Abstract
The association between regional economic status and the probability of renal recovery among patients with dialysis-requiring AKI (AKI-D) is unknown. The nationwide prospective multicenter study enrolled critically ill adult patients with AKI-D in four sampled months (October 2014, along with January, April, and July 2015) in Taiwan. The regional economic status was defined by annual disposable income per capita (ADIPC) of the cities the hospitals located. Among the 1,322 enrolled patients (67.1 ± 15.5 years, 36.2% female), 833 patients (63.1%) died, and 306 (23.1%) experienced renal recovery within 90 days following discharge. We categorized all patients into high (n = 992) and low economic status groups (n = 330) by the best cut-point of ADIPC determined by the generalized additive model plot. By using the Fine and Gray competing risk regression model with mortality as a competing risk factor, we found that the independent association between regional economic status and renal recovery persisted from model 1 (no adjustment), model 2 (adjustment to basic variables), to model 3 (adjustment to basic and clinical variables; subdistribution hazard ratio, 1.422; 95% confidence interval, 1.022–1.977; p = 0.037). In conclusion, high regional economic status was an independent factor for renal recovery among critically ill patients with AKI-D.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common and complex clinical entity associated with increased medical and economic burden1,2. Among the critically ill patients in the intensive care unit (ICU), about 50% have AKI3, and 4–15% have severe AKI necessitating renal replacement therapy (RRT)4. The in-hospital mortality rate of patients with dialysis-requiring AKI (AKI-D) might be up to 50–80%4. Among these patients with AKI-D, around 13–29% are dialysis-dependent at hospital discharge5, and 10–30% of patients with dialysis dependence are subsequently diagnosed with end-stage renal disease (ESRD)6,7.
It is well known that compared to renal recovery, the non-recovery of kidney function after AKI is associated with higher mortality and economic burden8. Several factors, such as older age, diabetes mellitus, congestive heart failure, the severity of underlying chronic kidney disease (CKD)9,10, as well as the severity of AKI11 and the number of AKI episode12, were considered as risk factors for non-recovery of AKI-D. However, the association between economic status and renal recovery among patients with AKI-D is rarely illustrated.
Previous studies evaluating the association between economic status and AKI disclosed that the predominant etiologies of AKI are different in regions with different economic statuses. AKI in lower economically developed regions, comparing to that in higher economic regions, is associated with less comorbidity burden and disease severity but may be associated with even poor prognoses due to the delayed recognition and treatment13,14,15. As to the recovery rate of AKI, it was higher in less economically developed regions than in higher economic regions13. These findings were explained by the young age and fewer comorbidities burden in patients in less economically developed regions. Nevertheless, the definitions of AKI and kidney recovery in these comparisons were diverse, and information regarding renal recovery in AKI-D was scarce13,14,15. Furthermore, the association between economic status and renal recovery probability is difficult to be determined meaningfully because of the foundational differences in etiology of AKI, practice pattern of AKI treatment, and the health care infrastructure, not to mention the significant under-report of data in lower-income regions14.
In Taiwan, the medical services for the total 23 million residents are provided by about 47,000 physicians in around 400 hospitals and ten thousand clinics, and over 99% of residents are covered by a single National Health Insurance with meager self-pay rates1. The high availability of medical services and the high coverage rate of medical insurance throughout the country minimize the confounding effects of health care infrastructure and economic consideration for seeking medical aids, making Taiwan an optimal place to evaluate the influence of regional economic status on renal recovery. Therefore, we conducted the current study in Taiwan to prove the hypothesis that the regional economic status is associated with the probability of renal recovery of critically ill patients with AKI-D.
Materials and methods
Study design and participants
This nationwide prospective multicenter study was conducted using the database of the nationwide epidemiology and prognosis of dialysis-requiring acute kidney injury (NEP-AKI-D) study16,17. Briefly, the NEP-AKI-D study was designed to enroll critically ill adult patients with AKI-D receiving RRT in the ICUs of both tertiary medical centers and regional hospitals located in the four geographical regions (north, middle, south, and east) of Taiwan. The four seasonal sampled months for enrolling participants were October 2014, along with January, April, and July 2015. The exclusion criteria included patients less than 20 years of age, patients with previous chronic dialysis before the index hospitalization, and patients who died within 48 h after admission to ICUs. After the enrollment process, we followed the clinical courses and documented the outcomes events of these enrolled participants until death or 90 days following hospital discharge. Then we evaluated the association between the regional economic status and the probability of renal recovery of these patients.
Demographic and clinical covariates
The demographic information and clinical data were documented in the registry. The laboratory data and clinical variables, including severity scores at four-time points (hospital admission, ICU admission, RRT initiation, and hospital discharge), were recorded. (The details of demographic and clinical covariates were provided in Supplementary files).
