Abstract
Leptospirosis is caused by pathogenic Leptospira transmitted through contact with contaminated environments. Most mammalian species are infectable by Leptospira but only few act as efficient reservoir being capable of establishing long term kidney colonization and shedding Leptospira in urine. In Madagascar, a large diversity of pathogenic Leptospira display a tight specificity towards their endemic volant or terrestrial mammalian hosts. The basis of this specificity is unknown: it may indicate some genetically determined compatibility between host cells and bacteria or only reflect ecological constraints preventing contacts between specific hosts. In this study, Rattus norvegicus was experimentally infected with either Leptospira interrogans, Leptospira borgpetersenii or Leptospira mayottensis isolated from rats, bats or tenrecs, respectively. Leptospira borgpetersenii and L. mayottensis do not support renal colonization as featured by no shedding of live bacteria in urine and low level and sporadic detection of Leptospira DNA in kidneys. In contrast 2 out of the 7 R. norvegicus challenged with L. interrogans developed renal colonization and intense Leptospira shedding in urine throughout the 3 months of experimental infection. These data suggest that host-Leptospira specificity in this biodiversity hotspot is driven at least in part by genetic determinants likely resulting from long-term co-diversification processes.
Similar content being viewed by others
Introduction
Leptospirosis is a bacterial zoonosis of global importance that is transmitted either by direct contact with infected animals or most commonly by indirect contact through an environment contaminated with the urine shed by infected mammalian reservoirs. Pathogenic Leptospira are highly diversified spirochetes currently composed of ten identified species, namely Leptospira alexanderi, Leptospira alstoni, Leptospira borgpetersenii, Leptospira interrogans, Leptospira kirschneri, Leptospira kmetyi, Leptospira mayottensis, Leptospira noguchii, Leptospira santarosai, and Leptospira weilii1,2. However, the Leptospira diversity is likely overlooked3 and full genome sequencing of environmental samples will surely increase the number of recognized pathogenic species in the next future.
Rodents are considered as important reservoirs of Leptospira, and have hence been investigated in a number of environmental settings4,5,6,7. Molecular typing of Leptospira hosted by rats from Reunion Island and Seychelles have revealed the dominance of a single species, L. interrogans, represented by three Sequence Types (STs), two of them being reported in different locations worldwide4,5. The very limited diversity of these rat-borne leptospires together with cosmopolitan lineage distribution support a recent introduction of L. interrogans in these oceanic islands, possibly concomitant with rat introduction.
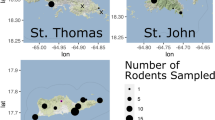
Besides rodents, a wide range of mammals can actually host Leptospira spp. (i.e. support kidney colonization), as confirmed by a thorough investigation of wild mammals from southwestern Indian Ocean (SWIO) islands8. Volant and terrestrial small mammals have been investigated in Madagascar and surrounding islands where bacterial isolation and molecular investigations have uncovered a remarkable diversity of mostly original Leptospira lineages2,9,10,11,12,13,14,15. Contrary to studies that indicate the lack of host specificity and a possible geographic structuring among Leptospira spp.16,17, detailed studies conducted in Madagascar highlighted that Malagasy Leptospira show a marked specificity towards their hosts, as best exemplified by the exploration of tenrec and bat reservoirs12,13. Indeed, each bat considered at the family or genus level in Madagascar shed Leptospira belonging to lineages that have co-diversified with their hosts, lineages which can hence be considered as endemic to Madagascar13. Similarly, L. mayottensis, a leptospiral species of public health concern on Mayotte island2,10,15, is found only in Tenrecidae in Mayotte and Madagascar12,15, suggesting a strong affinity of L. mayottensis for this mammalian family. Host specificity patterns have also been reported in other African environmental setups. In Benin, L. kirschneri is associated with shrews while L. interrogans may be found in several host species although mainly in Rattus norvegicus18. In Tanzania, unique lineages of L. borgpetersenii, different from references sequences, are found in cattle, while L. kirschneri can be found in several ruminant species9.
