crawl prone positioning devices. Shifts were extracted by positioning patients on reference lines and noting the shift needed to match the CBCT to the simulation CT as closely as possible. Each patient is represented by a separate colour.
Shifts along each axis for all crawl groups are reported in Table 2 while Table 3 shows the data for each patient and shows the subgroups for left versus right-sided breast cancer. The sign of the LL shift was inverted in left-sided patients, mirroring them to match the right-sided patients. When comparing crawl comparative and crawl validation positioning using an unpaired T-test, there was a significant difference in M for the AP shifts (p < 0.001), but not for CC and LL directions. F-test was significant for the LL and CC axis, but not for the AP axis. Individual patient SDs, treated as a separate measurement, had a statistically significant different mean (P < 0.01) along the LL axis only, with larger values for the validation group, but no significant difference in SD per axis between study groups.
Time registration
Table 4 shows measurement data for both treatment devices. In the comparative group, there was no significant difference in set-up time between the two support types (P > 0.717) using the unpaired Mann–Whitney U test. The paired Wilcoxon signed rank test on the means per patient also showed no significant difference in set-up time between the two devices (P > 0.952). The mean positioning time on the crawl couch was significantly longer for the validation group compared to the comparative group (P < 0.001). However, the median positioning time is the same between all groups (3 min).
Pressure/tension points and pain
We asked to evaluate pressure/tension and pain on several anatomical points, scored on the continuous visual-analogue scale provided in supplementary information Figs. 1 and 2. This scale was separated in pressure/tension scores (Fig. 3) and pain scores (Fig. 4). This division was made because, while some pressure/tension is acceptable, we mainly aimed to visualise the effect of using either support device on pain sensation. This means that these figures can only be correctly interpreted side by side: a decreased score on Fig. 4 (pain) can result in an increased score on Fig. 3 (pressure/tension), because these data originate from the same visual-analogue scale. Figure 5 shows the scores for the validation group at each measurement point.
Pressure/tension scores for the 11 different localizations as indicated by individual patients in the comparative group, to be viewed side by side with Fig. 4. Different circle sizes indicated different pressure/tension scores per patient. Overlapping circles intensify the circle colour. (A) Standard prone breastboard at simulation, (B) crawl couch at simulation, (C) standard prone breastboard after treatment (D) crawl couch after treatment.
Pain scores for the 11 different localizations as indicated by individual patients in the comparative group, to be viewed side by side with Fig. 3. Different circle sizes indicated different pain scores per patient. Overlapping circles intensify the circle colour. (A) Standard prone breastboard at simulation, (B) crawl couch at simulation, (C) standard prone breastboard after treatment, (D) crawl couch after treatment.
Comfort and preference
A crosstable showing the response for the comparative to the yes/no questions per device is shown in Table 5. At simulation, only one patient felt tense on the crawl couch, and she experienced the same on the standard breastboard. After treatment, none of the patients who answered the questions and returned the form experienced any pain or pressure, sliding sensation or tension on the crawl couch, whereas, on the standard breastboard, this was the case for some patients. When asked to indicate which support device they preferred, 9 out of 10 patients preferred the crawl couch. Figure 5 shows the responses to the yes/no questions for the validation group at each measurement point.
Discussion
This study was performed to evaluate the impact of the crawl couch on positioning accuracy & precision, timing and patient comfort in breast irradiation. First of all we discuss the comparative study group. As to accuracy of treatment, the difference in mean shifts (M) between both groups was not significant for any axis, but the crawl couch improved LL positioning, in terms of inter-patient (∑) as well as intra-patient variability (σ), improving precision.
This improvement in LL precision comes as a result of the design of the crawl couch: the armrest prevents the patient from sliding down the wedge, and the open design allows sagittal laser beam projection on the target tissue. This allows for smaller PTV margins, reduction of the dose to OARs, and it reduces the need for daily CBCT to evaluate random errors.
