Abstract
The human immunodeficiency virus (HIV) remains a leading cause of maternal morbidity and mortality in Sub-Saharan Africa. Prevention of mother-to-child transmission (PMTCT) has proven an effective strategy to end paediatric infections and ensure HIV-infected mothers access treatment. Based on cross-sectional data collected from June 2008 to May 2013, we assessed changes in HIV prevalence, risk factors for HIV, provision of PMTCT antiretroviral treatment (ART), and the association between HIV infection, birth outcomes and maternal characteristics at the Simão Mendes National Hospital, Guinea-Bissau’s largest maternity ward. Among 24,107 women, the HIV prevalence was 3.3% for HIV-1, 0.8% for HIV-2 and 0.9% for HIV-1/2. A significant decline in HIV-1, HIV-2, and HIV-1/2 prevalence was observed over time. HIV infection was associated with age and ethnicity. A total of 85% of HIV-infected women received ART as part of PMTCT, yet overall treatment coverage during labour and delivery declined significantly for both mothers and infants. Twenty-two percent of infants did not receive treatment, and 67% of HIV-2-infected mothers and 77% of their infants received ineffective non-nucleoside reverse transcriptase inhibitors for PMTCT. Maternal HIV was associated with low birth weight but not stillbirth. Inadequate continuity of care and ART coverage present challenges to optimal PMTCT in Guinea-Bissau.
Similar content being viewed by others
Introduction
Despite remarkable progress over the past decade, Sub-Saharan Africa (SSA) continues to have the highest global prevalence of HIV. Women remain disproportionately at risk of acquiring HIV, with an estimated 59% of all new infections occurring amongst females1. Furthermore, HIV remains one of the leading causes of mortality among women of reproductive age in the region2. In 2017, an estimated 1.3 million pregnant women were living with HIV, and 130,000 infants were infected with HIV in SSA3.
Approximately 90% of all new paediatric infections occur during the perinatal period, of which 50% occur in relation to labour and delivery4,5. Antiretroviral treatment (ART) as part of prevention of mother-to-child transmission (PMTCT) is a key strategy to combat the African HIV epidemic and decreases vertical transmission rates from as high as 45% to < 5% in breastfeeding populations6. PMTCT has yielded remarkable results, with an estimated 93% of pregnant women in eastern and southern Africa living with HIV receiving antiretroviral prophylaxis, resulting in mother-to-child transmission rates of less than 10%. Nevertheless, western and central Africa appear to lag behind, with fewer than half (48%) of pregnant women living with HIV in 2017 receiving PMTCT services1.
Guinea-Bissau is a West African country populated with 1.8 million inhabitants, of which 400,000 reside in the capital Bissau. According to the joint United Nations programme on HIV/AIDS (UNAIDS), 3.4% (95% CI 2.6–3.8) of the population in Guinea-Bissau is infected with HIV (UNAIDS, 2018c), yet the true number may be notably higher considering that HIV prevalence in the country’s capital is 6.7%7. A previous study among pregnant women conducted from 2002 to 2006 found that 5.7% were HIV-1 infected, and 2.4% were HIV-2 infected, including 0.7% HIV-1/2 dually infected women8.
The Ministry of Health in Guinea-Bissau implemented a national HIV program in 2005, providing free of charge ART. Yet, more than a decade later, the country remains far from achieving the 90–90–90 targets1. The delivery of HIV treatment has been impeded by numerous barriers including political instability, frequent HIV clinic relocations and inadequate drug supply resulting in treatment interruptions9. In addition, poor laboratory capacity, inadequate validation of HIV rapid tests, repeated unavailability of CD4 cell count measurements, and lack of access to HIV-RNA measurement have delayed initiation of ART and led to the identification of treatment failure9,10. As a result, UNAIDS estimated that only 32% of adults in the country accessed antiretroviral therapy in 201811.
PMTCT counselling and testing has been available at selected antenatal clinics (ANC) in Bissau since 20028. Between October 2007 and April 2013, 86% of pregnant women had at least one antenatal visit, but only 54% attended all four recommended visits in Bissau. In addition, only 29% of women in rural areas and 69% of women in urban settings delivered at health facilities in the country12. Previous qualitative research from Guinea-Bissau has shown that a lack of HIV and PMTCT knowledge, customary and cultural beliefs associated with HIV and ill health, HIV stigma and discrimination, and fear of partnership dissolution were common barriers to PMTCT13. In addition, a study exploring peripartum opt-out testing found that regular stock interruptions and political instability negatively affected the provision of PMTCT14. High rates of early mortality and loss to follow-up have recently been described among HIV-infected children (< 15 years of age) in Guinea-Bissau. Based on a study of 525 HIV-infected children, 11% died and 39% were lost to follow-up within the first year of follow-up, highlighting continuous challenges with implementing sustainable PMTCT services15. Consequently, there remains a paucity of research exploring the delivery of PMTCT services with the overall aim of improving treatment and care for HIV-infected mothers and their children in Guinea Bissau.
In this retrospective study, we assessed changes in HIV-1 and HIV-2 prevalence, factors associated with HIV infection, birth outcomes and the provision of ART as part of PMTCT services over a 5-year period at the national maternity ward in Bissau, Guinea-Bissau.
Methods
Study setting
The study was conducted by the Bandim Health Project (BHP) (https://www.bandim.org) at the Simão Mendes National Hospital (HNSM) maternity ward located in Bissau. The BHP, a health and demographic surveillance site present in Guinea-Bissau for 4 decades, routinely collects demographic and clinical data on all deliveries at HSNM. This public facility is the principal provider of comprehensive obstetric care in Guinea-Bissau, and approximately 90% of women who deliver at the facility are residents of the country’s capital, Bissau.