Noteworthily, rats in Mayotte, an introduced species, are infected with a handful of Leptospira species, suggesting that rats can be a reservoir of a wider diversity of Leptospira than endemic mammals13. However, the ability of rats to harbor endemic Leptospira lineages is not so clear. Thus, in 2016, a study conducted in Mayotte did not report L. mayottensis renal colonization in any of the 289 screened rats. However in Madagascar, this species was identified in a small percentage of infected Rattus through the development of a sophisticated screening strategy allowing the investigation of multiple infections19. Of note, L. mayottensis was found in Rattus as co-infections only. Authors claimed that rats may have acquired L. mayottensis infection through direct or indirect contact with tenrecs. These observations question the role of rats in the transmission of endemic strains of Leptospira in humans on SWIO islands and the ability of strains, likely host-specific, to be sheltered by introduced reservoirs such as rats. Beside these observations, endemic Leptospira seem to exhibit a strong specificity towards their hosts that may result from ecological drivers such as the absence of contact between endemic and introduced mammal hosts impeding trans-contamination of rats by endemic Leptospira. Alternatively, co-evolutionary processes taking place during the extraordinary radiation of tenrecs, rodents and bats in Madagascar during the last 20–30My20,21 may have led to specific host-parasite interactions driving strong host specificity13.
Rattus norvegicus is a well-known reservoir of Leptospira, including in SWIO, and has been proven as a good experimental model to study chronic infection22,23,24. To bring a first insight on the mechanisms responsible for the host specificity observed on the field, we tested whether isolates of L. borgpetersenii and L. mayottensis, obtained from bat and tenrec specimen, respectively, and considered endemic to SWIO, are able to replicate in a genetically different host such as R. norvegicus. An isolate of L. interrogans harboring a worldwide distributed ST and obtained from a rat from Reunion Island was used as a positive control.
Materials and methods
Animal experiments and ethical statement
Seven- to eight-week-old female Wistar rats (Janvier Labs, Le Genest, France) were housed by 4 in enriched cages at the CYROI platform’s animal facility. The appropriate number of animals was calculated using the Resource Equation method25. Experiments were conducted following the guidelines of the Office Laboratory of Animal Care at the CYROI platform. All animal procedures were performed in accordance with the European Union legislation for the protection of animals used for scientific purposes (Directive 2010/63/EU) and approved by the French Ministry of Sciences and Superior Education under the number APAFIS#8773–2016111615105111 v2.
Bacterial isolates
Leptospira were isolated from kidneys of field-trapped volant and terrestrial small mammals. Leptospira interrogans was isolated from Rattus rattus on Reunion Island (2013RR GLM983)5, L. mayottensis was isolated from Tenrec ecaudatus on Mayotte (2014TE MDI222)15, and L. borgpetersenii was isolated from an insectivorous bat, Triaenops menamena, endemic to Madagascar (2014TM FMNH228863)26. All isolates were genotyped through Multi Locus Sequence Typing (scheme 3). Of note, the used L. interrogans isolate has been previously genotyped as Sequence Type 02 (ST02, MLST scheme#3), an ST that is widespread in both R. rattus and R. norvegicus on Indian ocean islands such as Seychelles and Reunion4,5. The L. interrogans and L. mayottensis isolates were selected for being associated with acute leptospirosis human cases on Reunion Island and Mayotte, respectively. The L. borgpetersenii isolate exhibited an original ST that has never been identified in any human leptospirosis case. Although characterized as L. borgpetersenii, it is important to mention that Leptospira shed by Malagasy bats have very unique genetic profiles and display strong host-specificity: these lineages form monophyletic clades composed of lineages shed by bats belonging to the same genus13. All Leptospira isolates were grown in Ellinghausen-McCullough-Johnson-Harris (EMJH) liquid medium (Difco, Detroit, MI, USA) supplemented with albumin fatty acid supplement (AFAS) (purchased at AO/OIE and National Collaborating Centre for Reference and Research on Leptospirosis Academic Medical Center, Department of Medical Microbiology, Amsterdam) and 5-fluorouracil (5-Fu) at 28 °C (for detailed protocol, see http://dx.doi.org/10.17504/protocols.io.ifccbiw). The isolates were stored at −80 °C or in liquid nitrogen for three to four years and their virulence was restored by two serial passages in hamsters, then stored at −80 °C and passaged less than 5 times before the start of the experiments27. The virulence of the three isolates has been tested on hamsters in a previous study in our lab and revealed a higher virulence of L. interrogans compared to the two other strains27.
