Abstract
Elevated levels of serum uric acid (SUA) were considered to be risk factors for cardiovascular disease, it has been found to be associated with increased arteriosclerosis. The aim of this study was to explore the gender specific relationship between SUA and fundus arteriosclerosis in a healthy population. In a retrospective cross-sectional study, 23474 individuals without diabetes and hypertension were included in the present study. SUA levels were cut to four groups as Q1 to Q4, according to the quartiles. The odds ratio and 95% confidence interval of different SUA levels were estimated by a binomial logistic regression model. A restrictive cubic spline method was used to estimate the dose-response relationship between SUA and fundus arteriosclerosis. Subgroup analysis was performed to find the gender-specific association between SUA and incident fundus arteriosclerosis. In males, after adjusting for confounding factors, the highest SUA level was significantly associated with the risk of incident fundus arteriosclerosis. The OR with 95%CI for Q4 was 1.44(1.18, 1.76), Q1 as a reference. Specially, for females, SUA level was not associated with the incidence of fundus arteriosclerosis. In conclusion, elevated levels of SUA were associated with the incidence of fundus arteriosclerosis in males, but not in females.
Similar content being viewed by others
Introduction
Arteriosclerosis is one of the earliest signs of adverse structural and functional changes within the vessel wall1. Fundus arteriosclerosis is essentially retinopathy and belongs to small arteriosclerosis. Fundus arteriosclerosis has been shown to be a predictor of cardiovascular disease, coronary artery disease, new-onset hypertension, renal and cerebrovascular diseases in various populations2,3,4,5,6. In addition, fundus arteriosclerosis was the only blood vessel lesion that can be observed in vivo through non-invasive surgery7. Studies have suggested that the degree of fundus arteriosclerosis can better predict the extent of coronary artery disease3. Moreover, one study has shown that inflammatory response and endothelial dysfunction were associated with the pathogenesis of retinopathy8.
Serum uric acid (SUA) is the end product of purine metabolism, most of which is excreted in the urine by the kidneys9. Hyperuricemia (HUA) is a well-known cause of gout and is linked with metabolic syndrome10, owing to increased production of SUA coupled with excretion dysfunction. Epidemiological studies have shown that elevated levels of SUA were independent risk factors for cardiovascular events, kidney disease, metabolic syndrome, coronary heart disease, stroke and myocardial infarction11,12,13,14,15,16,17. A few experimental studies have suggested that uric acid may be involved in the formation of arteriosclerosis through multiple pathways. It may be related to arteriosclerosis by regulating important pro-inflammatory pathways18, may be induced by nitric oxide-related endothelial cell proliferation19, and may be stimulated by vascular smooth muscle proliferation20. Although several studies have explored the relationship between uric acid and arteriosclerosis, the results were not consistent21,22,23,24,25,26,27. Recent studies have shown that elevated SUA levels may be associated with a higher risk of increased arteriosclerosis in normotensive subjects22, and SUA could be used as a predictor of atherosclerosis27. In contrast, in a Korea study, SUA levels were not related to arteriosclerosis21. Animal experiment has shown that the administration of allopurinol and benzbromarone prevented the development of atherosclerosis in apoE (−/−) mice fed a uric acid-enriched diet25. Given these discordant results, the association between elevated uric acid and arteriosclerosis remains controversial. In addition, this association has been relatively underexplored in healthy population.
Therefore, we analyzed the relationship between SUA and funds arteriosclerosis in healthy examination population by a retrospective cross-sectional study, and explored whether there was a dose response relationship between them.
Results
Characteristics of study population
Baseline characteristics of participants by quartiles of SUA levels in total populations are shown in Table 1. Table 1 shows that the incidence of fundus arteriosclerosis was 9.3%. We could find that the incidence of fundus arteriosclerosis gradually increases with the increase of SUA levels (p for trend <0.0001). With the increase of SUA level, body mass index (BMI) gradually increased, and the number of smokers and drinkers also gradually increased. In addition, SUA levels were found significantly positive correlation with creatinine, eGFR, TG, TC and LDL. However, higher SUA levels were found to be negatively related to HDL.
Relationship between SUA and the incidence of fundus arteriosclerosis
As what is shown in Table 2, we found that in males the Q4 of SUA levels were independent risk of increasing incident fundus arteriosclerosis after adjustment for age, BMI, smoking, drinking, eGFR, TG, TC, LDL and HDL compared with the first quartile of SUA level. The OR with 95%CI for Q2-Q4 were 0.96(0.79, 1.16) with p = 0.66, 1.09(0.90, 1.32) with p = 0.40, and 1.44(1.18, 1.76) with p = 0.0003, respectively. Trend test was also significant with p = 0.0002. In females, the OR with 95%CI for Q2-Q4 were 0.96(0.69, 1.33) with p = 0.79, 1.03(0.75, 1.42) with p = 0.84, and 1.00(0.73, 1.38) with p = 0.98, respectively. Trend test was not significant with p = 0.85. The association between SUA and incident fundus arteriosclerosis was different in males and females. In total populations, the OR with 95%CI for Q2-Q4 were 1.08(0.89, 1.31) with p = 0.47, 1.03(0.84, 1.26) with p = 0.79, 1.40(1.13, 1.75) with p = 0.0027. p for trend = 0.0010 (Supplementary Table S1).
