Abstract
Few studies have researched the gender-specific effects of electronic nicotine delivery systems on the metabolic syndrome (MetS) and/or its risk factors (central obesity, raised triglycerides, decreased HDL cholesterol, raised blood pressure, raised fasting plasma glucose). Thus, this study investigated the association between smoking behavior (cigarette type, smoking history) and MetS in a nationally representative sample of Korean men and women. Our study employed data for 5,462 cases of MetS and 12,194 controls from the Korea National Health and Nutritional Examination Survey (KNHANES) for the years 2014 to 2017. Logistic regression analysis was employed to determine the association between type of cigarette (non-smoker, ex-smoker, and current smoker—conventional only, current smoker—conventional and electronic) and the prevalence of metabolic syndrome and its risk factors. Smoking history was clinically quantified by pack-year. No association between cigarette type and MetS was found for men. For women, relative to non-smokers, smokers of conventional cigarettes (OR 1.80, 95% CI 1.02–3.18) and both conventional and electronic cigarettes (OR 4.02, 95% CI 1.48–10.93) had increased odds of MetS. While there was no association between smoking history and MetS for women, for men, conventional smoking history was associated with MetS for individuals with a smoking history of > 25 pack-years (> 25 to ≤ 37.5 OR 1.45, 95% CI 1.04–2.02; > 37.5 to ≤ 50 OR 1.53, 95% CI 1.08–2.18; > 50 OR 1.56, 95% CI 1.07–2.27). Sex differences were found in the association between smoking behavior and MetS. Such findings reveal sociodemographic differences that should be considered for interventions regarding conventional and/or e-cigarette users at risk of metabolic complications.
Similar content being viewed by others
Introduction
The metabolic syndrome (MetS) and its risk factors (central obesity, raised triglycerides, decreased HDL cholesterol, raised blood pressure, raised fasting plasma glucose) have been vital in helping identify individuals at risk of type 2 diabetes and cardiovascular disease (CVD). Although a catalyst for heart disease, lipid problems, hypertension, dementia, cancer, polycystic ovarian syndrome, and non-alcoholic fatty liver disease1, the mechanisms underlying the development of MetS remain obscure. What is certain is that a growing body of literature asserts that various lifestyle factors including smoking, alcohol consumption2, diet, and physical activity3 contribute to its onset.
Electronic nicotine delivery systems, also known as e-cigarettes, are battery-powered products that deliver nicotine in the form of an aerosol4. Currently, the ever use of e-cigarettes is 8.5% in the United States and 6.6% in South Korea5. Often advertised as a “healthier” alternatives to conventional cigarettes or smoking cessation aids, e-cigarettes purportedly do not involve tobacco combustion and therefore, have reduced toxicant exposure compared to traditional cigarettes6.
However, research on long-term toxicity has been limited and studies attempting to show the efficacy of e-cigarettes as a healthier alternative to conventional smoking have had mixed results6. In particularly, while many studies have found a positive association between conventional cigarette smoking and the metabolic syndrome7,8,9,10,11, few have examined the effects of e-cigarettes, on MetS and/or its risk factors.
The existing body of literature on the effects of e-cigarettes on lipid profile is both limited and inconsistent. In one study, e-cigarettes were associated with weight loss and a decrease in some participants’ blood sugar and cholesterol levels12. In another study, users of e-cigarettes who completely quit regular cigarette smoking were less likely to report weight gain when compared with continuing smokers and reducers13. In a study comparing Wistar rats administered and not administered with e-liquid with nicotine exposure, a significant decrease in cholesterol and LDL levels were found in the e-cigarette group14. In a recent study comparing e-cigarette smokers to non-smokers, e-cigarette use was found to be associated with systemic oxidative stress, which is an indirect catalyst of cardiovascular risk15.
Conversely, in another study of mice exposed to e-cigarettes, it was shown that when exposed to equivalent doses of nicotine as conventional cigarettes, the weight reducing effects of nicotine were not found16. In another study of the effects of e-cigarettes on heart rate and blood pressure, it was found that e-cigarettes have no effect on blood pressure or pulse among daily users17 although it should be noted that Konstatinos Farsalinos has a long history of funding from e-cigarette companies.
Thus, scholars have emphasized that the metabolic effects of e-cigarettes should be further evaluated, especially with direct comparisons of the health effects of e-cigarettes with those of conventional cigarettes18. In the present study, we examined the association between electronic cigarette and/or conventional cigarette usage and MetS. This association was also stratified for the following risk factors of MetS: central obesity, raised triglycerides, decreased HDL cholesterol, raised blood pressure, raised fasting plasma glucose.