Image guided radiotherapy (IGRT) allows daily imaging, with possibilities for gating or tracking. These improvements in treatment techniques allow more accurate visualisation of the target, while treatment machines are increasingly capable of high precision and real-time treatment adaptation. Therefore, the continued use of Van Herk’s formula25 to calculate clinical PTV margins is becoming an anachronism. It is our opinion that in the era of IGRT, Van Herk’s formula and its parameters will mainly be used to compare positioning results to historical data, which we will do below.
We used van Herk’s parameters and formula to estimate the required margins along the 3 axes (Tables 1, 2, 3). We estimated a suggested anisotropic PTV margin for the whole group (50 patients) of 1.0, 1.1 and 1.2 cm for the AP, LL and CC axes, respectively. Our results are not always directly comparable to other published data, because margin recipes differ, or the recipe is not mentioned.
First, we compare our results to other reported results for prone WBI positioning. We updated the overview as cited by Mulliez et al.18 (Table 6), and calculated the margins according to the (\(2.5\sum + 0.7\sigma )\) formula where possible, so as to make direct comparison as valid as possible. Comparing our margins to these recalculated margins, we see similar results as Mulliez et al.18, except for the LL margin, which was substantially reduced using the crawl couch. The standard prone position did show a larger LL error in our sample. Only the group of Varga26 reported vastly superior margin results, but their setup was evaluated with EPID using a single treatment beam as portal. There is an inherent loss of information when only using 2D imaging as verification, and indeed they do not report the errors along each axis separately. Data cited in the publication of Mitchell et al.27 back this up. They state in their manuscript that CBCT catches more errors than the EPID technique and thus will require larger margins. While Joszef et al.28 report slightly superior margins along the LL and CC axis compared to the prone crawl setup, their report only concerns partial breast irradiation, so effects of edema on patient shift might not be as pronounced. In general, our crawl couch results compare favourably to most of the results published for prone radiotherapy13,14,15,18,22,26,27,28,29,30, especially for the AP and LL systematic error distribution defined by M and ∑. Because our random error σ is lower than in these other studies, we can obtain smaller PTV margins of around 1 cm in these directions. However, despite our CC margins being comparable to other studies, they range amongst the wider margins reported. This seems to be caused by a higher ∑ rather than σ, as the latter is among the lowest observed in prone position, but the former is amongst the highest. This higher ∑ could be due to less reproducible shoulder support on the irradiated side, as this position has more possible variation using this new positioning technique. As σ is low, this larger ∑ has more to do with inter-patient rather than intra-patient variation. Because each individual patient’s position will be less variable between fractions, margins could be safely reduced using eNAL-protocols31.
Comparing the validation study group with the crawl comparative group, there was a difference in mean AP shift that was larger in the validation group, but there was no difference between the groups for LL or CC mean shift. This difference in M does not factor into Van Herk’s equation. The most pronounced changes seen for the crawl position in the comparative group, being the LL and CC shifts, were somewhat toned down in the comparison with the validation group. Due to a significantly larger Σ and σ along the LL axis in the validation group, the LL margin became larger, and a significantly smaller ∑ along CC axis in the validation group made the CC margin smaller.
The reason for the decreased CC shift in the validation group might be the learning curve, resulting in more reproducible shoulder positioning between patients. It is unclear why the LL shifts on the crawl couch are larger in the validation group than in the comparative group. Looking at breast cancer laterality in the validation group shows a large difference in LL shifts between left and right-sided breast cancers, to the detriment of the left-sided patients, while right-sided patients confirm the observed data from the comparative group. Again, the difference between the two groups is found in a larger ∑ in the left-sided group, while σ remains comparable between the groups. A possible explanation may be found in the number of simulation CTs.
At simulation, left-sided breast cancer patients received multiple scans (breathhold followed by free breathing) without changing their position between scans. Isocenter lines were then marked based on the free breathing scan, because the breast is assumed not to change position between breathhold and free breathing12. It is possible that the patient shifts position as a result of longer simulation time and multiple table movements during this period. This could result in a discrepancy between imaging and skin demarcation, possibly leading to larger shifts on the treatment device. This also explains why there is no directional preference for these laterolateral shifts between patients (i.e. no large group mean error). In contrast, breathhold does not explain the shifts, as positioning correction is based on a free breathing CBCT which is co-registered with the free breathing simulation CT. Preparation and positioning is therefore the same for breathhold and free breathing patients.
