Abstract
Identification of people with diabetes and chronic kidney disease at high-risk of early mortality is a priority to guide intensification of therapy. We aimed to investigate the complementary prognostic value of baseline urine albumin-to-creatinine ratio (uACR) and plasma soluble tumour necrosis factor receptor-1 (sTNFR1) with respect to early mortality and renal functional decline in a population with type 2 diabetes and advanced chronic kidney disease. We measured plasma sTNFR1 in people with type 2 diabetes (HbA1c ≥ 48 mmol/mol) at 2 hospital sites in Dublin between October 15th, 2014 and July 17th, 2015. In a subgroup of patients with advanced chronic kidney disease at baseline (estimated glomerular filtration rate (eGFR) ≤ 60 mL/min/BSA) (n = 118), we collected clinical and longitudinal laboratory data to investigate relationships between sTNFR1 and renal and mortality endpoints by multivariable linear mixed-effects models and Cox proportional hazards regression models. The cohort was 64% male and 97% Caucasian. Mean age was 74 years, with a median type 2 diabetes duration of 16 years. Mean CKD-EPI eGFR was 42 mL/min/BSA and median [IQR] uACR was 3 [11] mg/mmol. Twenty-three (39%) people in quartiles 3 and 4 for plasma sTNFR1 died over 4-year follow-up. After adjustment for clinical variables, annual CKD-EPI eGFR decreased by − 0.56 mL/min/BSA/year for each logarithm unit increase in baseline uACR, corresponding to an annual loss of renal function of 3% per year. Furthermore, elevated uACR, but not sTNFR1, increased the risk of ≥ 40% decline in CKD-EPI eGFR (HR 1.5, p = 0.001) and doubling of serum creatinine (HR 2.0, p < 0.001). Plasma sTNFR1 did not predict a more negative trajectory in eGFR slope. However, for those people in quartiles 3 and 4 for plasma sTNFR1, an increased risk of incident mortality was detected (HR 4.9, p = 0.02). No such association was detected for uACR. In this elderly cohort of patients with type 2 diabetes and chronic kidney disease, sTNFR1 predicted short-to-medium term mortality risk but not risk of progressive renal functional decline. In contrast, parallel assessment of uACR predicted renal functional decline but not mortality, highlighting the complementary prognostic information provided by both parameters.
Similar content being viewed by others
Background
Diabetes is a major modifiable risk factor for cardiovascular disease and all-cause mortality, with the majority of excess mortality attributable to diabetes occurring in those with kidney disease1. Diabetes was the primary cause of end-stage kidney disease (ESKD) in 38.6% of the United States ESKD population in 20172. Over the past decade, new type 2 diabetes therapies including glucagon-like peptide-1 receptor analogues (GLP1RAs) and sodium-glucose co-transporter-2 inhibitors (SGLT2is) have been demonstrated to exert both cardioprotective and renoprotective effects3,4. Enhanced integration of diabetes and nephrology care, including earlier referral to nephrology services, can improve renal outcomes for people with diabetes and chronic kidney disease (CKD)5. Intentional weight loss strategies, including metabolic surgery, may also reduce the burden of cardiovascular disease and slow renal functional decline in people with type 2 diabetes and CKD6,7,8. Given the range of new and efficacious options for the treatment of diabetes and its complications, identifying subgroups at the highest risk of rapid renal functional decline and/or death will help clinicians to appropriately stratify intensification of therapy.
Plasma soluble tumour necrosis factor receptor-1 (sTNFR1/CD120a) is a circulating protein reflective of systemic inflammation and which is increased in diabetic kidney disease (DKD)9,10,11. Plasma sTNFR1 positively correlates with podocyte foot process effacement and predicts accelerated renal functional decline, ESKD, and increased cardiovascular and all-cause mortality risk in people with diabetes12,13,14,15,16,17,18. The extent to which the prognostic value of plasma sTNFR1 for renal and mortality outcomes extends to elderly people with type 2 diabetes and well advanced CKD remains to be defined. In the present study, we investigated the independent relationships between sTNFR1 and both all-cause mortality and accelerated renal functional decline and ESKD. We report on both individual and composite endpoints in this regard, in a population enriched for such events (elderly population with longstanding type 2 diabetes and CKD stage 3 or greater).