Materials and methods
Study population and data
This study was conducted using data from the Korea National Health and Nutrition Examination Survey (KNHANES). The KNHANES aims to evaluate the health and nutritional status of South Koreans and provide data for the development and evaluation of health policies and programs in Korea. The survey produces statistics regarding smoking, drinking, physical activity, and obesity for the WHO19 and the Organization for Economic Cooperation and Development (OECD).
The KNHANES is conducted by the Korean Ministry of Health and Welfare in conjunction with the Centers for Disease Control and Prevention (CDC). Survey data is obtained by specially trained interviewers who are not provided with any prior information about participants. Surveys are performed throughout 192 regions each year and 10,000 individuals ≥ 1 year of age are targeted.
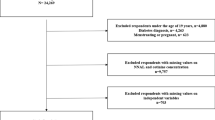
For the purpose of our study, we examined the data of 17,656 individuals who participated in the survey between the years of 2014 and 2017. 1,738 individuals diagnosed by a medical professional with type 1 or type 2 diabetes were excluded from our study, as well as subjects with missing information about cigarette type, smoking history (pack-year), and/or the risk factors of MetS.
Measures
Outcome variable
In this study, the prevalence of the metabolic syndrome and its components was selected as the outcome variable. The presence of MetS was measured using the International Diabetes Federation’s definition specific to South Asians2. According to the IDF’s worldwide definition, those with MetS are required to be centrally obese (measured by a waist circumference of ≥ 90 cm if male and ≥ 80 cm if female), as well as have two of the following four features: (1) an increased triglyceride level of ≥ 150 mg/dL or specific treatment; (2) a decreased high density lipoprotein cholesterol level of < 40 mg/dL in men and < 50 mg/dL in women or specific treatment; (3) raised blood pressure, indicated by a systolic blood pressure of ≥ 130 mmHg, a diastolic blood pressure of ≥ 85 mmHg, or treatment of previously diagnosed hypertension; and (4) an increased fasting plasma glucose level of ≥ 100 mg/dL or previously diagnosed type 2 diabetes. Such components, as well as all health-related components of the KNHANES, were collected via standardized physical examination by medical technicians serving as staff members for the survey2.
Cigarette type
The survey asked all subjects whether they used cigarettes or e-cigarettes currently or had ever used these products during their lifetime. Accordingly, we classified the subjects into four categories: non-smoker, ex-smoker, current smoker (conventional only), and current smoker (conventional and electronic). This classification was in accordance with that of previous studies investigating cigarette type with the same survey instrument20.
Covariates
Demographic, socioeconomic, and health-related covariates were included in this study. Covariates included age (20–29, 30–39, 40–49, 50–59, 60–69, ≥ 70), smoking history (≤ 5, > 5 to ≤ 10, > 10 to ≤ 15, > 15 to ≤ 20, > 20 to ≤ 25, > 25 to ≤ 37,0.5, > 37.5 to ≤ 50, > 50)21, level of physical activity (low, high), region (urban, rural), high-risk drinking (no, yes), menopause (no, yes- natural, yes-sartificial)22, serum hs-CRP levels (low: less than or equal to 3.0 mg/L, high: above 3.0 mg/L)23, household income group (low, medium–low, medium–high, high), occupation (white collar, sales and services, blue collar), and educational attainment (≤ elementary school, middle school, high school diploma, ≥ bachelor’s degree) and year of survey (2014, 2015, 2016, 2017). The International Physical Activity Questionnaire was adopted to determine the level of physical activity. “High” physical activity was defined as ≥ 20 min of vigorous-intensity physical activity for ≥ 3 days a week, or ≥ 30 min of light- or moderate-intensity physical activity ≥ 5 days a week24. Income groups were obtained by dividing household income by the square root of the number of members in a household, which is the standard method recommended by the Organization for Economic Cooperation and Development (OECD)25.
Statistical analysis
To examine the association between cigarette type and MetS, as well as its risk factors, multivariate logistic regression analysis was performed using weighted data, while controlling for all demographic, socioeconomic, and health-related covariates. Odds ratios and 95% confidence intervals26 were calculated to compare non-smokers with ex-smokers, current smokers (conventional only), and current smokers (conventional and electronic). The calculated p-values in this study were considered significant if lower than 0.05. All analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Table 1 presents the general characteristics of our study population. 5,462 cases of MetS and 12,194 controls were analyzed from the Korea National Health and Nutritional Examination Survey (KNHANES) for the years 2014 to 2017. Among cases of MetS, 45.9% were males and 54.1% were females. Among controls, 37.6% were males and 62.4% were females.