Next, we compare our set-up results for the crawl couch to the results for supine positioning14,15,18,26,29,32,33,34,35,36,37,38,39,40 (Table 6). We found our LL margins were higher than the mean of reported margins in these publications (8.1 mm). However, our margins are still lower than some of the reported margins in supine position. Furthermore, our ∑ is larger than most of the supine series, meaning that there is a higher grade of systematic error. The use of eNAL procedures with adequate image guidance should substantially decrease these errors and therefore the required margins. The AP margin for the crawl couch was higher than the mean margin (8.2 mm) in supine position, but lower than the highest registered supine margin (15.1 mm). The crawl couch’s CC margins are slightly larger than the margins in supine position (12.1 mm using the crawl couch, and 10.4 mm at most in supine position). These results show that our results of prone crawl positioning fall within the range of reported AP and LL margins for supine positioning, with only slightly larger CC margin requirements.
Although van Herk25 specifies that ∑ is actually the standard deviation from M, many authors report ∑ instead of M as systematic error, because it is used in the formula. However, disregarding M is wrong. While M remains small along most axes in the literature overview, the AP axis shows the biggest spread (− 5 mm up to 7.2 mm). This may lead to inaccurate interpretation of the calculated margins. Taking data from Veldeman et al.15 as an example, ∑ = 3.7 mm and σ = 4.3 mm for AP set-up error yields calculated PTV margins of 11.4 mm using van Herk’s formula. But, given M = 7.2 mm, this means that the mean patient shift will fall outside the margins calculated for M = 0 mm for about 13% of the population. Except for Veldeman et al.15, all authors in the overview included left and right-sided tumours, so systematic LL shifts would be corrected by different tumour laterality, resulting in M close to zero. Our study also corrected the sign of the LL shifts for left-sided breast cancer patients so as to not confound the effect on M.
We found no significant difference in set-up time between both support devices in the comparative group. Comparison with a previous report from our center by Veldeman et al.15 shows a shorter time needed for positioning for both support devices in the current study. This shows that a learning curve for implementation of prone positioning exists. However, the validation group had a mean positioning time that was 1 min longer than the comparative group on the crawl couch (3.8 vs. 2.8 min). Because about 22% timing measurements were missing, and the time was noted in minutes by different RTTs, we feel future time registration studies could benefit from automation. But although time differences of less than a minute cannot be detected in this study, the relevance of such differences can be questioned.
There was a near unanimous preference for the crawl couch. Regarding patient comfort, the crawl couch never performed worse than the standard breastboard. When evaluating pain and pressure/tension scores, we showed a substantial difference in favour of the crawl couch for the sternum at the time of simulation. The difference is probably most apparent at that time, because patients spend a longer time on the support device. Figures 3 and 4 illustrate the observed scores for all patients, and allow visual evaluation of the data. While the sample size might not allow to detect any differences perceived by these patients, it is quite clear from the graphs that the crawl couch causes the patient less pain.
While this trial reports on inter-fraction positioning variability on the crawl couch, we did not acquire data allowing us to evaluate the effect of intra-fraction motion and its impact on patient dosimetry. We assumed the intra-fraction motion to be negligible because there is evidence that the breast has no substantial respiration-related movement in prone positioning13,14,15. However, other factors influencing intra-fraction variation and their impact on dosimetry may merit further investigation.
Conclusion
Compared to standard prone positioning, the use of the novel crawl couch improves the positioning precision for prone WBI. The crawl position can almost match set-up errors that are seen in supine positioning without large increases in additional treatment time. In addition, patients generally preferred the crawl couch over a standard prone breastboard and experienced less discomfort, showing lower pain and pressure scores on the crawl couch.
Data availability
Data analysed during this study are available from the corresponding author on reasonable request within the confines of EU General Data Protection Regulations.
References
1Ferlay J et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11, https://globocan.iarc.fr (2013).
