Abstract
Although it has been reported that chronic kidney disease exacerbates sarcopenia progression, the mechanisms of the process remain unclear. Fifty-one patients who underwent renal transplantation at our hospital since 1998 (31 males and 20 females; aged 29–52 years at the time of transplantation) were retrospectively examined for the relationships among the psoas muscle index (PMI), intramuscular adipose tissue content (IMAC), serum adiponectin fractions (high-/low-molecular-weight) and new-onset diabetes after transplantation (NODAT). Before transplantation, age at kidney transplantation negatively correlated with PMI and positively correlated with IMAC (rS = − 0.427, p < 0.01; rS = 0.464, p < 0.01, respectively). Both at 1 and 5 years after transplantation, PMI was higher than before transplantation (p < 0.01). IMAC transiently decreased to − 0.39 at 1 year after kidney transplantation but subsequently increased to − 0.36 at 5 years after kidney transplantation. Multivariate analyses revealed that the mean increase in high-molecular weight adiponectin concentrations was an exacerbating factor for the mean change in PMI (p = 0.003). Moreover, the mean increases in IMAC were exacerbating factors for NODAT. In conclusion, the increase in the PMI is associated with high–molecular weight adiponectin levels after renal transplantation.
Similar content being viewed by others
Introduction
Sarcopenia is defined as loss of the mass, strength, and function of skeletal muscles1. It is associated with not only a decline in the activities of daily living and falls, which results in the need for long-term care, but also with an increase in mortality and is a significant clinical and social problem in the developed countries2. Sarcopenia is classified into primary sarcopenia and secondary sarcopenia3. Primary sarcopenia is an age-associated decrease in muscle mass, whereas secondary sarcopenia is a decrease in muscle mass associated with a reduced activity level, malnutrition, organ failure, invasion and diseases, including cancer. Therefore, contributing factors for secondary sarcopenia should be considered in the same way as ageing. Metabolic acidosis and the increased expression of angiotensin II have been shown to decrease muscle mass in patients with chronic kidney disease, particularly patients on dialysis4,5. However, studies on sarcopenia in patients with kidney transplantation are very few. Although sarcopenia is a clinically important manifestation, it is difficult to objectively evaluate its progression. As the quantity and quality of skeletal muscle is an essential component for sarcopenia, we focused on psoas muscle images on computed tomography (CT). Hamaguchi et al. reported that a decrease in muscle mass, expressed as the psoas muscle index (PMI), was related to the mortality rate after transplantation6. Muscle quality has recently been attracting attention, and the fatty degeneration of muscle has been associated with ageing and muscle weakness7 as well as with the development of diabetes mellitus8. Kitajima et al. evaluated the fatty generation of muscle according to the intramuscular adipose tissue content (IMAC) by abdominal CT9. Therefore, we used PMI and IMAC as sarcopenia markers in this study.
A wide variety of cytokines, called myokines, are secreted from skeletal muscle cells. Adiponectin (ADPN) is a member of myokines and is also secreted from fat cells. There are complex regulating mechanisms involved in ADPN secretion and crosstalk with effector cells. ADPN exerts anti-atherosclerotic, anti-diabetic and anti-inflammatory effects10 and also plays some roles in muscle fibre remodelling and fat cell metabolisms. Moreover, it is reported that ADPN expression levels are decreased under the condition of increasing inflammatory cytokines, such as TNF-α and IL-611. Therefore, crosstalk between muscle and fat cells by ADPN is speculated as a possible pathogenic mechanism of sarcopenia12. In addition, our previous study indicated that there was a strong negative correlation between serum high-molecular weight (HMW) ADPN concentrations and renal function13. Therefore, the fraction of ADPN is an important factor in these analyses. In addition to inflammatory processes, ADPN may contribute in cellular metabolism. It also plays a role in the onset of diabetes. ADPN increases the number of intramuscular mitochondria and enhances their function in skeletal muscles through ADPN receptor 1 signalling pathways14. In kidney transplantation, ischaemic stress in kidney induces various kinds of inflammatory processes. Additionally, steroid is one of the key immunosuppressive drugs for kidney transplantation, but it affects new onset diabetes. Although some ADPN fractions are speculated to play critical roles in the onset or progression of sarcopenia and newly onset diabetes, detailed studies on ADPN and sarcopenia in kidney transplantation are few.
