Abstract
There is a need to better understand key factors that impact sleep and circadian function for young adults of differing races and sexes. Sex and race are common factors contributing to disparities in health outcomes; however, the influence of these variables on sleep and circadian patterns for young adults are not well known. Multiple objective and self-report facets of sleep and circadian function were assessed (melatonin onset, actigraphy, and sleep diaries) in an ecological momentary assessment study of 150 emerging adults (Mage = 21.8 years; 58.7% female; 56% White, 22.7% Black, 21.3% Other ethnicity) at high or low risk for bipolar spectrum disorder (BSD). Controlling for BSD risk status, sex and race were significant predictors of objective and self-reported sleep and circadian rhythm measures. Males self-reported better sleep efficiency and exhibited later dim light melatonin onset phase than females, whereas females exhibited more actigraphy-measured sleep periods. White participants exhibited more actigraphy-measured total sleep time (TST), better sleep efficiency, and fewer sleep periods, and more self-reported TST and better sleep efficiency than Black participants. Our findings enhance the literature by utilizing robust measurement of sleep and circadian parameters to extend previous findings to a young adult sample at high or low risk for BSD.
Similar content being viewed by others
Introduction
Although sleep is a critical component of a healthy lifestyle1,2, many young adults do not obtain enough quality sleep3,4. Optimal sleep and circadian function are imperative for cognitive functioning (memory, mood regulation, etc.), metabolism, appetite regulation, immune and hormone functioning, and cardiovascular health2,5. Moreover, sleep and circadian disturbances relate to hypertension, heart disease, diabetes, obesity, and mortality2,5, and play a key role in the onset and course of Bipolar Spectrum Disorder (BSD)6.
In adult samples, females objectively slept better than males in the laboratory with earlier timing, longer duration of sleep, shorter sleep onset latency, better sleep efficiency and more slow-wave sleep7,8. Similarly, in a young adult sample, dim light melatonin onset (DLMO) phase was earlier in females than in males9, and in an adolescent sample, based on actigraphic estimates, wake after sleep onset (WASO) was greater and total sleep time was reduced for boys compared to girls10. However, females report significantly more sleep problems than males11 and less high-quality, uninterrupted sleep12,13. Further, beyond sleep measures, the intrinsic circadian period has been shown to be significantly shorter in healthy adult females than males in some studies14,15, and females also have been reported to have an earlier entrained melatonin circadian phase than males16.
Objective sleep studies have found decreases in slow-wave sleep (SWS) and increases in stage 1 and 2 non-rapid eye movement (NREM) sleep in Blacks compared to Whites17,18,19,20,21. Sleep duration also has been reported to be shorter, and sleep efficiency and self-rated sleep quality found to be poorer in Blacks than Whites17,22,23,24,25. Population-based studies also have reported racial differences using self-reported sleep26,27,28 or wrist actigraphy29, whereby Blacks are more likely to sleep less than Whites. The race-sleep relationship persists independently of socioeconomic status17, and there is an established association of self-identified race with sleep health inequalities30,31,32. In addition, beyond sleep, a number of studies show Blacks also have a shorter endogenous circadian period, larger phase advances, and smaller phase delays than Whites15,32,33,34,35,36; by contrast, self-reported chronotype as measured by the Morningness-Eveningness Questionnaire (MEQ)37 did not significantly differ between Blacks and Whites32.
There are several limitations of the existing literature. Sleep in some of these studies was assessed solely via self-report and/or along a single dimension or item, and research has shown that individuals overestimate self-reported sleep when compared to objective measures10,38. Furthermore, research including objective measures of sleep and circadian rhythms often derives from laboratory studies, which utilize well-controlled environments, but reduce generalizability. Much less is known about objective sleep and circadian rhythm parameters in emerging adults’ daily lives. Additionally, most studies have been cross-sectional, and few have investigated sex and racial differences in emerging adults at high or low risk for BSD.