Patients' disease severities were assessed using the Charlson Comorbidity Index (CCI), the acute physiology and chronic health evaluation II (APACHE-II) score, the sequential organ failure assessment (SOFA), and inotropic equivalent (IE)18. Sepsis was diagnosed according to the "sepsis-3" clinical criteria, which include (1) suspected or documented infection, along with (2) evidence of organ dysfunction represented by an acute increase in the SOFA score of ≥ 2 points19.
Definitions and details about AKI and RRT
The AKI was diagnosed according to the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for AKI20. The definitions regarding the AKI and RRT were detailed in our previous work16 and the supplementary file (Supplementary files).
Regional economic status
The regional economic status was defined by the "annual disposable income per capita (ADIPC)" of individual cities where the enrolled hospitals located within the period from July 1, 2014, to June 30, 2015. The per-capita expenditures were defined as the total individual expenditures divided by the total resident numbers of the city. The ADIPC was obtained from the "National Statistics, Republic of China (Taiwan)" website of "Directorate-General of Budget, accounting, and statistics, Executive Yuan, Taiwan" (accessed online: https://statdb.dgbas.gov.tw/pxweb/Dialog/CityItemlist_n.asp).
Outcomes
The primary endpoint of the current study was renal recovery before death or 90 days following hospital discharge. We also additionally compared the all-cause mortality on the 90th day after hospital discharge. Renal recovery was defined as weaning from RRT for at least 7 days.
Statistical analysis
The R 2.12.1 (R Foundation for Statistical Computing, Vienna, Austria) and Scientific Package for Social Science (PASW Statistics for Windows, Version 22.0, Chicago: SPSS Inc) software were applied for statistical analyses. A two-sided p ≤ 0.05 was considered statistically significant. Categorical variables were expressed as "numbers (percentages)." Continuous variables were expressed as mean ± standard deviation (SD) for those with normal distribution or median [interquartile range] for those with non-normal distribution. The chi-square test, or Fisher's exact test for those with an expected value of ≤ 5 in any box, was used to analyze categorical variables. The independent t-test for normal distribution, or the Mann–Whitney U test for non-normal distribution, was used to compare continuous variables. We used a multilevel discrete-time event history analysis and adopted a generalized additive model (GAM), with adjustment to risk factors, to evaluate the threshold of economic status. The model incorporated the subject-specific (longitudinal) random effects and expressed as the logarithm of the odds (logit)21,22. We demonstrated the association between the economic variable and the probability of renal function recovery. We further transformed the relevant economic variable into a categorical variable using the best cut-points determined by the GAM plots. Because of the high mortality in critical patients with AKI-D, we used the Fine and Gray competing risk regression model with mortality taken as a competing risk factor to calculate the subdistribution hazard ratio (sHR) and 95% confidence interval (CI) for the probability of renal function recovery23,24. The Cox proportional method was used to compare the mortality risk between groups.
Ethics, consent, and permissions
The study design conformed to the ethical guidelines, and the Helsinki Declaration revised in 2013. The study was approved by the National Research Program for Biopharmaceuticals (NRPB)-Institutional Review Board (IRB) (NRPB2014050014) and IRBs of all the participating hospitals. The above IRBs waived the need for informed consent because of the de-identified personal information.
Results
A total of 1,322 critically ill patients (67.1 ± 15.5 years of age, 36.2% female) with AKI-D in the ICUs were enrolled. Among them, 833 patients (63.1%) died, 306 patients (23.1%) had a renal recovery, and 183 patients (13.8%) were diagnosed with ESRD within the 90 days following discharge. The renal recovery rate was 23.1% in all patients and 62.6% in survivors within the 90 days. Overall speaking, 306 patients experience renal recovery, whereas 1,016 patients did not have renal recovery before death (in the non-survivors) or before the 90th day after discharge (in the survivors) (Fig. 1).
Next step, we demonstrated the association between ADIPC and the probability of renal recovery by the nonlinear GAM plot with adjustment to age, gender, baseline estimated glomerular filtration rate (eGFR), ventilator support, and SOFA at RRT initiation. From the plot, the best cut-point of ADIPC for differentiating the higher and lower probabilities of renal recovery was determined as 10.8 × 103 United States dollars (Fig. 2).
Generalized additive model plot demonstrating the association between economic status and the probability of renal recovery. Note: The model incorporated the subject-specific (longitudinal) random effects, expressed as the logarithm of the odds (logit). The probability of renal recovery was constructed with the ADIPC and was centered on having an average of zero over the range of the data. ADIPC, annual disposable income per capita; USD, United States dollar.