From June 2008 onwards, opt-out HIV counselling and testing has been offered to women admitted to the maternity ward for the management of labour- and delivery- and/or pregnancy-related complications when HIV tests were available. HIV testing and ART were free of charge and provided by the Guinean Ministry of Health, but all women paid a flat fee of 2000 XOF (3–4 USD) to give birth at HNSM14. All newly diagnosed women and their infants were referred to the Italian-Guinean NGO-clinic, Ceu e Terras, or to other local HIV centres for follow-up, counselling, and further PMTCT ART13. Data registration of testing for HIV at delivery ceased in May 2013 due to funding constraints. While HIV testing at labour and delivery was national policy at the time of the study, not all women were tested. We have previously described the characteristics of women tested compared with those not tested 14.
Study design and participants
We conducted a retrospective cross-sectional survey exploring HIV prevalence, risk factors for HIV, treatment provision, and birth outcomes (low birth weight, LBW, and stillbirth), drawing on data routinely collected through the BHP surveillance system at HNSM from June 2008 until May 2013. All women presenting to HNSM for delivery or immediate postpartum care who had been tested for HIV were included in this study.
Data collection
Data were recorded in the HNSM maternity ward registration system and included basic socio-demographic and clinical data. Data cleaning was performed daily (including weekends) by trained research assistants from BHP who also collected supplementary demographic and clinical information using separate case report forms (CRFs). We have previously described the data collected in detail14,16. During the study period, it was national policy that hospital midwives offer immediate HIV counselling and testing to all women presenting to the maternity for delivery or, as many women had not attended ANC or did not receive PMTCT testing or counselling during pregnancy. Midwives had been trained to complete a short CRF as part of the counselling and testing routine to collect data on previous HIV testing, known sero-status, and ART use14.
HIV testing
HIV screening was performed using the Determine® HIV-1/2 rapid test (Abbot Diagnostics, Maidenhead, United Kingdom). To confirm infection and to discriminate between HIV types, women with positive and inconclusive screening results were subsequently tested with another rapid test, SD Bioline HIV-1/2 3.0 (Standard Diagnostics, Kyonggi-do, South Korea).
HIV treatment regimens
Provision of PMTCT at the initiation of this survey was guided by the 2006 World Health Organization (WHO) recommendations, i.e., ART prophylaxis in the third trimester (28 weeks) of pregnancy consisting of a regimen of twice daily Zidovudine (AZT), single-dose nevirapine (sd NVP) at onset of labour and Zidovudine plus Lamivudine (AZT + 3TC) for 1 week from birth. Women diagnosed in labour were given a single-dose nevirapine followed by AZT + 3TC for 1 week starting in labour. For women who needed treatment for their own health, triple ART (cART) was initiated as soon as possible. For HIV-2 and HIV-1/2 dually infected mothers, a combination of (AZT + 3TC) + Lopinavir/Ritonavir was recommended. For infants, guidelines recommended sd NVP plus AZT twice a day for either 4 weeks if the mother had received less than 4 weeks AZT prophylaxis prior to labour or for 1 week if the mother had received at least 4 weeks AZT prophylaxis. Infants of mothers receiving cART were recommended AZT twice daily17. After 2010, in line with the revised WHO recommendations, all pregnant women with CD4 count levels < 350 cells/mm3, irrespective of clinical stage, and women with a WHO clinical stage 3 or 4 infection, were started on triple ART. In addition, women not receiving ART for their own health, received (Option A) prophylaxis with AZT as monotherapy from as early as 14 weeks of pregnancy plus a single dose NVP + AZT + 3TC during labour and delivery followed by AZT + 3TC for 7 days after delivery, or triple ART prophylaxis (Option B) from as early as 14 weeks of pregnancy. The infant regime consisted of daily NVP from birth for a minimum of 4–6 weeks, and until 1 week after all exposure to breastmilk had ended. For infants receiving replacement feeding only daily NVP or sd NVP + daily AZT from birth and until 4–6 weeks of age was recommended18. Due to logistical issues, treatment was often started without CD4 cell count measurements based on clinical assessment. Throughout the study period, repeated stock outages and lack of ART at times forced clinicians to switch treatment and often to provide more simple regimes than recommended9, 19. In 2015, Guinea-Bissau began implementing option B+, i.e., lifelong ART from diagnosis20,21.
Statistical methods
Maternity and HIV testing data were entered in password-secured databases (dBase 5.0, dataBased Inc, Vestal, NY, USA; Microsoft Access 2007, Microsoft, Redmond, WA, USA), and datasets were merged using unique birth numbers. The data were analysed using Stata 14.0 (Stata Corporation, College Station, TX, USA). Outcome variables such as LBW and stillbirths were dichotomized (0 = absent, 1 = present). Continuous explanatory variables were grouped categorically. Factors associated with HIV serostatus and birth outcomes were determined using univariate and multivariate logistical regression models. The multivariate analysis was fitted with statistically significant covariates (as determined by Wald’s test). Birth outcomes i.e., stillbirths and low birthweight (LBW) were examined according to HIV status and adjusted for significant covariates. In accordance with the WHO criteria, stillbirth was defined as a newborn at or above 1,000 g showing no vital signs immediately after birth (Apgar score = 0)22. Low birth weight was defined as birth weight of < 2,500 g23. Miscarriages (birth weight < 1,000 g) were excluded. In the birth outcome analysis, “births” pertain to the number of fetuses at risk. Therefore, the number of total births is higher than the number of pregnant women due to multiple pregnancies. In the logistic regression models, adjustment for birth outcomes was made for clustering of twins using a specific pair number. Inconclusive test results were categorized as HIV-negative. Missing values were included in the logistic regression models. Trends over time (calendar year) for HIV prevalence and treatment were determined using Pearson’s χ2 test. Due to a lack of data to confirm self-reported antenatal treatment regimens and reasons for selecting a given treatment at labour, we opted to assess antenatal and treatment at labour separately. A p value of < 0.05 was considered significant.
