Abstract
Kyphoplasty is the standard surgical treatment of vertebral compression fractures. We aimed to clarify the influence of kyphoplasty on the sagittal profile as well as the relation between posture improvement and pain relief. For this purpose, we evaluated various radiological parameters of the sagittal profile on whole spine standing radiographs of 73 Patients with a single vertebral fracture treated by kyphoplasty. The key outcome was the postoperative change of the sagittal vertical axis (SVA). Additionally, clinical parameters including pain scores on visual analogue scale (VAS) and use of analgesics were obtained from medical records. Pre- and postoperative radiological as well as clinical parameters were compared. Additionally, the correlation between changes of SVA and changes of local kyphotic angle (LKA) or VAS was examined. The clinical parameters as well as various radiographic parameters (SVA, LKA, Gardner, Cobb) improved significantly postoperatively. The improvement of SVA correlated significantly with the correction of the LKA but not with postoperative pain relief. We conclude that kyphoplasty helps to restore the global sagittal balance of the spine after vertebral fractures. The correction of the sagittal profile seems to depend on the correction of the local kyphotic angle but does not correlate with postoperative pain relief.
Similar content being viewed by others
Introduction
Osteoporosis is a major cause of fractures in elderly patients, leading to more than 8.9 million fractures per year worldwide1. The most common type of osteoporotic fractures are vertebral fractures2. With around 1 million incident vertebral fractures per year in Europe alone, causing costs of estimated €377 million, they constitute a major therapeutic and socioeconomic challenge in aging societies3,4.
Despite their high relevance, there is still no clear consensus regarding the optimal treatment. As osteoporotic fractures are mainly stable compression fractures, both conservative and operative treatment options can be considered5. Regarding operative treatment options, vertebroplasty and kyphoplasty are the most widely used techniques. While vertebroplasty mainly aims at quick pain relief by stabilizing the fractured vertebra with bone cement, kyphoplasty additionally offers the possibility to correct fracture-related deformities by inflating a balloon in the fractured vertebral body before filling it with bone cement. The efficacy of kyphoplasty for short-term pain relief is well documented and widely accepted6,7. However, the advantage of kyphoplasty over conservative therapy regarding pain relief seems to diminish over time8. Additionally, there is so far no study comparing the pain relief of kyphoplasty to the placebo-effect of a sham procedure8. Therefore, the key factors for the evaluation of the long-term benefit/risk ratio of kyphoplasty seem to be the restoration of lost vertebral body height and the correction of fracture-related spinal malposition.
Such spinal malposition can have various implications. In many cases, vertebral compression fractures result in a kyphosis of the affected vertebral body. The effects are not restricted to the area of the fracture but rather affect the spine as a whole. Any increase of kyphosis will inevitably shift the center of gravity ventrally, thereby changing the weight force distribution of the remaining vertebral bodies. This explains why hyperkyphosis is not only a common result of vertebral compression fractures, but also in itself an independent risk factor for future fractures9. Also, thoracic kyphosis and lumbar lordosis are positively correlated, so that thoracic hyperkyphosis may result in a compensatory increase in lumbar lordosis10. A higher lumbar lordosis has been reported to be associated with lower back pain11.
There is consistent evidence that kyphoplasty can achieve (partial) height restoration of the fractured vertebrae12,13,14. Yet, the effect of these local changes on the global sagittal profile of the spine has been hardly examined so far. Only few studies have been conducted in small populations and came to conflicting conclusions15,16,17,18. This lack of knowledge about the potential long-term benefits constitutes an important limitation when trying to determine the appropriate indication of the kyphoplasty. As a result, most guidelines remain rather vague and recommend the intervention only after a futile conservative treatment attempt5. The potential long-term advantages of a restored sagittal profile are not taken into account as no reliable evidence to this effect is available.
Therefore, more detailed knowledge about the effect of kyphoplasty on the sagittal profile of the spine is urgently needed for a differentiated evaluation of the long-term risk/benefit ratio and to thereby allow for more precise treatment recommendations for vertebral compression fractures.
In the present study, we hypothesized that percutaneous balloon kyphoplasty has a significant impact on parameters of the sagittal profile of the spine and conducted a retrospective analysis of patients treated in our department.