Figure 1 shows the dose–response relationships between SUA and the risk of incident fundus arteriosclerosis. The association between SUA and the incidence of fundus arteriosclerosis was modeled through multivariable-adjusted spline regression models with four knots, and revealed linear dose-response relationships between uric acid and incident fundus arteriosclerosis in males (p < 0.0001). But there was no significant linear dose-response relationship in females (p = 0.58). There were liner dose-response relationships between SUA and incident fundus arteriosclerosis in total (p < 0.0001) (see Supplementary Fig. S1).
Association of SUA with the incidence of fundus arteriosclerosis according to restricted cubic spline regressions using four knots in males and females (percentiles 5, 35, 65 and 95), with the reference point set at percentile 12.5. (a,b) Odds ratios were adjusted for age, BMI, smoking, drinking, eGFR, TG, TC, LDL and HDL, respectively.
The BMI subgroup analysis for association of SUA with incident fundus arteriosclerosis
We subsequently performed subgroups analysis by major characteristics of the study population. Table 3 shows the analysis of relationship between SUA and incident fundus arteriosclerosis by BMI subgroup analysis in different groups. We could find that after adjustment for age, smoking, drinking, eGFR, TG, TC, LDL and HDL, in male subgroup with BMI ≤ 25 kg/m2, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.15(0.88, 1.50) with p = 0.31, 1.23(0.93, 1.63) with p = 0.15, 1.96(1.45, 2.64) with p < 0.0001, respectively. p for trend < 0.0001. In male subgroup with BMI > 25 kg/m2, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 0.88(0.67, 1.17) with p = 0.39, 1.13(0.86, 1.48) with p = 0.38, 1.52(1.16, 1.98) with p = 0.0020, respectively. p for trend <0.0001. In female subgroup with BMI ≤ 25 kg/m2, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 0.92(0.64, 1.33) with p = 0.66, 0.98(0.68, 1.40) with p = 0.90, 1.23(0.86, 1.76) with p = 0.25, respectively. p for trend = 0.17. In female subgroup with BMI > 25 kg/m2, the OR for incident fundus arteriosclerosis were from the second to the highest SUA quartile were 1.64(0.77, 3.50) with p = 0.20, 1.80(0.90, 3.61) with p = 0.10, 1.32(0.67, 2.59) with p = 0.42, respectively. p for trend = 0.94. As can be seen from the Table 3, in the BMI subgroup analysis, there was a gender difference in the relationship between uric acid and incident fundus arteriosclerosis, which was statistically significant in males and not statistically significant in females. In total subgroup with BMI ≤ 25 kg/m2, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.04(0.83, 1.32) with p = 0.72, 1.26(0.98, 1.63) with p = 0.08, 1.76(1.32, 2.35) with p = 0.0001, respectively. p for trend < 0.0001. In total subgroup with BMI > 25 kg/m2, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.32(0.92, 1.90) with p = 0.14, 1.05(0.73, 1.50) with p = 0.81, 1.67(1.15, 2.41) with p = 0.01, respectively. p for trend = 0.0010 (Supplementary Table S2).
In the BMI subgroup analysis, which revealed liner dose-response relationships between SUA and incident fundus arteriosclerosis in males BMI ≤ 25 kg/m2 and BMI > 25 kg/m2 (p < 0.0001 and p < 0.0001). But there were no linear dose-response relationships in females BMI ≤ 25 kg/m2 and BMI > 25 kg/m2 (p = 0.09 and p = 0.96) (Fig. 2). The BMI subgroup analysis, which revealed liner dose-response relationships between SUA and incident fundus arteriosclerosis in total BMI ≤ 25 kg/m2 and BMI > 25 kg/m2 (p < 0.0001 and p < 0.0001) (see supplementary Fig. S2).
In the BMI subgroups, association of SUA with the incidence of fundus arteriosclerosis according to restricted cubic spline regressions using four knots in males and females (percentiles 5, 35, 65 and 95), with the reference point set at percentile 12.5. (a–d) Odds ratios were adjusted for age, smoking, drinking, eGFR, TG, TC, LDL and HDL, respectively.
The age Subgroup analysis for association of SUA with incident fundus arteriosclerosis
Table 4 shows that relationship between uric acid and incident fundus arteriosclerosis by age subgroup in different groups. We could observe that in male subgroup with age ≤50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.09(0.63, 1.89) with p = 0.75, 0.99(0.57, 1.71) with p = 0.97, 1.41(0.85, 2.36) with p = 0.19, respectively. p for trend = 0.15. In male subgroup with age >50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 0.99(0.82, 1.18) with p = 0.89, 1.15(0.96, 1.37) with p = 0.14, 1.56(1.29, 1.86) with p < 0.0001, respectively. p for trend < 0.0001. In female subgroup with age ≤50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 0.60(0.24, 1.48) with p = 0.26, 0.83(0.37, 1.85) with p = 0.64, 0.53(0.23, 1.24) with p = 0.14, respectively. p for trend = 0.25. In female subgroup with age >50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 0.92(0.66, 1.28) with p = 0.61, 0.92(0.67, 1.26) with p = 0.61, 0.87(0.64, 1.19) with p = 0.39, respectively. p for trend = 0.43. As can be seen from the Table 4, in the age subgroup analysis, there was a gender difference in the relationship between uric acid and incident fundus arteriosclerosis, which was statistically significant in males age >50 years and not statistically significant in females. In total age ≤50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.08(0.62, 1.87) with p = 0.78, 0.99(0.55, 1.78) with p = 0.97, 1.23(0.67, 2.25) with p = 0.51, respectively. p for trend = 0.41. In total age >50 years, the OR for incident fundus arteriosclerosis from the second to the highest SUA quartile were 1.23(1.03, 1.47) with p = 0.02, 1.29(1.07, 1.56) with p = 0.01, 1.80(1.47, 2.21) with p < 0.0001, respectively. p for trend < 0.0001 (Supplementary Table S3).
