Abstract
Recent studies have investigated whether the human histo-blood group antigen (HBGAs) could affect the effectiveness of the oral rotavirus vaccines, suggesting secretor positive individuals develop a more robust response. We investigated the Rotavirus A (RVA) shedding in association with the host susceptibility profile in children from a birth community-cohort in Rio de Janeiro, Brazil, from 2014 to 2018. A total of 132 children were followed-up between 0 to 11-month-old, stool samples were collected before/after the 1st/2nd RV1 vaccination doses and saliva samples were collected during the study. RVA shedding was screened by RT-qPCR and G/P genotypes determined by multiplex RT-PCR and/or Sanger nucleotide sequencing. The sequencing indicated an F167L amino acid change in the RV1 VP8* P[8] in 20.5% of shedding follow-ups and these mutant subpopulations were quantified by pyrosequencing. The HBGA/secretor status was determined and 80.3% of the children were secretors. Twenty-one FUT2 gene SNPs were identified and two new mutations were observed. The mutant F167L RV1 VP8* P[8] was detected significantly more in Le (a+b+) secretors (90.5%) compared to non-secretors and even to secretors Le (a−b+) (9.5%). The study highlights the probable association between RV1 shedding and HBGAs as a marker for evaluating vaccine strain host susceptibility.
Similar content being viewed by others
Introduction
After implementation of the rotavirus vaccines, Rotarix® (RV1, GlaxoSmithKline Biologicals, Rixensart, Belgium) and RotaTeq® (RV5, Merck Inc., USA), in over 100 countries worldwide1, the burden of severe group A rotaviruses (RVA) diarrhea has decreased substantially, with reductions in hospitalizations and deaths in many countries, including Brazil2,3,4,5,6. However, RVA still are one of major causes of severe viral diarrhea in infants and young children <5-years-old worldwide6,7. Due to the zoonotic potential, variability of the RVA strains and host genetic factors, the surveillance of circulating RVA strains is necessary for evaluating and monitoring the effectiveness of the implemented immunization programs, mainly in low-income countries8. Currently, 36 G- and 51 P- genotypes have been described9 and globally, six G/P combinations are the most prevalent in humans: G1P[8], G2P[4], G3P[8], G9P[8], G4P[8] and G12P[8]10.
Studies involving the histo-blood group antigens (HBGA) have shown the importance of the VP8* domain (subunit of the VP4 protein of RVA); in the early stages of the pathogenesis of RVA infection11,12,13 as well as identifying RV1 G1P[8] shedding by nucleotide sequencing14,15.
HBGAs are complex glycans (type 1 H, Lea, Leb) present on cell surfaces and in biological fluids, such as blood, breast milk, saliva, and intestinal mucosa16. These glycans are catalyzed by glycosyltransferases, through sequential addition of monossaccharides to an initial precursor; these transferases are encoded by the AB0, FUT2 (Secretor) and FUT3 (Lewis) genes17. Secretor status is a host susceptibility factor in several infectious diseases, such as viral gastroenteritis by some RVA and noroviruses genotypes, and gastritis-ulcers by H. pylori18.
The HBGAs are highly polymorphic and differ across populations worldwide17,19. The epistatic interaction between FUT2 (Se) and FUT3 (Le) genes determines the Lewis phenotype20 and, principally, missense mutations in these genes interfere with the level of expression and activity of the α(1,2)-fucosyltransferase and α(1,3/1,4)-fucosyltransferase enzymes, determining ‘non-secretor’ and ‘Lewis negative’ Le (a−b−) phenotypes, respectively21,22,23. The HBGA genes’ mutations distributed worldwide as single nucleotide polymorphisms (SNPs) work as identity markers favoring certain conditions of susceptibility or resistance to infections or disorders.
In most studies on interaction between HBGAs and RVAs, the P[4] and P[8] VP8* genotypes preferentially infect the secretor and/or (Leb) individuals24; while non-secretor individuals (Lea) were less susceptible to these genotypes25,26,27. Recent studies have investigated whether the HBGA profile could contribute to the effectiveness of oral RVA vaccines28,29,30,31,32,33, suggesting secretor positive individuals develop a more robust response28,29,30.
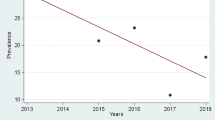
This prospective study aimed to follow newborns up to <1-year of age in a low-income community-cohort in Manguinhos, Rio de Janeiro, Brazil, vaccinated with RV1 between November 2014 and November 2018, in order to assess the G1P[8] vaccine shedding in association to HBGA profile.
Results
Sampling of the children from Manguinhos community, Rio de Janeiro
The 132 children were followed for 16,212 child-days, ranging from 7–285 days, with 79% monitored up to at least 90 days. A total of 569 stool samples were collected and a median of five samples were obtained per child (no less than two samples/per child) and 132 saliva samples were obtained (1 sample/per child). Gender distribution was 50.8% (67) male and 49.2% (65) female.