In this study, we examined muscle mass and fatty degeneration as sarcopenia markers and evaluated relationships between these factors and serum ADPN levels. We found that HMW-ADPN levels indicate increase of muscle mass until 5 years after kidney transplantation.
Results
Baseline characteristics of patients classified according to sexes
The clinical characteristics of 31 male and 20 female patients at the beginning of observations (before transplantation) are shown in Table 1. Although no difference was observed in age between the gender at transplantation or duration of dialysis, body mass index (BMI) and serum albumin was higher in males. Systolic and diastolic blood pressure were controlled. No difference was observed in the total cholesterol (T Chol), TG or non-high-density lipoprotein cholesterol (non-HDL-C) levels between the gender. IMAC for assessing muscle fat change wash higher in female (p < 0.01) and PMI was higher in males (p < 0.01). No significant difference in gender was observed in medication both before and after transplantation.
Relationships between muscle imaging data (PMI and IMAC) and clinical factors (duration of dialysis and age at transplantation) before transplantation
The relationships between muscle imaging data (PMI and IMAC) and clinical factors (duration of dialysis and age at transplantation) are shown in Fig. 1. PMI before transplantation did not correlate with the duration of dialysis but negatively correlated with age at transplantation (rS = − 0.427, p < 0.01). IMAC before transplantation positively correlated with the duration of dialysis and age at transplantation (rS = 0.371, p < 0.01 and rS = 0.464, p < 0.01, respectively). Factors that affected PMI and IMAC before transplantation were evaluated using multiple regression analysis (Table 2). Gender female and old age at the time of transplantation were identified as factors contributing to low PMI before transplantation, and Gender female, long-term dialysis and old age at the time of transplantation were identified as factors for high IMAC.
Relationships between PMI and IMAC before kidney transplantation, duration of dialysis and age at transplantation. (a) PMI before kidney transplantation did not correlate with the duration of dialysis (rS = − 0.146, p = 0.305, according to Spearman’s rank coefficient). (b) PMI before kidney transplantation negatively correlated with age at transplantation (rS = − 0.427, p = 0.002, according to Spearman’s rank coefficient). (c, d) IMAC before kidney transplantation positively correlated with the duration of dialysis and age at kidney transplantation (rS = 0.371, p = 0.007 and rS = 0.464, p = 0.001, respectively, according to Spearman’s rank coefficient). PMI psoas muscle mass index, IMAC intramuscular adipose tissue content.
Changes in PMI and IMAC and after kidney transplantation
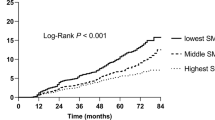
Changes in PMI and IMAC after transplantation are shown in Fig. 2. The median of PMI was 3.03 before transplantation and significantly increased to 3.36 and 3.58 at 1 and 5 years after transplantation, respectively (1 year, p < 0.001; 5 years, p < 0.001). The median of IMAC was − 0.37 before transplantation and significantly decreased to − 0.39 1 year after transplantation (p < 0.01). However, IMAC increased to − 0.36 5 years after transplantation.
Changes in PMI and IMAC after kidney transplantation. (a) PMI before kidney transplantation was 3.03 cm2/m2, which significantly increased to 3.36 cm2/m2 at 1 year after kidney transplantation and 3.58 cm2/m2 at 5 years after kidney transplantation (p < 0.001 and p < 0.001, respectively, according to Dunn’s test for multiple comparisons). (b) IMAC significantly decreased to − 0.39 at 1 year after kidney transplantation, and no significant difference was observed after 5 years. PMI psoas muscle mass index, IMAC intramuscular adipose tissue content.