In the age subgroup analysis, which revealed linear dose-response relationships between uric acid and fundus arteriosclerosis in males age >50 years (p < 0.0001). But there were no linear dose-response relationships in males age ≤50 years and females age ≤50 years and females age >50 years (p = 0.60, p = 0.14 and p = 0.82) (Fig. 3). In the age subgroup analysis, which revealed liner dose-response relationships between uric acid and fundus arteriosclerosis in total age >50 years (p < 0.0001), but there was no linear dose-response relationship in total age ≤50 years (p = 0.89) (see Supplementary Fig. S3).
In the age subgroups, association of SUA with the incidence of fundus arteriosclerosis according to restricted cubic spline regressions using four knots in males and females (percentiles 5, 35, 65 and 95), with the reference point set at percentile 12.5. (a–d) Odds ratios were adjusted for BMI, smoking, drinking, eGFR, TG, TC, LDL and HDL, respectively.
Discussion
The results of this study showed that 9.3% of people without diabetes and hypertension showed signs of fundus arteriosclerosis. In addition, the incidence of fundus arteriosclerosis in males and females were 12.3% and 5.8%, respectively. The incidence of fundus arteriosclerosis was similar to many previous studies and should be of great concern28,29,30,31. In this study, we observed a particularly important result that there was a gender-specific association between serum uric acid and fundus arteriosclerosis, and there was a significant dose-response relationship between higher SUA levels and the incidence of fundus arteriosclerosis.
Fundus arteriosclerosis is a microvascular disease that belongs to arteriosclerosis. To rule out the effects of traditional factors on arteriosclerosis, this study excluded traditional cardiovascular risk factors such as diabetes and hypertensions, and screened for a healthy physical examination. Our study showed that the association between SUA and fundus arteriosclerosis was statistically significant in males without diabetes or hypertension. Chen’s32 study showed that uric acid was positively associated with aortic stiffness in men. Previous studies have shown that uric acid was found to be an independent risk factor for carotid atherosclerosis in men without metabolic syndrome33. When the SUA level was above 5.2 mg/dl, arterial stiffness was increased in healthy Korean men34. Some longitudinal studies have shown that uric acid was a risk factor for arteriosclerosis, the relationship was more pronounced in men35. Shin’s21 and Tomiyama’s36 studies showed an insignificant relationship between uric acid and arterial stiffness in women with normal uric acid level. Recently, a cohort study disclosed a significant independent relationship between increased SUA and increased pulse wave velocity (PWV) over time, this association was restricted to men, and possibly explained by the higher SUA levels in men than in women throughout their lifespan37. Ishizaka, N., et al. confirmed that in both genders, SUA level was associated with arterial stiffness, and was in part independent of other conventional risk factors for atherosclerosis and metabolic syndrome38. However, Yuan, Y., et al. showed that in the Chinese coastal female populations, the association of high SUA and increased arterial stiffness was dependent on the coexistence of at least one cardiovascular risk factor, especially dyslipidemia39.
Some studies also showed that there was a gender-specific association between higher uric acid and coronary artery disease, only statistically different among women40. It should be noted that our results were inconsistent with those of some predecessors, and we concluded that elevated uric acid was associated with fundus arteriosclerosis in males, but not in females. Possible explanations were as follows. First, different subjects were selected, and dietary habits and genes of different populations could also cause differences in the incidence of fundus arteriosclerosis. Secondly, uric acid levels were generally higher in males than in females37. However, this gender difference has often been attributed to the role of estrogen in females to promote uric acid excretion before menopause41 and possibly to impair renal clearance and excess uric acid secretion in male patients, especially in the presence of visceral fat obesity or metabolic syndrome42, the pathophysiology and clinical significance of this finding have not been clearly elucidated40. In addition, the incidence of fundus arteriosclerosis in males was higher than that of females. The mechanisms of gender difference in the effect of uric acid on fundus arteriosclerosis are still unclear, and require further research.
In the subgroup analysis of age >50 years, SUA levels related to Q4 quartile were associated with the incidence of fundus arteriosclerosis in males, but not in females. Recently, studies have shown that with the increase of age, male individuals with higher SUA values had an accelerated increase in PWV, which was not related to major confounding factors such as age, blood pressure, renal function, and metabolic measurement37. A prospective cohort study of adults in northern China aged 40 years and older showed that uric acid was associated with arteriosclerosis, but not in women35. Previous studies have shown that SUA was an independent risk factor for arteriosclerosis in women older than 55 years1, but our studies showed that there were not statistically significant in females. The results of this study are inconsistent with previous results. The mechanism of SUA affecting fundus arteriosclerosis is complex and unclear, so this relationship needs further study.