Ethical considerations
All patient data were fully anonymised before being accessed. The use of government surveillance maternity data was approved by the National Ethical Committee in Guinea-Bissau (CNES-2010-018). A separate ethical approval was obtained for the analysis of HIV data and linkage of delivery and HIV databases (CNES-2011-030). The study was carried out in accordance with Guinea-Bissau Medical Research Ethics Committee requirements and the Helsinki declaration. All participants were counselled and asked for verbal informed consent before data collection and HIV testing. Newly diagnosed women were offered ART at labour and subsequently referred for follow-up. The manuscript was prepared in accordance with the STROBE guidelines (Supplemental Checklist 1).
Results
Participant characteristics
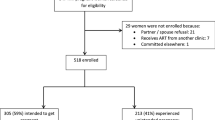
From June 2008 to May 2013, a total of 31,443 women presented to the HNSM maternity ward for delivery and/or pregnancy-related care, of which 77% (n = 24,107) were tested for HIV (Fig. 1). The median age of women was 24 years (inter-quartile range [IQR] 20–29, range 13–49). The principal ethnic groups were the Balanta (23%) and the Fula (22%). Forty-five percent of women had no or little (primary) education, and 19% reported a polygamous marriage (Table 1).
Prevalence of HIV
A total of 5.1% (1,232/24,107) of women were infected with HIV. The overall prevalence of HIV-1 was 3.3% (95% CI 3.1–3.5), the HIV-2 prevalence was 0.8% (95% CI 0.7–0.9), and HIV-1/2 dually infected women accounted for 0.9% (95% CI 0.8–1.1). Nineteen women who tested positive did not have the HIV type discriminatory test performed (Fig. 1).
Among women tested at birth, 47% (11,233/24,107) reported prior HIV testing during antenatal visits. Among them, 5.0% (566/11,233) were HIV positive, 93% (10,444/11,233) were HIV negative, 0.1% (9/11,233) were indeterminate and 1.9% (214/11,233) could not remember. Comparing self-reported and observed HIV test results, we found that 3.4% (19/566) of women with self-reported HIV-positive status tested HIV negative in labour, and 1.9% (197/10,444) of self-reported HIV negative women were HIV positive at delivery. Of the women who could not remember their HIV status, 15% (32/214) were HIV positive.
Variations in HIV-1 and HIV-2 prevalence
There was a significant decline in HIV-1 prevalence from 4.0% (95% CI 3.5–4.6) in 2009 to 2.5% (95% CI 1.8–3.3) in 2013, p < 0.024. HIV-2 prevalence declined from 1.2% (95% CI 0.9–1.5) in 2009 to 0.5% (95% CI 0.2–0.8) in 2013, p < 0.017 (Fig. 2). Exploring changes in HIV prevalence by age groups, we observed that the decline in HIV-1 and HIV-1/2 prevalence was largely confined to older women (aged ≥ 25 years), while the decline in HIV-2 prevalence was independent of age (Supplemental Figure 1).
Prevalence of HIV-1 and HIV-2 in pregnant women by calendar year, Simão Mendes National Hospital, Bissau, Guinea-Bissau, 2008–2013. The figure displays the changes in HIV-1 (a), HIV-2 (b), and HIV-1/2 (c) prevalence (point estimates and corresponding 95% confidence intervals) among pregnant women presenting for birth by calendar year. HIV-1, HIV-2 and HIV-1/2 all declined significantly from 2009 to 2013 (chi2 test for trend).
Risk determinants of HIV-1 and HIV-2 infection
Based on univariate analysis, we found maternal age, marital status, parity, and calendar year were associated with HIV-1, HIV-2 and HIV-1/2. Surprisingly, education was not significantly associated with HIV status and was therefore excluded from the multivariate analysis. As expected, the risk of HIV-1 increased significantly with age in the multivariate model (Table 2). Women belonging to the Balanta [adjusted odds ratio [AOR] 1.41 (95% CI 1.09–1.82)], Fula [1.33 (95% CI 1.02–1.73)] and Mandinga [1.37 (95% CI 1.01–1.86)] ethnic groups, and women from smaller ethnic groups or non-Guinean heritage [2.08 (95% CI 1.60–2.70)], had a higher HIV-1 prevalence compared with the Pepel ethnic group. For HIV-2, only age was significantly associated with HIV infection. Lastly, we found age, the Mandinga ethnicity and calendar year were associated with HIV-1/2 (Table 2).