Clinical characteristics of the two groups stratified by economic status
According to the best cut-point of ADIPC, we categorized all patients into high (n = 992) and low economic status groups (n = 330). Compared to the low economic status group, the patients in the high economic status group had higher proportions of coronary artery disease (28.7% versus 22.4%, p = 0.03) and congestive heart failure (denoted as congestive heart failure with New York Heart Association Functional Classifications 3 and 4) (43.5% versus 20.0%). At hospital admission, the high economic status group had higher baseline CCI (7.0 ± 3.1 versus 6.3 ± 3.1 points, p = 0.01), BUN (59.1 ± 45.3 versus 49.5 ± 38.8 mg/dL), SCr (3.7 ± 3.4 versus 3.2 ± 2.9 mg/dL, p = 0.01) but lower IE (5.7 ± 14.8 versus 9.0 ± 21.4 points, p = 0.01) than the low economic status group (all p < 0.001 unless otherwise denoted).
At ICU admission, the high economic status group had a higher proportion of ventilator support (77.0% versus 50.9%) as well as higher BUN (66.4 ± 46.9 versus 57.1 ± 43.9 mg/dL, p = 0.01) and SCr (4.0 ± 3.3 versus 3.6 ± 3.0 mg/dL, p = 0.04), but lower surgical indication (21.3% versus 28.2%, p = 0.01) and IE (9.8 ± 17.3 versus 14.5 ± 30.0 points, p = 0.01). At RRT initiation, the high economic status group had higher BUN (88.5 ± 49.4 versus 81.8 ± 49.0 mg/dL, p = 0.03), potassium (4.7 ± 1.2 versus 4.5 ± 1.2 mg/dL, p = 0.03), and higher proportion of receiving diuretics (65.1% versus 58.8%, p = 0.04), but lower IE (11.7 ± 18.5 versus 19.0 ± 31.6 points) and SOFA scores (11.8 ± 4.2 versus 12.7 ± 4.4 points, p = 0.01) (all p < 0.001 unless otherwise denoted) (Tables 1 and S1, and Figure S1).
Clinical characteristics of the two groups stratified by renal recovery status
Compared to those without renal recovery, the patients with renal recovery were younger (64.4 ± 16.0 versus 67.9 ± 15.2 years) and had a lower proportion of congestive heart failure (32.0% versus 39.4%, p = 0.02). At hospital admission, the patients with renal recovery had lower baseline CCI (5.9 ± 3.0 versus 7.1 ± 3.1 points) but higher urine output (921.3 ± 1,099.1 versus 758.8 ± 828.3 ml/day, p = 0.02) than those without renal recovery. At ICU admission, the patients with recovery had a lower proportion of ventilator support (62.7% versus 72.8%, p = 0.01). They also had higher urine output (879.7 ± 985.8 versus 699.7 ± 819.6 ml/day, p = 0.01) and Glasgow coma scale (GCS) (10.3 ± 4.6 versus 9.4 ± 4.6 points, p = 0.01), but lower APACHE-II (21.4 ± 7.2 versus 22.8 ± 7.4 points, p = 0.01) and SOFA scores (9.6 ± 3.9 versus 10.4 ± 4.1 points, p = 0.01) than those without recovery (all p < 0.001 unless otherwise denoted).
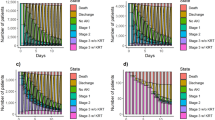
At RRT initiation, the patients experiencing renal recovery had better hemodynamic status (higher mean arterial pressure [MAP] along with lower IE and heart rate [HR]), lower disease severity (higher GCS along with lower APACHE-II and SOFA scores), and better residual kidney function (higher urine output and lower BUN) than those without recovery. The patients with renal recovery had less proportion of "sepsis" (58.8% versus 74.3%) but more "nephrotoxic drug" (8.5% versus 4.5%, p = 0.01) as "etiology of AKI," as well as less azotemia (43.8% versus 57.1%) and oliguria (51.3% versus 70.1%) as "indications of RRT" than those without renal recovery. As to the economic status, the patients with renal recovery had high ADIPC (11.6 ± 2.0 versus 11.3 ± 1.9 × 103 united states dollar [USD], p = 0.02) than those without recovery (all p < 0.001 unless otherwise denoted) (Fig. 3 and Table S2).
Time chart demonstrating the statistical differences between patients with and without renal recovery. Note: We only listed the variables which were statistically different between the two groups and were indicative of "worse condition" (ex: lower urine output) rather than "better condition" (ex: higher urine output). #Statistical significance of the corresponding period (lines with the same colors) between the two groups. APACHE, acute physiology and chronic health evaluation; BUN, blood urea nitrogen; CCI, Charlson Comorbidity Index; CHF, congestive heart failure; ES, economic status; GCS, Glasgow coma scale; Hb, hemoglobin; HR, heart rate; ICU, intensive care unit; IE, inotropic equivalent; MAP, mean arterial pressure; RRT, renal replacement therapy; SOFA, sequential organ failure assessment; UO, urine output.