Relationship between changes in ADPN and PMI after kidney transplantation
HMW-ADPN, middle-molecular-weight (MMW)-ADPN and low-molecular-weight (LMW)-ADPN concentrations were 5.17 ± 2.82, 1.97 ± 0.69 and 3.73 ± 1.12 μg/mL, respectively, at 1 year after kidney transplantation, and 5.61 ± 3.61, 2.06 ± 0.82 and 3.68 ± 1.26 μg/mL, respectively, at 5 years after kidney transplantation. The serum levels of ADPN fractions were stable, showing no marked difference between 1 and 5 years after kidney transplantation. In addition, the relationships between serum HMW-ADPN concentrations and PMI at 1 and 5 years after kidney transplantation are shown in Fig. 3. HMW-ADPN negatively correlated with PMI at 1 and 5 years after kidney transplantation (rS = − 0.373, p = 0.007 and rS = − 0.308, p = 0.028, respectively). The mean change in serum HMW-ADPN levels within 4 years from 1 to 5 years after kidney transplantation negatively correlated with the mean change in PMI during the 4 years (rS = − 0.296, p = 0.034). Furthermore, multiple regression analysis of the factors causing changes in PMI identified the increase in HMW-ADPN as a factor for the decrease in PMI (Table 3). The mean change in estimated glomerular filtration rate (eGFR) within 4 years from 1 to 5 years after kidney transplantation negatively correlated with the mean change in LMW-ADPN concentrations (rS = − 0.362, p = 0.009).
Relationships among the development of new onset diabetes after transplantation (NODAT), PMI and IMAC
No significant differences were observed regarding changes in PMI between non-NODAT and NODAT patients, whereas IMAC was significantly higher in NODAT patients ([3B]: p = 0.008). Multiple logistic analysis revealed that increases in IMAC and HMW-ADPN were exacerbating factors (Table 4).
Discussion
This long-term retrospective cohort study clearly showed that serum ADPN concentrations play important roles the muscle mass and fatty degeneration of muscles after kidney transplantation. Muscle mass gradually increased and the fatty degeneration of muscles was reversed in kidney transplant recipients after transplantation. Furthermore, an increase in HMW-ADPN concentrations was identified as a factor contributing to decrease in PMI. In addition, increases in PMI and IMAC were exacerbating factors for the development of NODAT.
We observed that PMI increased after kidney transplantation, and this finding indicates that sarcopenia was improved by kidney transplantation. Frailty is observed in approximately 42% of dialysis patients and has been identified as a risk factor that increases the hospitalisation rate by 1.43-fold and mortality rate by 2.6-fold, independent of age and complications15,16. Increases in inflammatory cytokines, an imbalance in muscle protein synthesis/degradation, reduced physical activity, an insufficient nutritional intake, metabolic acidosis, vitamin D deficiency, insulin resistance, excessive myostatin expression, increases in intramuscular angiotensin and decrease and dysfunction in satellite cells have been suggested as factors involved in the development of sarcopenia in chronic kidney disease patients17. Dialysis patients have a high risk of developing sarcopenia due to ageing and progressing uremic sarcopenia with prolonged dialysis. However, some of these risk factors are removed by kidney transplantation. It has been reported that 23–73% of dialysis patients suffer from malnutrition18. Furthermore, a decreased physical activity level is an important factor in the development of sarcopenia19. Patients undergoing dialysis are also at a higher risk of sarcopenia due to the loss of proteins and amino acids into the dialysis solution20. Increased muscle mass following kidney transplantation may be attributed to an increased level of physical activity, as well as increased protein intake without any loss of proteins that would otherwise occur during dialysis. We herein objectively demonstrated that PMI, which reflects muscle mass, clearly increased, and IMAC, which reflects muscle quality, was maintained for a long time after kidney transplantation.
Fat cells that have the ability to secrete hormones secrete anti-inflammatory cytokines, such as ADPN and leptin, as well as pro-inflammatory cytokines such as PAI-1, IL-6, and TNF-α. Among these cytokines, TNF-α and IL-6 are known to promote sarcopenia21. Studies also suggest that with aging, the serum ADPN concentration increases from adulthood while skeletal muscle mass peaks around adulthood and decreases gradually22. Previous studies also demonstrated that ADPN and AdipoR1 regulate the expression and activation of PPARγcoactivator-1α [PCG-1α], a key component of sarcopenia, by Ca2+ signalling, AMP-activated protein kinase (AMPK), and SIRT1. Thus, there is an increasing interest in the role of ADPN and AdipoR1 in the regulation of skeletal muscle fibers23. We also revealed that an increase in HMW-ADPN concentrations was identified as a factor contributing to decrease in PMI. In the present study, a negative correlation was observed between serum ADPN concentrations and muscle mass, a marker of sarcopenia. Although this finding seems to conflict with previous reports, similar observation was also reported. There was a significant inverse correlation between serum adiponectin levels with arm lean mass and muscle strength in patients with HF24. In addition, muscle weakness in the limbs was reported to be related to an increase in serum ADPN concentrations in elderly patients and leg muscle strength inversely correlated with blood ADPN concentrations in patients aged ≥ 70 years25. A previous study confirmed that the percentage of type IIB muscle fibres increased in ADPN knockout mice26, and an epidemiological study on 461 elderly subjects showed that IIB fibres were reduced in those with high blood ADPN concentrations27. In addition, a recent study showed that administration of AdipoRon, an adiponectin receptor agonist, increases blood ADPN concentrations and induces atrophy of type II muscle fibres via the adiponectin receptor 1-AMP-dependent protein kinase signal pathway in mice28. Since the present study found a negative correlation between blood levels of HMW-ADPN and the cross-sectional area of the greater psoas muscle, the muscle fibres that correlated with ADPN may be primarily type II muscle fibres. Collectively, these findings and the present results suggest that muscles of kidney transplant patients would similarly react to HMW-ADPN as aged cases. HMW-ADPN exerts different effects on different muscle fibre types, i.e. HMW-ADPN increases the percentage of type I fibres but decreases that of type II fibres, as the mechanism of action of ADPN in sarcopenia.