ART and PMTCT regimens
Of women diagnosed antenatally (N = 566), 70% (396/566) reported receiving AZT prophylaxis, while 11% (62/566) reported receiving cART. Nineteen percent (108/566) reported that they were not receiving treatment or could not remember. Among women diagnosed in labour and women reporting no antenatal ART, 19% (149/774) received cART, 14% (108/774) received AZT prophylaxis plus a sd NVP + initiation of 3TC + AZT at childbirth, while 52% (408/774) of women, first diagnosed at delivery, received only sd NVP. Fourteen percent (109/774) did not receive any treatment at delivery. For women with HIV-2 (n = 196), 39% (76/196) received prophylaxis AZT plus a single dose-NVP + initiation of 3TC + AZT at childbirth, while 28% (55/196) received sd NVP only. Among women aware of their HIV status prior to labour and delivery, we observed a significant increase in self-reported antenatal treatment coverage from 60% in 2008 to 85% in 2013, p < 0.001. Specifically, there was an increase in women receiving antenatal AZT prophylaxis from 55% in 2008 to 82% in 2013, while there was no overall increase in cART during the same period (Fig. 3a). For women diagnosed at delivery and HIV-positive women not receiving antenatal ART (excluding women already on treatment, n = 458), overall treatment coverage declined from 99% in 2008 to 50% in 2013, p < 0.001. Notably, the proportion of women not receiving treatment at birth increased steadily throughout the study period (Fig. 3b). Figure 3 shows the provision of self-reported antenatal treatment and treatment at birth among HIV-infected women at the HNSM. During the study period, 85% of all HIV-infected women (1,049/1,232) received some form of ART in relation to labour for PMTCT. The majority (34%, n = 418) received option A, 33% (n = 408) received sd NVP, 18% (n = 223) received triple ART and 15% (n = 183) did not receive any treatment. As with women diagnosed at delivery, we observed a steady increase in the number of women not receiving any treatment despite including women diagnosed antenatally (Fig. 4).
Self-reported antenatal treatment (a) and treatment provided at birth (b) by calendar year, Simão Mendes National Hospital, Bissau, Guinea-Bissau, 2008–2013. cART combined antiretroviral therapy, AZT Zidovudine, 3TC Lamivudine, sd NVP single-dose Nevirapine. (a) Self-reported treatment regimens received by HIV-positive women presenting for labour by calendar year (N = 566). As shown, the percentage of women receiving AZT prophylaxis increased between 2008 and 2013, while the percentage of women on cART increased slightly from 2008 to 2011 and declined thereafter. (b) The provision of antiretroviral treatment at birth by calendar year, excluding women who reported initiating ART during the antenatal period (N = 774). The figure shows that the proportion of women receiving combined antiretroviral treatment increased steadily between 2009 and 2012, yet the percentage decreased between 2012 and the first quarter of 2013. Conversely, a decline in women receiving option A [AZT prophylaxis + (AZT + 3TC and sd NVP at labour)] between 2008 and 2013 was observed. Women receiving only sd NVP declined notably, suggesting that more women were initiated on treatment before labour. During the same period, we observed a notable increase in the number of HIV-infected women not receiving treatment at delivery. The p values shown were estimated using the chi2 test for trend.
The provision of antiretroviral treatment for all HIV-infected women by calendar year, Simão Mendes National Hospital, Bissau, Guinea-Bissau, 2008–2013. cART combined antiretroviral therapy, AZT Zidovudine, 3TC Lamivudine, sd NVP single-dose Nevirapine. The figure displays the provision of antiretroviral treatment at birth by calendar year for all HIV women in this study (N = 1,232). Overall coverage for cART and option A (AZT + 3TC + sd NVP) remained relatively low throughout the study period. There was a decline in the number of women receiving sd NVP, while the overall number of women not receiving any treatment increased over time. The p value shown was estimated using the chi2 test for trend.
Among infants of HIV-infected mothers (including twins and triplets), 8% (103/1,275) received the recommended treatment of sd NVP followed by AZT treatment, 70% (891/1,275) received sd NVP, and 22% (281/1,275) did not receive any treatment. Among infants of HIV-2 infected mothers, 77% (156/202) received sd NVP or sd NVP followed by AZT. The number of infants not receiving treatment to prevent mother-to-child transmission increased from 7% in 2008 to 36% in 2013, p < 0.001 (Supplemental Figure 2).
Birth outcomes
Seventeen percent (4,213/25,232) of births were LBW, and 10% (2,513/25,256) of babies were stillborn. Factors independently associated with LBW and stillbirths are displayed in Supplemental Table 1. We found no association between antenatal treatment and birth outcomes. Assessing birth outcomes for HIV-1, HIV-2 and HIV-1/2 dually infected women compared with HIV negative women, we found that maternal HIV-1 and HIV-1/2 co-infection were associated with LBW, AOR 1.25 (95% CI 1.03–1.52) and AOR 1.73 (95% CI 1.26–2.37), respectively (Table 3). No significant association was found between HIV status and stillbirth in univariate or multivariate analyses (Table 4).
Discussion
This retrospective cross-sectional study examined HIV-1 and HIV-2 prevalence and factors associated with HIV, PMTCT treatment coverage and adverse birth outcomes at the largest maternity ward in Guinea-Bissau. It shows a decline in HIV-1, HIV-2, HIV-1/2 prevalence among pregnant women presenting for labour during a 5-year period. Women from the Balanta and Fula ethnic groups had a significantly higher risk of HIV-1. Antenatal treatment coverage appears to be improving over time, yet an increase in the proportion of mothers and infants not receiving treatment at birth was observed, inevitably increasing the overall risk of mother-to-child transmission. This is specifically alarming as nearly half of the women were unaware of their HIV status prior to presenting for labour. Over the 5-year period, 15% of HIV-infected mothers and 22% of infants born to HIV-infected mothers did not receive any treatment. In addition, 67% of mothers with HIV-2 received NVP, which is ineffective against HIV-2 infection. Lastly, infants born to mothers with HIV-1 or HIV-1/2 dually infected were at risk of being LBW.