A recent cross-sectional analysis of adults aged from 30 to 45 showed that the relationship between SUA and early atherosclerosis has been eliminated after BMI adjustment43. A longitudinal study has shown that SUA might be an early biomarker for subclinical atherosclerosis in young adults; starting in early middle age, SUA predicted subclinical atherosclerosis independently of BMI44. This study showed that in males, regardless of the extent of BMI, the highest SUA was associated with the incidence of fundus arteriosclerosis, independent of the effects of BMI, and consistent with previous studies.
Fundus Arteriosclerosis was the result of a complex interaction between the structural and geometric properties of the arterial wall and the dynamic effects of inflation pressure37. There are several aspects can explain the mechanism of uric acid and fundus arteriosclerosis. Uric acid may stimulate the inflammatory pathways18 and promote vascular smooth muscle cells (VSMC) proliferation and oxidative stress by vascular renin-angiotensin system45. In human vascular cells and endothelial cells, SUA has been also found to upregulate c-reactive protein and was directly involved in pro-inflammatory and atherogenic processes46,47, then leads to endothelial cell damage. Uric acid also promotes endothelial dysfunction through inactivation of NO and impairment of endothelial cells proliferation46. Moreover, urate crystals are deposited on the arterial wall, which causes inflammation, stimulates mast cells, induces lipid infiltration, and further destroys the intimal cells of the arteries, thereby blocking the metabolism of apolipoprotein B (apoB) and eventually leading to the aggravation of atherosclerosis27. Uric acid has a dual role, in addition to an oxidative effect, it also has an antioxidant effect48. Although uric acid has a protective effect, elevated uric acid levels are often associated with increased risk of cardiovascular disease and death12. Our study also showed that the association between elevated uric acid and fundus arteriosclerosis was statistically significant. There are two possible reasons that can explain our findings: either uric acid is causing arteriolosclerosis or it is generated to protect against arteriolosclerosis. Our research suggested that there was a relationship between elevated uric acid and fundus arteriosclerosis. However, the relationship between uric acid and fundus arteriosclerosis is unclear, and further research is needed.
It is worth noting that the dose-response relationship between SUA levels and the incidence of fundus arteriosclerosis is seen in males. Although the underlying pathophysiological mechanisms are unclear, excluding interference from traditional risk factors leaving significant deleterious effects in relatively healthy adults. The role of uric acid in atherosclerosis might be related to other cardiovascular risk factors, such as hypertension and metabolic syndrome23. However, some studies have shown that SUA was associated with increased aortic stiffness in Chinese adults and was not associated with conventional cardiovascular risk factors24. This finding was consistent with previous studies, which were associated with increased levels of SUA and were not associated with traditional cardiovascular risk factors24. The results of this study suggested that elevated levels of SUA were associated with the incidence of fundus arteriosclerosis in subjects without diabetes and hypertension, especially in males. Therefore, more attention should be paid to this type of population in health screening. Preventing the incident of fundus arteriosclerosis in advance, on the one hand, preventing visual impairment, on the other hand, it can provide timely and effective basis for clinicians to further assist in the diagnosis of cardiovascular and cerebrovascular diseases.
In this study, we used uric acid quartiles for statistical analysis. At the same time, we included uric acid as a continuous variable in the logistic model analysis, and the results were consistent with those in the article. We found that in males SUA levels were independent risk of increasing incident fundus arteriosclerosis after adjusting for confounding factors, the OR with 95%CI for SUA was 1.002(1.001, 1.003) with p < 0.0001. In females, the OR with 95%CI for SUA was 1.000(0.999, 1.002) with p = 0.59. We could also find that there was a gender specific association between uric acid and fundus arteriosclerosis, which was statistically significant in males, but not in females. (see supplementary Table S4). In the analysis of uric acid as a continuous variable, the OR value of the relationship between uric acid and fundus arteriosclerosis was generally small. In order to research the association between uric acid and fundus arteriosclerosis more deeply, we have used uric acid quartile as the study variable to analyze, and also to be more clearly describe the effect of uric acid increase on fundus arteriosclerosis.
In addition, we used the clinical reference value of uric acid as an independent variable for statistical analysis, and we found that the number of males and females were relatively small (54 and 38 respectively) at the low levels of uric acid. (see supplementary Table S5). The statistical power will be reduced if the number of people was small. Then, we combined the number of people with low and normal levels of uric acid, and uric acid was divided into two categories for statistical analysis (Q1: less than high level; Q2: more than high level) (See Supplementary Table S6). After adjusted for other confounding factors, elevated levels of SUA were associated with the incidence of fundus arteriosclerosis in males, but not in females. This result was consistent with our previous findings. If we take the clinical reference value of uric acid as the study variable, more sample size is needed to confirm the relationship between uric acid and fundus arteriosclerosis.
Moreover, we divided the independent variables into those with or without hyperuricemia by using clinical reference values of hyperuricemia, and conducted a logistics regression analysis. We found that the association between hyperuricemia and fundus arteriosclerosis was statistically significant in males, but not in females. (See Supplementary Table S7). This result was consistent with our previous results. There was a gender difference in the relationship between elevated uric acid and fundus arteriosclerosis, the mechanism of which was not clear, and more research was needed to confirm this.