To address these limitations, we examined multiple facets of sleep and circadian rhythms including objective and self-report assessments in a naturalistic ecological momentary assessment (EMA) study using a large sample of emerging adults, some of whom were at risk for BSD.
Accordingly, the aims and hypotheses of this study were as follows: 1. To examine the influence of sex and race on sleep and circadian measures in a novel population and setting. Given the research outlined above indicating poorer self-reported, but better objective, sleep quality in females, we hypothesized females would report poorer sleep ratings, but would show better objective sleep outcomes, compared to males. Because previous literature demonstrates poorer objective and subjective sleep quality in Black compared to White participants, we also hypothesized White participants would show better self-reported and objective sleep indices compared to Black participants. 2. To strengthen the rigor of construct measurement for sleep and circadian rhythms in a naturalistic EMA study by examining multiple facets of sleep and circadian rhythms including objective and self-report assessments. We hypothesized self-report and objective sleep indices would be significantly different from each other in a naturalistic EMA study.
Results
Relationships between sleep and circadian measures
Bivariate Pearson correlations between the primary sleep and circadian measures indicated that actigraphy-measured total sleep time (TST) was positively associated with actigraphy-measured sleep efficiency (SE) (r(129) = 0.28, p = 0.001), actigraphy-measured number of sleep periods (SP) (r(129) = 0.26, p = 0.003), and average self-reported TST (r(129) = 0.43, p < 0.001). Actigraphy-measured SE was positively associated with self-reported SE (r(127) = 0.19, p = 0.035). Actigraphy-measured number of SP was negatively associated with average self-reported TST (r(129) = − 0.18, p = 0.045) and self-reported SE (r(127) = -0.25, p = 0.005). Average self-reported TST was positively correlated with self-reported SE (r(146) = 0.44, p < 0.001).
Additionally, there was a significant negative association between DLMO phase and average self-reported TST (r(122) = − 0.27, p = 0.002) and between DLMO phase and MEQ (r(84) = − 0.33, p = 0.002), but DLMO phase was not significantly associated with any other primary sleep variable (i.e., TST, SE, and SP), all p’s > 0.05). MEQ was not associated with any other primary sleep variable (all p’s > 0.05).
Sex differences in sleep, circadian, and activity measures
There were significant sex differences in sleep and circadian measures (see Table 1). Specifically, there were significant sex differences in actigraphy-measured number of SP (F(2, 126) = 5.84, p = 0.017, η2 = 0.043), such that females evidenced a greater number of SP, and in DLMO phase (F(2, 120) = 8.40, p = 0.004, η2 = 0.065), whereby males showed a later DLMO phase. There also were significant sex differences in self-reported SE (F(2, 143) = 4.18, p = 0.043, η2 = 0.028), whereby females reported less SE than males. No significant sex differences were found for actigraphy-measured TST (F(2, 126) = 1.78, p = 0.185, η2 = 0.013), actigraphy-measured SE (F(2, 126) = 0.23, p = 0.630, η2 = 0.001), MEQ score (F(2, 101) = 0.00, p = 0.971, η2 = 0.000), actigraphy-measured activity counts (F(2, 119) = 1.10, p = 0.30, η2 = 0.01), or DLMO-sleep onset time phase angle (F(2, 121) = 0.49, p = 0.49, η2 = 0.004). Similarly, no significant sex differences were found in self-reported TST (F(2, 145) = 0.00, p = 0.973, η2 = 0.000).