The HIV-2 prevalence of 0.8% in this survey was notably lower than in previous surveys among pregnant women, suggesting a continuing decline in HIV-2 prevalence in Guinea-Bissau8,24,25,26. A national survey from 2013 conducted in all 10 regions of the country reported an HIV-2 (including HIV-1 co-infected) prevalence of 1.0% (95% CI 0.5–1.8)27. In addition, a recently published study from the Bandim Health Project demographic surveillance site found an HIV-2 prevalence of 1.5% among younger women (aged 15–44 years)7. Changes in risk behaviour over the past decades and competitive exclusion have been proposed as explanations28,29. Modelling predicts that new HIV-2 cases in the country will cease within a few decades 30. In contrast, previous surveys from Guinea-Bissau have shown increasing or stabilized HIV-1 prevalence among a range of populations7,24,26,31. Gianelli et al.8 found that HIV-1 prevalence among pregnant women stabilized between 2003 and 2006. Our study is supported by findings from a recent national survey suggesting that the HIV-1 prevalence has stabilized and may be declining among women of reproductive age27. The risk of HIV transmission decreases substantially with ART32, and the decline in HIV-1 and HIV-2 may in part reflect the fruits of national interventions, including efforts to strengthen prevention measures during the roll-out of ART. Nevertheless, inadequate health infrastructure, repeated drug stock outages, poor adherence, and high rates of loss to follow in Guinea-Bissau increase the risk of treatment failure7,10,14,33,34,35 and thus infectivity, which could reverse current encouraging trends in HIV prevalence. Sustained and sustainable long-term management of affected patients, combined with prevention, is required10.
The Mandinga and Fula, two important West African ethnic groups, had a significantly higher prevalence of HIV-1 compared with other ethnic groups. A study by Kenyon et al.36 has suggested that differences in sexual behaviour according to ethnic group may contribute to a large variation in HIV prevalence. Previous research from Guinea-Bissau has suggested that female genital mutilation and polygamy among these ethnicities may play a role8,37,38. Furthermore, a recent study from the HIV clinic at HNSM found Fula and Mandinga ethnicity to be associated with late presentation at HIV diagnosis39. These findings underline the importance of identifying vulnerable populations, understanding sociocultural motivators, and targeting interventions accordingly.
Overall, self-reported HIV treatment coverage among women accessing antenatal care increased significantly over the course of this study. However, only 47% of women presenting for labour had received antenatal testing and counselling, and only 77% of women were tested for HIV at birth, leaving a large number of women unaware and untreated14. HIV-infected women not identified during pregnancy miss out on the benefits of treatment and prevention and remain part of a “hidden epidemic”; they are prone to late diagnosis, poor health outcomes and at risk of infecting their infants40,41.
While some national interventions, such as strengthening the early provision of ART as recommended by the WHO, have shown promise18, repeated political instability, and inadequate management of HIV tests and medicine stocks appear to have significant negative impacts on the clinical management of HIV in the country10,14,42. After a civil war in 1999, Guinea-Bissau suffered five military coups between 2002 and 201243,44, which left the country in a chronic state of political instability14. This has hampered development despite national and international efforts and inevitably discouraged donors, as was seen in 2012 after the Global Fund, the World Bank, the African Development Bank and the European Union suspended HIV funding activities in Guinea-Bissau12,21. These cuts in funding may explain the increase in HIV-infected women and their infants not receiving ART in labour in 2012 and 2013 as observed in this study, as well as the decline in national ART coverage from 56% in 2011 to 23% in 201421. Repeated drug stock outages were common in Guinea-Bissau9,10,42 and may have forced doctors and midwives to choose treatments no longer recommended by national guidelines, as reflected by the high proportion of women receiving sd NVP, or no treatment. In addition, a high number of HIV-2-infected patients received NVP, a non-nucleoside reverse transcriptase inhibitor (NNRTI), for PMTCT. This is problematic because NNRTIs are ineffective against HIV-2 due to natural resistance45. Periods of drug shortages and the resulting use of NNRTI-based regimes may explain the high levels of NNRTI resistance found in Guinea-Bissau42,46,47. Conditions in the country appear to have improved after international donors, led by the Global Fund, have resumed funding activities, which is reflected by a 30% increase (49.5–81.9%) in the number of HIV-positive mothers who received ART for PMTCT in 201421. Current estimates from UNAIDS report that 65% of pregnant women living with HIV in Guinea-Bissau accessed ART in 201748. While these results show promise, overall ART coverage remains low in Guinea-Bissau48. Preliminary results from a routine analysis of nationwide HIV Cohort in the country show that only 14% of HIV infected individuals are aware of their HIV-status and of these only 20% are on treatment underling the urgent need to determine the treatment retention and long-term outcomes of mothers and their infants during and after PMTCT10.
This study found an increase in the number of infants not receiving PMTCT. An increase in the number of HIV-infected children and high rates of HIV infection (9.3%) despite PMTCT have been reported in Guinea-Bissau, suggesting poor treatment retention and challenges to PMTCT coverage and follow-up15. While an increase in the number of HIV-infected children may be due to better diagnostics, the late diagnosis of children (median age 3.5 years) suggests a large proportion of children die before being diagnosed with HIV15.
In line with other studies, women infected with HIV-1 and HIV-1/2 in this study had an increased risk of delivering LBW babies49,50. LBW babies have an increased risk of mortality and may experience negative health outcomes during childhood and later in life51. Studies have described an increasing risk of LBW with advancing stage of HIV disease52, but also according to maternal ART regimens51, emphasizing the importance of identifying HIV-infected mothers early in pregnancy and insuring they receive the optimal ART regimen to improve health outcomes, prevent MTCT and minimize the risk of LBW.
In Guinea-Bissau, stillbirths are common. A previous study from the capital Bissau found a community stillbirth rate of 71/1,000 among mothers who did not attend ANC and 36/1,000 among mothers who attended 7 or more ANC16. While HIV infection is known to be associated with stillbirths50, this study did not find a significant association. Many factors affect the risk of stillbirths, including maternal age, education, marital status and ethnicity, in our setting16. In addition, the stage of maternal disease, ART regimen and timing of treatment play a role in the risk of stillbirth and other adverse birth outcomes among HIV-infected mothers4,53. Therefore, our analysis may have been limited by our inability to control sufficiently for these factors.