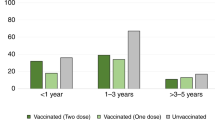
Rotavirus A shedding
A total of 19.2% (109/569) of stool specimens were positive for RVA by one-step reverse transcription-quantitative polymerase chain reaction (RT-qPCR), corresponding to 62.1% (82/132) of all children enrolled in this prospective study. By age range analysis, the highest RVA detection rate (39.3%, 92/234) was observed in children aged between 2 and 5 months (vaccination period) (Table 1). RVA acute diarrheic episodes (ADE) and non-ADE cases corresponded to 26.8% (11/41) and 18.5% (98/528) of stool samples respectively, and the G1P[8] was the most prevalent genotype (88.1%, 96/109). The G12P[8] (1.8%, 2/109), G3P[8] (0.9%, 1/109), and G3P[9] (0.9%, 1/109) genotypes were also detected. Four samples (3.7%) were G- not typed (G[NT]P[8]) and five samples (4.6%) were G- and P-not typed (G[NT]P[NT]).
Through nucleotide analysis of the VP8* gene by sanger sequencing, the G1P[8] strains were characterized as RV1 G1P[8] shedding in 88.5% of stool samples (85/96), with a range of 99.6–100% and 99.5–100% for nucleotide (nt) and amino acid (aa) similarity with RV1, respectively. Additionally, 33% (28/85) of the samples characterized as RV1-sourced G1P[8] were confirmed by Sanger sequencing of the VP7 (G1) and NSP4 genes presenting >99% of similarity (data not showed).
The RV1 G1P[8] in the analyzed strain was detected before the 1st dose (3 non-vaccinated cases) and from day 1 to day 58 (median of 7 days) post-vaccination (1st dose: 59 stool samples; 2nd dose: 23 stool samples), with the Ct value (RT-qPCR) varying from 19.6 to 40 (median Ct value 35.6, range from 1.6 × 100 to 2.4 × 105 genome copies/mL).
ADE was detected in two RV1 vaccinated children, one 2 and one 6-month-old (1st and 2nd doses, respectively), and in Sanger sequencing of the VP8* gene from both children’s stool samples, RV1 G1P[8] shedding was detected. The RV1 G1P[8] recovered from the 2-month-old child’s stool presented a VP8* P[8] mutation.
In relation to the other non-G1P[8] genotypes detected in this cohort in acute diarrheic episodes (ADE), the G3P[9] genotype was observed 11 days after the 1st dose of RV1 (RT-qPCR Ct value of 19) and G3P[8] was detected in one 6 month-old child (RT-qPCR Ct value of 32.5). The G12P[8] genotype was detected in one 4-month-old child (7 days after the RV1 2nd dose, RT-qPCR Ct value of 39.1) and one 10-month-old child (RT-qPCR Ct value of 36.4).
Detection of VP8* P[8] gene mutation
The F167L VP8* gene mutation in the RV1 G1P[8] characterized strains (F167L RV1 VP8* P[8]) was detected in 20.5% (27/132) of children monitored with shedding and was present in 23 children after the 1st dose, 2 children after the 2nd dose, 1 child before the 1st dose (persisting after the 1st dose, and 1 child before the 1st vaccine dose; see Supplementary Table S1). The F167L RV1 VP8* P[8] was detected from day 5 to day 31 (median of 8 days, except for 2 cases detected before the 1st dose), with a median RT-qPCR Ct value of 32.9. The RV1 G1P[8] shedding period (days post-vaccination) for children releasing these particles either with or without the F167L mutation was similar (median of 7 and 8 days).
Nucleotide analysis of the RV1 VP8* P[8] shedding by sanger sequencing showed a mutation at nt 499 T > C (1st position of the codon, T/CTT) in 26 samples (30.6%, 26/85), besides the mutation at nt 501 T > A (3rd position of the codon, T/CTA/T) in 2 samples (2.4%, 2/85), both positions resulting in the altered aa in position 167 in the VP4 protein (phenylalanine - Phe, substituted by leucine - Leu) (Table 2). Results obtained from pyrosequencing showed an allelic quantification of C/T for the 1st position and T/A for the 3rd position of the T/CTA/T codon, demonstrating a mixture of virus subpopulations containing Phe (TTT) and Leu (CTT, TTA or CTA) aa in RV1 G1P[8] characterized shedding. The stool samples varied from 1 to 95.5% (TTT) and 4.5% to 99% (CTT) in the 1st position (see Supplementary Fig. S1 and Table 1), 14 to 4% (CTA) and 86 to 96% (CTT), and 68 to 89% (TTA) and 32 to 11% (TTT) in the 3rd position. Besides that, two other aa substitutions were detected in the F167L RV1 VP8* P[8] shedding (in two stool samples): one (Y80H) in a conserved region and the other (N87S) in a hypervariable region (antigenic site 8–4). Furthermore, one silent mutation was detected in the nt position 219 A > G (aa 73 T), in other sample.
HBGA phenotyping and FUT2 genotyping
Regarding the secretor status, 80.3% (106/132) of the children were classified as secretors and 15.9% (21/132) were non-secretors. Secretor status definition for 3.8% (5/132) of children was inconclusive. The Lewis phenotypes detected were: 59.8% (79/132) Le (a+b+), 15.9% (21/132) Le (a − b − ), 13.6% (18/132) Le (a − b + ), and 10.6% (14/132) Le (a+b−).