Early Breast Cancer Trialists' Collaborative Group et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378, 1707–1716 https://doi.org/10.1016/S0140-6736(11)61629-2 (2011).
Berrington de Gonzalez, A. et al. Second solid cancers after radiotherapy for breast cancer in SEER cancer registries. Br. J. Cancer 102, 220–226. https://doi.org/10.1038/sj.bjc.6605435 (2010).
Darby, S. C., McGale, P., Taylor, C. W. & Peto, R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 6, 557–565. https://doi.org/10.1016/S1470-2045(05)70251-5 (2005).
Darby, S. C. et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 368, 987–998. https://doi.org/10.1056/NEJMoa1209825 (2013).
Marks, L. B. et al. Radiation dose-volume effects in the lung. Int. J. Radiat. Oncol. Biol. Phys. 76, S70–S76. https://doi.org/10.1016/j.ijrobp.2009.06.091 (2010).
Vogelius, I. R., Bentzen, S. M., Maraldo, M. V., Petersen, P. M. & Specht, L. Risk factors for radiation-induced hypothyroidism: a literature-based meta-analysis. Cancer 117, 5250–5260. https://doi.org/10.1002/cncr.26186 (2011).
Taylor, C. W. et al. Cardiac doses from Swedish breast cancer radiotherapy since the 1950s. Radiother. Oncol. 90, 127–135. https://doi.org/10.1016/j.radonc.2008.09.029 (2009).
Viren, T. et al. Tangential volumetric modulated arc therapy technique for left-sided breast cancer radiotherapy. Radiat. Oncol. 10, 79. https://doi.org/10.1186/s13014-015-0392-x (2015).
Mulliez, T. et al. Whole breast radiotherapy in prone and supine position: is there a place for multi-beam IMRT?. Radiat. Oncol. 8, 151. https://doi.org/10.1186/1748-717X-8-151 (2013).
Bartlett, F. R. et al. The UK HeartSpare Study (Stage II): multicentre evaluation of a voluntary breath-hold technique in patients receiving breast radiotherapy. Clin. Oncol. (R. Coll. Radiol.) 29, e51–e56. https://doi.org/10.1016/j.clon.2016.11.005 (2017).
Mulliez, T. et al. Deep inspiration breath hold in the prone position retracts the heart from the breast and internal mammary lymph node region. Radiother. Oncol. 117, 473–476. https://doi.org/10.1016/j.radonc.2015.09.030 (2015).
Morrow, N. V., Stepaniak, C., White, J., Wilson, J. F. & Li, X. A. Intra- and interfractional variations for prone breast irradiation: an indication for image-guided radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 69, 910–917. https://doi.org/10.1016/j.ijrobp.2007.06.056 (2007).
Kirby, A. M. et al. A randomised trial of supine versus prone breast radiotherapy (SuPr study): comparing set-up errors and respiratory motion. Radiother. Oncol. 100, 221–226. https://doi.org/10.1016/j.radonc.2010.11.005 (2011).
Veldeman, L. et al. Alternated prone and supine whole-breast irradiation using IMRT: setup precision, respiratory movement and treatment time. Int. J. Radiat. Oncol. Biol. Phys. 82, 2055–2064. https://doi.org/10.1016/j.ijrobp.2010.10.070 (2012).
Lymberis, S. C. et al. Prospective assessment of optimal individual position (prone versus supine) for breast radiotherapy: volumetric and dosimetric correlations in 100 patients. Int. J. Radiat. Oncol. Biol. Phys. 84, 902–909. https://doi.org/10.1016/j.ijrobp.2012.01.040 (2012).
Formenti, S. C., DeWyngaert, J. K., Jozsef, G. & Goldberg, J. D. Prone vs supine positioning for breast cancer radiotherapy. JAMA 308, 861–863. https://doi.org/10.1001/2012.jama.10759 (2012).
Mulliez, T. et al. Setup accuracy for prone and supine whole breast irradiation. Strahlenther. Onkol. 192, 254–259. https://doi.org/10.1007/s00066-016-0943-6 (2016).