This study is based on data from a large sample of women presenting for labour and delivery at the country’s largest maternity ward and thus reflects the challenges to PMTCT services in a setting with limited resources. Our research has several limitations. First, the cross-sectional nature of this study means we are unable to determine trends in incidence and causality. Twenty-three percent of women presenting for labour during the study period were not counselled or tested for HIV. These women were not included in this study due to missing information on HIV status presenting a potential selection bias. Data regarding condom use, number of previous partners, and additional high-risk behaviours were unavailable, limiting our risk factor analysis. HIV type discrimination was performed using SD Bioline HIV-1/2 3.0. A study from Guinea-Bissau found that SD Bioline HIV-1/2 3.0 overestimates the number of HIV-1/2 dually infected individuals54, and high inter-observer variation was noted55, which could have led to misclassification of HIV type in this study. HIV prevalence was determined based on women presenting at the HNSM maternity ward and may differ from women giving birth at other urban health centres or at home. Only half (47%) of women tested at birth reported previous testing during antenatal visits. There were discrepancies between self-reported antenatal test results and results at labour suggesting either insufficient pre and post testing counselling, lack of HIV awareness, or stigma13, recall bias or seroconversion.
The HNSM maternity ward receives women from all parts of the capital and other regions in Guinea-Bissau for care and treatment of obstetric complications, yet little is known regarding the specific referral process to give birth. The lack of continuity of care and registration systems made it almost impossible for midwives to corroborate self-reported antenatal treatment, which may have been affected by recall bias. In addition, the lack of confidentiality and time to perform pre- and post-test counselling at labour13 could have limited midwives’ and doctors’ ability to make treatment decisions regarding the type and length of treatment based on self-reported antenatal treatment regimes.
Conclusion
The prevalence of HIV-1, HIV-2 and HIV-1/2 among pregnant women presenting for labour and delivery at the HNSM declined between 2008 and 2013. The observed increase in the proportion of women and infants not receiving treatment at birth is concerning. Less than half of the women in this study reported attending antenatal counselling and testing, and 23% were not tested in relation at birth, resulting in many mothers unaware of their HIV status and hence deprived of the benefits of treatment and prevention. As Guinea-Bissau continues to take strides towards improving PMTCT testing and ART coverage to mitigate the risk of poor health outcomes of HIV-infected mothers and their infants, further operational research focusing on provision of PMTCT services and continuity of care, retention to PMTCT services, including treatment and patient follow-up, is urgently needed to support future interventions and policy.
Data availability
The original data are stored at the Bandim Health Project, National Institute of Public Health in Guinea-Bissau. The ethical approvals received from The National Committee on Ethics in Health, National Institute of Public Health, Ministry of Public Health, Guinea-Bissau (e-mail: inasagb@gmail.com) do not allow for general data sharing of this dataset. Data access can therefore be granted to individual researchers only after obtaining ethical permission. Any party interested in accessing the relevant data can do so by contacting the Bandim Health Project (e-mail: bandim@ssi.dk). The Bandim Health Project will facilitate the request for ethical permission from the National Committee on Ethics in Health and provide the data on approval. We can confirm that others will be able to access the relevant data in the same manner and form as the authors, provided ethical approval is obtained from Guinea-Bissau’s National Committee on Ethics in Health.
References
UNAIDS. Miles to go—Closing Gaps, Breaking Barriers, Righting Injustices. (Geneva, Switzerland 2018).
Zaba, B. et al. Effect of HIV infection on pregnancy-related mortality in sub-Saharan Africa: secondary analyses of pooled community-based data from the network for Analysing Longitudinal Population-based HIV/AIDS data on Africa (ALPHA). The Lancet 381, 1763–1771 (2013).
UNICEF. Women: At the Heart of the HIV Response for Children (United Nations Children’s Fund (UNICEF), New York, 2018).
Bailey, H., Zash, R., Rasi, V. & Thorne, C. HIV treatment in pregnancy. Lancet HIV 5, e457–e467. https://doi.org/10.1016/S2352-3018(18)30059-6 (2018).
De Cock, K. M. et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. JAMA 283, 1175–1182 (2000).
UNAIDS. 2015 Progress Report on the Global Plan Towards the Elimination of New HIV Infections Among Children and Keeping their Mothers Alive (Geneva, Switzerland, 2015).
Olesen, J. S. et al. HIV-2 continues to decrease, whereas HIV-1 is stabilizing in Guinea-Bissau. Aids 32, 1193–1198 (2018).
Gianelli, E. et al. Prevalence and risk determinants of HIV-1 and HIV-2 infections in pregnant women in Bissau. J. Infect. 61, 391–398. https://doi.org/10.1016/j.jinf.2010.08.012 (2010).
Jespersen, S. et al. Challenges facing HIV treatment in Guinea-Bissau: the benefits of international research collaborations. Bull. World Health Organ. 92, 909–914. https://doi.org/10.2471/BLT.14.135749 (2014).
Jespersen, S. et al. HIV treatment in Guinea-Bissau: room for improvement and time for new treatment options. AIDS Res. Ther. 17, 3. https://doi.org/10.1186/s12981-020-0259-6 (2020).
UNAIDS. UNAIDS Data 2018 (UNAIDS, Geneva, 2018).
UNICEF. UNICEF Annual Report 2012 for Guinea Bissau, WCARO (UNICEF, 2012).