Infection and sample collection
Challenged rats were inoculated intraperitoneally (i.p.) with 1.5 × 108 bacteria of L. interrogans (n = 7 animals), L. mayottensis (n = 8) or L. borgpetersenii (n = 7) resuspended in 500 µl sterile phosphate buffered saline (PBS) 1×. This inoculated bacterial load was chosen following a pilot study because it induced live Leptospira interrogans excretion in the urine of rats after four weeks post-infection. Although i.p. inoculation is not a natural route of infection, this method is acknowledged as the most convenient method to inject a reproducible volume of inoculum28. Control rats (n = 8) were injected i.p. with 500 µl sterile PBS 1X. Animals were monitored for three months and urine samples were collected once a week during the whole experiment. After three months, animals were anesthetized with 50 mg/kg pentobarbital injected i.p. and subsequently euthanized by cardiac puncture. The animals were then transcardially perfused with PBS 1X to flush out the blood. The kidneys were then collected and processed for further experiments or immediately frozen at −80 °C.
Bacterial load measurement
A piece of up to 25 mg of frozen kidney was lyzed in ATL buffer (Qiagen, Germany) for 3 hours minimum. DNA from frozen kidneys and from urine samples (30 to 100 µl) was extracted using DNeasy Blood & Tissue Kit (Qiagen, Germany). The DNA of pathogenic Leptospira was quantified in each sample by a probe-specific real-time PCR using Quantinova probe PCR mix (Qiagen, Germany). All samples were triplicated and samples with at least two replicates leading to a PCR amplification at Ct <45 were considered positive. Results are expressed as genome copies per milligram of tissue for kidney samples or as genome copies per microliter for urine samples. The genome size of L. interrogans strain Fiocruz L1–130 was used to calculate the number of genome copies29.
Viability of excreted leptospires
2 ml of EMJH liquid medium supplemented with AFAS and 5-Fu were inoculated with 30 to 50 µl urine. Cultures were observed regularly for three months to check the presence of cultivable leptospires under a dark-field microscope (Axio Lab.A1, Zeiss France).
Histological studies
For each animal, a whole kidney was fixed in 4% paraformaldehyde for 24 to 48 hours. Kidneys were then serially dehydrated using a spin tissue processor STP120 (Myr, Spain) as follows: three baths of Ottix Shaper at room temperature (10 minutes, 1 hour and 1.5 hours) were followed by 6 baths of Ottix Plus at room temperature (1 hour, 1.5 hour twice, 2 hours and 2.5 hours), and 2 paraffin baths at 62 °C (1.5 hour and 2.5 hours). Kidney tissues were then embedded in paraffin. Four- to six-µm-thick paraffin kidney sections were deparaffinized in three successive xylene baths, 10 minutes each, rehydrated in 3 successive ethanol baths (100%, 70% and 50%, 2 minutes each) and in distilled water bath, 2 minutes each. Rehydrated sections were eventually stained with hematoxylin and eosin, and observed using a digital slide scanner (NanoZoomer S60, Hamamatsu, France). Altogether, a minimum of three distinct animals were examined for each Leptospira infection and control.