Methods
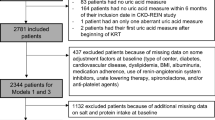
Study cohort
Permission was obtained from St Vincent’s Healthcare Group, Dublin, Ireland for two subsequent prospective clinical audits (reference numbers 2014/1103 and 2019/2324) evaluating reporting practice on biochemical risk factors for microvascular and macrovascular disease in people with diabetes (HbA1c, lipid profile, eGFR, and albuminuria). Contemporaneous to establishment of the audit we instigated measurement of sTNFR1 as part of routine care on clinical grounds in people with diabetes during 2014 and 2015 (suboptimal glycaemic control as defined by HbA1c ≥ 48 mmol/mol). We previously reported cross-sectional associations between plasma sTNFR1 and renal injury in this cohort19. Herein we report on the ability of plasma sTNFR1 to predict mortality and renal endpoints at follow-up in a subgroup of 118 people with established type 2 diabetes and CKD (baseline Chronic Kidney Disease-Epidemiology Collaboration (CKD-EPI) eGFR ≤ 60 mL/min/BSA). Individuals with type 1 diabetes or active malignancy (save for non-melanoma skin cancers) at study enrolment were excluded. The performance of sTNFR1 as a predictor of both mortality and renal end-points was compared and contrasted to that of the routine clinical measure of urinary albumin-to-creatinine ratio (uACR). People with ESKD on renal replacement therapy or with a prior kidney transplant were excluded.
Clinical information
Plasma sTNFR1 was routinely measured between October 15th, 2014 and July 17th, 2015. Longitudinal clinical and laboratory data were obtained from October 15th, 2014 to the end of follow-up on August 31st, 2019. Clinical information (demographics, anthropometry, smoking status, type 2 diabetes duration, blood pressure, diabetes complications, comorbidities, and medication usage) was extracted for each participant from an electronic health record for people with diabetes (TYMAX), as well as from hospital discharge and outpatient records entered into medical charts. Clinical indices were assigned to a specific date. If the exact date of commencement/onset was not available (eg, prescription of non-diabetes medications), the indices were recorded as being either present or absent before the end of longitudinal follow-up on August 31st, 2019.
Biochemical measures
As previously described, sTNFR1 was measured in tenfold diluted plasma samples using the EKF Diagnostics Human sTNFR1 ELISA assay (Cat# EIA—BIO94; EKF Diagnostics Ltd., Cardiff, UK)19. Assay run validity was established based on pass/fail criteria for technical duplicates for low (290 pg/ml) and high (2834 pg/ml) control test concentrations resulting in an overall inter-assay coefficient of variation of 6%19.
All recorded clinical biochemistry tests were analysed via routine clinical biochemistry services at St Vincent’s University Hospital, Dublin. Glycated hemoglobin (HbA1c) was measured by high-performance liquid chromatography (A. Menarini Diagnostics HA-8180 V). Creatinine and albumin were measured on a Roche/Hitachi Cobas c502 modular auto-analyser. The creatinine assay changed from the Jaffe method to an enzymatic assay in January 2016 (both assays were IDMS traceable). Longitudinal laboratory data was manually abstracted from the hospital laboratory information systems.
CKD-EPI eGFR was calculated from serum creatinine using standard formulae and expressed as mL/min/body surface area (BSA)20,21. Only patients with ≥ 3 eGFR determinations over ≥ 1 year were included in analyses of longitudinal renal functional data. Sensitivity analyses were also performed in which only individuals with ≥ 3 eGFR determinations over ≥ 2 years were included in regression models of renal outcomes. Serum creatinine values subsequent to renal replacement therapy initiation were excluded. Annual slopes of CKD-EPI eGFR were calculated by linear regression of eGFR over time in years. Determination of mortality, renal (≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, need for renal replacement therapy), and composite endpoints was performed manually for each patient on a case-by-case basis. Cause of death was categorised as cardiovascular, neoplastic, or infectious based on the primary aetiology. Time to event was recorded for each relevant endpoint reached.
Statistical analyses
RStudio version 3.6.1 was used for analysis. Baseline characteristics at study enrolment and clinical characteristics of the cohort during follow-up (renal and mortality endpoints) were summarised by descriptive statistics. Categorical variables are presented as frequencies and percentages, and were compared across plasma sTNFR1 quartiles using χ2 tests. Continuous variables with normal and skewed distributions are presented as mean ± SD and median [interquartile range], respectively. One-way between-groups ANOVAs and Kruskal–Wallis tests were used to assess for differences across plasma sTNFR1 quartiles in continuous variables with normal and skewed distributions, respectively. P < 0.05 was considered statistically significant.