Materials and methods
Patients
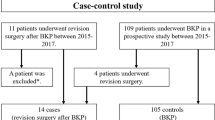
For this retrospective cohort study we included consecutive patients that received balloon kyphoplasty of a single vertebra due to a vertebral compression fracture between January 2014 and December 2018. Kyphoplasty was performed in a standardized manner with the patients being placed in a lordosing prone position and using a biportal technique. Only patients with pre- and postoperative upright whole spine radiographs obtained within not more than 30 days before and after the operation were eligible. All patients had undergone a futile conservative treatment attempt prior to the operation. Patients were excluded if they had received additional spinal operations (e.g. instrumented spinal fusion) or sustained new vertebral fractures between pre- and postoperative radiographs. Patients were also excluded if they had undergone a prior instrumented spinal fusion including L5/S1 as this would not have allowed a reliable measurement of spinopelvic parameters.
Data collection and image analysis
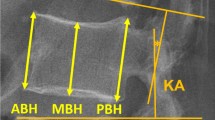
Pre- and postoperative lateral whole spine standing radiographs were evaluated regarding radiologic parameters of fracture morphology and global sagittal profile (Fig. 1). Image analysis was carried out in a standardized manner according to previously published methods using Centricity DICOM Viewer (GE Healthcare, Buckinghamshire, United Kingdom)19. The mean values from independent measurements by two reviewers (a spinal surgeon experienced with the measurements of radiologic spinal parameters and an associate researcher who received prior training) were used for statistical analysis in order to minimize the risk of systematic bias. The following parameters were measured: angle between cephalad and caudad endplate of the fractured vertebra (local kyphotic angle, LKA); angle between the cephalad endplate of the vertebra proximally adjacent to the fracture and the caudad endplate of the fractured vertebra (Gardner angle, GA); angle between the cephalad endplate of the vertebra proximally adjacent to the fracture and the caudad endplate of the vertebra distally adjacent to the fracture (Cobb angle, CA); distance between the C7 plumb line and the rear edge of S1 (sagittal vertical axis, SVA); angle between the sacral endplate and a horizontal reference line (sacral slope, SS); angle formed by a line connecting the centre of the hip with the centre of the sacral endplate and a vertical reference line (pelvic tilt, PT); angle between the cephalad endplate of L1 and the caudad endplate of L5 (lumbar lordosis, LL); angle between the caudad endplate of Th12 and the sacral endplate (thoracolumbosacral lordosis, TLSL); angle between the cephalad endplate of Th10 and the caudad endplate of L3 (thoracolumbal alignment, TLA); and the angle between the cephalad endplate of Th4 and the caudad endplate of Th12 (thoracal kyphosis, TK). The key outcome was defined as the postoperative change in SVA.
Global and Local Radiographic Parameters (Cobb: Cobb angle, Gardner: Gardner angle, LKA: locaFigurephotic angle, LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SS: sacral slope, SVA: sagittal vertical alignment, TK: thoracic kyphosis, TLA: thoraco-lumbar alignment, TLSL: thoraco-lumbo-sacral lordosis). Figure adapted from19 with kind permission from the author and Deutscher Ärzteverlag.
In addition, clinical data including the presumed time of the fracture (defined as the moment of symptom onset), pre- and postoperative pain at rest or in motion (on visual analog scale, VAS) and need of analgesics (according to WHO Analgesic Ladder) were obtained from the medical records.
Statistical analysis
Statistical analysis was performed using SPSS software version 23 (IBM, New York, USA). Mean and standard deviation were calculated for descriptive patient characteristics. Pre- and postoperative values for VAS scores (at rest and in motion) and radiographic measurements were compared using Student's t-test for paired samples. Pre- and postoperative need for analgesics according to the WHO pain ladder were tested for significant differences using Wilcoxon signed-rank test. The difference between pre- and postoperative radiographic parameters was tested for correlation with pre- and postoperative differences in VAS score and LKA by calculating Pearson's correlation coefficient.
Ethics approval
The study was approved by the institutional review board of Charité – Universitätsmedizin Berlin (EA1/188/18). The study was carried out in accordance with relevant guidelines and regulations.