Analysis of Leptospira DNA detection in urine
Regarding DNA detection in urine, two approaches were implemented to cope with particularities observed in the sampled dataset: a high number of urine samples without any detected copy of Lesptospira genome, leading to zero-inflation in the distribution of the number of detected copies (Y = 0, where Y is the number of copies detected in one urine sample), and strong variability across tested rats, indicative of inter-individual effects. Hence, we first analyzed the overall load measured over the study period, that is the total number of genome copies (Ytot) for differences in variance and mean across groups. Means were compared in a simple ANOVA after log-transformation in the latter case to improve the normality of the distribution (log(Ytot + 1)). Residuals were checked for normality and variance homogeneity. Second, we built a linear mixed model to account for the different experimental variables that are strain and rat identity as well as time after infection (WPI: week post-infection), while taking advantage of the full variability of the sampled dataset. A Gaussian model of the transformed unitary response (log(Y + 1)) was constructed while accounting for zero-inflation in the distribution. Leptospira strain identity and WPI were used as fixed-effects variables while rat identity nested within strain was used as a random-effect variable in both the conditional and the zero-inflated components of the model. The final model was defined and validated after model comparison with varying structure of the fixed and random effects and for residual normality and homogeneity.
Results
Experimentally infected rats show no clinical signs
After i.p. inoculation of Leptospira, none of the challenged rats showed any clinical sign of disease during the whole experiment and all animals survived after three months. A non-parametric Kruskal-Wallis test was performed to compare the mean body weight percentage. The weight gain of challenged rats was not significantly distinct from that of the control rat group at the end of the experiment (from 37.93% to 41.70% of increase, H = 0.25, df = 3, p-value = 0.9, Fig. 1).
Differential Leptospira urinary shedding from rats
Leptospira shedding in the urine of experimentally infected rats was addressed through culture and DNA detection on urine samples collected every week throughout the 3 months experiment. Overall, 286 urines samples excreted by 22 monitored rats could be analyzed. As shown in Table 1, no leptospires grew in culture medium inoculated with urine from any of the L. mayottensis- and L. borgpetersenii-infected rats. By contrast, live leptospires could be observed in culture medium inoculated with urine from 2 out of 7 L. interrogans-infected rats, starting from 4 weeks post-infection and until the end of the experiment. The shedding of Leptospira appeared intermittent as no cultivable leptospires could be detected at weeks 8 and 10 after infection.
Leptospira DNA was detected in the urine of all L. interrogans infected rats, although discontinuously and with distinct concentration (Table 1, Fig. 2). Leptospira DNA was detected in urine samples during 10 and 12 consecutive weeks for 2 out of 7 L. interrogans-infected rats, with amounts ranging from 7,303.0 to 94,599.8 genome copies/µl. Urine samples of 1 additional rat tested positive during the first 3 weeks of the experiment. On the other hand, the detection of Leptospira DNA in the 4 remaining rats was sporadic and ranged from 230.2 to 100,746.5 genome copies/µl.
Leptospira DNA was detected less often and at lower levels in the urine of rats infected with L. mayottensis and L. borgpetersenii in comparison to individuals infected with L. interrogans. Leptospira DNA was sporadically detected in the urine of all L. mayottensis-infected rats with amounts ranging from 168.4 to 34,816.1 genome copies/µl.
Six out of seven L. borgpetersenii-infected rats shed Leptospira DNA in their urine. The detection was continuous in the first three weeks of the experiment for 2 rats and sporadic for the 4 remaining rats. Continuous DNA excretion ranged from 132.9 to 11,625.2 genome copies/µl while sporadic excretion ranged from 19.9 to 4,323.3 genome copies/µl.
Statistical analyses of the total number of copies detected for each rat over the study course revealed significant differences in the variability of Leptospira detection across strains (Bartlett’s test on Ytot: n = 22, K2 = 48.922, df = 2, p < 10−10). Hence, total individual Leptospira load varied across strains indicating significant variability across individual rats. A simple linear regression of the log-transformed total numbers revealed a weak effect of strain identity on the response (ANOVA: SS = 37.92, F21,2 = 2.673, p = 0.095).