Diabetes duration, urine albumin-to-creatinine ratio (uACR), and plasma sTNFR1 were log-transformed for regression analyses due to non-Gaussian distributions. Univariate relationships between uACR and sTNFR1 with ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, and mortality were investigated using logistic regression. Multivariable Cox proportional hazards and logistic regression models were created to further investigate relationships between uACR, and sTNFR1 with renal endpoints and mortality. Two models were constructed for each endpoint: firstly, a clinical model adjusting for conventional risk factors for renal functional decline including age, gender, diabetes duration, systolic blood pressure, HbA1c, CKD-EPI eGFR, and uACR; and secondly a clinical + sTNFR1 model incorporating the aforementioned variables and plasma sTNFR1. Cox models were constructed using the R package survival22; unadjusted (Kaplan–Meier) and adjusted survival curves were plotted using the R package survminer according to sTNFR1 quartiles23. Comparisons between sTNFR1 quartiles on the Kaplan–Meier plot were made using the log-rank test. We tested each Cox proportional hazards model for proportionality assumptions using Schoenfeld residuals.
Cox model results are presented as the hazard ratio (HR), 95% confidence interval (CI), and p-value. Logistic regression model results are presented as the odds ratio (OR), 95% CI, and p-value. Comparisons of model adequacy (clinical model versus clinical + sTNFR1 model) were assessed for Cox and logistic regression models using likelihood ratio χ2 tests. We used the competing risk model of Fine and Gray to estimate the subdistribution HRs for ≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine while accounting for the competing risk of all-cause mortality. The function crr from the R package cmprsk was used to construct Fine-Gray models24. Plots of Schoenfeld residuals versus time failure for each term in the models were used to examine the proportional hazard sub-distribution assumption. Cumulative incidence of events of interest (≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine) and the competing risk of death were calculated using the cuminc function in the R package cmprsk24. Cumulative incidence plots were generated using ggcompetingrisks from the R package survminer23.
Linear mixed-effects models were constructed to investigate relationships between uACR and sTNFR1 with annual changes in CKD-EPI eGFR. Separate models were fitted for CKD-EPI eGFR and log-transformed CKD-EPI eGFR. Similarly, a clinical model was constructed that adjusted for the same clinical fixed effects as the aforementioned Cox proportional hazards and logistic regression models, and a clinical + sTNFR1 model which was additionally adjusted for plasma sTNFR1. All linear mixed-effects models incorporated subject-specific random intercepts and slopes for the duration of renal functional follow-up. Models fitted to the absolute eGFR values determine yearly changes in renal function in native units (mL/min/BSA/year), whereas models fitted using log-transformed eGFR estimate annual percentage changes in renal function. Comparisons of model adequacy (clinical model versus clinical + sTNFR1 model) were assessed for linear mixed-effects models using likelihood ratio χ2 tests. The function lmer (from the R package lmerTest) was used to fit and test the models25. No serious violations of logistic regression or linear mixed-effects models was found on examination of the distribution of residuals.
Ethics approval and consent to participate
The study was approved by the clinical audit committee at St. Vincent’s Healthcare Group, Dublin, Ireland (reference numbers 2014/1103 and 2019/2324). Under clinical audit guidelines, informed consent from individual participants was not obtained but all data was handled as per General Data Protection Regulation guidelines (EU), 2016/679. The need for informed consent was waived by the St. Vincent’s Healthcare Group research ethics committee. All procedures performed were in accordance with the ethical standards of the institutional audit committee and with the 1964 Helsinki declaration and its later amendments.
Results
Baseline characteristics
Table 1 presents baseline characteristics of the study cohort (n = 118) according to sTNFR1 quartile (n = 29–30 per quartile). The study population had a mean age of 74 years, and predominantly consisted of Caucasian subjects with longstanding type 2 diabetes. The study population had advanced CKD at baseline (mean CKD-EPI eGFR 41.7 ± 11.4 mL/min/BSA), with baseline renal function steadily declining from quartile 1 to quartile 4 of sTNFR1. Baseline albuminuria was higher and glycaemic control worsened in those people in quartile 4 for plasma sTNFR1.
Over 15% of the study population had coronary artery disease, while 50% had diabetic retinopathy. There were no significant differences in the presence of macrovascular or non-renal microvascular complications of diabetes across the sTNFR1 quartiles. Over 70% of the study cohort were treated with either an angiotensin-converting enzyme-inhibitor or angiotensin-II receptor blocker, and most people were on at least 2 antihypertensives. Usage of GLP1RAs and SGLT2is was low across all quartiles.