Independent predictors for renal recovery
Finally, we conducted three models of competing risk regression analyses to evaluate the predictive ability of economic status for renal recovery. Model 1 included economic status alone. Model 2 included basic clinical variables besides economic status. Model 3 included clinical variables at RRT initiation in addition to the variables in Model 2. All the variables put into the models were of statistical significance in univariate analyses or those considered essential. We found that high economic status was independently associated with renal recovery in all three models of competing risk regression analyses (Table 2).
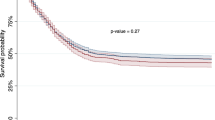
Figure 4A, drawn by a competing risk regression model with mortality taken as a competing risk factor, showed that the high economic status group had a significantly higher probability for renal recovery (p = 0.036). The sharp upticks in both curves on the 149th day were resulted from the three deaths on the day. The association between economic status and mortality risk was not significant in Fig. 4B depicted by the Cox proportional plot with multiple factors adjustment (p = 0.070). The sharp upticks in both curves on the 122nd day were resulted from the four deaths on that day.
The adjusted factors of these two plots included all the variables, except for economic status, in Model 3 (Table 2). They included gender, age, baseline eGFR, CHF, variables at RRT initiation (heart rate, MAP, urine output, BUN, IE, SOFA), sepsis (etiology), azotemia (indication), and oliguria (indication).
Discussion
To the best of our knowledge, the current nationwide study is an unprecedented study that found that the hospital located in the cities with high average ADIPC, comparing to those in the city with lower value, independently associated with a higher probability of renal recovery among critically ill patients with AKI-D.
In Taiwan, there are both local hospitals and tertiary medical centers in most of the cities. In the current study, the proportions of patients admitted to tertiary medical centers were not different between groups with high and low regional economic status (Table 1). The high availability of medical facilities allows residents to search for appropriate medical aids within the same cities they live in. Thus the average economic status of the cities where the hospitals located might be considered as the regional economic status of the patients live in the same city.
Besides, the hospitals enrolled in the study are either public hospitals or religious hospitals. All the medical professional works following the universal practice guidelines and regulations of the Taiwan National Health Insurance, and get payment from the health insurance rather than the patient personally. Thus the confounding influences from different hospital levels and varied practice patterns could be minimized. The findings of the current study pointed out the importance of regional economic status and opened a new avenue for better acute kidney disease care with an issue of economic status25.
In the current study, the patients with renal recovery were younger and had fewer comorbidities (lower prevalence of CHF and lower CCI), and clinically better than the patients who did not experience renal recovery throughout the whole hospital course (Fig. 3 and Table S1). Besides, high economic status, higher baseline eGFR, younger age, and lower SOFA scores were independently associated with a higher probability of renal recovery. In contrast, those with azotemia and oliguria as indications of RRT were less likely to have renal recovery among critically ill patients with AKI-D (Table 2). Most of the independent predictors of renal function recovery, except for economic status, are well recognized in the previous work14,26,27,28,29,30,31,32.
Regional socioeconomic deprivation has long been considered as an indicator of poor health and life expectancy33. In the nephrology field, socioeconomic status is well identified as an essential factor influencing the clinical outcomes of patients with CKD and kidney transplantation34,35, as well as the incidence and severity of AKI and mortality of AKI patients25.
Three potential reasons were proposed to explain the association between economic status and patients' prognoses25,36,37,38,39. Firstly, previous investigations found that low economic status disproportionally associates with a lack of health literacy, which refers to the ability to access, understand, and apply health-related information36. Limited health literacy links to the development of long-term health problems, decreased use of preventative medicine, deficient ability to handle medications, and elevated mortality37. Secondly, low economic status is also associated with worse patient-related health beliefs and behavior (e.g., higher prevalence of smoking, alcohol, obesity, poor control of blood sugar and blood pressure, unhealthy diet, and inactivity), as well as inadequate access to medical service (such as a delayed presentation to medical service)25. Thirdly, previous studies disclosed that insufficient insurance coverage results in a lower post-AKI follow-up rate and a lower prescription rate of drugs, which may be beneficial for renal function, such as angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers38,39. Indeed, insurance coverage is theoretically an essential issue regarding the association between economic status and renal recovery. Although most of the residents in Taiwan are covered by the National Health Insurance with minimal copayment from the patients, the influence of financial consideration on the behavior of seeking medical service could not be eliminated by the higher insurance coverage rate.
In the current nationwide cohort, the patients with the high regional economic status group were more likely to be medical patients with a higher baseline comorbidity burden, including a worse baseline kidney function. They were also more likely to have sepsis, receive diuretics for AKI, and started RRT for hyperkalemia. Despite this unfavorable baseline kidney function, the patients with high regional economic status were still associated with a similar risk of mortality and higher possibility of renal recovery when compared to their counterparts.