Results
Study population
A total of 73 patients (average age 70 years) were identified that matched the inclusion criteria (Table 1). All included patients only had a single fracture, with 33 (45%) in the thoracic and 40 (55%) in the lumbar spine. 8 fractures were due to an adequate trauma and 65 fractures were not caused by an adequate trauma (atraumatic or due to low-energy trauma, i.e. a fall from standing height or below). Osteoporotic treatment with bisphosphonates was preoperatively documented in 14 (19%) patients. The average time between fracture and surgical intervention was 4.7 weeks, ranging from 1 to 40 weeks. The average time between preoperative X-ray and operation was 5.1 (±4.5) days, the average time between operation and postoperative X-ray was 2.8 (±3.3) days.
Pain scores
Patients showed a significant decrease in pain at rest and in motion (Table 2). Furthermore, comparison between pre- and postoperative need of analgesics according to the WHO pain ladder revealed a significant decrease of pain medication use after kyphoplasty (Z = −4.01, p <0.001).
Radiographic measurements
The detailed pre- and post-operative radiographic measurements are depicted in Table 3. In summary, the SVA significantly decreased post-operatively. Furthermore, LKA, Gardner and Cobb angle changed significantly. However, pelvic parameters as the PT did not change significantly. Inter-rater reliability was generally high with intraclass correlation coefficients ranging from 0.841 (postoperative LKA) to 0.995 (preoperative SVA).
Correlation of SVA with clinical and radiographic parameters
The correlation analysis revealed a significant correlation between pre-/postoperative difference in SVA and pre-/postoperative difference in LKA (Table 4). However, the change in SVA did not correlate to postoperative pain reduction.
Subgroup analyses of patients with positive sagittal imbalance
31 patients presented with a positive sagittal imbalance (defined as SVA > 50 mm) preoperatively. In the subgroup analysis of these patients, the mean SVA decreased from 84.36 (±32.48) to 58.61 (±33.3). The mean increase in SVA was 25.75 (±27.43) (p < 0.001). 25 patients still had a positive sagittal imbalance postoperatively.
Discussion
In the present work, we have conducted the largest study so far regarding the influence of kyphoplasty on the sagittal profile of the spine. Our results show a significant improvement of the SVA in patients with vertebral fractures after kyphoplasty. This result is of wide-ranging significance as it suggests a long-term benefit of kyphoplasty over conservative treatment. The results are in concordance with those from a smaller previous study, which included 21 patients17. However, two other previous studies did not find a significant change in SVA after kyphoplasty. One reason for this might be the timed passed since the occurrence of the fracture. In our study, the average time between fracture and kyphoplasty was 1.2 months. In both studies that did not find a change in SVA postoperatively, the time from injury to kyphoplasty was either much higher with an average of 3.4 months15 or not reported at all16. In a reverse conclusion, a long conservative treatment attempt might actually reduce the benefit of a subsequent kyphoplasty and cause sustained postural disadvantages to the patient as fracture consolidation hinders LKA restoration. However, there is no consistent data available yet regarding the influence of surgical timing on vertebral height restoration20,21,22.
Apart from the radiographic benefits of the operation, we also observed a significant pain reduction in our patients postoperatively. This is in keeping with existing studies on the short-term clinical outcome after kyphoplasty6,7. However, this observation might also raise suspicion regarding the origin of the postoperative SVA improvement. It seems plausible that pain relief by itself might lead to a more upright posture, even in the absence of a local height restoration of the fractured vertebra. In this case, one would have to suspect the effect of kyphoplasty on posture to be temporary as the acute fracture-related pain often fades over time under conservative treatment as well. Therefore, we examined for the first time whether the global postoperative changes of spinal alignment correlate rather with postoperative pain relief or vertebral body height restoration. Our results demonstrate that postoperative improvement in SVA correlates significantly with the correction of the LKA, but not with postoperative pain relief. This is remarkable, as it might indicate a long-lasting advantage of kyphoplasty over conservative treatment. However, it should be noted that the patients included in our study had (on average) only mild to moderate pain with an average VAS score of 3.7 at rest and 5.1 in motion. A stronger relationship between VAS and SVA might be conceivable in other populations where patients have stronger preoperative pain and therefore a more pronounced pain-related spinal malposition preoperatively. Theoretically, it is therefore possible that there might be an even better restoration of the sagittal profile in patients with stronger preoperative pain than in our cohort. However, this does not influence the correlation between LKA restoration and SVA improvement observed in our study independently from pain relief. Those to profit particularly from the procedure seem to be patients with a severely compromised posture preoperatively as the mean postoperative improvement in SVA was more than twice as high in patients with a positive sagittal imbalance preoperatively as compared to the general cohort.