Incidence of renal and mortality endpoints
Mean duration of renal functional follow-up was 3.5 ± 1.2 years, with each participant having a median of 14 eGFR determinations (Table 2). The median rate of annual decline in CKD-EPI eGFR was − 2.0 mL/min/BSA/year for the study cohort. Decline of CKD-EPI eGFR ≥ 40% trended to occur more frequently in people in sTNFR1 quartile 4 during follow-up, although this did not reach statistical significance (p = 0.06). Twenty-eight people (23.7% of the study cohort) died during follow-up. There was a linear increase in mortality rates from quartile 1 to 4 during follow-up (p < 0.001). Causes of death in our study cohort included n = 13 (46.4%) due to cardiovascular disease, n = 6 (21.4%) due to cancer, n = 5 (17.9%) due to infection, with cause of death missing in n = 4 (14.3%) cases. Over 50% of people in sTNFR1 quartile 4 died during follow-up. Consequently, the incidence of composite renal and mortality endpoints increased from quartile 1 to quartile 4 during follow-up, although this was mostly driven by high mortality rates in sTNFR1 quartiles 3–4 rather than a higher rate of interim renal endpoints.
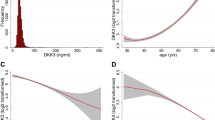
Univariate relationships of baseline uACR and sTNFR1 with renal and mortality endpoints
uACR strongly associated with ≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine by univariate binary logistic regression. Similarly, baseline uACR associated with the development of ESKD requiring renal replacement therapy during follow-up (p = 0.005), but more modestly predicted incident mortality (p = 0.05). Conversely, baseline sTNFR1 associated with death (p < 0.001) and the need for renal replacement therapy (p = 0.02), but not interim renal endpoints including ≥ 40% decline in CKD-EPI eGFR (p = 0.38) and doubling of serum creatinine (p = 0.65). Figure 1 presents univariate relationships of uACR and sTNFR1 with ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, and death, highlighting that uACR strongly predicted interim renal endpoints while sTNFR1 strongly predicted incident mortality. Conversely, baseline uACR weakly predicted incident mortality but sTNFR1 did not predict interim renal endpoints. Figure 2 presents an unadjusted Kaplan–Meier survival plot for the study cohort stratified by sTNFR1 quartile, demonstrating that there is an early and sustained increased incidence of death in sTNFR1 quartile 4 (log-rank p < 0.0001).
Univariate associations between uACR and plasma sTNFR1 with ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, and death. A: ≥ 40% decline in CKD-EPI eGFR with uACR; B: ≥ 40% decline in CKD-EPI eGFR with plasma sTNFR1; C: doubling of serum creatinine with uACR; D: doubling of serum creatinine with plasma sTNFR1; E: mortality with uACR; F: mortality with plasma sTNFR1. Individuals who did and did not develop the outcomes of interest are identified as 1 and 0 on the y-axis, respectively. Log-transformation of uACR and plasma sTNFR1 was performed prior to modelling. 95% confidence interval is represented by blue shading surrounding orange regression line of best fit.
Unadjusted Kaplan–Meier survival plot stratified by plasma sTNFR1 quartile over the study period. Number of patients at risk of death and cumulative number of deaths are tabulated by plasma sTNFR1 quartile below the Kaplan–Meier plot. Log-rank p < 0.0001 for survival differences across the plasma sTNFR1 quartiles.
uACR, but not sTNFR1, predicts accelerated renal functional decline (linear mixed-effects models)
Table 3 presents results of linear mixed-effects models of annual absolute and percentage changes in renal function according to baseline HbA1c, uACR and sTNFR1. Only uACR independently predicted subsequent accelerated renal functional decline. After adjusting for sTNFR1, per unit increase in the logarithm of baseline uACR, annual CKD-EPI eGFR decreased by − 0.56 mL/min/BSA/year, which corresponded to an annual loss of kidney function of 3.0% per year. Neither HbA1c nor plasma sTNFR1 independently predicted a more negative eGFR slope trajectory in our study cohort. In a sensitivity analysis of annual changes in CKD-EPI eGFR restricted to those with ≥ 2 years of renal functional follow-up data, baseline uACR remained similarly predictive of subsequent renal functional decline (Supplementary Table 1). Baseline HbA1c and sTNFR1 continued to show no association with subsequent loss of renal function.
sTNFR1 predicts mortality but not interim renal endpoints (multivariable Cox proportional hazards regression and Fine-Gray models)
Table 4 presents results of multivariable Cox proportional hazards regression analyses for mortality, renal, and composite endpoints according to baseline HbA1c, uACR and sTNFR1.
Elevated sTNFR1, but not uACR, increased the risk of incident mortality (HR 4.87, p = 0.02). Elevated uACR, but not sTNFR1, increased the risk of ≥ 40% decline in CKD-EPI eGFR (HR 1.49, p = 0.001) and doubling of serum creatinine (HR 2.00, p < 0.001). A Cox proportional hazards regression model adjusted for clinical variables and sTNFR1 quartile is presented in Fig. 3, reinforcing the high incident mortality rates over 4 years in people in quartile 4 of sTNFR1.