FUT2 genotyping was performed for 78 children with Le (a+b+) secretor and 21 with non-secretor status. Twenty-one SNPs were determined in 82.1% (64/78) of the Le (a+b+) secretor children and 17.9% (14/78) of them did not present any SNP. Twenty-eight genotypes were identified in Le (a+b+) secretors children (see Supplementary Table S2) and the most frequent genotype was Se 171A>G, 216C>T, 357T>C, 428G>A, 739G>A, 960A>G, 1009A>G, 1011T>C (35.9%, 28/78). The rs281377 SNP (357 C > T) was detected in high frequency (80.7%, 63/78) and two new mutations were detected in the Le (a+b+) secretor phenotype (107 T > A and 257 C > T). Twelve SNPs were detected at a low frequency: rs1800021 (40 A > G), rs138507381 (212 T > C), rs200157007 (302 C > T), rs28362836 (315 C > A), rs1800026 (375 A > G), rs1800027 (480 C > T), rs1800025 (481 G > A), rs148371614 (544 G > A), rs142741127 (771 G > A), rs141630650 (855 A > C), rs916106939 (880 T > C), and rs144809245 (969 C > T). The rs1047781 SNP (385 A > T) was not detected in any children phenotyped as Le (a+b+) in this cohort. Twelve (58.3%, 14/21)
children classified as non-secretor presented the following homozygous genotype: se 171A>G, 216C>T, 357T>C, 428G>A, 739G>A, 960A>G, 1009A>G, 1011T>C (see Supplementary Table S3). In addition, one non-secretor child presented a new mutation (257 C > A) and the SNPs rs28362836 (315 C > T), rs138954645 (542 C > T), rs148371614 (544 G > A) and rs142741127 (771 G > A) were identified at a low frequency in three children, and were considered heterozygous at these positions (see Supplementary Table S3). One non-secretor child did not present any SNP in the FUT2 gene.
Rotavirus A shedding and host susceptibility
Six genotypes in the FUT2 gene were identified in 69.6% (16/23) of the Le (a+b+) secretor children with F167L RV1 VP8* P[8] shedding, and rs281377 (357 C > T) was present in 100% (16/16) of them. F167L RV1 VP8* P[8] shedding was more commonly detected in children with secretor status (p = 0.0433), and a Le (a+b+) phenotype (p = 0.0354) (Tables 3 and 4).
Other RVA genotypes isolated in ADE in this cohort were detected in the secretor children, these being G12P[8] in Le (a−b+) and Le (a+b+) and G3P[8] in Le (a+b+). The G3P[9] RVA was isolated from a child both Le (a−b−) and positive for fucose detection. A P[8] genotype, untypable for G[NT], was detected in three Le (a+b+) secretor children and in one secretor Le (a−b+) child. Untypable (G[NT]P[NT]) RVA cases were detected in Le (a+b+) secretors (four children) and in one non-secretor Le (a+b−) child.
Discussion
This prospective study focused mainly on assessing the RVA shedding in association to the HBGA profile in a birth community-cohort in Rio de Janeiro, Brazil. Through monitoring the RV1 G1P[8] shedding, it was possible to detect the F167L RV1 VP8* P[8] from stool samples of children from prior to the 1st dose and during the RV1 immunization period. The evaluation of these children’s host susceptibility profile showed that secretor as well as Lewis b positive children were significantly more likely to shed RV1 G1P[8] with occurrence of the F167L VP8* mutation.
Via VP8* P[8] Sanger sequencing, 88.5% of the G1P[8] RVA detected were identified as RV1, mainly after the 1st dose (96.5%), at 2 months of age, similar to previously documented in clinical trials34,35,36. The G1P[8] genotype was detected in eight non-vaccinated children (before the 1st dose) and due to the low viral load, only three cases could be sequenced and determined as RV1 G1P[8]. Despite the VP8* P[8] Sanger sequencing having been used to differ between RV1 and non-RV1 shedding14,15, we should strictly consider the possibility of the RV1 G1P[8] shedding here characterized containing a RVA constellation differing from the source RV1. Therefore, this study shows the importance of characterizing the RV1 via the RVA constellation method before a vaccine batch can be used to produce RV1 doses.
The horizontal transmission of vaccine viruses has been previously demonstrated between vaccinated and unvaccinated infants or other close contacts35,36. RV1 G1P[8] shedding was reported in two diarrhea cases after the 1st dose, with the F167L mutation being detected in one of them. In this study we observed a low diarrhea incidence, mainly in the first 4 months of age, which could be related to RV1 protection and the effect of exclusive breastfeeding (and transferred maternal antibodies) in these first months of life37.
In the few diarrhea cases detected in this study, a rare G3P[9] was identified in one 2-month-old child after the 1st dose, with the VP8* P[9] gene exhibiting 97% nucleotide similarity to an AU-1-like Brazilian strain (KJ820906) collected from an inpatient 2-year-old, indicating a possible feline/canine-to-human interspecies transmission38. The effectiveness of the RVA vaccines against genogroups 1 and 2 (Wa-like and DS-1-like strains, respectively) has been proven, but still remains unclear against the genogroup 3 (AU-1-like)39,40. As to this rare genotype detected in Manguinhos, further studies are being conducted to determine the complete genomic constellation.