The patients in the low regional economic status group had worse hemodynamic status (higher IE) throughout the whole hospitalization and had higher SOFA scores and more shock at RRT initiation (Tables 1 and S1, and Figure S1). For the patients with low regional economic status, the worse initial hemodynamic status in those with less underlying comorbidity burden could be potentially interpreted as "the delayed medical access." It is worthy of mentioning that delayed medical access exists even in a country with high availability of medical service and coverage rate of medical insurance. These findings underscored that, besides insurance coverage, other factors such as health literacy, as well as patient-related health beliefs and behavior are also essential regarding patients' prognoses.
In light of the results of the current study, the population level-based economic status is a crucial element in acute kidney disease and post-AKI care. To eliminate all avoidable deaths from AKI worldwide by 2025, the 0by25 initiative from the International Society of Nephrology proposed the 5Rs (Risk assessment, Recognition, Response, Renal support, and Rehabilitation) as a core to optimize the management of AKI worldwide40. Our findings extendedly add values in 5R approaches for acute kidney disease and post-AKI care. Examples include that physicians are encouraged to assess the probability of renal recovery (Risk assessment), as well as identify AKI-D patients experiencing renal recovery (Recognition) and stop the dialysis at the earliest time when the patients have renal recovery (Response and Renal support). Subsequently, the patients who experience renal recovery should receive regular follow-up (Rehabilitation). We also raised the incremental efforts in education to improve patients' health literacy, as well as health beliefs and behavior, might be an effective way, together with an increase in medical insurance coverage, to improve the probability of renal recovery in AKI patients.
Several limitations of this study should be addressed. Firstly, in the current study, which focused on the dialysis-withdrawal probability among AKI-D patients, the "indication bias" regarding the indication for dialysis existed. Nevertheless, the similar mortality rates between the high and low economic status groups minimized the "healthy worker survivor bias" regarding the dialysis-withdrawal probability. Secondly, the current study enrolled a sampled population of critically ill patients with AKI-D, including 23.0% of surgical patients and 77.0% of medical patients. Thus the results may not serve as a representative sample of all patients with varied types of AKI throughout the world. Thirdly, kidney recovery following AKI is challenging to define because it involves both structural and functional levels in the cell to whole organ level40. In the current study, we defined renal recovery by "dialysis-withdrawal." Although the decision of "dialysis-withdrawal" was made according to the clinical judgment of the physicians, the decision-making is clinical driven and of valuable clinical relevance41. Fourthly, despite the comprehensive adjustment for potential confounders in the current study, some factors which may associate with renal recovery might still be not available. Fifthly, as a population-level based investigation, the "ecological fallacy" is an unavoidable concern. Since we used population-level based data to demonstrate the association with renal recovery, the results in the current study are appropriate for population-level based application, but not for person-level practice. Further study using individuals' economic data is warranted to confirm our results and investigate the factors behind our findings.
In conclusion, we found that high regional economic status was independently associated with a higher possibility of renal recovery among critically ill patients with AKI-D, although with a similar mortality rate. The delayed presentation was a primary potential reason for the worse renal recovery rates in patients with low regional economic status. Further studies are warranted to exam the findings and determine the exact role of the economic status for renal recovery among patients with AKI-D.
References
Wu, V. C. et al. Long-term risk of coronary events after AKI. J. Am. Soc. Nephrol. 25, 595–605. https://doi.org/10.1681/ASN.2013060610 (2014).
Siew, E. D. & Davenport, A. The growth of acute kidney injury: a rising tide or just closer attention to detail?. Kidney Int. 87, 46–61. https://doi.org/10.1038/ki.2014.293 (2015).
Hoste, E. A. et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 41, 1411–1423. https://doi.org/10.1007/s00134-015-3934-7 (2015).
Clark, E., Wald, R., Walsh, M. & Bagshaw, S. M. Timing of initiation of renal replacement therapy for acute kidney injury: a survey of nephrologists and intensivists in Canada. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfr740 (2012).
Rewa, O. & Bagshaw, S. M. Acute kidney injury-epidemiology, outcomes and economics. Nat. Rev. Nephrol. 10, 193–207. https://doi.org/10.1038/nrneph.2013.282 (2014).
Korkeila, M., Ruokonen, E. & Takala, J. Costs of care, long-term prognosis and quality of life in patients requiring renal replacement therapy during intensive care. Intensive Care Med. 26, 1824–1831 (2000).
Wu, V. C. et al. Long-term outcomes after dialysis-requiring acute kidney injury. Biomed. Res. Int. 2014, 365186. https://doi.org/10.1155/2014/365186 (2014).
Pannu, N., James, M., Hemmelgarn, B., Klarenbach, S. & Alberta Kidney Disease Network. Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin. J. Am. Soc. Nephrol. 8, 194–202. https://doi.org/10.2215/CJN.06480612 (2013).