Vieira, N. et al. Awareness, attitudes and perceptions regarding HIV and PMTCT amongst pregnant women in Guinea-Bissau—a qualitative study. BMC Women’s Health 17, 71 (2017).
Rasmussen, D. N. et al. Political instability and supply-side barriers undermine the potential for high participation in HIV testing for the prevention of mother-to-child transmission in Guinea-Bissau: a retrospective cross-sectional study. PLoS ONE 13, e0199819. https://doi.org/10.1371/journal.pone.0199819 (2018).
Steiniche, D. et al. Excessive mortality and loss to follow-up among HIV-infected children in Guinea-Bissau, West Africa: a retrospective follow-up study. Trop. Med. Int. Health 23, 1148–1156 (2018).
Bjerregaard-Andersen, M. et al. Stillbirths in urban Guinea-Bissau: a hospital- and community-based study. PLoS ONE 13, e0197680. https://doi.org/10.1371/journal.pone.0197680 (2018).
PNLS. (Programa Nacional de Luta contra o VIH/SIDA, Bissau, Guinea-Bissau, 2009).
WHO. Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants: Recommendations for a Public Health Approach-2010 Version (World Health Organization, Geneva, 2010).
Jespersen, S. et al. Lack of awareness of treatment failure among HIV-1-infected patients in Guinea-Bissau-a retrospective cohort study. J. Int. AIDS Soc. 18, 20243–20243 (2014).
WHO. Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants (World Health Organisation WHO, Geneva, 2012).
SNLS. UNGASS Country Progress Report Guinea-Bissau—2015 (Secretariado Nacional de Luta Contra SIDA, Guinea-Bissau, 2015).
Lawn, J. E. et al. Stillbirths: where? When? Why? How to make the data count?. The Lancet 377, 1448–1463. https://doi.org/10.1016/S0140-6736(10)62187-3 (2011).
WHO. International Statistical Classification of Diseases and Related Health Problems. 10th revision, edition 2010 (World Health Organization, Geneva, Switzerland, 2011).
Mansson, F. et al. Trends of HIV-1 and HIV-2 prevalence among pregnant women in Guinea-Bissau, West Africa: possible effect of the civil war 1998 1999. Sex. Transm. Infect. 83, 463–467. https://doi.org/10.1136/sti.2007.025353 (2007).
Tienen, C. et al. Two distinct epidemics: the rise of HIV-1 and decline of HIV-2 infection between 1990 and 2007 in rural Guinea-Bissau. J. Acquir. Immune Defic. Syndr. 53, 640–647. https://doi.org/10.1097/QAI.0b013e3181bf1a25 (2010).
da Silva, Z. J. et al. Changes in prevalence and incidence of HIV-1, HIV-2 and dual infections in urban areas of Bissau, Guinea-Bissau: is HIV-2 disappearing?. Aids 22, 1195–1202. https://doi.org/10.1097/QAD.0b013e328300a33d (2008).
INASA. Estudo Sentinela de II Geração sobre prevalência do VIH nas Grávidas na Guiné-Bissau-Relatório-Final (Instituto Nacional de Saúde Pública, Guinea-Bissau, 2014).
Schmidt, W. P. et al. Behaviour change and competitive exclusion can explain the diverging HIV-1 and HIV-2 prevalence trends in Guinea-Bissau. Epidemiol. Infect. 136, 551–561. https://doi.org/10.1017/S0950268807008758 (2008).
de Silva, T. I. et al. Population dynamics of HIV-2 in rural West Africa: comparison with HIV-1 and ongoing transmission at the heart of the epidemic. Aids 27, 125–134. https://doi.org/10.1097/QAD.0b013e32835ab12c (2013).
Fryer, H. R. et al. Predicting the extinction of HIV-2 in rural Guinea-Bissau. Aids 29, 2479–2486 (2015).
Mansson, F. et al. Prevalence and incidence of HIV-1 and HIV-2 before, during and after a civil war in an occupational cohort in Guinea-Bissau, West Africa. Aids 23, 1575–1582. https://doi.org/10.1097/QAD.0b013e32832cedfb (2009).
Cohen, M. S. et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N. Engl. J. Med. 375, 830–839. https://doi.org/10.1056/NEJMoa1600693 (2016).
Dyrehave, C. et al. Nonadherence is associated with lack of HIV-related knowledge: a cross-sectional study among HIV-infected individuals in Guinea-Bissau. J. Int. Assoc. Provid. AIDS Care (JIAPAC) 15, 350–358 (2016).
Jespersen, S. et al. Protease inhibitors or NNRTIs as first-line HIV-1 treatment in West Africa (PIONA): a randomised controlled trial. JAIDS J. Acquir. Immune Defic. Syndr. 79, 386–393 (2018).
Hønge, B. L. et al. Loss to follow-up occurs at all stages in the diagnostic and follow-up period among HIV-infected patients in Guinea-Bissau: a 7-year retrospective cohort study. BMJ open 3, e003499 (2013).
Kenyon, C. R., Vu, L., Menten, J. & Maughan-Brown, B. Male circumcision and sexual risk behaviors may contribute to considerable ethnic disparities in HIV prevalence in Kenya: an ecological analysis. PLoS ONE 9, 106230 (2014).
Pepin, J., Plamondon, M., Alves, A. C., Beaudet, M. & Labbe, A. C. Parenteral transmission during excision and treatment of tuberculosis and trypanosomiasis may be responsible for the HIV-2 epidemic in Guinea-Bissau. Aids 20, 1303–1311. https://doi.org/10.1097/01.aids.0000232239.05545.33 (2006).