Racial differences in sleep, circadian, and activity measures
There were significant racial differences in all sleep measures, but not in the circadian measures (see Table 2). Specifically, there were significant racial differences in actigraphy-measured TST (F(2, 97) = 5.44, p = 0.022, η2 = 0.053), SE (F(2, 97) = 6.97, p = 0.010, η2 = 0.067), and number of SP (F(2, 97) = 5.87, p = 0.017, η2 = 0.053). White participants showed more actigraphy-measured TST and SE, as well as fewer total SP, compared to Black participants. There also were significant racial differences in the self-reported sleep indices. In line with the actigraphy-measured sleep findings, White participants evidenced more self-reported TST (F(2, 113) = 13.86, p < 0.001, η2 = 0.107) and better SE (F(2, 112) = 15.33, p < 0.001, η2 = 0.120). There were no significant racial differences in the circadian measures of DLMO phase (F(2, 94) = 0.22, p = 0.638, η2 = 0.002) or MEQ (F(2, 82) = 0.08, p = 0.779, η2 = 0.001), in actigraphy-measured activity counts (F(2, 92) = 0.59, p = 0.45, η2 = 0.01), or DLMO-sleep onset time phase angle (F(2, 95) = 0.89, p = 0.35, η2 = 0.01).
Discussion
Our results show for the first time that sex and race both are significant predictors of several objective and self-reported sleep and circadian rhythm measures, controlling for BSD risk group differences, in a large sample of emerging adults participating in a naturalistic EMA study. Males exhibited later DLMO phase and fewer actigraphy-measured discrete sleep periods compared to females. Males also self-reported higher sleep efficiency than females. Actigraphy results indicated that White participants exhibited more total sleep time, better sleep efficiency, and fewer discrete sleep periods than Black participants. White participants also self-reported greater total sleep time and sleep efficiency compared to Black participants. Our study is the first to examine both objective and self-reported sleep and circadian parameters in a large, well-characterized, young adult sample. Furthermore, our findings represent a novel and meaningful contribution to the current literature, given that our measurement of sleep and circadian variables occurred in a naturalistic setting, allowing for external validity beyond what can be offered by laboratory studies. As such, the present findings address critical limitations of much of the previous literature (e.g., cross-sectional, mainly reliant on self-report, carried out in non-naturalistic laboratory settings), and thus inform ongoing research on sex and racial health disparities in sleep and in circadian rhythms.
With respect to actigraphy-measured sex differences in sleep, females in the current study exhibited more sleep periods than males, although their objective total sleep time and sleep efficiency did not differ. Our results contradict previous laboratory findings indicating that females objectively show longer sleep duration and better sleep efficiency than males7,8,10. It is possible that the measurement setting accounts for these differences, given that we measured sleep in a naturalistic setting, whereas previous studies were conducted in a laboratory. Perhaps females evince better sleep in the laboratory but encounter more environmental or social stressors in a naturalistic setting that prevent the same quality of sleep.
The current self-reported sex differences in sleep generally support previous findings indicating that males report fewer sleep problems and better sleep quality than females12,13. Our study results show that males self-reported better sleep efficiency, although their objective sleep efficiency did not differ. Inconsistencies between self-report and objective measures of sleep have been well documented in sleep research10,38. Given that females had more actigraphy-measured discrete sleep periods than males, it is possible that females perceived their sleep to be more fragmented, and thus poorer in quality, than did males.
Females in the current study also had earlier dim light melatonin onset times, indicating more phase advanced circadian rhythms, replicating earlier studies done in controlled lab environments9,16, and thus, generalizing these results to naturalistic settings, and thereby suggesting the sex difference in circadian rhythms is biological.
With respect to race, actigraphy findings demonstrated that Whites exhibited more total sleep time, better sleep efficiency, and fewer total sleep periods compared to Blacks. Self-reported racial differences in sleep fall in line with our objective measurements and with previous literature17,25; Whites in our study self-reported more sleep time and better sleep efficiency than Blacks. Our results support past findings demonstrating that Whites have better sleep efficiency than minority groups and corroborate existing evidence that Blacks sleep less overall, and exhibit less continuous sleep17,23,25. Despite evidence from previous research suggesting phase differences between Blacks and Whites15,32,33,34,35,36, there were no significant racial differences found for DLMO phase in the current study. Consistent with previous findings32, there were no significant racial differences for self-reported morningness-eveningness (chronotype).