Through our molecular characterization of the RV1 G1P[8] shedding, it was possible to observe a high frequency of the mutation in the 167 position of the VP8* P[8] gene. In our study, only the VP8* domain was analyzed because it is directly related to interactions with HBGAs. In the previous studies with the G1P1A[8] rotavirus vaccine candidate 89‐12, the precursor to RV1, Ward et al.41 identified five aa changes in the VP4 gene (G51D and L167F in VP8* domain; D331Y, D385Y and N695I in VP5* domain) that occurred during vaccine attenuation. It was proposed that these alterations could reduce cross neutralizing antibody responses. Indeed, according to Gozalbo-Rovira et al.42, the 167 position is placed at the bottom of the sugar-binding pocket, and Phe residue contained in RV1 G1P[8] could influence the interaction between the vaccine strain and the sugar of the cellular receptor, due to hydrophobic residue decreasing the binding affinity. 32.9% of the RV1 G1P[8] shedding samples detected in this birth-cohort presented the mutation in the 167 position, with a mixture of virus subpopulations of both amino acids, Leu (CTT, TTA, CTA) and Phe (TTT), in different percentages. We could hypothesize that this suggest an initial process of reversion of attenuation or a selective pressure, through the one and/or two alteration(s) in this codon (positions nt 499, 501), favoring the highest amount of circulation of strains containing the Leu residue, which has a greater avidity for the HBGA’s binding site in the secretor profile. Zeller et al.43 also reported the mutation in position 167 in the 3rd position of the codon (nt 501), in one vaccine derived strain (BE00048) detected in Belgium, in 2009.
Positive secretor status was the most prevalent (80.3%) in this community-cohort, and the Le (a+b+) profile (59.8%) frequency was similar to that observed in younger children from the Amazon (58.8%) as presented in our previous study44. The rs1047781 (385 A > T) SNP, responsible for the weak genotype in the Asian population, was not detected in Le (a+b+) children in the Manguinhos community, Rio de Janeiro state. The rs281377 (357 C > T), a synonymous mutation, was the most frequent SNP detected in this Le (a+b+) secretor profile, and this SNP has been detected in the Brazilian population44,45. According to Ferrer-Admetlla et al.19, the rs281377 (357 C > T) SNP has been detected in a worldwide distribution profile in the natural population, and the se357/385 haplotype is frequently detected in the Asian population. We could explain the high frequency of the Le (a+b+) phenotype detected in children in Rio de Janeiro, Brazil under an evolutionary view that, at some point in the molecular clock, the se357/385 haplotype had diverged and separated from the rs1047781 (385 A > T) SNP. However, epistatic interactions between rs281377 (357 C > T) and other SNPs could affect the expression of the FUT2 gene. The failure in detecting the rs1047781 (385 A > T) SNP, which has been attributed as responsible for the weak secretor phenotype detected in Le (a+b+), in the children in the Manguinhos community in the state of Rio de Janeiro could be explained by the presence of new SNPs in conjunction with rs281377 (357 C > T). Further studies encompassing larger populations, including Le (a − b + ) secretors will be needed to evaluate whether particular SNPs in FUT2 gene can explain the phenotypes Le (a+b+) vs Le (a − b + ) (or similar).
Our study identified SNPs in the FUT2 gene in children from the Manguinhos community, in Rio de Janeiro as rs1800021 (40 A > G), rs48703160 (171 A > G), rs681343 (216 C > T), rs281377 (357 T > C), rs601338 (428 G > A), rs602662 (739 G > A) and rs485186 (960 A > G), also reported by Vicentini et al.45 in children from a Quilombola community (black population, slave descendants) in Espírito Santo (borders with the state of Rio de Janeiro, both states in Southeastern Brazil).
The Brazilian population has a high ethnical diversity and through this study in the Manguinhos children community-cohort, it was possible identify two new mutations: 107 T > A and 257 C > T/A and other SNPs, at a low frequency, not yet reported in Brazil: rs138507381 (212 T > C), rs200157007 (302 C > T), rs28362836 (315 C > A/T), rs1800026 (375 A > G), rs1800025 (481 G > A), rs138954645 (542 C > T), rs148371614 (544 G > A), rs142741127 (771 G > A), rs141630650 (855 A > C), rs916106939 (880 T > C), and rs144809245 (969 C > T).
Le (a+b+) phenotype is very common in infants and children under 2 years-old, usually being a transient status in most children46. In the infancy period, the Lewis phenotypes have not yet fully matured47, due to the activity of the fucosyltransferases (FUT2 and FUT3 genes) not yet reaching the normal levels (enzyme activity of Le > Se)20.
In relation to the non-secretor phenotype, a unique child (0Le (a−b−)) did not present any SNP in the FUT2 gene, i.e., not showing the nonfunctional allele se428 (rs601338)21. This child shed the RV1 G1P[8] strain virus in both doses (6 days post-1st dose; 7 days post-2nd dose); however, only in the 2nd dose was the F167L mutation detected, with mixed virus subpopulations of 63.5% Phe/36.5% Leu. Possibly, other genetic factors could be related to this profile and vaccinal response.
The P[9] RVA genotype interacts with A-type HBGA antigen48, and the AB0 enzyme assay was performed in a saliva sample from the unique child that was infected with this genotype (G3P[9]) in this cohort, presenting positivity for type A antigen (ALe (a−b−) secretor) (data not shown), thus in line with the proposed susceptibility of A to genotype P[9].
The Manguinhos cohort showed a high prevalence of secretors, being a common profile in Latin America30,31,44,45,49. In this study, we were able to investigate RVA shedding and a common mutation was identified in many samples characterized as RV1 according to VP8* Sanger sequencing criteria. This mutational event suggests that the vaccine could be replicating and therefore a more robust immune response may be produced in these infants. In summary, our study demonstrated that Le (a+b+) secretors can influence vaccine replication.