Despite our efforts for a rigorous methodology to ensure reliable results, there are limitations to our study and the results should be interpreted accordingly. As the study relies on the assessment of retrospectively gathered patients treated with kyphoplasty, it is not possibly to precisely quantify the actual advantage over non-surgical treatment. Prospective studies will be needed to evaluate the long-term effect of the restoration of the sagittal profile on quality of life. Yet, existing literature indicates that the adverse effects of vertebral compression fractures on the quality of life, physical function, mental health, and life-span are related to the severity of the spinal deformity and partly independent of pain, which suggests a significant benefit from a restoration of the sagittal profile21,23,24. Finally, we performed multiple testing using data from the same patients, which may result in a risk of erroneous inferences. We this issue in our statistical analysis by rigorously adjusting the p-values according to the established Bonferroni-Holm method.
As a conclusion, we think that our data provide important new points to consider when deciding upon conservative vs. operative treatment in patients with vertebral fractures. While guidelines mainly recommend to consider kyphoplasty only after a futile conservative treatment attempt, treating physicians should also keep in mind that patients (especially those with a sagittal imbalance) might benefit from a restored posture irrespective of pain relief and that this might only be possible for a certain time after fracture occurrence.
References
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17, 1726–1733, https://doi.org/10.1007/s00198-006-0172-4 (2006).
Wasnich, R. D. Vertebral fracture epidemiology. Bone 18, 179S–183S (1996).
Finnern, H. W. & Sykes, D. P. The hospital cost of vertebral fractures in the EU: estimates using national datasets. Osteoporos Int 14, 429–436, https://doi.org/10.1007/s00198-003-1395-2 (2003).
Kasperk, C. et al. Treatment of painful vertebral fractures by kyphoplasty in patients with primary osteoporosis: a prospective nonrandomized controlled study. J Bone Miner Res 20, 604–612, https://doi.org/10.1359/JBMR.041203 (2005).
Dachverband Osteologie e.V. Prophylaxe, Diagnostik und Therapie der Osteoporose. (2017).
Berlemann, U., Franz, T., Orler, R. & Heini, P. F. Kyphoplas; ty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J 13, 496–501, https://doi.org/10.1007/s00586-004-0691-7 (2004).
Dong, R. et al. Pain reduction following vertebroplasty and kyphoplasty. Int Orthop 37, 83–87, https://doi.org/10.1007/s00264-012-1709-0 (2013).
Rodriguez, A. J. et al. Pain, Quality of Life, and Safety Outcomes of Kyphoplasty for Vertebral Compression Fractures: Report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res 32, 1935–1944, https://doi.org/10.1002/jbmr.3170 (2017).
Huang, M. H., Barrett-Connor, E., Greendale, G. A. & Kado, D. M. Hyperkyphotic; posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res 21, 419–423, https://doi.org/10.1359/JBMR.051201 (2006).
Roussouly, P. & Nnadi, C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19, 1824–1836, https://doi.org/10.1007/s00586-010-1476-9 (2010).
Sorensen, C. J., Norton, B. J., Callaghan, J. P., Hwang, C. T. & Van Dillen, L. R. Is lumbar lordosis related to low back pain development during prolonged standing? Man Ther 20, 553–557, https://doi.org/10.1016/j.math.2015.01.001 (2015).
Hiwatashi, A. et al. Kyphoplasty and vertebroplasty produce the same degree; of height restoration. AJNR Am J Neuroradiol 30, 669–673, https://doi.org/10.3174/ajnr.A1442 (2009).
Kim, K. H. et al. Kyphoplasty versus vertebroplasty: restoration of vertebral body height and correction of kyphotic deformity with special attention to the shape of the fractured vertebrae. J Spinal Disord Tech 25, 338–344, https://doi.org/10.1097/BSD.0b013e318224a6e6 (2012).
Yokoyama, K. et al. In not only vertebroplasty but also kyphop; lasty, the resolution of vertebral deformities depends on vertebral mobility. AJNR Am J Neuroradiol 34, 1474–1478, https://doi.org/10.3174/ajnr.A3424 (2013).