Explanations for the observed racial disparities in sleep are likely complex. Given that some aspects of sleep have demonstrated heritability, genetic differences or other biological factors may exist that account for some racial differences in our findings31,32. However, it also is likely that a number of environmental and sociodemographic factors (e.g. stress, family burden, or neighborhood or economic effects) and health behaviors account for some racial differences in sleep duration and quality30,32. Given that sleep impacts many health outcomes (e.g., cognitive functioning, immune and hormone functioning, cardiovascular and mental health), future studies should strive to understand how genetic, environmental, sociodemographic, and mental health factors differentially contribute to racial differences and health disparities in sleep duration and quality.
The current study exhibits several notable strengths, including use of a well-characterized, representative, large emerging adult sample. Our young adult sample was demographically representative of a larger screened sample (N = 18,618) drawn from local high schools and universities in the Philadelphia, PA, USA region. These individuals were screened as part of the larger Teen Emotion and Motivation (TEAM) Project and selected based on high or moderate reward sensitivity. Indeed, there are benefits and drawbacks to conducting analyses with this specific sample. Noted benefits include the fact that our sample is demographically representative in terms of race and sex of young adults in a large metropolitan area, thus conferring high external validity to our findings, particularly compared to laboratory studies. Drawbacks include the fact that the sample was selected on the basis of high or low risk for developing BSD, thus limiting the generalizability of our findings to young adults more broadly. However, we controlled for BSD risk status in all analyses, removing the variance associated with BSD risk and decreasing the likelihoodthat BSD risk was a confound in our findings.
Our study also makes important contributions to understanding sleep and circadian function by utilizing both objective and self-report measures, allowing for a more accurate assessment of the constructs of interest in young adults’ daily lives. Employment of melatonin onset, actigraphy, and sleep diaries in a naturalistic environment allowed for a robust examination of sleep and circadian-related differences by sex and race. However, the study had some limitations. First, the analyses examining sleep differences by race were limited to White and Black participants, and behavioral reports were not used to constrain the sleep periods for the actigraphy data. Future research should examine other racial groups (e.g., Asian, American Indian, etc.) and add behavioral reports to corroborate the actigraphy data. In addition, future research should strive to replicate results with a view toward measuring latent variables, comparing objective and self-report sleep measurements more closely, and ultimately exploring race and sex-based differences in sleep and circadian characteristics in order to maximize the positive health outcomes associated with high quality sleep and circadian alignment.
Methods
Participants
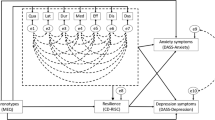
Participants were recruited from the TEAM Project, a prospective study that identifies factors related to the onset and course of bipolar spectrum disorder (BSD)39,40. Participants were recruited from Philadelphia-area high schools and universities and participated in a two-phase screening process. In Phase 1, adolescent participants (N = 18,618) were administered two measures assessing behavioral activation system (BAS) sensitivity, with students scoring in the upper 15th percentile on both measures categorized as High BAS (HBAS), and students scoring between the 40th and 60th percentiles categorized as Moderate BAS (MBAS). Students who were included in the HBAS and MBAS (n = 1,180) groups were invited for Phase II screening, where they were administered self-report questionnaires and a diagnostic interview to assess mood and psychotic disorders. Participants were excluded from the study if they met DSM-IV-TR (American Psychiatric Association, 2000) criteria for a BSD or a psychotic disorder, or if they were not sufficiently fluent in English. The study was approved by the Institutional Review Board at Temple University, and all methods were performed in accordance with the relevant guidelines and regulations. All participants provided written informed consent before participating in the study. Only procedures and measures relevant to the current study are described here.