This study highlights the detection of the new mutations in the FUT2 gene detected in the community of Manguinhos, Rio de Janeiro, Brazil and the association between vaccine strain shedding and HBGAs as a marker for evaluating vaccine efficiency. The results in this study indicate the importance of the full molecular monitoring of the RV1 vaccine virus stool shedding, mainly if the F167L VP8* mutation is frequent in other populations, and how the host susceptibility profile can influence this viral selective pressure, besides the questions about circulation and fluctuations of the emergent RVA genotypes and ensuring vaccine efficacy in a post-RVA vaccine era.
Material and methods
Study design, clinical specimens and Ethics Statement
This is a prospective cohort study that aims to perform acute gastroenteritis surveillance in the Manguinhos community, Rio de Janeiro, Brazil, which has one of the lowest Human Development Indexes (HDI) of the municipality50. This project has been approved by the Ethics Committee of the Evandro Chagas National Institute of Infectious Diseases (CEP 688.566/14). Written informed consent was obtained from each child’s parent or legal guardian. The RV1 vaccine was the one received by all vaccinated newborn infants enrolled in this study (2-dose series at ages 2 and 4 months and with a minimum interval between doses of 4 weeks). The vaccination card of each child was verified. A vaccination inquiry was performed at Germano Sinval Faria Health Center (GSFHC) by a pediatrician who accompanied this study, questioning each child’s parent or guardians as to vaccination for RVA (double-checking).
A flow diagram including the participants and the specific steps of methods applied in this study are presented in Supplementary Fig. S2. All clinical specimens were sent to the Regional Rotavirus Reference Laboratory/Laboratory of Comparative and Environmental Virology (RRRL-LCEV) and kept at −20 °C, until the moment of processing and further analysis. The methods were performed in accordance with guidelines and regulations.
RNA extraction from fecal specimens and viral RVA detection
Viral RNA was extracted from clarified stool specimens (10–20% w/v) using an automatic RNA extraction procedure according to the manufacturer’s instructions (QIAcube® Automated System and QIAamp® Viral RNA Mini kit; Qiagen, CA, USA). RVA detection was performed using RT-qPCR on an Applied Biosystems® 7500 Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) as previously described51. The RVA RT-qPCR result was considered positive if the cycle threshold (Ct) value was ≤ 40.
G- and P- RVA genotyping
Semi-nested multiplex reverse transcription-polymerase chain reaction (RT-PCR) was performed for G- and P- RVA genotyping using SuperScript® III One-Step RT-PCR System with Platinum® Taq DNA Polymerase High Fidelity (Invitrogen) and 9con1L/VP7deg (VP7) and 4con3/4con2 (VP8*) primers to generate 904-base-pair (bp) and 876-bp fragments, respectively. These amplicons were used as a template in a second round of amplification with genotype-specific primers as described on WHO/IVB/08.1752. In parallel with the amplicons obtained from child stool samples, the batch named RV1 vaccine identified as GlaxoSmithKline Biologicals Rixensart – Belgium, Human Rotavirus Live Attenuated RIX4414 strain – 1 dose, AROLB385A - Fab: February/2015 – Expiration date: January/2017, was used for RNA extraction and VP8* gene amplification using the same 4con3/4con2 (VP8*) primers cited above.
VP8* RVA molecular characterization
Products of one-step reverse transcription-polymerase chain reaction (RT-PCR) using 4con3/4con2 (876-pb) were purified using Wizard® SV Gel and a PCR Clean-Up System kit (Promega, Madison, USA) following the manufacturer’s instructions. The purified amplicons of the VP8* gene of RVA were analyzed by Sanger sequencing using a BigDye® Terminator v3.1 Cycle Sequencing Kit and the ABI Prism 3730 or 3500 Genetic Analyser® (Applied Biosystems, Foster City, CA, USA). Chromatograms were analyzed and nt sequences (consensus) were edited using the BioEdit 7.2.1 Sequence Alignment Editor53 and nt similarity was assessed using the Basic Local Alignment Search Tool (https://blast.ncbi.nlm.nih.gov/Blast.cgi). RVA genotypes were assigned using the RotaC2.0 automated genotyping tool for Group A rotaviruses (https://rotac.regatools.be/)54. Deduced aa sequences of VP8* (G1P[8]) were aligned and compared with the RV1 (JX943612), RV1 vaccine and G1P[8] Wa-like (JX406750) strains, and nt and aa similarities values between RV1 and G1P[8] strains were verified using the BioEdit 7.2.1 Sequence Alignment Editor53. The representative gene sequences of VP8* RVA obtained in the current study were submitted to GenBank under the accession numbers MN366044-MN366074. Pyrosequencing for mutation analysis of RV1 VP8* P[8] shedding A pyrosequencing assay was performed using PyroMark Q96 ID (QIAGEN Valencia, CA, USA). The following primers were designed to amplify a 203-bp fragment of the VP8* P[8] subdomain containing the target (cytosine or thymine/nt 499, and adenine or thymine/nt 501): forward (VP8*RV1F) 5′-AGCAATTTAATGTGAGTAACGA-3′ (nt 346–368) and reverse (VP8*RV1R) 5′-BIOTIN-AAATTTGCAGTACTTGAACTGTCA-3′ (nt 548–525) using PyroMark® Assay Design 2.0 software (QIAGEN Valencia, CA, USA). The