Our study showed that increases in IMAC were exacerbating factors for the development of NODAT. Since the mass of muscle, a target organ of insulin, decreases in sarcopenia, patients with sarcopenia have insulin resistance. In obese patients with sarcopenia (sarcopenic obesity), blood levels of IL-6 and CRP are elevated, and these factors lead to an increase in insulin resistance and decrease in skeletal muscle mass29, 30. This would be a vicious cycle in sarcopenic obesity. Moreover, insulin also stimulates protein synthesis. Therefore, skeletal muscle synthesis may be suppressed in diabetic patients, and leg neuropathy has been strongly implicated in muscle weakness31. Landi et al. reported that sarcopenia and diabetes may be interrelated via factors such as insulin resistance, inflammatory cytokines and mitochondrial hypofunction32. Furthermore, in addition to subcutaneous and visceral fat, ectopic fat, called the third fat, is now being investigated. Akima et al. showed that the accumulation of fat in the muscles of elderly individuals was related to sarcopenia and impaired motor function33, and a decline in mitochondrial function and fat accumulation in muscles has been suggested to increase insulin resistance34. Although the state of uremic sarcopenia is ameliorated and muscle mass increases after kidney transplantation, serial increases in IMAC, i.e. the progression of the fatty degeneration of muscles, are considered to be involved in the development of NODAT. Therefore, the preservation of not only muscle mass, but also muscle quality are important for the prevention of NODAT.
The limitations of the present study include (1) the small number of subjects, (2) its retrospective design, and (3) evaluation limited to muscle mass of the greater psoas and multifidus muscles. Further studies are warranted to examine other muscles, such as the extensor digitorum longus muscle, which is reported to have a high content of type II muscle fibres and to investigate differences among muscles in the same individuals. We also intend to perform a prospective study, extend the observation period and examine relationships with the prognoses of and cardiovascular complications in these patients.
Conclusion
Our study showed that PMI gradually increased and IMAC decreased after kidney transplantation. The increase in PMI was associated with HMW-ADPN levels after kidney transplantation, which indicates its involvement in the development of NODAT in renal allograft recipients. Therefore, sufficient exercise therapy is also considered to be necessary after transplantation to preserve skeletal muscle mass and prevent the fatty degeneration of muscle.
Methods
Patients
Fifty-one patients who underwent kidney transplantation since 1998 at our hospital and showed stable renal function for at least 6 months thereafter (40 recipients from living donors and 11 recipients from deceased donors; 31 males and 20 females) were retrospectively examined. The causes of renal failure in the transplant patients were chronic glomerulonephritis (n = 35), purpura nephritis (n = 3), membranoproliferative glomerulonephritis (n = 3), hypoplasia (n = 3), nephrosclerosis (n = 3), polycystic kidney disease (n = 2), focal segmental glomerulosclerosis (n = 1), reflux nephropathy (n = 1). Since the time required for the stabilisation of kidney graft functions differs between kidney transplant recipients from living donors and those from deceased donors, the changes in serum ADPN fractions within 4 years from 1 to 5 years after transplantation were investigated in the present study.