A subset of participants from Project TEAM falling into three groups39,40 were invited to complete the current study. Participants were 43 individuals with high behavioral activation system (BAS)/reward sensitivity and bipolar spectrum disorder (BSD), 64 individuals with high BAS/reward sensitivity and no history of BSD, and 43 individuals with moderate BAS/reward sensitivity and no history of BSD. Overall, 150 emerging adults (Mage = 21.8 years old, SD = 2.11; range = 18.6–27.9; 88 female; 84 White, 34 Black, 15 Asian or Pacific Islander, and 12 other ethnicity (e.g., Mexican, Native American, Hispanic) participated in the study.
Measures
Objective sleep
To measure objective sleep parameters, participants wore an Actiwatch Spectrum (Philips Healthcare, Bend, OR), a well-validated motion-detecting device worn on the non-dominant wrist, continuously for 20 days, only removing it when it might get wet (e.g., bathing). Data were collected in 1-min epochs and scored using the Actiware software. Standard sleep parameters derived from actigraphy are moderately to strongly correlated with those derived from polysomnography in normal healthy sleepers41 and in clinical samples42,43. The following standard sleep parameters were derived from the actigraphy data: total sleep time (TST), the number of minutes spent asleep between bedtime and final arising; sleep efficiency (SE), the percentage of time spent asleep while in bed; and sleep periods (SP), the number of discrete sleep periods within a day.
Self-reported sleep
To assess self-reported sleep parameters, participants were asked to answer questions about their sleep for 20 consecutive days on electronic sleep diaries. The sleep diary is reliable44 and is considered the gold standard for measuring self-reported sleep–wake rhythms45. The following standard sleep parameters were derived from the self-report diary data: TST and SE, as defined above.
Activity
Actigraphy provides an objective, reliable and valid method for assessing activity patterns with minimal restrictions on normal routines46,47. Participants wore an Actiwatch Spectrum (described above) for continuous measurement of activity level. Actiwatches recorded the number of times a participant moved their wrist; this has been shown to be a validated proxy for overall physical activity level48. We took a daily average of the number of times a participant moved their wrist (activity count) and averaged this over the 20-day study period.
Chronotype
The Morningness-Eveningness Questionnaire (MEQ)37 was administered to assess chronotype. It is a 19-item self-report well-validated measure of the morningness-eveningness dimension, with reliability coefficients ranging from 0.78 to 0.86 across samples in several countries49,50,51.
Dim light melatonin onset (DLMO)
Participants completed the DLMO procedure on 3 evenings during the EMA study: day 1, day 10, and day 20. Participants provided 10 saliva samples at 30-min intervals at home wearing light-attenuating goggles (Noir Medical Technologies, South Lyon, MI) beginning 5 h before their habitual bedtime. Participants were instructed to finish dinner at least 30 min before sampling began. No food was allowed during sampling and water was permitted only within 5 min after each sample. Nonsteroidal anti-inflammatory drugs (NSAID) were prohibited during the protocol, and alcohol and caffeine were prohibited for > 24 h before each DLMO procedure. Saliva (1.0–3.0 ml) was deposited into Salivette tubes using absorbent polyester swabs placed in the mouth for 5 min. Salivettes were refrigerated immediately and collected for continued storage at −20 °C in the laboratory pending assay. DLMO, a reliable marker of circadian phase52,53 was defined as the first interpolated point (derived from between two points) at 3.0 pg/ml on the rising curve of melatonin concentration. Melatonin was assayed with ELISA. The minimum detectable limit of the assay was 0.5 pg/ml with intra- and inter-assay coefficients of variation of 6.8% and 7.3%, respectively; 10% of samples were run in duplicate for quality control. DLMO-sleep onset time phase angle was calculated by subtracting DLMO onset clock time from sleep onset clock time.
Statistical analysis
To ensure enough power to detect an effect, prior to collecting data for the study, power analyses were conducted with the G*Power 3.1 program54. We conducted a power analysis for ANCOVA with fixed effects. To detect significant main effects of sex and race, given Power (1 − β) = 0.80 and α = 0.05 to detect a medium effect, a total sample size of N = 90 is required. Thus, the analyses should be adequately powered to detect an effect.