Hickson, L. J. et al. Predictors of outpatient kidney function recovery among patients who initiate hemodialysis in the hospital. Am. J. Kidney Dis. 65, 592–602. https://doi.org/10.1053/j.ajkd.2014.10.015 (2015).
Wu, V. C. et al. Acute-on-chronic kidney injury at hospital discharge is associated with long-term dialysis and mortality. Kidney Int. 80, 1222–1230. https://doi.org/10.1038/ki.2011.259 (2011).
Chawla, L. S., Amdur, R. L., Amodeo, S., Kimmel, P. L. & Palant, C. E. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 79, 1361–1369. https://doi.org/10.1038/ki.2011.42 (2011).
Thakar, C. V., Christianson, A., Himmelfarb, J. & Leonard, A. C. Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin. J. Am. Soc. Nephrol. 6, 2567–2572. https://doi.org/10.2215/CJN.01120211 (2011).
Mehta, R. L. et al. Recognition and management of acute kidney injury in the International Society of Nephrology 0 by 25 global snapshot: a multinational cross-sectional study. Lancet 387, 2017–2025. https://doi.org/10.1016/S0140-6736(16)30240-9 (2016).
Hoste, E. A. J. et al. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol. 14, 607–625. https://doi.org/10.1038/s41581-018-0052-0 (2018).
Yang, L. et al. Acute kidney injury in China: a cross-sectional survey. Lancet 386, 1465–1471. https://doi.org/10.1016/S0140-6736(15)00344-X (2015).
Shiao, C. C. et al. Nationwide epidemiology and prognosis of dialysis-requiring acute kidney injury (NEP-AKI-D) study: design and methods. Nephrology (Carlton) 21, 758–764. https://doi.org/10.1111/nep.12670 (2016).
Chen, Y. Y. et al. Norepinephrine administration is associated with higher mortality in dialysis requiring acute kidney injury patients with septic shock. J. Clin. Med. https://doi.org/10.3390/jcm7090274 (2018).
Chen, Y. S. et al. Preliminary result of an algorithm to select proper ventricular assist devices for high-risk patients with extracorporeal membrane oxygenation support. J. Heart Lung Transplant. 20, 850–857 (2001).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Section 2: AKI definition. Kidney Int. Suppl. 2, 19–36. https://doi.org/10.1038/kisup.2011.32 (2012).
Wu, V. C. et al. Endothelial progenitor cells in primary aldosteronism: a biomarker of severity for aldosterone vasculopathy and prognosis. J. Clin. Endocrinol. Metab 96, 3175–3183. https://doi.org/10.1210/jc.2011-1135 (2011).
Shu, K. H. et al. Urinary pi-glutathione S-transferase predicts advanced acute kidney injury following cardiovascular surgery. Sci. Rep. 6, 26335. https://doi.org/10.1038/srep26335 (2016).
Wu, V. C. et al. Risk of new-onset diabetes mellitus in primary aldosteronism: a population study over 5 years. J. Hypertens. 35, 1698–1708. https://doi.org/10.1097/HJH.0000000000001361 (2017).
Wu, V. C. et al. Outcome prediction of acute kidney injury biomarkers at initiation of dialysis in critical units. J. Clin. Med. https://doi.org/10.3390/jcm7080202 (2018).
Holmes, J. et al. Acute kidney injury, age, and socioeconomic deprivation: evaluation of a national data set. Kidney Int. Rep. 4, 824–832. https://doi.org/10.1016/j.ekir.2019.03.009 (2019).
Schiffl, H. Discontinuation of renal replacement therapy in critically ill patients with severe acute kidney injury: predictive factors of renal function recovery. Int. Urol. Nephrol. 50, 1845–1851. https://doi.org/10.1007/s11255-018-1947-1 (2018).
Jones, S. L. & Devonald, M. A. How acute kidney injury is investigated and managed in UK intensive care units: a survey of current practice. Nephrol. Dial. Transplant. 28, 1186–1190. https://doi.org/10.1093/ndt/gft015 (2013).
Frohlich, S., Donnelly, A., Solymos, O. & Conlon, N. Use of 2-hour creatinine clearance to guide cessation of continuous renal replacement therapy. J. Crit. Care 27(744), e741-745. https://doi.org/10.1016/j.jcrc.2012.08.012 (2012).
Schiffl, H. & Lang, S. M. Severe acute hypophosphatemia during renal replacement therapy adversely affects outcome of critically ill patients with acute kidney injury. Int. Urol. Nephrol. 45, 191–197. https://doi.org/10.1007/s11255-011-0112-x (2013).
Wu, V. C. et al. Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med. 34, 101–108. https://doi.org/10.1007/s00134-007-0813-x (2008).
Uchino, S. et al. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit. Care Med. 37, 2576–2582. https://doi.org/10.1097/CCM.0b013e3181a38241 (2009).