Kanayama, M., Oha, F., Iwata, A. & Hashimoto, T. Does balloon kyphoplasty improve the global spinal alignment in osteoporotic vertebral fracture? Int Orthop 39, 1137–1143, https://doi.org/10.1007/s00264-015-2737-3 (2015).
Korovessis, P., Zacharatos, S., Repantis, T., Michael, A. & Karachalios, D. Evolution of; bone mineral density after percutaneous kyphoplasty in fresh osteoporotic vertebral body fractures and adjacent vertebrae along with sagittal spine alignment. J Spinal Disord Tech 21, 293–298, https://doi.org/10.1097/BSD.0b013e31812e6295 (2008).
Yokoyama, K. et al. Postoperative change in sagittal balance after Kyphoplasty for the treatment of osteoporotic vertebral compression fracture. Eur Spine J 24, 744–749, https://doi.org/10.1007/s00586-014-3678-z (2015).
Pradhan, B. B., Bae, H. W., Kropf, M. A., Patel, V. V. & Delamarter, R. B. Kyphoplasty; reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine (Phila Pa 1976) 31, 435–441, https://doi.org/10.1097/01.brs.0000200036.08679.1e (2006).
Ferraris, L., Koller, H., Meier, O. & Hempfing, A. Die Bedeutung der sagittalen Balance in der Wirbelsäulenchirurgie. OUP 1, 502-508, doi:10.3238/oup.2012.0502–0508 (2012).
Oh, G. S. et al. Comparison of the results of balloon kyphoplasty performed at different times after injury. J Korean Neurosurg Soc 47, 199–202, https://doi.org/10.3340/jkns.2010.47.3.199 (2010).
Park, H. T. L., Chang Bum; Ha, Jeong Han; Choi, Sun Jin; Kim, Myoung Soo; Ha, Jung; Min. Results of kyphoplasty according to the operative timing. Current Orthopaedic Practice 21, p. 489-493 (2010).
Vivek Kushwaha, B. L. Vertebral height restoration after kyphoplasty. The Spine Journal 2, 120 (2002).
Gold, D. & Lyles, K. Fractures: effects on quality of life. in: Bilezikian JP, Glowacki J, Rosen CJ, eds. The Aging Skeleton San Diego: Academic Press, p. 373-382 (1999).
Silverman, S. L. The clinical consequences of vertebral compression; fracture. Bone 13(Suppl 2), S27–31, https://doi.org/10.1016/8756-3282(92)90193-z (1992).
Acknowledgements
Dr. Palmowski is participant in the BIH-Charité Junior Clinician Scientist Program funded by the Charité –Universitätsmedizin Berlin and the Berlin Institute of Health.
Author information
Authors and Affiliations
Contributions
Matthias Pumberger: conception and design of the work; interpretation of data; revising the work; approval of the submitted version. Florian Schitz: acquisition and interpretation of data; revising the work; approval of the submitted version. Justus Bürger: interpretation of data; revising the work; approval of the submitted version. Friederike Schömig: interpretation of data; revising the work; approval of the submitted version. Michael Putzier: conception and design of the work; interpretation of data; approval of the submitted version. Yannick Palmowski: conception and design of the work; acquisition, analysis and interpretation of data; drafting and revising the work; approval of the submitted version. All authors agree both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which they were not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pumberger, M., Schitz, F., Bürger, J. et al. Kyphoplasty Restores the Global Sagittal Balance of the Spine Independently from Pain Reduction. Sci Rep 10, 8894 (2020). https://doi.org/10.1038/s41598-020-65798-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65798-0
This article is cited by
-
Osteoporotische Wirbelkörperfrakturen der Brust- und Lendenwirbelsäule
Die Unfallchirurgie (2024)
-
The influence of osteoporotic vertebral fractures on global sagittal alignment in elderly patients: a systematic review and meta-analysis
European Spine Journal (2023)
-
Does kyphoplasty affect the global sagittal alignment in patients with osteoporotic vertebral fractures? A systematic review and meta-analysis
European Spine Journal (2023)
-
Osteoporotische Wirbelkörperfrakturen
Die Orthopädie (2023)
-
A nomogram for predicting residual low back pain after percutaneous kyphoplasty in osteoporotic vertebral compression fractures
Osteoporosis International (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.