Bivariate Pearson correlations (two-tailed, p < 0.05 significance level) were conducted between the primary sleep and circadian measures. We examined the associations between sex/race and group membership (moderate behavioral activation, high behavioral activation without BSD, and high behavioral activation with BSD). Pearson Chi-square Tests of Independence revealed that sex and group membership were not significantly associated (χ2(2) = 1.93, p = 0.38), whereas race and group membership were significantly related (χ2(2) = 6.82, p = 0.03). Thus, in all of our main analyses, we chose to control for group membership in order to mitigate the fact that there may be a pre-existing association between race and group membership. A series of ANCOVAs, controlling for initial group status, were conducted to evaluate differences on sleep, circadian, and activity characteristics by sex and race (p < 0.05 significance level). The actigraphy-measured and self-report sleep variables (TST, SP, and SE) were averaged over the 20-day study period, as were actigraphy-measured activity counts, which resulted in a single score for each measure. The DLMO was averaged over three time points (day 1, day 10, and day 20) to derive a single score. The MEQ was measured at baseline. For the analyses involving race, White participants were compared to Black participants. The sample sizes were too small to conduct comparisons among other races (e.g., Asian, Pacific Islander, American Indian/Alaskan Native).
Data availability
The dataset generated and analyzed during the current study is available from Dr. Lauren Alloy on a reasonable request.
References
Alvarez, G. G. & Ayas, N. T. The impact of daily sleep duration on health: a review of the literature. Prog. Cardiovasc. Nurs.19, 56–59 (2007).
Watson, N. F. et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep38, 1161–1183 (2015).
Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. Short sleep duration among US adults. https://www.cdc.gov/sleep/data_statistics.html. (2017).
Ford, E. S., Cunningham, T. J. & Croft, J. B. Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep38, 829–832 (2015).
Brainard, J., Gobel, M., Scott, B., Koeppen, M. & Eckle, T. Health implications of disrupted circadian rhythms and the potential for daylight as therapy. Anesthesiology122, 1170–1175 (2015).
Alloy, L. B., Ng, T. H., Titone, M. K. & Boland, E. M. Circadian rhythm dysregulation in bipolar spectrum disorders. Curr. Psychiatry Rep.19, 1–10 (2017).
Goel, N., Kim, H. & Lao, R. P. Gender differences in polysomnographic sleep in young healthy sleepers. Chronobiol. Int.22, 905–915 (2005).
Santhi, N. et al. Sex differences in the circadian regulation of sleep and waking cognition in humans. Proc. Natl. Acad. Sci.113, E2730–E2739 (2016).
Van Reen, E. et al. Sex of college students moderates associations among bedtime, time in bed, and circadian phase angle. J. Biol. Rhythms28, 425–431 (2013).
Short, M. A., Gradisar, M., Lack, L. C., Wright, H. & Carskadon, M. A. The discrepancy between actigraphic and sleep diary measures of sleep in adolescents. Sleep Med.13, 378–384 (2012).
Hinz, A. et al. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med.30, 57–63 (2017).
Burgard, S. A. The needs of others: gender and sleep interruptions for caregiving. Soc. Forces.89, 1189–1215 (2011).
Maume, D. J., Sebastian, R. A. & Bardo, A. R. Gender differences in sleep disruption among retail food workers. Am. Sociol. Rev.74, 989–1007 (2009).
Duffy, J. F. et al. Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc. Natl. Acad. Sci.108, 15602–15608 (2011).
Eastman, C. I., Tomaka, V. A. & Crowley, S. J. Sex and ancestry determine the free-running circadian period. J Sleep Res.26, 547–550 (2017).
Cain, S. W. et al. Sex differences in phase angle of entrainment and melatonin amplitude in humans. J. Biol. Rhythms25, 288–296 (2010).
Mezick, E. J. et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE Project. Psychosom. Med.70, 410–416 (2008).