Boute, B. et al. Potential benefits of crawl position for prone radiation therapy in breast cancer. J. Appl. Clin. Med. Phys. 18, 200–205. https://doi.org/10.1002/acm2.12118 (2017).
Speleers, B. A. et al. Comparison of supine or prone crawl photon or proton breast and regional lymph node radiation therapy including the internal mammary chain. Sci. Rep. 9, 4755. https://doi.org/10.1038/s41598-019-41283-1 (2019).
Deseyne, P. et al. Whole breast and regional nodal irradiation in prone versus supine position in left sided breast cancer. Radiat. Oncol. 12, 89. https://doi.org/10.1186/s13014-017-0828-6 (2017).
Veldeman, L. et al. Preliminary results on setup precision of prone-lateral patient positioning for whole breast irradiation. Int. J. Radiat. Oncol. Biol. Phys. 78, 111–118. https://doi.org/10.1016/j.ijrobp.2009.07.1749 (2010).
Mulliez, T. et al. Hypofractionated whole breast irradiation for patients with large breasts: a randomized trial comparing prone and supine positions. Radiother. Oncol. 108, 203–208. https://doi.org/10.1016/j.radonc.2013.08.040 (2013).
Boute, B. et al. The relation between patient discomfort and uncompensated forces of a patient support device for breast and regional lymph node radiotherapy. Appl. Ergon. 72, 48–57. https://doi.org/10.1016/j.apergo.2018.05.002 (2018).
van Herk, M. Errors and margins in radiotherapy. Semin. Radiat. Oncol. 14, 52–64. https://doi.org/10.1053/j.semradonc.2003.10.003 (2004).
Varga, Z. et al. Individual positioning: a comparative study of adjuvant breast radiotherapy in the prone versus supine position. Int. J. Radiat. Oncol. 75, 94–100. https://doi.org/10.1016/j.ijrobp.2008.10.045 (2009).
Mitchell, J., Formenti, S. C. & DeWyngaert, J. K. Interfraction and intrafraction setup variability for prone breast radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 76, 1571–1577. https://doi.org/10.1016/j.ijrobp.2009.07.1683 (2010).
Jozsef, G., DeWyngaert, J. K., Becker, S. J., Lymberis, S. & Formenti, S. C. Prospective study of cone-beam computed tomography image-guided radiotherapy for prone accelerated partial breast irradiation. Int. J. Radiat. Oncol. Biol. Phys. 81, 568–574. https://doi.org/10.1016/j.ijrobp.2010.11.029 (2011).
Ahunbay, E. E. et al. Interfractional target variations for partial breast irradiation. Int. J. Radiat. Oncol. Biol. Phys. 82, 1594–1604. https://doi.org/10.1016/j.ijrobp.2011.01.041 (2012).
Lakosi, F. et al. Feasibility evaluation of prone breast irradiation with the Sagittilt((c)) system including residual-intrafractional error assessment. Cancer Radiother. 20, 776–782. https://doi.org/10.1016/j.canrad.2016.05.014 (2016).
de Boer, H. C. J. & Heijmen, B. J. M. eNAL: an extension of the NAL setup correction protocol for effective use of weekly follow-up measurements. Int. J. Radiat. Oncol. 67, 1586–1595. https://doi.org/10.1016/j.ijrobp.2006.11.050 (2007).
Cai, G. et al. Impact of residual and intrafractional errors on strategy of correction for image-guided accelerated partial breast irradiation. Radiat. Oncol. 5, 96. https://doi.org/10.1186/1748-717X-5-96 (2010).
Donovan, E. M., Castellano, I., Eagle, S. & Harris, E. Clinical implementation of kilovoltage cone beam CT for the verification of sequential and integrated photon boost treatments for breast cancer patients. Br. J. Radiol. 85, e1051–e1057. https://doi.org/10.1259/bjr/28845176 (2012).
Hasan, Y. et al. Comparison of planned versus actual dose delivered for external beam accelerated partial breast irradiation using cone-beam CT and deformable registration. Int. J. Radiat. Oncol. Biol. Phys. 80, 1473–1476. https://doi.org/10.1016/j.ijrobp.2010.04.013 (2011).