There were still some limitations in this research. Firstly, this was a retrospective cross-sectional study that did not demonstrate the causal relationship between SUA and fundus arteriosclerosis. Secondly, this study was a retrospective study, some potential factors could not be controlled. Nevertheless, the advantage of our research was that the sample size was large, excluded those with hypertension, diabetes and the total populations, males and females were analyzed separately, which ensured sufficient parameters and accurate results, and drawn a solid conclusion that there was a difference between males and females. Finally, a future prospective study is needed to determine whether the SUA level is an independent predictor of long-term fundus arteriosclerosis outcomes, and whether its reduction could reduce the occurrence of adverse fundus arteriosclerosis events.
Materials and methods
Study population
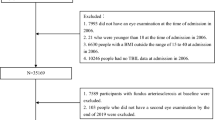
This study analyzed data from Hua Dong Sanatorium. A total of 70,313 non-manual workers underwent health examination in 2018. To avoid confounding factors, subjects with a history of hypertension, diabetes, and those taking medications influencing blood pressure, plasma glucose, lipid profile and uric acid were all excluded. In addition, subjects with blood pressure 140/90 mmHg, fasting plasma glucose≥7.0 mmol/L, haemoglobinA1c (HbA1c) ≥6.5%, and estimated glomerular filtration rate (eGFR) <30 ml/min/1.73 m2 were also excluded. A total of 23474 (12625 males and 10849 females) aged 18–91 years were included in this study. Data clean steps were presented in Fig. 4. This study was approved by the Ethical Committee and the Institutional Review Board of Hua Dong Sanatorium, Wuxi. The informed consent was waived and the need for waiving the informed consent was also supported by the Ethical Committee. All methods were performed in accordance with the Declaration of Helsinki and the relevant guidelines.
Assessment of SUA
SUA levels were determined at the Hua Dong Sanatorium laboratory with Enzymatic methods by AU 5400 BECKMAN COULTER. Total population SUA quartile (Q1–Q4) were ≤274.60, 274.61–339.20, 339.21–410.70, >410.70 μmol/L, respectively. SUA levels were categorized into four groups(Q1–Q4) according to the quartiles of gender-specific distribution: ≤349.30, 349.31–398.90, 398.91–453.40, >453.40 μmol/L for males; ≤237.30, 237.31–275.30, 275.31–316.60, >316.60 μmol/L for females.
Questionnaire data
A standard questionnaire was conducted by trained staff to obtain information about demographic characteristics (age, gender) and lifestyle risk factors such as smoking, drinking. The interview included questions related to the diagnosis and treatment of diabetes, hypertension, cardiovascular events. Smoking habit was categorized as current smoking or nonsmoking (including never smoke or ex-smokers). Drinking was categorized as current drinking or nondrinking (including never drink or ex-drinkers).
Anthropometrics measurement
When measuring height and weight, the population stood upright, wearing a single layer of clothing, without wearing a hat or shoes. Body mass index (BMI) was calculated as weight in kilogram divided by the square of height in meter(kg/m2). Hypertension was defined as blood pressure ≥140/90 mmHg, or a self-reported physician diagnosed with hypertension, or a diagnosis code in the system, or an individual currently using antihypertensive drugs49. Diabetes was defined as fasting glucose level ≥7.0 mmol/L, or a self-reported physician diagnosis of diabetes, or a diagnosis code in the system, or taking oral hypoglycemic medication or insulin50.
Laboratory testing
After fasting for at least 8 hours, blood samples were collected from the anterior cubital vein in the morning. Fasting blood glucose levels were determined by a colorimetry method (AU5400, BECKMAN COULTER). Enzymatic methods were used to measure creatinine, total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL) (AU5400, BECKMAN COULTER), and haemoglobinA1c (HbA1c) was measured with high pressure liquid chromatography (HPLC) by Tosoh Automated Glycohemoglobin Analyzer HLC-723G8. The eGFR was estimated by using the Modification of Diet in Renal Disease (MDRD)-4 equation: eGFR = 186 × serum creatinine−1.154 × age−0.203 × 0.742(in women) × 1.21251.
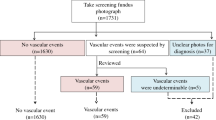
Diagnosis of fundus arteriosclerosis
An eye exam was performed by a trained ophthalmologist. Fundus photography was completed following a standardized Protocol52. Both eyes of each participant were photographed with a 45° digital nonmydriatic camera and were seated in a dark room. The analysis of fundus arteries was conducted with the non-dilated fundus camera TRC.NW400TOPCON. All images were evaluated by trained ophthalmologist.
Subjects were classified with regard to their retinal photography based on the Keith-Wagener-Barker classification53. Grade 1 is defined as retinal artery spasm or mild sclerosis. Grade 2 is defined as moderate to marked sclerosis of the retinal arterioles, arteriovenous intersection can present different degrees of pathological changes, or arteriosclerotic retinopathy or thrombosis of retinal veins. Grade 3 is defined as angiospastic retinopathy, characterized by edema, cotton-wool patches, and hemorrhages in the retina, in addition to marked sclerosis of the retinal arterioles. Grade 4 is defined as measurable edema of the disks in addition to grade 3 pictures54. In the present study, subjects without retinopathy were graded as normal, and subjects with any of the four grades is considered to be fundus arteriosclerosis.