Profant, J., Ancoli-Israel, S. & Dimsdale, J. E. Are there ethnic differences in sleep architecture?. Am. J. Hum. Biol.14, 321–326 (2002).
Rao, U. et al. Relationship between ethnicity and sleep patterns in normal controls: implications for psychopathology and treatment. J. Psychiatr. Res.33, 419–426 (1999).
Stepnowsky, C. J., Moore, P. J. & Dimsdale, J. E. Effect of ethnicity on sleep: complexities for epidemiologic research. Sleep26, 329–332 (2003).
Thomas, K. S., Bardwell, W. A., Ancoli-Israel, S. & Dimsdale, J. E. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychol.25, 635–642 (2006).
Adenekan, B. et al. Sleep in America: role of racial/ethnic differences. Sleep Med. Rev.17, 255–262 (2013).
Durrence, H. H. & Lichstein, K. L. The sleep of African Americans: a comparative review. Behav. Sleep Med.4, 29–44 (2006).
Hall, M. H. et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep32, 73–82 (2009).
Ruiter, M. E., Decoster, J., Jacobs, L. & Lichstein, K. L. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep Med.12, 209–214 (2011).
Hale, L. & Do, D. P. Racial differences in self-reports of sleep duration in a population-based study. Sleep30, 1096–1103 (2007).
Nunes, J. et al. Sleep duration among black and white Americans: results of the National Health Interview Survey. J. Natl. Med. Assoc.100, 317–322 (2008).
Whinnery, J., Jackson, N., Rattanaumpawan, P. & Grandner, M. A. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep37, 601–611 (2014).
Lauderdale, D. S. et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am. J. Epidemiol.164, 5–16 (2006).
Chen, X. et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep38, 877–888 (2015).
Egan, K. J. et al. The role of race and ethnicity in sleep, circadian rhythms and cardiovascular health. Sleep Med. Rev.33, 70–78 (2017).
Prasad, B., Saxena, R., Goel, N. & Patel, S. R. Genetic ancestry for sleep research: leveraging health inequalities to identify causal genetic variants. Chest153, 1478–1496 (2018).
Eastman, C. I., Molina, T. A., Dziepak, M. E. & Smith, M. R. Blacks (African Americans) have shorter free-running circadian periods than whites (Caucasian Americans). Chronobiol. Int.29, 1072–1077 (2012).
Eastman, C. I., Suh, C., Tomaka, V. A. & Crowley, S. J. Circadian rhythm phase shifts and endogenous free-running circadian period differ between African-Americans and European-Americans. Sci. Rep.5, 1–8 (2015).
Eastman, C. I., Tomaka, V. A. & Crowley, S. J. Circadian rhythms of European and African-Americans after a large delay of sleep as in jet lag and night work. Sci. Rep.6, 1–11 (2016).
Smith, M. R., Burgess, H. J., Fogg, L. F. & Eastman, C. I. Racial differences in the human endogenous circadian period. PLoS ONE4, 1–6 (2009).
Horne, J. A. & Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness. Int. J. Chronobiol.4, 97–110 (1976).
Silva, G. E. et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS). J. Clin. Sleep Med.3, 622–630 (2007).
Alloy, L. B. et al. High Behavioral Approach System (BAS) sensitivity, reward responsiveness, and goal-striving predict first onset of bipolar spectrum disorders: a prospective behavioral high-risk design. J. Abnorm. Psychol.121, 339–351 (2012).
Alloy, L. B. et al. Progression along the bipolar spectrum: a longitudinal study of predictors of conversion from bipolar spectrum conditions to bipolar I and II disorders. J Abnorm. Psychol.121, 16–27 (2012).
Cole, R. J., Kripke, D. F., Gruen, W., Mullaney, D. J. & Gillin, J. C. Automatic sleep/wake identification from wrist activity. Sleep15, 461–469 (1992).