Lee, B. J. et al. Predicting renal recovery after dialysis-requiring acute kidney injury. Kidney Int. Rep. 4, 571–581. https://doi.org/10.1016/j.ekir.2019.01.015 (2019).
Diez Roux, A. V. et al. Neighborhood of residence and incidence of coronary heart disease. N. Engl. J. Med. 345, 99–106. https://doi.org/10.1056/NEJM200107123450205 (2001).
Vart, P., Gansevoort, R. T., Joosten, M. M., Bultmann, U. & Reijneveld, S. A. Socioeconomic disparities in chronic kidney disease: a systematic review and meta-analysis. Am. J. Prev. Med. 48, 580–592. https://doi.org/10.1016/j.amepre.2014.11.004 (2015).
Stephens, M. R., Evans, M., Ilham, M. A., Marsden, A. & Asderakis, A. The influence of socioeconomic deprivation on outcomes following renal transplantation in the United Kingdom. Am. J. Transplant. 10, 1605–1612. https://doi.org/10.1111/j.1600-6143.2010.03041.x (2010).
Taylor, D. M. et al. A systematic review of the prevalence and associations of limited health literacy in CKD. Clin. J. Am. Soc. Nephrol. 12, 1070–1084. https://doi.org/10.2215/CJN.12921216 (2017).
Taylor, D. M. et al. Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrol. Dial. Transplant. 33, 1545–1558. https://doi.org/10.1093/ndt/gfx293 (2018).
Ke, C. et al. Impact of socioeconomic status on incidence of end-stage renal disease and mortality after dialysis in adults with diabetes. Can. J. Diabetes 43, 483–489. https://doi.org/10.1016/j.jcjd.2019.04.006 (2019).
Crews, D. C., Liu, Y. & Boulware, L. E. Disparities in the burden, outcomes, and care of chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 23, 298–305. https://doi.org/10.1097/01.mnh.0000444822.25991.f6 (2014).
Mehta, R. L. et al. International Society of Nephrology’s 0 by 25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 385, 2616–2643. https://doi.org/10.1016/S0140-6736(15)60126-X (2015).
Romagnoli, S., Clark, W. R., Ricci, Z. & Ronco, C. Renal replacement therapy for AKI: When? How much? When to stop?. Best Pract. Res. Clin. Anaesthesiol. 31, 371–385. https://doi.org/10.1016/j.bpa.2017.10.001 (2017).
Acknowledgements
We appreciate and thank all the members of the Taiwan Clinical Trial Consortium (TCTC) and the National Taiwan University Study Group on Acute Renal Failure (NSARF). We also give thanks to Miss Simone Yu for her English-editing. The members of the TCTC are listed in alphabetical order of their affiliation names: [Fu Jen Catholic University Hospital]: Kuo-Cheng Lu, MD. [Chi-Mei Medical Center, Liouying]: Jian-Jhong Wang, MD. [Chi-Mei Medical Center, Yongkang]: Wei-Chih Kan, MD. [China Medical University Hospital]: Chiu-Ching Huang, MD, PhD, Che-Yi Chou, MD, PhD, Ya-Fei Yang, MD, PhD. [Dalin Tzu-Chi Hospital]: Jen-Pi Tsai, MD, PhD. [International-Harvard Statistical Consulting Company]: Fu-Chang Hu, Ph.D. [Kaohsiung Chang Gung Memorial Hospital]: Chien-Te Lee, MD, PhD, Jin-Bor Chen, MD, Chih-Hsiung Lee, MD, Wen-Chin Lee, MD, PhD, Lung-Chih Li, MD, PhD, Te-Chuan Chen, MD. [Kaohsiung Municipal Ta-Tung Hospital]: Hugo You-Hsien Lin, MD. [Keelung Chang Gung Memorial Hospital]: Yung-Chang Chen, MD, Chin-Chan Lee, MD, Chiao-Yin Sun, MD, Heng-Chih Pan, MD. [Linkou Chang Gung Memorial Hospital]: Ji-Tseng Fang, MD, Ming-Yang Chang, MD, PhD, Chang-Chyi Jenq, MD, Chan-Yu Lin, MD, PhD, Chih-Hsiang Chang, MD, Tsung-Yu Tsai, MD. [Lin-Shin Hospital]: Cheng-Min Chen, MD. [Lotung Poh-Ai Hospital]: En-Tzu Lin, MD. [Saint Mary's Hospital Luodong]: Chih-Chung Shiao, MD. [Mackay Memorial Hospital]: Chih-Jen Wu, MD, PhD, Cheng-Jua Lin, MD, Pei-Chen Wu, MD. [Mackay