The relationship between skeletal muscle masses evaluated by PMI 1 and 5 years after transplantation and the serum levels of ADPN fractions (HMW, MMW and LMW fractions) were assessed as the primary endpoint. The relationship between intramuscular adipose tissue contents (IMAC) at 1 and 5 years after transplantation, the serum levels of ADPN fractions and changes in PMI and IMAC after transplantation and among NODAT, PMI, IMAC and serum ADPN fractions were investigated as the secondary endpoints.
The following clinical factors were evaluated: age at transplantation, gender, duration of dialysis, blood pressure at 1 and 5 years after transplantation, BMI, serum creatinine (SCr), eGFR, serum albumin, T chol, HDL-C, non-HDL-C (T chol-HDL-C), ADPN fractions (HMW, MMW and LMW), types of immunosuppressants used, statins and anti-hypertensive agents.
The present study did not include any vulnerable populations, such as prisoners, subjects with reduced mental capacity due to illness or age or children. Furthermore, we used blood samples, radiological scans and renal biopsy specimens. The study protocol was approved by the Ethics Committee of Kanazawa Medical University (Kanazawa Medical University Epidemiological Study Review No. I293). All patients provided written informed consent, and the study was conducted according to the principles of the Declaration of Helsinki and Istanbul.
Measurement methods
Serum levels of total HMW-, MMW- and LMW-ADPN were measured using a sensitive enzyme-linked immunosorbent assay kit (SEKISUI MEDICAL Co., Tokyo, Japan). Renal function was evaluated based on eGFR [194 × SCr−1.094 × age−0.287 (× 0.739 for females), mL/min/1.73 m2]. eGFR was calculated based on patient SCr levels, as described previously35.
Imaging analysis
The skeletal muscle mass index proposed by Prado et al., calculated by dividing total skeletal muscle mass at the L3 level by the square of height, is a typical index for evaluating skeletal muscle mass by CT36. Evaluation method of CT image are shown in SI Fig. S1. we calculated PMI (cm2/m2) as the cross-sectional area of the greater psoas muscle (cm2)/height2 (m2) using image analysis software (MITANI Co., Ltd., Fukui, Japan) and examined regions of interest (ROI) in the bilateral greater psoas muscles in a slice of abdominal CT at the L3 level. IMAC was measured using AZE Virtual Place (AZE Co., Ltd., Kanagawa, Japan) and setting ROIs over the bilateral multifidus muscles in a slice of abdominal CT at the L3 level. Moreover, ROIs were set in 4 areas of subcutaneous fat distant from the large vessels, and the mean CT value of the multifidus muscle/mean CT value of the subcutaneous fat region in the back was calculated and evaluated.
Statistical analyses
All continuous variables are expressed as median values and interquartile ranges. Comparisons between sexes were made using the Mann–Whitney test. The relationships between PMI and IMAC before transplantation, duration of dialysis and age at transplantation as well as between the mean change in eGFR and mean change in serum ADPN levels were examined according to Spearman’s rank correlation coefficient. Changes in PMI and IMAC after transplantation were evaluated using Dunn’s test. Factors affecting PMI and IMAC before transplantation and those affecting mean changes in serum HMW-ADPN levels and PMI were analysed using multiple regression analysis. In addition, factors that affected the development of posttransplant diabetes mellitus were assessed by multiple logistic regression analysis. The statistical software Stat Flex Ver6 (Artech Co., Ltd., Osaka, Japan) was used for analyses.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39, 412–423. https://doi.org/10.1093/ageing/afq034 (2010).
Landi, F. et al. Sarcopenia as a risk factor for falls in elderly individuals: Results from the ilSIRENTE study. Clin. Nutr. 31, 652–658. https://doi.org/10.1016/j.clnu.2012.02.007 (2012).
Cruz-Jentoft, A. J. et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 43, 748–759. https://doi.org/10.1093/ageing/afu115 (2014).
Burks, T. N. et al. Losartan restores skeletal muscle remodeling and protects against disuse atrophy in sarcopenia. Sci. Transl. Med. 3, 82ra37. https://doi.org/10.1126/scitranslmed.3002227 (2011).
de Brito-Ashurst, I., Varagunam, M., Raftery, M. J. & Yaqoob, M. M. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J. Am. Soc. Nephrol. 20, 2075–2084. https://doi.org/10.1681/ASN.2008111205 (2009).