Table 2 presents the factors associated with MetS, found through the results of our logistic regression analysis. While there was no association between cigarette type and MetS for men, for women, relative to non-smokers, smokers of conventional cigarettes (OR 1.80, 95% CI 1.02–3.18) and both conventional and electronic cigarettes (OR 4.02, 95% CI 1.48–10.93) had increased odds of MetS. While there was no association between smoking history and MetS for women, for men, conventional smoking history was associated with MetS for individuals with a smoking history of > 25 pack-years (> 25 to ≤ 37.5 OR 1.45, 95% CI 1.04–2.02; > 37.5 to ≤ 50 OR 1.53, 95% CI 1.08–2.18; > 50 OR 1.56, 95% CI 1.07–2.27). A high level of physical activity was associated with decreased odds of MetS for both males (OR 0.88, 95% CI 0.80–0.98) and females (OR 0.85, 95% CI 0.78–0.94) compared to low, while high-risk drinking was associated with increased odds of MetS for both males (OR 1.89, 95% CI 1.67–2.14) and females (OR 1.52, 95% CI 1.21–1.91). Females with artificial menopause also had increased odds of MetS (OR 1.54, 95% CI 1.54–1.23–1.92). A serum hs-CRP level greater than 3.0 mg/L was associated with increased odds of MetS for both males (OR 1.51, 95% CI 1.26–1.80) and females (OR 2.45, 95% CI 2.01–2.98).
Figures 1 and 2 show the association between cigarette usage and the odds of MetS and its components for both males and females. For females, the combined usage of both conventional and electronic cigarettes was associated with increased odds of high triglycerides (OR 3.90, 95% CI 1.54–9.89) and high fasting plasma glucose (OR 2.73, 95% CI 1.02–7.31).
Discussion
We found that the prevalence of MetS was significantly associated with cigarette type for females only. We also found that for females, cigarette type was associated with some of the components of MetS (high triglycerides, high fasting plasma glucose levels). This was in alignment with some previous studies which show that type of both conventional and electronic cigarettes is higher in toxicity than single type of the conventional cigarette only27,28. Interestingly, raised blood pressure was not associated with electronic cigarette type although previous studies have noted that electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers (age: 30 ± 8 years)29.
What is undeniable is that cigarette smoking is associated with increased total cholesterol, low-density lipoprotein, while decreasing the cardio-protective high-density lipoprotein18. Smoking cessation has also been associated with decreased odds of MetS after a certain period of time18. While our study shows no clear association between MetS and cigarette type with regard to the type of smoke used (conventional vs. conventional and electronic), the conventional smoking history variable continuously shows that a pack year of 20 or above is consistently associated with increased odds of MetS, central obesity, high triglycerides, low HDL cholesterol, high blood pressure, and high fasting plasma glucose among males. Our findings show that while cigarette type may be relevant for female users, for male users, the number and duration of cigarettes smoked may be more important.
Regarding sexual differences, previous studies have acknowledged that smoking is more strongly associated with insulin resistance and increased cardiovascular risk among women than men28. More research is necessary to determine how cigarette type and/or type may be more hazardous, than smoking history for women, as opposed to men. This study has several limitations that must be taken into consideration. Firstly, cigarette type, as well as variables related to smoking history and health-related behaviors were measured and classified based on self-reports, meaning that there may be various recall and information biases. A more accurate analysis would be possible if health-related behaviors could be measured through medical tests e.g. a urinary cotinine test for tobacco use. Likewise, in the KNHANES, individuals were not asked about e-cigarette use in the past, and so exclusive ex-smokers of e-cigarettes could not be separated from conventional ex-smokers in our main analysis, nor could the history or duration of e-cigarette smoking be adjusted for in pack-years.
Our study population was limited to adults, however, many studies have highlighted the popularity of e-cigarette and dual e-cigarette and tobacco use among middle and high school adolescents which future studies should take into account28, 30. Also, complete causal inferences are impossible to determine because the study design is cross-sectional and does not allow for lifetime trajectories of smoking, smoking cessation, and/or the development of MetS over time. Studies have shown that the risk of metabolic syndrome can persist up to 20 years after the cessation of smoking31. Thus, it is impossible to know if the use of e-cigarettes, and/or conventional cigarettes is responsible for the onset of MetS or its risk factors.