Consequently, increased baseline uACR (HR 1.34, p = 0.003), but not sTNFR1, increased the risk of a composite endpoint of ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, renal replacement therapy, or death. Baseline HbA1c did not predict individual renal and mortality outcomes during follow-up. However, increased baseline HbA1c did independently predict the development of a composite endpoint of ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, renal replacement therapy, or death (p = 0.03), albeit in a much weaker fashion (HR 1.03) than baseline uACR. The strong univariate association between sTNFR1 and mortality persisted on multivariable regression, while associations with interim renal endpoints were not evident when sTNFR1 was considered in addition to other clinical variables. sTNFR1 did not improve model performance for prediction of ≥ 40% decline in CKD-EPI eGFR, doubling of serum creatinine, or composite renal and mortality endpoints. However, sTNFR1 did improve prediction of incident mortality by Cox regression models (p = 0.01). In a sensitivity analysis, results from multivariable Cox proportional hazards regression were validated using multivariable logistic regression adjusting for the same clinical covariates, with essentially identical findings (Supplementary Table 2). An additional sensitivity analysis which restricted multivariate Cox and logistic regression analyses to those with ≥ 2 years of renal functional follow-up data similarly identified baseline uACR, but not plasma sTNFR1, as strongly predictive of interim renal endpoints (Supplementary Table 3).
Considering all-cause mortality as a competing risk, subdistribution HRs for the risk of ≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine are presented in Table 5. Similar to Cox models, an increased risk of renal endpoints was observed with elevated uACR: subdistribution HRs 1.46 (p = 0.001) and 1.99 (p < 0.001) for ≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine, respectively. sTNFR1 did not independently predict interim renal endpoints. Figure 4 presents the cumulative incidence of renal endpoints and the competing risk of all-cause mortality. The incidence of death increased linearly and significantly across baseline sTNFR1 quartiles over the study period. Increases in the incidence of interim renal endpoints across baseline sTNFR1 quartiles were much smaller in magnitude and did not reach statistical significance. P-values for differences in the incidence of ≥ 40% decline in CKD-EPI eGFR and death across sTNFR1 quartiles were 0.22 and 0.01, respectively. P-values for differences in the incidence of doubling of serum creatinine and death across sTNFR1 quartiles were 0.19 and 0.006, respectively.
Cumulative incidence of ≥ 40% decline in CKD-EPI eGFR and death (A) and doubling of serum creatinine and death (B) stratified by plasma sTNFR1 quartile over the study period. Cumulative incidence of events of interest (≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine) and the competing risk of death were calculated using the cuminc function in the R package cmprsk. Cumulative incidence plots were generated using ggcompetingrisks from the R package survminer. Panels are labelled by baseline plasma sTNFR1 quartiles 1, 2, 3, and 4, respectively. The cumulative incidence of renal outcomes over the study period is depicted by the red lines; the cumulative incidence of the competing risk of death is represented by the blue lines. In plasma sTNFR1 quartiles 3 and 4, the competing risk of death occurred more commonly than renal outcomes including ≥ 40% decline in CKD-EPI eGFR and doubling of serum creatinine.
Discussion
This study provides insight into the complementary predictive performance of plasma sTNFR1 and uACR in the identification of subjects at high-risk of mortality and accelerated renal functional decline in older persons with longstanding type 2 diabetes and eGFR ≤ 60 mL/min/BSA in real-world clinical practice. We demonstrate that mortality rates are high in this population, and are strongly and independently predicted by sTNFR1. sTNFR1 provided no incremental benefit to conventional clinical variables in the identification of subjects at increased risk of accelerated renal functional decline.
Our study reaffirms the strong prognostication of accelerated renal functional decline by baseline levels of albuminuria in people with diabetes and CKD26. That sTNFR1 provided no incremental benefit in the identification of such patients in our dataset was somewhat surprising and contrary to the findings of Saulnier et al. who demonstrated that in a French cohort of patients with type 2 diabetes (SURDIAGENE), adjusting for the same clinical parameters used herein, plasma sTNFR1 independently identified an increased risk of ≥ 40% decline in eGFR and decline of GFR < − 5 mL/min/BSA/year13. However, mean age (64 versus 74 years) and diabetes duration (14 versus 16 years) were lower while mean eGFR (76 versus 42 mL/min/BSA) was higher in the SURDIAGENE study than in our cohort13.