Rasmussen, D. N. et al. The when and how of male circumcision and the risk of HIV: a retrospective crosssectional analysis of two HIV surveys from Guinea-Bissau. Pan Afr. Med. J. 23, 21 (2016).
Hønge, B. L. et al. High prevalence and excess mortality of late presenters among HIV-1, HIV-2 and HIV-1/2 dually infected patients in Guinea-Bissau-a cohort study from West Africa. Pan Afr. Med. J. 25, 40 (2016).
Supervie, V., Ndawinz, J. D., Lodi, S. & Costagliola, D. The undiagnosed HIV epidemic in France and its implications for HIV screening strategies. Aids (London, England) 28, 1797 (2014).
Ghosn, J., Taiwo, B., Seedat, S., Autran, B. & Katlama, C. Hiv. Lancet 392, 685–697. https://doi.org/10.1016/S0140-6736(18)31311-4 (2018).
Oliveira, I. et al. Assessment of simple risk markers for early mortality among HIV-infected patients in Guinea-Bissau: a cohort study. BMJ Open 2, e001587 (2012).
Ferreira, P. M. GUINEA-BISSAU. Afr. Secur. Rev. 13, 44–56. https://doi.org/10.1080/10246029.2004.9627317 (2004).
Security Council. Update Report on Guinea-Bissau (Security Council, New York, 2012).
Witvrouw, M. et al. Activity of non-nucleoside reverse transcriptase inhibitors against HIV-2 and SIV. Aids 13, 1477–1483. https://doi.org/10.1097/00002030-199908200-00006 (1999).
Oliveira, I. et al. Epidemic Stevens-Johnson syndrome in HIV patients in Guinea-Bissau: a side effect of the drug-supply policy?. Aids 24, 783–785 (2010).
Jespersen, S. et al. High level of HIV-1 drug resistance among patients with HIV-1 and HIV-1/2 dual infections in Guinea-Bissau. Virol. J. 12, 41 (2015).
UNAIDS. Country factsheets Guinea-Bissau 2017. https://www.unaids.org/en/regionscountries/countries/guinea-bissau (2018).
Evans, C., Jones, C. E. & Prendergast, A. J. HIV-exposed, uninfected infants: new global challenges in the era of paediatric HIV elimination. Lancet Infect. Dis. 16, e92–e107 (2016).
Wedi, C. O. et al. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV 3, e33–e48 (2016).
Saleska, J. L., Turner, A. N., Maierhofer, C., Clark, J. & Kwiek, J. J. Use of antiretroviral therapy during pregnancy and adverse birth outcomes among women living with HIV-1 in low- and middle-income countries: a systematic review. JAIDS J. Acquir. Immune Defic. Syndr. 79, 1–9. https://doi.org/10.1097/qai.0000000000001770 (2018).
Coley, J. L. et al. The association between maternal HIV-1 infection and pregnancy outcomes in Dar es Salaam, Tanzania. BJOG Int. J. Obstet. Gynaecol. 108, 1125–1133 (2001).
Zash, R. et al. Comparative safety of antiretroviral treatment regimens in pregnancy. JAMA Pediatr. 171, e172222–e172222 (2017).
Honge, B. L. et al. Performance of 3 rapid tests for discrimination between HIV-1 and HIV-2 in Guinea-Bissau, West Africa. J. Acquir. Immune Defic. Syndr. 65, 87–90. https://doi.org/10.1097/QAI.0b013e3182a97b81 (2014).
Hønge, B. L. et al. Interobserver variation of the rapid test SD bioline HIV-1/2 3.0 for HIV type discrimination: experiences from Guinea-Bissau. JAIDS J. Acquir. Immune Defic. Syndr. 68, e23–e25 (2015).
Acknowledgements
The authors are grateful to the mothers at HNSM for their participation in this study and to the midwives who helped collect these data. We also thank the members of the Bandim Health Project in Bissau for their support with this research, especially Professor Peter Aaby, Aureliano Gomes, Neusa Andersen and Andreas Andersen. In addition, we would like to thank Professor Jens Søndergaard, Dr Amabelia Rodrigues and Oscar Bosiso. This study was made possible by a research grant from the Albert McKern Bequest, Edinburgh, UK to HWU, and financial support from the Department of Infectious Diseases, Odense University Hospital, and the Department of Public Health, Research Unit for General Practice, University of Southern Denmark, to DNR.
Author information
Authors and Affiliations
Contributions
D.N.R., H.W.U., I.O., C.W. and M.S. conceptualized this study. D.N.R., H.W.U., M.B.A., I.O. and M.A.G. participated in data curation. D.N.R., H.W.U. and M.S. were responsible for data analysis. D.dS.T., N.V., A.F., B.L.H., S.J., M.B.A. and C.W. helped interpret and validate the findings. D.N.R. wrote the original draft, and all authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rasmussen, D.N., Vieira, N., Hønge, B.L. et al. HIV-1 and HIV-2 prevalence, risk factors and birth outcomes among pregnant women in Bissau, Guinea-Bissau: a retrospective cross-sectional hospital study. Sci Rep 10, 12174 (2020). https://doi.org/10.1038/s41598-020-68806-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-68806-5
This article is cited by
-
A pilot investigation of the association between HIV-1 Vpr amino acid sequence diversity and the tryptophan-kynurenine pathway as a potential mechanism for neurocognitive impairment
Virology Journal (2024)
-
Epidemiological and virological surveillance of the prevention of mother-to-child transmission of HIV among pregnant women in Togo
BMC Pregnancy and Childbirth (2024)
-
HIV is still a major public health problem among pregnant women attending ANC in Referral Hospitals of the Amhara Regional State, Ethiopia: a cross sectional study
BMC Women's Health (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.