The analysis based on linear mixed modeling of the (log-transformed) number of copies, Y, allowed us to account for significant zero-inflation in the data (229 cases without detection out of 286) as well as inter-individual variability. Four individual observations (out of 286), corresponding to zero values in the 2 rats showing high excretion of L. interrogans showed extreme values of response residuals. We present here the results after these observations were removed from analysis to improve the validity of the model, but we checked that the conclusions drawn from statistical inference did not depend on those observations. The final model retained was of the following form: Y ~ WPI + strain + (1 | strain / rat) for the conditional component, where WPI stands for week post-infection, strain indicates the strain and rat identity, and ~ (1 | strain / rat) for the zero-inflation component. Both random effects, in the conditional and in the zero-inflation components, improved the model, indicating significant variability across rats within strain groups with rats showing no or very weak excretion (Supplementary Table), as explained in the first part of the section. Regarding fixed effects, time after infection and strain identity showed both significant effects (ANOVA-II: WPI: Χ2 = 4.513, df = 1, p = 0.0336, strain: Χ2 = 8.705, df = 2, p = 0.013), negative for WPI (slope = −0.115, s.e. = 0.055) and with a significant positive coefficient for L. interrogans only (1.927, s.e. = 0.736, using contrasts by treatment with L. borgpetersenii as reference, vs 0.221, s.e. = 0.742 for L. mayottensis). No significant interaction was detected between WPI and strain.
Leptospira spp. experimental infection does not necessarily induce chronic renal carriage and histological damage
Following euthanasia, kidneys were screened by qPCR for Leptospira DNA. The test was negative for all rats infected with either L. borgpetersenii or L. mayottensis. Only those two rats chronically infected with L. interrogans, as shown by qPCR on urine, tested positive with loads of 108,670.8 ± 8178.1 and 201,132.3 ± 1077.7 copies/mg of kidney tissue. The kidneys from rats experimentally infected with all three Leptospira species were histologically studied using hematoxylin-eosin staining. Kidney sections showed no particular renal damage induced by the infection of rats with any of the three Leptospira isolates, including the two rats that were chronically shedding L. interrogans. Glomeruli and renal tubules of infected rats harbored the same phenotype as the control rats (Fig. 3).
Discussion
In this study, we tested the ability of Leptospira isolates obtained from bats (L. borgpetersenii) and tenrecs (L. mayottensis), two reservoirs endemic to SWIO islands, to replicate in a genetically different host via i.p. inoculation of these isolates in rats, a well-known Leptospira reservoir of L. interrogans worldwide including on several SWIO islands4,5,6,15.
As expected, our data indicate that rats do not develop any symptom of disease after inoculation of either of the three Leptospira species used in this study. However, they differed in their ability to develop an asymptomatic chronic renal carriage and Leptospira shedding in urine. This feature characterized only rats infected by the rat-borne L. interrogans cosmopolitan isolate but none of the rats infected by the tenrec-borne L. mayottensis and the bat-borne L. borgpetersenii isolates. Indeed, Leptospira DNA was detected during 10 to 12 consecutive weeks in the urine of two out of seven L. interrogans-infected rats while more sporadically and for not more than 3 consecutive weeks in rats infected with either L. mayottensis or L. borgpetersenii. Moreover, live leptospires could grow in cultures of urine samples obtained from the two aforementioned L. interrogans-infected rats during several consecutive weeks, whereas urine samples obtained from L. mayottensis- and L. borgpetersenii-infected rats did not lead to any detectable growth of Leptospira. When controlling for inter-individual variability, which includes the absence of shedding in some rats, the injected Leptospira isolate was retained in the final linear mixed model. In addition, strain identity shows a significant effect when analyzing fixed effect, with a significant positive coefficient found for L. interrogans only. Of note, the two rats harboring chronic infection with L. interrogans were housed in the same cage with 2 other rats seemingly not chronically infected with Leptospira. The two chronically infected rats shed bacteria with comparable kinetics throughout the experiment. Hence direct or indirect horizontal contamination was likely not involved in renal colonization in our experiment.