In later CKD stages, is it possible that a combination of improved clinical prognostication of renal functional decline with routine variables (supported by the accuracy of the Kidney Failure Risk Equation in this setting) coupled with higher cardiovascular mortality diminishes the ability of sTNFR1 to independently identify people at risk of renal functional loss27,28. Median annual loss of CKD-EPI eGFR was relatively low in our cohort at − 2 mL/min/BSA/year, compared with − 5.6 mL/min/BSA/year in an Irish cohort study of patients with type 2 diabetic kidney disease (mean baseline eGFR 47 mL/min/BSA)5. Additionally, the study cohort had a relatively low burden of proteinuria, with median uACR for the study cohort being at the threshold for diagnosis of microalbuminuria (3.0 mg/mmol). Our study cohort was also elderly (mean age 74 years) with a high burden of coronary and peripheral artery disease (18% each). Non-proteinuric or minimally proteinuric diabetic kidney disease appears to be more common in those with prior cardiovascular events, and such patients are at higher risk of future cardiovascular than renal events29. Therefore, it is plausible that our elderly cohort with a high burden of established cardiovascular disease, minimal proteinuria, and slow rate of renal functional decline were primed for cardiovascular rather than renal events, which diminished statistical power to detect relationships between plasma sTNFR1 and progressive renal disease. Survival bias may also explain the lack of association between plasma sTNFR1 and progressive renal disease in our study, given that the population is older and had survived with CKD for longer than other younger cohorts in which sTNFR1 has been evaluated to date30. In a subset of the SURDIAGENE cohort (mean age 70 years, diabetes duration 18 years, and eGFR 49 mL/min/BSA) more similar to our study population, sTNFR1 independently predicted a composite of doubling of serum creatinine or ESKD and also all-cause mortality12. Individual renal endpoints were not reported therein.
Management of diabetic kidney disease centres on intensification of blood pressure control and renin-angiotensin-aldosterone system blockade to control proteinuria31. Currently, SGLT2is are relatively contraindicated in people with diabetes and eGFR ≤ 45 mL/min/BSA due to lack of glycaemic efficacy32. New therapies which improve outcomes for people with type 2 diabetes and more advanced CKD are required. Intentional weight loss strategies, including metabolic surgery, and mesenchymal stem cells hold promise in this regard6,7,33. Integrated diabetes and nephrology care at later CKD stages may also improve patient outcomes, particularly for people with diabetes and additional CKD aetiologies5, and should be considered to lower cardiovascular and renal risk in those with higher sTNFR1 values.
The predominance of white Caucasians in our cohort limits the applicability of our findings to adults from other racial and ethnic backgrounds, but there is no evidence at present to suggest that sTNFR1 behaves differently in patients from other racial backgrounds. Our study cohort was relatively small which may have limited statistical power to detect significant relationships between baseline plasma sTNFR1 and renal outcomes. However, our patient population was well characterised clinically and analyses of trends in renal function were made on the basis of a median of 14 eGFR values over mean 3.5 years of follow-up. Additionally, event rates of renal and mortality outcomes were high in our study cohort which improved statistical power, while study findings were replicated using several multivariate regression modelling approaches.
Baseline HbA1c values may have been falsely lowered by anaemia accompanying CKD, although mean haemoglobin for the study cohort was 12.7 g/dL and no patients were treated with an erythropoietin-stimulating agent. Future studies assessing the prognostic value of biomarkers in people with diabetes and CKD should consider adjusting multivariate analyses with alternative indicators of glycaemic control, such as glycated albumin34. Our study does lacks detail on the prevalence of additional CKD aetiologies other than diabetes. However, given the median diabetes duration of almost 16 years in the study cohort, it is reasonable to assume that most patients had CKD as a sequel to their diabetes. The generalisability of our findings to patients without diabetes is unknown and should be investigated in future studies.
Conclusions
In conclusion, mortality rates were high (over 50% over 4-year follow-up) in people with type 2 diabetes, CKD, and elevated plasma sTNFR1. uACR, but not sTNFR1, identified patients with subsequent accelerated renal functional decline. Conversely, increased sTNFR1 identified subjects at significantly increased risk of all-cause mortality but not accelerated renal functional decline. Thus, in this elderly cohort with longstanding type 2 diabetes and established CKD, plasma sTNFR1 and uACR provided complementary risk prediction of mortality and progressive renal disease, respectively.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ARB:
-
Angiotensin-II receptor blocker
- BSA:
-
Body surface area
- CKD:
-
Chronic kidney disease
- CKD-EPI:
-
Chronic kidney disease-epidemiology collaboration
- DKD:
-
Diabetic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- ESA:
-
Erythropoietin-stimulating agent
- ESKD:
-
End-stage kidney disease
- GLP1RA:
-
Glucagon-like peptide-1 receptor analogue
- HbA1c :
-
Glycated haemoglobin
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- Q1:
-
Quartile 1
- Q2:
-
Quartile 2
- Q3:
-
Quartile 3
- Q4:
-
Quartile 4
- RRT:
-
Renal replacement therapy
- SD:
-
Standard deviation
- SGLT2i:
-
Sodium-glucose co-transporter-2 inhibitor
- sTNFR1:
-
Soluble tumour necrosis factor receptor-1
- uACR:
-
Urine albumin-to-creatinine ratio
References
Afkarian, M. et al. Kidney disease and increased mortality risk in type 2 diabetes. J. Am. Soc. Nephrol. 24(2), 302–308 (2013).