Likewise, some valuable but unknown or immeasurable confounders may have been excluded from our analysis because of the study design. Factors such as lifetime smoking trajectories, and/or the use of medications like statin were immeasurable from our data but likely had an effect on the association between cigarette type and MetS. Furthermore, because of the cross-sectional nature of our data, reverse causality bias is a concern; individuals with unhealthy profiles for MetS components may have been induced to stop smoking or not use e-cigarettes. This must be taken into account when interpreting our results. Lastly, other parameters that have recently been linked to MetS including levels of plasminogen activator inhibitor-1 (PAI-1) should be considered in future studies.
Despite these limitations, this investigation shows a statistically significant association between cigarette type and MetS, which adheres to the existing body of literature that debates over this relationship. It also implies that smoking both conventional cigarettes and electronic cigarettes is more hazardous for MetS and its causal factors, relative to not smoking, previously smoking, and /or smoking conventional cigarettes only.
Although South Korea has a relatively low prevalence rate of MetS compared to the rest of the OECD, our results suggest that the rate can be lowered even further if individuals are educated of such ideas. Such findings also reveal opportunities for intervention with regard to conventional and/or e-cigarette users at risk of metabolic complications.
References
Wilson, P. W., D’Agostino, R. B., Sullivan, L. & Meigs, J. Metabolic syndrome and risk of CVD and type 2 diabetes mellitus. Circulation 107, E7004–E7004 (2003).
Oh, S. S., Kim, W., Han, K.-T., Park, E.-C. & Jang, S.-I. Alcohol consumption frequency or alcohol intake per drinking session: which has a larger impact on the metabolic syndrome and its components?. Alcohol 71, 15–23 (2018).
Yoon, S. H. et al. Combined effect of body mass index and body size perception on metabolic syndrome in South Korea: results of the fifth Korea National Health and Nutrition Examination Surveys (2010–2012). BMC Public Health 15, 554 (2015).
4Schoenborn, C. A. & Gindi, R. M. Electronic cigarette use among adults: United States, 2014. (US Department of Health and Human Services, Centers for Disease Control and …, 2015).
Lee, J. A., Kim, S. H. & Cho, H.-J. Electronic cigarette use among Korean adults. Int. J. Public Health 61, 151–157. https://doi.org/10.1007/s00038-015-0763-y (2016).
Callahan-Lyon, P. Electronic cigarettes: human health effects. Tobacco Control 23, ii36–ii40 (2014).
Bermudez, V. et al. Cigarette smoking and metabolic syndrome components: a cross-sectional study from Maracaibo City, Venezuela. F1000Res 7, 565. https://doi.org/10.12688/f1000research.14571.3 (2018).
Cheng, E. et al. Light smoking is associated with metabolic syndrome risk factors in Chilean young adults. Acta Diabetol. 56, 473–479. https://doi.org/10.1007/s00592-018-1264-2 (2019).
Kim, J. Y., Yang, Y. & Sim, Y. J. Effects of smoking and aerobic exercise on male college students’ metabolic syndrome risk factors. J. Phys. Ther. Sci. 30, 595–600. https://doi.org/10.1589/jpts.30.595 (2018).
Owczarczyk-Saczonek, A. B. & Nowicki, R. The association between smoking and the prevalence of metabolic syndrome and its components in patients with psoriasis aged 30 to 49 years. Postepy Dermatol. Alergol. 32, 331–336. https://doi.org/10.5114/pdia.2015.54743 (2015).
Yankey, B. N., Strasser, S. & Okosun, I. S. A cross-sectional analysis of the association between marijuana and cigarette smoking with metabolic syndrome among adults in the United States. Diabetes Metab. Syndr. 10, S89-95. https://doi.org/10.1016/j.dsx.2016.03.001 (2016).
Glover, M., Breier, B. H. & Bauld, L. Could vaping be a new weapon in the battle of the bulge?. Nicotine Tob. Res. 19, 1536–1540 (2016).
Russo, C. et al. Evaluation of post cessation weight gain in a 1-year randomized smoking cessation trial of electronic cigarettes. Scientific reports 6, 18763 (2016).
El Golli, N. et al. Comparison between electronic cigarette refill liquid and nicotine on metabolic parameters in rats. Life Sci. 146, 131–138. https://doi.org/10.1016/j.lfs.2015.12.049 (2016).
Moheimani, R. S. et al. Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: implications for cardiovascular risk. JAMA Cardiol. 2, 278–284 (2017).