Memorial Hospital Taitung Branch]: Feng-Chi Kuo, MD. [Min-Sheng General Hospital]: Chih-Jen Weng, MD. [National Health Research Institutes]: Li-Kwang Chen, PhD. [National Taiwan University Hospital]: Kwan-Dun Wu, MD, PhD, Tzong-Shinn Chu, MD, PhD, Yung-Ming Chen, MD, Shuei-Liong Lin, MD, PhD, Vin-Cent Wu, MD, PhD, Tao-Min Huang, MD, Yu-Feng Lin, MD, Chun-Fu Lai, MD, PhD. Tai-Shuan Lai, MD, PhD. [National Taiwan University Hospital Hsin Chu Branch]: Wei-Shun Yang, MD. [New Taipei City Hospital Sanchong Branch]: Wen-Ding Hsu, MD, MS. [Shin-Kong Wo Ho-Su Memorial Hospital]: Jyh-Gang Leu, MD, PhD, Jui-Ting Chang MD. [Sin-Ren Hospital]: Hung-Hsiang Liou, MD. [Taichung Veteran General Hospital]: Kuo-Hsiung Hsu, MD, Ming-Ju Wu, MD, PhD, Chun-Te Huang, MD. [Taichung Veteran General Hospital Chiayi Branch]: Zi-hong You, MD. [Taipei City Hospital Heping Branch]: Chao-Fu Chang, MD. [Taipei Medical University Hospital]: Tzen-Wen Chen, MD, PhD, Hsi-Hsien Chen, MD, PhD, Fan-Chi Chang, MD, PhD, Yen- Chung Lin, MD, Mai-Szu Wu, MD, Chih-Chin Kao, MD. [Taipei Tzu Chi Hospital]: Szu-Chun Hung, MD, Ko-Lin Kuo, MD, PhD, Che-Hsiung Wu, MD. [Taipei Veterans General Hospital]: Der-Cherng Tarng, MD, PhD, Jinn-Yang Chen, MD, Chih-Yu Yang, MD, PhD, Kuo-Hua Lee, MD. [Taoyuan General Hospital, Ministry of Health and Welfare]: Wei-Jie Wang, MD, PhD, Sheng-Wen Ko, MD, Jui-Hsiang Lin, MD. We also express our sincere gratitude to all staff of the Taiwan Clinical Trial Consortium (TCTC).
Funding
This study was founded by Taiwan National Science Council [101-2314-B-002-085-MY3, 102-2314-B-002-140-MY2, 104-2314-B-002-125-MY3, 106-2314-B-002-166-MY3, 107-2314-B-002-026-MY3], National Health Research Institutes [PH-102-SP-09], National Taiwan University Hospital [106-FTN20, 106-P02, UN106-014, 106-S3582, 105-P05, VN105-04, 105-S3061, 107-S3809, 107-T02] and Ministry of Science and Technology (MOST) of the Republic of China (Taiwan) [MOST 106-2321-B-182-002, 105-2314-B-002-045, Most 109-2321-B-182-001].
Author information
Authors and Affiliations
Contributions
Conceptualization, C.-C.S., V.-C.W., T.-S.C., M.-S.W. and K.-D.W.; Data curation, Y.-F.Y., E.-T.L., H.-C.P., C.-H.C., C.-T.H., M.-T.K., T.-F.C., Y.-C.C., W.-C.K., F.-C.K., T.-C.C., Y.M.C., C.-J.W., H.-H.L., J.-T.F. and C.-C.H.; Formal analysis, C.-C.S., Y.-H.C., W.-C.K., Y.M.C., H.-H.L., V.-C.W., T.-S.C. and C.-C.H.; Funding acquisition, Y.-C.C., K.-D.W. and J.-T.F.; Investigation, C.-C.S., Y.-H.C., E.-T.L., H.-C.P., C.-H.C., C.-T.H., T.-F.C., Y.-C.C., W.-C.K., H.-H.L., K.-C.L., V.-C.W., K.-D.W., J.-T.F. and C.-C.H.; Methodology, C.-C.S., H.-C.P., C.-H.C., C.-T.H., T.-F.C., Y.-C.C., F.-C.K., T.-C.C., Y.M.C. and T.-S.C.; Project administration, Y.-H.C.; Resources, H.-H.L. and K.-C.L.; Software, Y.-H.C.; Supervision, Y.M.C., C.-J.W., K.-C.L., V.-C.W., T.-S.C., M.-S.W., K.-D.W., J.-T.F. and C.-C.H.; Writing—original draft, C.-C.S. and W.-C.K.; Writing—review and editing, C.-C.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shiao, CC., Chang, YH., Yang, YF. et al. Association between regional economic status and renal recovery of dialysis-requiring acute kidney injury among critically ill patients. Sci Rep 10, 14573 (2020). https://doi.org/10.1038/s41598-020-71540-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71540-7
This article is cited by
-
Wet depositions of cations in forests across NADP, EMEP, and EANET monitoring networks over the last two decades
Environmental Science and Pollution Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.