Kaplan, K. A., Talbot, L. S., Gruber, J. & Harvey, A. G. Evaluating sleep in bipolar disorder: comparison between actigraphy, polysomnography, and sleep diary. Bipolar Disord.14, 870–879 (2012).
Ng, T. H. et al. Sleep–wake disturbance in interepisode bipolar disorder and high-risk individuals: a systematic review and meta-analysis. Sleep Med. Rev.20, 46–58 (2015).
Morin, C. M., & Espie, CA. Insomnia: A Clinician’s Guide to Assessment and Treatment. (Springer, 2003).
Buysse, D. J., Ancoli-Israel, S., Edinger, J. D., Lichstein, K. L. & Morin, C. M. Recommendations for a standard research assessment of insomnia. Sleep29, 1155–1173 (2006).
Ancoli-Israel, S. et al. The role of actigraphy in the study of sleep and circadian rhythms. Sleep26, 342–392 (2003).
Sadeh, A. The role of actigraphy in sleep medicine. Sleep Med. Rev.6, 113–124 (1995).
Neil-Sztramko, S. E., Rafn, B. S., Gotay, C. C., & Campbell, K L. Determining activity count cut-points for measurement of physical activity using the Actiwatch2 accelerometer. Physiol. Behav.173, 95–100 (2017).
Adan, A. & Natale, V. Gender differences in morningness–eveningness preference. Chronobiol. Int.19, 709–720 (2002).
Chelminski, I., Ferraro, F. R., Petros, T. & Plaud, J. J. Horne and Ostberg questionnaire: a score distribution in a large sample of young adults. Pers. Individ. Dif.23, 647–652 (1997).
Neubauer, A. C. Psychometric comparison of two circadian rhythm questionnaires and their relationship with personality. Pers. Individ. Dif.13, 125–131 (1992).
Goel, N. Late-night presentation of an auditory stimulus phase delays human circadian rhythms. Am. J. Physiol. Regul. Integr. Comp. Physiol.289, R209–R216 (2005).
Goel, N. An arousing musically-enhanced bird song stimulus mediates circadian rhythm phase advances in dim light. Am. J. Physiol. Regul. Integr. Comp. Physiol.291, R822–R827 (2006).
Faul, F., Erdfelder, E., Lang, A.-G. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods39, 175–191 (2007).
Acknowledgements
This research was supported by National Institutes of Health grants MH77908 and MH102310 to Lauren B. Alloy. Brae Anne McArthur was supported by a Banting Postdoctoral Fellowship from the Social Sciences and Humanities Research Council. Taylor A. Burke was supported by a National Science Foundation Graduate Student Research Fellowship. Namni Goel was supported in part by National Aeronautics and Space Administration (NASA) grants NNX14AN49G and 80NSSC20K0243 and National Institutes of Health grant R01DK117488.
Author information
Authors and Affiliations
Contributions
B.M., N.G. and L.A. contributed to conception and design. M.T., T.N., and T.B. acquired the data. M.T., T.N., T.B., L.Mac., and L.Mc. cleaned and prepared the data. B.M. and M.T. analyzed the data. M.T., B.M., N.G. and L.A. contributed to interpretation of data. B.M., M.T., T.N., T.B., and L.Mac. drafted the article. N.G. and L.A. critically reviewed the manuscript for important intellectual content and provided supervision. L.A. and N.G. obtained funding. All authors revised the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Titone, M.K., McArthur, B.A., Ng, T.H. et al. Sex and race influence objective and self-report sleep and circadian measures in emerging adults independently of risk for bipolar spectrum disorder. Sci Rep 10, 13731 (2020). https://doi.org/10.1038/s41598-020-70750-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70750-3
This article is cited by
-
Sleep disturbances in the context of neurohormonal dysregulation in patients with bipolar disorder
International Journal of Bipolar Disorders (2022)
-
Demographic characteristics associated with circadian rest-activity rhythm patterns: a cross-sectional study
International Journal of Behavioral Nutrition and Physical Activity (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.