Hamaguchi, Y. et al. Impact of quality as well as quantity of skeletal muscle on outcomes after liver transplantation. Liver Transpl. 20, 1413–1419. https://doi.org/10.1002/lt.23970 (2014).
Marcus, R. L., Addison, O., Kidde, J. P., Dibble, L. E. & Lastayo, P. C. Skeletal muscle fat infiltration: Impact of age, inactivity, and exercise. J. Nutr. Health Aging 14, 362–366. https://doi.org/10.1007/s12603-010-0081-2 (2010).
Bachmann, O. P. et al. Effects of intravenous and dietary lipid challenge on intramyocellular lipid content and the relation with insulin sensitivity in humans. Diabetes 50, 2579–2584. https://doi.org/10.2337/diabetes.50.11.2579 (2001).
Kitajima, Y. et al. Severity of non-alcoholic steatohepatitis is associated with substitution of adipose tissue in skeletal muscle. J. Gastroenterol. Hepatol. 28, 1507–1514. https://doi.org/10.1111/jgh.12227 (2013).
Hara, K. et al. Measurement of the high-molecular weight form of adiponectin in plasma is useful for the prediction of insulin resistance and metabolic syndrome. Diabetes Care 29, 1357–1362. https://doi.org/10.2337/dc05-1801 (2006).
Rajala, M. W. & Scherer, P. E. Minireview: The adipocyte—at the crossroads of energy homeostasis, inflammation, and atherosclerosis. Endocrinology 144, 3765–3773. https://doi.org/10.1210/en.2003-0580 (2003).
Li, F. et al. Myokines and adipokines: Involvement in the crosstalk between skeletal muscle and adipose tissue. Cytokine Growth Factor Rev. 33, 73–82. https://doi.org/10.1016/j.cytogfr.2016.10.003 (2017).
Adachi, H. et al. Adiponectin fractions influence the development of posttransplant diabetes mellitus and cardiovascular disease in Japanese Renal Transplant Recipients. PLoS One 11, e0163899. https://doi.org/10.1371/journal.pone.0163899 (2016).
Okada-Iwabu, M. et al. A small-molecule AdipoR agonist for type 2 diabetes and short life in obesity. Nature 503, 493–499. https://doi.org/10.1038/nature12656 (2013).
Johansen, K. L., Delgado, C., Bao, Y. & Kurella Tamura, M. Frailty and dialysis initiation. Semin. Dial. 26, 690–696. https://doi.org/10.1111/sdi.12126 (2013).
McAdams-DeMarco, M. A. et al. Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J. Am. Geriatr. Soc. 61, 896–901. https://doi.org/10.1111/jgs.12266 (2013).
Fahal, I. H. Uraemic sarcopenia: Aetiology and implications. Nephrol. Dial. Transplant. 29, 1655–1665. https://doi.org/10.1093/ndt/gft070 (2014).
Kobayashi, I. et al. Geriatric Nutritional Risk Index, a simplified nutritional screening index, is a significant predictor of mortality in chronic dialysis patients. Nephrol. Dial. Transplant. 25, 3361–3365. https://doi.org/10.1093/ndt/gfq211 (2010).
Painter, P. Physical functioning in end-stage renal disease patients: Update 2005. Hemodial. Int. 9, 218–235. https://doi.org/10.1111/j.1492-7535.2005.01136.x (2005).
Ikizler, T. A., Flakoll, P. J., Parker, R. A. & Hakim, R. M. Amino acid and albumin losses during hemodialysis. Kidney Int. 46, 830–837. https://doi.org/10.1038/ki.1994.339 (1994).
Mitch, W. E., Du, J., Bailey, J. L. & Price, S. R. Mechanisms causing muscle proteolysis in uremia: The influence of insulin and cytokines. Miner. Electrolyte Metab. 25, 216–219. https://doi.org/10.1159/000057450 (1999).
Carmeli, E., Coleman, R. & Reznick, A. Z. The biochemistry of aging muscle. Exp. Gerontol. 37, 477–489. https://doi.org/10.1016/s0531-5565(01)00220-0 (2002).
Iwabu, M. et al. Adiponectin and AdipoR1 regulate PGC-1alpha and mitochondria by Ca(2+) and AMPK/SIRT1. Nature 464, 1313–1319. https://doi.org/10.1038/nature08991 (2010).