Penninkhof, J., Quint, S., Baaijens, M., Heijmen, B. & Dirkx, M. Practical use of the extended no action level (eNAL) correction protocol for breast cancer patients with implanted surgical clips. Int. J. Radiat. Oncol. Biol. Phys. 82, 1031–1037. https://doi.org/10.1016/j.ijrobp.2010.12.059 (2012).
Shah, A. P., Dvorak, T., Curry, M. S., Buchholz, D. J. & Meeks, S. L. Clinical evaluation of interfractional variations for whole breast radiotherapy using 3-dimensional surface imaging. Pract. Radiat. Oncol. 3, 16–25. https://doi.org/10.1016/j.prro.2012.03.002 (2013).
Topolnjak, R. et al. Image-guided radiotherapy for breast cancer patients: surgical clips as surrogate for breast excision cavity. Int. J. Radiat. Oncol. Biol. Phys. 81, e187–e195. https://doi.org/10.1016/j.ijrobp.2010.12.027 (2011).
van Mourik, A. et al. Effects of setup errors and shape changes on breast radiotherapy. Int. J. Radiat. Oncol. 79, 1557–1564. https://doi.org/10.1016/j.ijrobp.2010.07.032 (2011).
White, E. A. et al. Cone beam computed tomography guidance for setup of patients receiving accelerated partial breast irradiation. Int. J. Radiat. Oncol. 68, 547–554. https://doi.org/10.1016/j.ijrobp.2007.01.048 (2007).
Cravo Sa, A. et al. Radiotherapy setup displacements in breast cancer patients: 3D surface imaging experience. Rep. Pract. Oncol. Radiother. 23, 61–67. https://doi.org/10.1016/j.rpor.2017.12.007 (2018).
Acknowledgements
This research was supported by Cancer Plan Action 29 by the Federal Public Service of Health, Food Chain Safety and Environment, Belgium, a Career Catalyst Grant from Susan G. Komen® (Grant 377841), and a Foundation against Cancer grant (FAF-C/2016/854. Prototype research was funded by StarTT 241 grant of the Industrial Research Fund, Ghent University. Bert Boute is recipient of a research grant Emmanuel van der Schueren of Kom op tegen Kanker. Liv Veldeman holds a Clinical Mandate of Kom op tegen Kanker.
Author information
Authors and Affiliations
Contributions
P.D. wrote the main manuscript. SB made the treatment plans for this trial. B.S., B.B., W.D.N., V.L., J.D. and M.S. were involved in the development of the crawl couch for this trial. G.P., A.V.G., L.P., H.V.H., V.V. and M.S. were responsible for data collection from patients. Positioning verification was performed by P.D., C.M., L.V., G.P., A.V.G. Data analysis was performed by D.P. Figures were designed by P.D. and L.V. and made by P.D., using drawings from B.B. for Figs. 3 and 4. Questionnaires were designed by C.M., L.V., H.D. and B.B. All authors contributed to the manuscript and agree with its current form.
Corresponding author
Ethics declarations
Competing interests
Ghent University is the applicant of the patent entitled Radiotherapy Board and Couch [WO2015144654A1] filed on 25.03.2014. Inventors are Wilfried De Neve, Bruno Speleers, Bert Boute and Liv Veldeman. Status of the patent: pending. The patent applies to the Prone Crawl Breast Couch used in this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deseyne, P., Speleers, B., De Neve, W. et al. Crawl positioning improves set-up precision and patient comfort in prone whole breast irradiation. Sci Rep 10, 16376 (2020). https://doi.org/10.1038/s41598-020-72702-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72702-3
This article is cited by
-
Prone versus supine free-breathing for right-sided whole breast radiotherapy
Scientific Reports (2022)
-
Effects of deep inspiration breath hold on prone photon or proton irradiation of breast and regional lymph nodes
Scientific Reports (2021)
-
A comparative study on hypofractionated whole-breast irradiation with sequential or simultaneous integrated boost on different positions after breast-conserving surgery
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.