Statistical analyses
All participants were classified according to the quartiles of SUA. The baseline characteristics were compared across the SUA quartiles of the total populations. Baseline characteristics of the participants were reported as medians (quartile intervals) for continuous variables (the continuous variables were not normally distributed) and numbers (percentages) for categorical variables. Kruskal–Wallis tests were employed to compare continuous variables, whereas categorical variables were compared by χ2 trend tests. Univariate and multivariate logistic regression analysis were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for changes in SUA in total populations, males and females.
To detect any possible linear or non-linear dependency in regression models and to allow for flexible interpretation of the relationship between continuous covariates and study outcomes, continuous changes in SUA were assessed through shape-restricted cubic spline regression models with knots at the 5th, 35th, 65th and 95th percentiles, and with the 12.5th percentile as the reference category55.
To examine the consistency of the observed association between SUA and fundus arteriosclerosis, we performed subgroup analyses of participants according to BMI ( ≤ 25, >25 kg/m2), age (≤50, >50 years) in different populations. Statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC, USA). A 2-sided p value < 0.05 was considered to be statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to cooperation unit needs to be confidential, but are available from the corresponding author on reasonable request.
References
Choi, H. Y. et al. Hyperuricemia and risk of increased arterial stiffness in healthy women based on health screening in Korean population. Plos one 12, e0180406, https://doi.org/10.1371/journal.pone.0180406 (2017).
Xie, J. et al. Association of Diabetic Macular Edema and Proliferative Diabetic Retinopathy With Cardiovascular Disease: A Systematic Review and Meta-analysis. JAMA Ophthalmol. 135, 586–593, https://doi.org/10.1001/jamaophthalmol.2017.0988 (2017).
Kim, G. H., Youn, H. J., Kang, S., Choi, Y. S. & Moon, J. I. Relation between grade II hypertensive retinopathy and coronary artery disease in treated essential hypertensives. Clin. Exp. hypertension 32, 469–473, https://doi.org/10.3109/10641963.2010.496515 (2010).
Kario, K., Kanegae, H., Oikawa, T. & Suzuki, K. Hypertension Is Predicted by Both Large and Small Artery Disease. Hypertension 73, 75–83, https://doi.org/10.1161/HYPERTENSIONAHA.118.11800 (2019).
Hsieh, Y.-T., Tsai, M.-J., Tu, S.-T. & Hsieh, M.-C. Association of Abnormal Renal Profiles and Proliferative Diabetic Retinopathy and Diabetic Macular Edema in an Asian Population With Type 2 Diabetes. JAMA Ophthalmol. 136, 68–74, https://doi.org/10.1001/jamaophthalmol.2017.5202 (2018).
Kabedi, N. N., Mwanza, J. C., Lepira, F. B., Kayembe, T. K. & Kayembe, D. L. Hypertensive retinopathy and its association with cardiovascular, renal and cerebrovascular morbidity in Congolese patients. Cardiovasc. J. Afr. 25, 228–232, https://doi.org/10.5830/CVJA-2014-045 (2014).
Cheung, C. Y., Ikram, M. K., Sabanayagam, C. & Wong, T. Y. Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension 60, 1094–1103, https://doi.org/10.1161/hypertensionaha.111.189142 (2012).
van Hecke, M. V. et al. Inflammation and endothelial dysfunction are associated with retinopathy: the Hoorn Study. Diabetologia 48, 1300–1306, https://doi.org/10.1007/s00125-005-1799-y (2005).
Maiuolo, J., Oppedisano, F., Gratteri, S., Muscoli, C. & Mollace, V. Regulation of uric acid metabolism and excretion. Int. J. cardiology 213, 8–14, https://doi.org/10.1016/j.ijcard.2015.08.109 (2016).
Abbasian, M., Ebrahimi, H., Delvarianzadeh, M., Norouzi, P. & Fazli, M. Association between serum uric acid (SUA) levels and metabolic syndrome (MetS) components in personnel of Shahroud University of Medical Sciences. Diabetes Metab. Syndr. 10, 132–136, https://doi.org/10.1016/j.dsx.2016.01.003 (2016).
Chang, C.-C. et al. Association between serum uric acid and cardiovascular risk in nonhypertensive and nondiabetic individuals: The Taiwan I-Lan Longitudinal Aging Study. Sci. Rep. 8, 5234, https://doi.org/10.1038/s41598-018-22997-0 (2018).
Chen, J.-H., Chuang, S.-Y., Chen, H.-J., Yeh, W.-T. & Pan, W.-H. Serum uric acid level as an independent risk factor for all-cause, cardiovascular, and ischemic stroke mortality: a Chinese cohort study. Arthritis Rheum. 61, 225–232, https://doi.org/10.1002/art.24164 (2009).
Leow, M. K. Uric acid and cardiovascular risk. N Engl J Med 360, https://doi.org/10.1056/NEJMc082360 (2009).
Obermayr, R. P. et al. Elevated uric acid increases the risk for kidney disease. J. Am. Soc. Nephrol. 19, 2407–2413, https://doi.org/10.1681/ASN.2008010080 (2008).
Johnson, R. J. et al. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes 62, 3307–3315, https://doi.org/10.2337/db12-1814 (2013).