Ponzoni, L. et al. Different physiological and behavioural effects of e-cigarette vapour and cigarette smoke in mice. Eur. Neuropsychopharmacol. 25, 1775–1786 (2015).
Farsalinos, K. et al. Effect of continuous smoking reduction and abstinence on blood pressure and heart rate in smokers switching to electronic cigarettes. Intern. Emerg. Med. 11, 85–94 (2016).
Verhaegen, A. & Van Gaal, L. Do E-cigarettes induce weight changes and increase cardiometabolic risk? A signal for the future. Obes. Rev. 18, 1136–1146 (2017).
WHO. Global status report on alcohol and health. Global Alcohol Report (2014).
Choi, D.-W. et al. Association between smoking behavior patterns and glycated hemoglobin levels in a general population. Int. J. Environ. Res. Public Health 15, 2260 (2018).
Siemiatycki, J., Karp, I., Sylvestre, M.-P. & Pintos, J. Estimating the proportion of cases of lung cancer legally attributable to smoking: a novel approach for class actions against the tobacco industry. Am. J. Public Health 104, e60–e66. https://doi.org/10.2105/AJPH.2014.302040 (2014).
Jung, S. J., Shin, A. & Kang, D. Hormone-related factors and post-menopausal onset depression: Results from KNHANES (2010–2012). J. Affect. Disord. 175, 176–183. https://doi.org/10.1016/j.jad.2014.12.061 (2015).
Lee, S., Oh, S. S., Jang, S.-I. & Park, E.-C. Sex difference in the association between high-sensitivity C-reactive protein and depression: the 2016 Korea National Health and Nutrition Examination Survey. Sci. Rep. 9, 1918. https://doi.org/10.1038/s41598-018-36402-3 (2019).
Kwon, Y.-J. et al. Long sleep duration is associated with sarcopenia in Korean adults based on data from the 2008–2011 KNHANES. J. Clin. Sleep Med. 13, 1097–1104. https://doi.org/10.5664/jcsm.6732 (2017).
Lee, K. Income movement in South Korea: current status and characteristics. Defence Peace Econ. 15, 55–77. https://doi.org/10.1080/10242694.2014.960247 (2009).
Radaelli, G. et al. Causes of mortality in early infantile epileptic encephalopathy: a systematic review. Epilepsy Behav. 85, 32–36. https://doi.org/10.1016/j.yebeh.2018.05.015 (2018).
Borderud, S. P., Li, Y., Burkhalter, J. E., Sheffer, C. E. & Ostroff, J. S. Electronic cigarette use among patients with cancer: characteristics of electronic cigarette users and their smoking cessation outcomes. Cancer 120, 3527–3535 (2014).
Wills, T. A., Knight, R., Williams, R. J., Pagano, I. & Sargent, J. D. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics 135, e43–e51 (2015).
Vlachopoulos, C. et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers. J. Am. Coll. Cardiol. 67, 2802–2803 (2016).
Cho, J. H., Shin, E. & Moon, S.-S. Electronic-cigarette smoking experience among adolescents. J. Adolesc. Health 49, 542–546 (2011).
Wada, T., Urashima, M. & Fukumoto, T. Risk of metabolic syndrome persists twenty years after the cessation of smoking. Intern. Med. 46, 1079–1082 (2007).
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine (6-2018-0174 and 6-2017-0157).
Author information
Authors and Affiliations
Contributions
S.S.O. wrote the main manuscript text and conducted all statistical analyses. J.J. and D.L. assisted with the statistical analyses. E.C.P. and S.I.J. reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oh, S.S., Jang, JE., Lee, DW. et al. Cigarette type or smoking history: Which has a greater impact on the metabolic syndrome and its components?. Sci Rep 10, 10467 (2020). https://doi.org/10.1038/s41598-020-67524-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67524-2
This article is cited by
-
Association between having a meal together with family and smoking: a cross-sectional nationwide survey
BMC Public Health (2023)
-
Association between smoking and obstructive sleep apnea based on the STOP-Bang index
Scientific Reports (2023)
-
Temporal associations between leukocytes DNA methylation and blood lipids: a longitudinal study
Clinical Epigenetics (2022)
-
Risk factors for metabolic syndrome in individuals with recent-onset psychosis at disease onset and after 1-year follow-up
Scientific Reports (2022)
-
Synergistic associations of visual and self-reported hearing acuity with low handgrip strength in older adults: a population-based cross-sectional study
BMC Geriatrics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.