forward (VP8*RV1-S1) (5′-TGATACCAGACTTGTAGGA-3′; nt 447–465) was designed for the pyrosequencing assay. The biotinylated fragment (203-pb) was amplified using SuperScript® III One-Step RT-PCR System with Platinum® Taq DNA Polymerase (Invitrogen). Initially, the samples were denatured with primers at 97 °C/7 min. Next, the master mix was added in each tube, and incubated under the following thermocycling conditions: cDNA synthesis and pre-denaturation at 50 °C/30 min, denaturation at 94 °C/10 min, then 40 cycles of 94 °C/15 s, 53 °C/30 s and 68 °C/1 min, followed by a final elongation step (68 °C/5 min). Each sample and controls (positive and negative) were tested in duplicate and the quality of the RT-PCR products were checked by agarose gel electrophoresis. Biotinylated amplicons were hybridized to streptavidin-coated beads and purified using the PyroMark Q96 Vacuum Prep Workstation (Qiagen, Valencia, CA, USA) according to the manufacturer’s instructions. Pyrosequencing reactions were performed using the PyroMark Gold Q96 SQA Reagents in the PyroMark Q96 ID (QIAGEN) following the manufacturer’s instructions, and the analysis of the peaks was performed using PyroMark ID software. The allelic quantification results (%) were calculated by the duplicate media. The primers designed for this analysis and thermocycling conditions were previously tested and validated. As a positive control, a fragment of the VP8* P[8] region (encoding aa 7–257) of the RV1 stool shedding was isolated. The fragment without the mutation (nt 499/T) was ligated into the pCR®4-TOPO® vector using the TOPO TA Cloning® Kit for Sequencing (Invitrogen, Life Technologies, UK) and then transformed into competent Escherichia coli Top 10 (Invitrogen, Life Technologies, UK) following the classical methodologies previous described55.
HBGA phenotyping and secretor status in saliva
The saliva samples were collected using sterile cotton-swabs (CHEMBIO®, Medford, NY, USA). Two enzyme immunoassays (EIA) were performed, as described previously44,56, to detect AB0 (H) histo-blood groups and Lewis phenotypes, and specifically define the secretor status of Le (a−b−) saliva samples (using Ulex europaeus lectin).
DNA extraction from saliva and FUT2 genotyping
Genomic DNA recovered from epithelial cells was extracted from each saliva sample collected from children phenotyped as Le (a+b+) secretor and non-secretor Le (a+b−) or Le (a−b−) and were used in the touchdown PCR for the genotyping of SNPs in the FUT2 gene, by Sanger sequencing as previously described44,57.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 8 v.8.2.0 (GraphPad Software, San Diego, CA, USA). Detection of the G1P[8] RVA genotype (RV1 stool shedding) in association with the host susceptibility profile was investigated, when appropriate, through the Chi-square or Fisher’s exact test, with a significance level of 5.0%.
References
ROTA Council. Global introduction status. http://rotacouncil.org/vaccine-introduction/global-introduction-status/ (2019).
do Carmo, G. M. I. et al. Decline in Diarrhea Mortality and Admissions after Routine Childhood Rotavirus Immunization in Brazil: A Time-Series Analysis. PLoS Med. 8, e1001024 (2011).
Desai, R. et al. Reduction in morbidity and mortality from childhood diarrhoeal disease after species A rotavirus vaccine introduction in Latin America: a review. Mem. Inst. Oswaldo Cruz 106, 907–911 (2011).
Lanzieri, T. M. et al. Impact of rotavirus vaccination on childhood deaths from diarrhea in Brazil. Int. J. Infect. Dis. 15, e2016–e210 (2011).
de Oliveira, L. H., Camacho, L. A., Coutinho, E. S., Ruiz-Matus, C. & Leite, J. P. Rotavirus vaccine effectiveness in Latin American and Caribbean countries: A systematic review and meta-analysis. Vaccine 1, A248–254 (2015).
Troeger, C. et al. Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea Among Children Younger Than 5 Years. JAMA Pediatr. 172, 958–965 (2018).
Bányai, K., Estes, M. K., Martella, V. & Parashar, U. D. Viral gastroenteritis. Lancet 392, 175–186 (2018).
Patton, J. T. Rotavirus diversity and evolution in the post-vaccine world. Discov. Med. 13, 85–97 (2012).
Rotavirus Classification Working Group. https://rega.kuleuven.be/cev/viralmetagenomics/virus-classification/rcwg (2018).
Dóró, R. et al. Review of global rotavirus strain prevalence data from six years post vaccine licensure surveillance: Is there evidence of strain selection from vaccine pressure? Infect. Genet. Evol. 28, 446–461 (2014).
Liu, Y. et al. Rotavirus VP8*: phylogeny, host range, and interaction with histo-blood group antigens. J. Virol. 86, 9899–9910 (2012).
Huang, P. et al. Spike protein VP8* of human rotavirus recognizes histo-blood group antigens in a type-specific manner. J. Virol. 86, 4833–4843 (2012).
Sun, X. et al. Binding specificity of P[8] VP8* proteins of rotavirus vaccine strains with histo-blood group antigens. Virology 495, 129–135 (2016).
Mokomane, M. et al. Diversity of Rotavirus Strains Circulating in Botswana before and after introduction of the Monovalent Rotavirus Vaccine. Vaccine 37, 6324–6328 (2019).
Gautam, R. & Bowen, M. D. One-step Quantitative RT-PCR Assays for Detecting, Genotyping and Differentiating Wild-Type Group a Rotaviruses and Vaccine (Rotarix® and RotaTeq®) Strains in Stool Samples. J. Vaccines Vaccin. 7, 341 (2016).