No particular lesion was observed in the kidneys of any rat following infection, which is not unexpected as rats are resistant to Leptospira infection30,31. Indeed, previous studies have already reported the absence of renal lesions in rats experimentally infected by L. interrogans30,32, although such rats can also harbor nephritis and cellular infiltrates23,24.
One should note that in our study, the rate of renal colonization induced in rats by L. interrogans isolate was lower (2 out 7 rats) than previously reported in comparable experiments also carried out using Wistar rats22,24,33. In addition, the kinetics of shedding (4–5 weeks for detection of live bacteria) was slower than reported in these previous studies (only one week despite lower bacterial inoculums) (Athanazio et al., 2008). These results might reflect a lower virulence of the L. interrogans used in our study. Similarly, one may consider that the inability of L. borgpetersenii and L mayottensis recovered from endemic hosts to colonize rats’ kidneys may also reflect an attenuated virulence of these isolates. In a previous study27, we have shown that the L. interrogans isolate, the same than the one used in the present study, was (i) significantly more virulent than L. mayottensis and L. borgpetersenii isolates and (ii) able to colonize kidneys after experimental infection of the highly sensitive hamsters more efficiently than did the Leptospira isolates recovered from endemic hosts.
An alternative explanation of our observations is that the absence of renal colonization in rats by the endemic strains could result from some natural incompatibility possibly genetically determined between the bacterium and this alternative vertebrate host: the L. mayottensis and L. borgpetersenii isolates may not be able to adhere to cells of the host kidney tubules of rats and hamsters and organize bacterial biofilms27,34. Noteworthily, L. mayottensis has been recently detected in rats from Madagascar but mostly as co-infections with L. interrogans19. Hence, a primary infection in rats with L. interrogans may be a prerequisite for a secondary infection with L. mayottensis. In other words, L. mayottensis may be able to form a mixed biofilm with L. interrogans, but unable to form a mono species biofilm. This could be tested experimentally by inoculating L. mayottensis into rats that are already chronically shedding L. interrogans, or by injecting a mixture of L. interrogans and L. mayottensis.
Studies on Friend virus virulence evolution have shown that viral fitness could be impaired by several passages of the virus through hosts of different genotypes. By contrast, several passages of the pathogen through hosts of identical genotypes led to an increase in pathogen fitness35. Thus, the Leptospira isolates obtained from bat and tenrec specimens may have a decreased fitness in rats, hence impairing chronic infection in this species. Further investigations are needed to test whether serial passages of a specific Leptospira lineage through a novel animal target (such as rats) can allow its adaptation to this alternative host.
In conclusion, Leptospira isolates obtained from small volant and terrestrial mammals endemic to western Indian Ocean were not experimentally able to colonize rats’ kidneys, in keeping with the host specificity observed in natural conditions8,15. Our results suggest that the strong host specificity of Leptospira species/lineages endemic to SWIO islands towards their mammalian hosts8 is at least in part related to host genetics. These data certainly do not rule out the existence of ecological factors. Indeed, frequent inter-species physical contacts such as those reported between two bat species, namely Myotis goudoti and Miniopterus spp., have been proposed to facilitate Leptospira host switches13,36. However, presented data support the existence of genetic determinants involved in host-Leptospira specificity. Symmetrical experiments, i.e. challenging bats and tenrecs with all three isolates, would bring further relevant information although such experiments require accessing to lab colonies of bats and tenrecs, which are very few worldwide. Other biological characteristics of the Leptospira isolates may also account for our results such as attenuated virulence;27 low growth rate of Leptospira may also hamper L. mayottensis and L. borgpetersenii from chronically infecting mammalian host other than their natural reservoir. Further experiments are needed to solve this issue and unravel factors that may be at play in such interactions.
References
Adler, B. Leptospira and Leptospirosis. Curr. Top. Microbiol. Immunol. 387, 1–293 (2015).