Battelli, M. G., Bortolotti, M., Polito, L. & Bolognesi, A. The role of xanthine oxidoreductase and uric acid in metabolic syndrome. Biochim. Biophys. Acta Mol. Basis Dis. 1864, 2557–2565, https://doi.org/10.1016/j.bbadis.2018.05.003 (2018).
Bos, M. J., Koudstaal, P. J., Hofman, A., Witteman, J. C. M. & Breteler, M. M. B. Uric acid is a risk factor for myocardial infarction and stroke: the Rotterdam study. Stroke 37, 1503–1507 (2006).
Kanellis, J. et al. Uric acid stimulates monocyte chemoattractant protein-1 production in vascular smooth muscle cells via mitogen-activated protein kinase and cyclooxygenase-2. Hypertension 41, 1287–1293 (2003).
Khosla, U. M. et al. Hyperuricemia induces endothelial dysfunction. Kidney Int. 67, 1739–1742 (2005).
Johnson, R. J. et al. Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension 41, 1183–1190 (2003).
Shin, J. Y., Lee, H. R. & Shim, J. Y. Significance of high-normal serum uric acid level as a risk factor for arterial stiffness in healthy Korean men. Vasc. Med. 17, 37–43, https://doi.org/10.1177/1358863X11434197 (2012).
Nagano, S. et al. Association of serum uric acid with subsequent arterial stiffness and renal function in normotensive subjects. Hypertens. Res. 40, 620–624, https://doi.org/10.1038/hr.2017.10 (2017).
Li, L. X. et al. Serum uric acid levels are associated with hypertension and metabolic syndrome but not atherosclerosis in Chinese inpatients with type 2 diabetes. Journal of hypertension 33, 482–490; discussion 490, https://doi.org/10.1097/hjh.0000000000000417 (2015).
Liang, J. et al. Synergistic effects of serum uric acid and cardiometabolic risk factors on early stage atherosclerosis: the cardiometabolic risk in Chinese study. Plos one 7, e51101, https://doi.org/10.1371/journal.pone.0051101 (2012).
Wakuda, H. et al. Is hyperuricemia a risk factor for arteriosclerosis? Uric acid and arteriosclerosis in apolipoprotein e-deficient mice. Biol. Pharm. Bull. 37, 1866–1871 (2014).
Nieto, F. J., Iribarren, C., Gross, M. D., Comstock, G. W. & Cutler, R. G. Uric acid and serum antioxidant capacity: a reaction to atherosclerosis? Atherosclerosis 148, 131–139 (2000).
Luo, F. & Zhuo, C. Association between uric acid and brachial-ankle pulse wave velocity: secondary analysis of data from a cross-sectional study. Sci. Rep. 10, 2282, https://doi.org/10.1038/s41598-020-59391-8 (2020).
Zhu, Z., Wang, W., Scheetz, J., Zhang, J. & He, M. Prevalence and risk profile of retinopathy in non-diabetic subjects: National Health and Nutrition Examination Survey 2005 to 2008. Clinical & experimental ophthalmology, https://doi.org/10.1111/ceo.13595 (2019).
Kelly, E., Wen, Q., Haddad, D. & O’Banion, J. Effects of an Aging Population and Racial Demographics on Eye Disease Prevalence: Projections for Georgia through 2050. American journal of ophthalmology, https://doi.org/10.1016/j.ajo.2019.10.028 (2019).
Peng, X. Y. et al. Retinopathy in persons without diabetes: the Handan Eye Study. Ophthalmology 117(531–537), 537.e531–532, https://doi.org/10.1016/j.ophtha.2009.07.045 (2010).
Bhargava, M. et al. Prevalence and risk factors for retinopathy in persons without diabetes: the Singapore Indian Eye Study. Acta ophthalmologica 92, e602–609, https://doi.org/10.1111/aos.12446 (2014).
Chen, X. et al. Association of serum uric acid with aortic stiffness and pressure in a Chinese workplace setting. Am. J. Hypertens. 23, 387–392, https://doi.org/10.1038/ajh.2009.277 (2010).
Ishizaka, N., Ishizaka, Y., Toda, E., Nagai, R. & Yamakado, M. Association between serum uric acid, metabolic syndrome, and carotid atherosclerosis in Japanese individuals. Arteriosclerosis, thrombosis, Vasc. Biol. 25, 1038–1044 (2005).
Shin, J. Y., Lee, H. R. & Shim, J. Y. Significance of high-normal serum uric acid level as a risk factor for arterial stiffness in healthy Korean men. Vasc. Med. 17, 37–43, https://doi.org/10.1177/1358863x11434197 (2012).
Song, M. Y. et al. Longitudinal association between serum uric acid levels and multiterritorial atherosclerosis. J. Cell Mol. Med. 23, 4970–4979, https://doi.org/10.1111/jcmm.14337 (2019).
Tomiyama, H. et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement–a survey of 12517 subjects. Atherosclerosis 166, 303–309 (2003).
Canepa, M. et al. Longitudinal Association Between Serum Uric Acid and Arterial Stiffness: Results From the Baltimore Longitudinal Study of Aging. Hypertension 69, 228–235, https://doi.org/10.1161/HYPERTENSIONAHA.116.08114 (2017).
Ishizaka, N. et al. Higher serum uric acid is associated with increased arterial stiffness in Japanese individuals. Atherosclerosis 192, 131–137 (2007).