Daniels, G. Human Blood Groups (third ed. Blackwell) (London, 2013).
Marionneau, S. et al. ABH and Lewis histo-blood group antigens, a model for the meaning of oligosaccharide diversity in the face of a changing world. Biochimie 83, 565–573 (2001).
Heggelund, J. E., Varrot, A., Imberty, A. & Krengel, U. Histo-blood group antigens as mediators of infections. Curr. Opin. Struct. Biol. 44, 190–200 (2017).
Ferrer-Admetlla, A. et al. A natural history of FUT2 polymorphism in humans. Mol. Biol. Evol. 26, 1993–2003 (2009).
Henry, S., Oriol, R. & Samuelsson, B. Lewis histo-blood group system and associated secretory phenotypes. Vox Sang. 69, 166–182 (1995).
Kelly, R. J., Rouquier, S., Giorgi, D., Lennon, G. G. & Lowe, J. B. Sequence and expression of a candidate for the human Secretor blood group alpha(1,2)fucosyltransferase gene (FUT2). Homozygosity for an enzyme-inactivating nonsense mutation commonly correlates with the non-secretor phenotype. J. Biol. Chem. 270, 4640–4649 (1995).
Koda, Y., Soejima, M. & Kimura, H. The polymorphisms of fucosyltransferases. Leg. Med. 3, 2–14 (2001).
Le Pendu J. Histo-Blood Group Antigen and Human Milk Oligosaccharides. In: Pickering L. K., Morrow A.L., Ruiz-Palacios G. M., Schanler R.J. (eds.) Protecting Infants through Human Milk. Advances in Experimental Medicine and Biology, vol 554. Springer (Boston, MA, 2004).
Cooling, L. Blood groups in infection and host susceptibility. Clin. Microbiol. Rev. 28, 801–870 (2015).
Kambhampati, A., Payne, D. C., Costantini, V. & Lopman, B. A. Host genetic susceptibility to enteric viruses: a systematic review and metaanalysis. Clin. Infect. Dis. 62, 11–18 (2016).
Sun, X. et al. Rotavirus infection and histo-blood group antigens in the children hospitalized with diarrhoea in China. Clin. Microbiol. Infect. 22, 740.e1–3 (2016).
Yang, T., Hou, J., Huang, Y. & Chen, C. Genetic susceptibility to Rotavirus Gastroenteritis in Taiwanese Children. Sci. Rep. 7, 6412 (2017).
Kazi, A. M. et al. Secretor and salivary ABO blood group antigen status predict rotavirus vaccine take in infants. J. Infect. Dis. 215, 786–789 (2017).
Armah, G. E. et al. Rotavirus vaccine take in infants is associated with secretor status. J. Infect. Dis. 219, 746–749 (2019).
Bucardo, F. et al. Histo-blood group antigens and rotavirus vaccine shedding in Nicaraguan infants. Sci. Rep. 9, 10764 (2019).
Bucardo, F. et al. The Lewis A phenotype is a restriction factor for Rotateq and Rotarix vaccine-take in Nicaraguan children. Sci. Rep. 8, 1502 (2018).
Pollock L., et al. Non-secretor histo-blood group antigen phenotype is associated with reduced risk of clinical rotavirus vaccine failure in Malawian infants. Clin Infect Dis, ciy 1067 (2018).
Lee, B. et al. Histo-Blood Group Antigen Phenotype Determines Susceptibility to Genotype-Specific Rotavirus Infections and Impacts Measures of Rotavirus Vaccine Efficacy. J. Infect. Dis. 217, 1399–1407 (2018).
Phua, K. B. et al. Evaluation of RIX4414, A Live, Attenuated Rotavirus Vaccine, in a Randomized, Double-Blind, Placebo-Controlled Phase 2 Trial Involving 2464 Singaporean Infants. J. Infect. Dis. 192, S6–S16 (2005).
Anderson, E. Rotavirus vaccines: viral shedding and risk of transmission. Lancet Infect. Dis. 8, 642–649 (2008).
Rivera, L. et al. Horizontal transmission of a human rotavirus vaccine strain - A randomized, placebo-controlled study in twins. Vaccine 29, 9508–9513 (2011).
Turin, C. G. & Ochoa, T. J. The Role of Maternal Breast Milk in Preventing Infantile Diarrhea in the Developing World. Curr. Trop. Med. Rep. 1, 97–105 (2014).
Tsugawa, T., Rainwater-Lovett, K. & Tsutsumi, H. Human G3P[9] rotavirus strains possessing an identical genotype constellation to AU-1 isolated at high prevalence in Brazil, 1997-1999. J. Gen. Virol. 96, 590–600 (2015).
Braeckman, T. et al. Effectiveness of rotavirus vaccination in prevention of hospital admissions for rotavirus gastroenteritis among young children in Belgium: case-control study. BMJ 345, e4752 (2012).
Payne, D. C. et al. Effectiveness of pentavalent and monovalent rotavirus vaccines in concurrent use among US children, 5 years of age, 2009-2011. Clin. Infect. Dis. 57, 13–20 (2013).
Ward, R. L. et al. Reductions in Cross-Neutralizing Antibody Responses in Infants after Attenuation of the Human Rotavirus Vaccine Candidate 89-12. J. Infect. Dis. 194, 1729–1736 (2006).