Bourhy, P., Collet, L., Brisse, S. & Picardeau, M. Leptospira mayottensis sp. nov., a pathogenic species of the genus Leptospira isolated from humans. Int. J. Syst. Evol. Microbiol. 64, 4061–4067 (2014).
Thibeaux, R. et al. Deciphering the unexplored Leptospira diversity from soils uncovers genomic evolution to virulence. Microb. Genomics 4, (2018).
Biscornet, L. et al. Human leptospirosis in Seychelles: A prospective study confirms the heavy burden of the disease but suggests that rats are not the main reservoir. PLoS Negl. Trop. Dis. 11, e0005831 (2017).
Guernier, V. et al. Human leptospirosis on Reunion Island, Indian Ocean: Are rodents the (only) ones to blame? PLoS Negl. Trop. Dis. 10, e0004733 (2016).
Rahelinirina, S. et al. First isolation and direct evidence for the existence of large small-mammal reservoirs of Leptospira sp. in Madagascar. PLoS One 5, e14111 (2010).
Cosson, J. F. et al. Epidemiology of Leptospira transmitted by rodents in Southeast Asia. PLoS Negl. Trop. Dis. 8, e2902 (2014).
Dietrich, M. et al. Biogeography of Leptospira in wild animal communities inhabiting the insular ecosystem of the western Indian Ocean islands and neighboring Africa. Emerg. Microbes Infect. 7, (2018).
Allan, K. J. et al. Assessment of animal hosts of pathogenic Leptospira in northern Tanzania. PLoS Negl. Trop. Dis. 12, e0006444 (2018).
Bourhy, P. et al. Isolation and characterization of new Leptospira genotypes from patients in Mayotte (Indian Ocean). PLoS Negl. Trop. Dis. 4, e724 (2010).
Bourhy, P. et al. Human Leptospira isolates circulating in Mayotte (Indian Ocean) have unique serological and molecular features. J. Clin. Microbiol. 50, 307–311 (2012).
Dietrich, M. et al. Diversification of an emerging pathogen in a biodiversity hotspot: Leptospira in endemic small mammals of Madagascar. Mol. Ecol. 23, 2783–2796 (2014).
Gomard, Y. et al. Malagasy bats shelter a considerable genetic diversity of pathogenic Leptospira suggesting notable host-specificity patterns. FEMS Microbiol. Ecol. 92, fiw037 (2016).
Lagadec, E. et al. Pathogenic Leptospira spp. in bats, Madagascar and Union of the Comoros. Emerg. Infect. Dis. 18, 1696–1698 (2012).
Lagadec, E. et al. Identification of Tenrec ecaudatus, a wild mammal introduced to Mayotte Island, as a reservoir of the newly identified human pathogenic Leptospira mayottensis. PLoS Negl. Trop. Dis. 10, e0004933 (2016).
Ballados-González, G. G. et al. Detection of pathogenic Leptospira species associated with phyllostomid bats (Mammalia: Chiroptera) from Veracruz, Mexico. Transbound. Emerg. Dis. 65, 773–781 (2018).
Lei, B. R. & Olival, K. J. Contrasting patterns in mammal–bacteria coevolution: Bartonella and Leptospira in bats and rodents. PLoS Negl. Trop. Dis. 8, e2738 (2014).
Houéménou et al. Pathogenic Leptospira in commensal small mammals from the extensively urbanized coastal Benin. Urban Sci. 3, 99 (2019).
Moseley, M. et al. Mixed Leptospira infections in a diverse reservoir host community, Madagascar, 2013–2015. Emerg. Infect. Dis. 24, 1138–1140 (2018).
Poux, C., Madsen, O., Glos, J., De Jong, W. W. & Vences, M. Molecular phylogeny and divergence times of Malagasy tenrecs: Influence of data partitioning and taxon sampling on dating analyses. BMC Evol. Biol. 8, 102 (2008).
Samonds, K. E. et al. Imperfect isolation: factors and filters shaping Madagascar’s extant vertebrate fauna. PLoS One 8, e62086 (2013).