Saran, R. et al. US renal data system 2019 annual data report: epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 75(1), A6–A7 (2020).
Mann, J. F. E. et al. Liraglutide and renal outcomes in type 2 diabetes. N. Engl. J. Med. 377(9), 839–848 (2017).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380(24), 2295–2306 (2019).
Martin, W. P. et al. Influence of referral to a combined diabetology and nephrology clinic on renal functional trends and metabolic parameters in adults with diabetic kidney disease. Mayo Clinic Proc. Innov. Quality Outcomes 1(2), 150–160 (2017).
Martin, W. P., Docherty, N. G. & Le Roux, C. W. Impact of bariatric surgery on cardiovascular and renal complications of diabetes: a focus on clinical outcomes and putative mechanisms. Expert Rev. Endocrinol. Metab. 2018, 1–12 (2018).
Holland, J. A., Martin, W. P., Docherty, N. G. & le Roux, C. W. Impact of intentional weight loss on diabetic kidney disease. Diabetes Obes. Metab. 21(10), 2338–2341 (2019).
Martin, W. P., White, J., Lopez-Hernandez, F. J., Docherty, N. G. & le Roux, C. W. Metabolic surgery to treat obesity in diabetic kidney disease, chronic kidney disease, and end-stage kidney disease; what are the unanswered questions? Front. Endocrinol. 11:289. https://doi.org/10.3389/fendo.2020.00289 (2020).
Bullo, M., Garcia-Lorda, P., Megias, I. & Salas-Salvado, J. Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes. Res. 11(4), 525–531 (2003).
Hawari, F. I. et al. Release of full-length 55-kDa TNF receptor 1 in exosome-like vesicles: a mechanism for generation of soluble cytokine receptors. Proc. Natl. Acad. Sci. USA 101(5), 1297–1302 (2004).
Van Zee, K. J. et al. Tumor necrosis factor soluble receptors circulate during experimental and clinical inflammation and can protect against excessive tumor necrosis factor alpha in vitro and in vivo. Proc. Natl. Acad. Sci. USA 89(11), 4845–4849 (1992).
Saulnier, P.-J. et al. Association of serum concentration of TNFR1 with all-cause mortality in patients with type 2 diabetes and chronic kidney disease: follow-up of the SURDIAGENE cohort. Diabetes Care 37(5), 1425 (2014).
Saulnier, P.-J. et al. Association of circulating biomarkers (Adrenomedullin, TNFR1, and NT-proBNP) with renal function decline in patients with type 2 diabetes: a french prospective cohort. Diabetes Care 40(3), 367 (2017).
Carlsson, A. C. et al. Association of soluble tumor necrosis factor receptors 1 and 2 with nephropathy, cardiovascular events, and total mortality in type 2 diabetes. Cardiovasc Diabetol 15, 40–40 (2016).
Niewczas, M. A. et al. Circulating TNF receptors 1 and 2 predict ESRD in type 2 diabetes. J. Am. Soc. Nephrol. 23(3), 507 (2012).
Pavkov, M. E. et al. Tumor necrosis factor receptors 1 and 2 are associated with early glomerular lesions in type 2 diabetes. Kidney Int. 89(1), 226–234 (2016).
Coca, S. G. et al. Plasma biomarkers and kidney function decline in early and established diabetic kidney disease. J. Am. Soc. Nephrol. 28(9), 2786–2793 (2017).
Niewczas, M. A. et al. A signature of circulating inflammatory proteins and development of end-stage renal disease in diabetes. Nat. Med. 25(5), 805–813 (2019).
Doody, A. et al. Validating the association between plasma tumour necrosis factor receptor 1 levels and the presence of renal injury and functional decline in patients with Type 2 diabetes. J. Diabetes Complicat. 32(1), 95–99 (2018).
Levey, A. S. et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 145(4), 247–254 (2006).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150(9), 604–612 (2009).