Gozalbo-Rovira, R. et al. Unraveling the role of the secretor antigen in human rotavirus attachment to histo-blood group antigens. PLoS Pathog. 15, e1007865 (2019).
Zeller, M. et al. Comparative analysis of the Rotarix™ vaccine strain and G1P[8] rotaviruses detected before and after vaccine introduction in Belgium. PeerJ 5, e2733 (2017).
Moraes, M. T. B. et al. Phenotyping of Lewis and secretor HBGA from saliva and detection of new FUT2 gene SNPs from young children from the Amazon presenting acute gastroenteritis and respiratory infection. Infect. Genet. Evol. 70, 61–66 (2019).
Vicentini, F. et al. Molecular Characterization of Noroviruses and HBGA from Infected Quilombola Children in Espirito Santo State, Brazil. PLoS ONE 8, e69348 (2013).
Cooling L., Down T. Immunohematology. In McPherson RA, Pincus MR. Henry’s clinical diagnosis and management by laboratory methods (22nd ed. Elsevier Saunders) 674–730 (Philadelphia, PA, 2011).
Molthan, L. Lewis phenotypes of American Caucasians, American Negroes and their children. Vox Sang. 39, 327–330 (1980).
Hu, L. et al. Cell attachment protein VP8* of a human rotavirus specifically interacts with A-type histo-blood group antigen. Nature 485, 256–259 (2012).
Lopman, B. A. et al. Norovirus Infection and Disease in an Ecuadorian Birth Cohort: Association of Certain Norovirus Genotypes With Host FUT2 Secretor Status. J. Infect. Dis. 211, 1813–1821 (2015).
Pedro, R. S. et al. A populational-based birth cohort study in a low-income urban area in Rio de Janeiro, Brazil: implementation and description of the characteristics of the study. Cad. Saúde Pública 35, e00023918 (2019).
Zeng, S. Q. et al. One-step quantitative RT-PCR for the detection of rotavirus in acute gastroenteritis. J. Virol. M. 153, 238–240 (2008).
WHO. Manual of Rotavirus Detection and Characterization Methods, https://apps.who.int/iris/bitstream/handle/10665/70122/WHO_IVB_08.17_eng.pdf?sequence=1&isAllowed=y (2019).
Hall, T. A. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucl. Acids Symp. Ser. 41, 95–98 (1999).
Maes, P., Matthijnssens, J., Rahman, M. & Van Ranst, M. RotaC: a web-based tool for the complete genome classification of group A rotaviruses. BMC Microbiol. 9, 238 (2009).
Sambrook J. & Russel D. W. Molecular Cloning: a laboratory manual. 3 ed. Cold Spring Harbor, NY: CSHL Press (2001).
Nordgren, J. et al. Both Lewis and secretor status mediate susceptibility to rotavirus infections in a rotavirus genotype-dependent manner. Clin. Infect. Dis. 59, 1567–1573 (2014).
Elmgren, A., Börjeson, C., Svensson, L., Rydberg, L. & Larson, G. DNA sequencing and screening for point mutations in the human Lewis (FUT3) gene enables molecular genotyping of the human Lewis blood group system. Vox Sang. 70, 97–103 (1996).
Acknowledgements
We would like to thank the parents and infants who participated in this study. We would like to thank Miriã Alves Gonçalves Trindade for her help with the collection of specimens and clinical data, and Messias da Silva, Sérgio da Silva e Mouta Junior, Alexandre Madi Fialho, Fábio Correia Malta, Yan Cardoso Pimenta and Letícia Campos for the laboratorial support. We would like to thank the staff members of “the FIOCRUZ Institutional Platform for DNA sequencing (PDTIS)” and of “the Quality Control of the Bio-Manguinhos (DEQUA)” for technical support including the batch of rotavirus vaccine (RV1) supplied. Special thanks to Bruno Baroni de Moraes e Souza for the English revision of this manuscript. This study was funded by “The Oswaldo Cruz Institute/Fiocruz/PAEF”, “The Carlos Chagas Filho Foundation for Research Support in the State of Rio de Janeiro” (FAPERJ E-26/202.968/2015) and “The National Council for Scientific and Technological Development” (CNPq 424376/2016-4), “Coordination for the Improvement of Higher Education Personnel -CAPES"- PrInt-Fiocruz-CAPES and “PROGRAMA DE PROFESSOR VISITANTE NO EXTERIOR (88881.337140/2019-01)”. M.P.M. and J.P.G.L. are researchers at the “Scientist from Our State” (CNE/FAPERJ).
Author information
Authors and Affiliations
Contributions
C.P.C., M.P.M., J.P.G.L. and M.T.B.M., proposed the study and designed the experiments. D.C.C. and P.B., designed the clinical study, collected the samples and followed-up on the children. C.P.C., A.J.V., R.M.S.A., F.C.A.M. and J.J.F.B., performed laboratory experiments and analysis. C.P.C., M.P.M., J.P.G.L. and M.T.B.M., interpreted the data and wrote the manuscript. J.N. and L.S., discussed the results and critically reviewed the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cantelli, C.P., Velloso, A.J., Assis, R.M.S.d. et al. Rotavirus A shedding and HBGA host genetic susceptibility in a birth community-cohort, Rio de Janeiro, Brazil, 2014–2018. Sci Rep 10, 6965 (2020). https://doi.org/10.1038/s41598-020-64025-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64025-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.