Athanazio, D. A. et al. Rattus norvegicus as a model for persistent renal colonization by pathogenic Leptospira interrogans. Acta Trop. 105, 176–180 (2008).
Nally, J. E., Mullen, W., Callanan, J. J., Mischak, H. & Albalat, A. Detection of urinary biomarkers in reservoir hosts of leptospirosis by capillary electrophoresis-mass spectrometry. Proteomics - Clin. Appl. 9, 543–551 (2015).
Tucunduva de Faria, M. et al. Morphological alterations in the kidney of rats with natural and experimental Leptospira infection. J. Comp. Pathol. 137, 231–238 (2007).
Festing, M. F. Design and statistical methods in studies using animal models of development. ILAR J. 47, 5–14 (2006).
Lebarbenchon, C. et al. Astroviruses in bats, Madagascar. Emerg. Microbes Infect. 6, e58 (2017).
Cordonin, C. et al. Three Leptospira strains from western Indian Ocean wildlife show highly distinct virulence phenotypes through hamster experimental infection. Front. Microbiol. (2019).
Haake, D. A. Hamster model of leptospirosis. Curr. Protoc. Microbiol. Chapter 12, Unit12E.2 (2006).
Nascimento, A. L. T. O. et al. Comparative genomics of two Leptospira interrogans serovars reveals novel insights into physiology and pathogenesis. J. Bacteriol. 186, 2164–2172 (2004).
Nally, J. E., Wilson-Welder, J. H., Hornsby, R. L., Palmer, M. V. & Alt, D. P. Inbred rats as a model to study persistent renal leptospirosis and associated cellular immune responsiveness. Front. Cell. Infect. Microbiol. 8, 66 (2018).
Bonilla-Santiago, R. & Nally, J. E. Rat model of chronic leptospirosis. Curr. Protoc. Microbiol. 1–8 (2011). https://doi.org/10.1002/9780471729259.mc12e03s20
Nally, J. E., Chow, E., Fishbein, M. C., Blanco, D. R. & Lovett, M. A. Changes in lipopolysaccharide O antigen distinguish acute versus chronic Leptospira interrogans infections. Infect. Immun. 73, 3251–3260 (2005).
Zilber, A. L. et al. Comparison of mucosal, subcutaneous and intraperitoneal routes of rat Leptospira infection. PLoS Negl. Trop. Dis. 10, e0004569 (2016).
Baumler, A. & Fang, F. C. Host specificity of bacterial pathogens. Cold Spring Harb. Perspect. Med. 3, a010041 (2013).
Kubinak, J. L., Cornwall, D. H., Hasenkrug, K. J., Adler, F. R. & Potts, W. K. Serial infection of diverse host (Mus) genotypes rapidly impedes pathogen fitness and virulence. Proc. R. Soc. B Biol. Sci. 282, 20141568 (2014).
Goodman, S. M. Les chauves-souris de Madagascar. (2011).
Acknowledgements
The study received funding from FEDER INTERREG V program ECOSPIR (GURDTI/20170789-6875). Colette Cordonin’s thesis was financed by the French Ministry of Superior Education and Research. Some of the data presented herein is part of the thesis manuscript accessible through the library of the University of La Réunion (http://www.theses.fr/2019LARE0002). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: C.C., K.D., P.T., M.R., P.M. Performed the experiments: C.C., M.R., P.T., M.T., M.B. Contributed resources/reagents/materials/analysis tools: C.C., P.T., P.M., M.R., M.B., J.B., O.F. Wrote the paper: C.C. Revised the paper: all co-authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cordonin, C., Turpin, M., Bringart, M. et al. Pathogenic Leptospira and their animal reservoirs: testing host specificity through experimental infection. Sci Rep 10, 7239 (2020). https://doi.org/10.1038/s41598-020-64172-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64172-4
This article is cited by
-
Identifying Leptospira interrogans putative virulence factors with a yeast protein expression screen
Applied Microbiology and Biotechnology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.