Loncar, G. et al. Association of adiponectin with peripheral muscle status in elderly patients with heart failure. Eur. J. Int. Med. 24, 818–823. https://doi.org/10.1016/j.ejim.2013.09.011 (2013).
Huang, C. et al. High circulating adiponectin levels predict decreased muscle strength among older adults aged 70 years and over: A prospective cohort study. Nutr. Metab. Cardiovasc. Dis. 25, 594–601. https://doi.org/10.1016/j.numecd.2015.03.010 (2015).
Krause, M. P. et al. Adiponectin is expressed by skeletal muscle fibers and influences muscle phenotype and function. Am. J. Physiol. Cell Physiol. 295, C203-212. https://doi.org/10.1152/ajpcell.00030.2008 (2008).
Ingelsson, E. et al. Associations of serum adiponectin with skeletal muscle morphology and insulin sensitivity. J. Clin. Endocrinol. Metab. 94, 953–957. https://doi.org/10.1210/jc.2008-1772 (2009).
Ito, R. et al. Activation of adiponectin receptors has negative impact on muscle mass in C2C12 myotubes and fast-type mouse skeletal muscle. PLoS One 13, e0205645. https://doi.org/10.1371/journal.pone.0205645 (2018).
Schrager, M. A. et al. Sarcopenic obesity and inflammation in the InCHIANTI study. J. Appl. Physiol. 1985(102), 919–925. https://doi.org/10.1152/japplphysiol.00627.2006 (2007).
Abbatecola, A. M. et al. Insulin resistance and muscle strength in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 60, 1278–1282. https://doi.org/10.1093/gerona/60.10.1278 (2005).
Almurdhi, M. M. et al. Reduced lower-limb muscle strength and volume in patients with type 2 diabetes in relation to neuropathy, intramuscular fat, and vitamin D levels. Diabetes Care 39, 441–447. https://doi.org/10.2337/dc15-0995 (2016).
Landi, F. et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: Results from ilSIRENTE study. Age Ageing 42, 203–209. https://doi.org/10.1093/ageing/afs194 (2013).
Akima, H. et al. Relationship between quadriceps echo intensity and functional and morphological characteristics in older men and women. Arch. Gerontol. Geriatr. 70, 105–111. https://doi.org/10.1016/j.archger.2017.01.014 (2017).
Dela, F. & Helge, J. W. Insulin resistance and mitochondrial function in skeletal muscle. Int. J. Biochem. Cell Biol. 45, 11–15. https://doi.org/10.1016/j.biocel.2012.09.019 (2013).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 53, 982–992. https://doi.org/10.1053/j.ajkd.2008.12.034 (2009).
Prado, C. M. et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 9, 629–635. https://doi.org/10.1016/S1470-2045(08)70153-0 (2008).
Acknowledgements
The authors gratefully acknowledge the help and assistance of their colleagues at the Department of Nephrology. This study was supported in part by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science; (C) 18K08256 (HY); Grants for Intractable Renal Disease Research and for Health and Labour Sciences Research from the Ministry of Health, Labour, and Welfare of Japan (HY); a Grant-in-Aid for Investigating New Evidences to Understand the safety of Kidney Transplantation from marginal Donors, Promotion of renal Disease Control Grants from Japan Agency for Medical Research and Development (KF, HY), Grants for a Syourei Study at Kanazawa Medical University (no. S2017-7) (HA) and Grants for a Cooperative Study at Kanazawa Medical University (no. C2017-4) (HY).
Author information
Authors and Affiliations
Contributions
H.A. contributed to the study design, clinical data collection, data analysis, and writing-original draft. K.F. contributed to clinical data collection, data analysis, and supervision. A.F., K.Y., K.O., T.M., and K.O. contributed to clinical data collection. K.F. contributed to supervision, and writing—review and editing. H.Y. contributed to conceptualization, funding acquisition, supervision, and writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adachi, H., Fujimoto, K., Fujii, A. et al. Long-term retrospective observation study to evaluate effects of adiponectin on skeletal muscle in renal transplant recipients. Sci Rep 10, 10723 (2020). https://doi.org/10.1038/s41598-020-67711-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67711-1
This article is cited by
-
Frailty and sarcopenia in older kidney transplant recipients: a cross-sectional study
European Geriatric Medicine (2023)
-
Tissue-specific role and associated downstream signaling pathways of adiponectin
Cell & Bioscience (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.