Therneau TM: A Package for Survival Analysis in S. version 2.38. https://CRAN.R-project.org/package=survival. 2015.
Kassambara A, Kosinski M, Biecek P: survminer: Drawing Survival Curves using 'ggplot2'. R package version 0.4.6. https://CRAN.R-project.org/package=survminer. 2019.
Gray B: cmprsk: Subdistribution Analysis of Competing Risks. R package version 2.2–9. https://CRAN.R-project.org/package=cmprsk. 2019.
Kuznetsova, A., Brockhoff, P. B. & Christensen, R. H. B. lmerTest package: tests in linear mixed effects models. J. Stat. Softw. 82(13), 26 (2017).
Carrero, J. J. et al. Albuminuria changes are associated with subsequent risk of end-stage renal disease and mortality. Kidney Int. 91(1), 244–251 (2017).
Tangri, N. et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 305(15), 1553–1559 (2011).
Keith, D. S., Nichols, G. A., Gullion, C. M., Brown, J. B. & Smith, D. H. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch. Intern. Med. 164(6), 659–663 (2004).
Robles, N. R., Villa, J., Felix, F. J., Fernandez-Berges, D. & Lozano, L. Non-proteinuric diabetic nephropathy is the main cause of chronic kidney disease: results of a general population survey in Spain. Diabetes Metabolic Syndrome 11(Suppl 2), S777-s781 (2017).
Ferguson, T. W. & Tangri, N. Identifying potential biases in the nephrology literature. Adv. Chronic Kidney Disease 23(6), 373–376 (2016).
Alicic, R. Z., Rooney, M. T. & Tuttle, K. R. Diabetic kidney disease: challenges, progress, and possibilities. Clin. J. Am. Soc. Nephrol. CJASN 12(12), 2032–2045 (2017).
Davidson, J. A. SGLT2 inhibitors in patients with type 2 diabetes and renal disease: overview of current evidence. Postgrad. Med. 131(4), 251–260 (2019).
Griffin, T. P., Martin, W. P., Islam, N., O’Brien, T. & Griffin, M. D. The promise of mesenchymal stem cell therapy for diabetic kidney disease. Curr. Diab. Rep. 16(5), 42 (2016).
Vos, F. E., Schollum, J. B. & Walker, R. J. Glycated albumin is the preferred marker for assessing glycaemic control in advanced chronic kidney disease. NDT Plus 4(6), 368–375 (2011).
Acknowledgements
We acknowledge the support of Fergus Fleming, EKF Diagnostics in the realisation of this study.
Funding
Funding support from the following agencies is acknowledged; Science Foundation Ireland (12/YI/B2480) to ClR, Swedish Medical Research Council (2015-02733) and European Foundation for the Study of Diabetes/Boehringer Ingelheim European Diabetes Research Programme (BI 2017_3) to ClR and NGD. WPM’s contribution was performed within the Irish Clinical Academic Training (ICAT) Programme, supported by the Wellcome Trust and the Health Research Board (Grant Number 203930/B/16/Z), the Health Service Executive National Doctors Training and Planning and the Health and Social Care, Research and Development Division, Northern Ireland. Costs related to measurement of baseline plasma sTNFR1 concentrations were covered by an educational grant to NGD from The University College Dublin Foundation sponsored by EKF Diagnostics Ltd., Cardiff, U.K. The funding bodies had no direct input into the study design, data analysis, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
N.G.D. and C.l.R. designed the study. R.J.C., D.S., and M.J.M. provided diabetes care to the study cohort. A.D. and S.J. measured plasma sTNFR1 in clinical samples, with assistance from PJT and ClR. A.D. and S.J. collected baseline clinical and laboratory information for the study cohort. C.T. and W.P.M. collected further clinical and longitudinal laboratory data for the study cohort. W.P.M. performed the statistical analyses. W.P.M., C.l.R., and N.G.D. interpreted the data. W.P.M., C.l.R., and N.G.D. drafted the manuscript with critical input from all authors. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
ClR discloses personal fees outside of the submitted work from Novo Nordisk, GI Dynamics, Eli Lilly, Johnson and Johnson, Sanofi, Aventis, Astra Zeneca, Janssen, Bristol-Myers Squibb and Boehringer-Ingelheim. WPM, CT, AD, SJ, RJC, DS, PJT, MJM, and NGD declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martin, W.P., Tuohy, C., Doody, A. et al. Parallel assessment of albuminuria and plasma sTNFR1 in people with type 2 diabetes and advanced chronic kidney disease provides accurate prognostication of the risks of renal decline and death. Sci Rep 10, 14852 (2020). https://doi.org/10.1038/s41598-020-71684-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71684-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.