Yuan, Y., Huang, F., Lin, F., Lin, M. & Zhu, P. Association of High Serum Uric Acid and Increased Arterial Stiffness is Dependent on Cardiovascular Risk Factors in Female Population. Hormone Metab. Res. = Horm. und Stoffwechselforschung = Hormones et. metabolisme 51, 367–374, https://doi.org/10.1055/a-0882-7382 (2019).
Barbieri, L. et al. Impact of sex on uric acid levels and its relationship with the extent of coronary artery disease: A single-centre study. Atherosclerosis 241, 241–248, https://doi.org/10.1016/j.atherosclerosis.2015.03.030 (2015).
Antón, F. M., García Puig, J., Ramos, T., González, P. & Ordás, J. Sex differences in uric acid metabolism in adults: evidence for a lack of influence of estradiol-17 beta (E2) on the renal handling of urate. Metab. Clin. Exp. 35, 343–348 (1986).
Matsuura, F. et al. Effect of visceral fat accumulation on uric acid metabolism in male obese subjects: visceral fat obesity is linked more closely to overproduction of uric acid than subcutaneous fat obesity. Metab. Clin. Exp. 47, 929–933 (1998).
Oikonen, M. et al. Associations between serum uric acid and markers of subclinical atherosclerosis in young adults. The cardiovascular risk in Young Finns study. Atherosclerosis 223, 497–503, https://doi.org/10.1016/j.atherosclerosis.2012.05.036 (2012).
Wang, H. et al. Longitudinal association between serum urate and subclinical atherosclerosis: the Coronary Artery Risk Development in Young Adults (CARDIA) study. J. Intern. Med. 274, 594–609, https://doi.org/10.1111/joim.12120 (2013).
Corry, D. B. et al. Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system. J. hypertension 26, 269–275, https://doi.org/10.1097/HJH.0b013e3282f240bf (2008).
Kang, D. H., Park, S. K., Lee, I. K. & Johnson, R. J. Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J. Am. Soc. Nephrol. 16, 3553–3562, https://doi.org/10.1681/ASN.2005050572 (2005).
Kang, D. H. et al. Uric acid causes vascular smooth muscle cell proliferation by entering cells via a functional urate transporter. Am. J. Nephrol. 25, 425–433, https://doi.org/10.1159/000087713 (2005).
Sautin, Y. Y., Nakagawa, T., Zharikov, S. & Johnson, R. J. Adverse effects of the classic antioxidant uric acid in adipocytes: NADPH oxidase-mediated oxidative/nitrosative stress. Am. J. Physiol., Cell Physiol 293, C584–C596 (2007).
Meng, L., Chen, D., Yang, Y., Zheng, Y. & Hui, R. Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies. J. hypertension 30, 842–851, https://doi.org/10.1097/HJH.0b013e32835080b7 (2012).
Lam, K. B. et al. Napping is associated with increased risk of type 2 diabetes: the Guangzhou Biobank Cohort Study. Sleep 33, 402–407 (2010).
Cirillo, M. Evaluation of glomerular filtration rate and of albuminuria/proteinuria. J. Nephrol. 23, 125–132 (2010).
Klein, R. et al. Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology 113, 373–380, https://doi.org/10.1016/j.ophtha.2005.12.013 (2006).
Keith, N. M., Wagener, H. P. & Barker, N. W. Some different types of essential hypertension: their course and prognosis. Am. J. Med. Sci. 268, 336–345, https://doi.org/10.1097/00000441-197412000-00004 (1974).
Sairenchi, T. et al. Mild retinopathy is a risk factor for cardiovascular mortality in Japanese with and without hypertension: the Ibaraki Prefectural Health Study. Circulation 124, 2502–2511, https://doi.org/10.1161/circulationaha.111.049965 (2011).
Durrleman, S. & Simon, R. Flexible regression models with cubic splines. Stat. Med. 8, 551–561 (1989).
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China (81773541 and 81573253), funds from the Priority Academic Program Development of Jiangsu Higher Education Institutions at Soochow University, the National Key Laboratory of Radiation Medicine and Radiation Protection (GZK1201919) to ZT, National Natural Science Foundation of China (U1967220) to JPC. The funding body did not play any roles in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Q.q. L., C.x. L., Y.h. G., X.y. Z., N.j. Y. and Z.x. T. participated in literature search, study design. Q.q. L., C.x. L., J.p. C., Y.m. W. and Y.b. J. participated in data analysis and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Q., Liu, C., Gao, Y. et al. Gender-Specific Association between Serum Uric Acid and Incident Fundus Arteriosclerosis in Chinese Population: A Retrospective Cross-Sectional Study. Sci Rep 10, 8595 (2020). https://doi.org/10.1038/s41598-020-65575-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-65575-z
This article is cited by
-
Sex-specific association between carotid atherosclerosis and fundus arteriosclerosis in a Chinese population: a retrospective cross-sectional study
European Journal of Medical Research (2023)
-
Association between total bilirubin and gender-specific incidence of fundus arteriosclerosis in a Chinese population: a retrospective cohort study
Scientific Reports (2023)
-
Association between urinary phthalate metabolites and hyperuricemia in US adults
Environmental Science and Pollution Research (2023)
-
Retinal circulation time/arm-to-retina time ratio in the fluorescein angiography to evaluate retina-specific hemodynamics
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.