Abstract
The objective of this review was to compare the efficacy and safety of conservative surgery with or without adjunctive presacral neurectomy (PN) for chronic endometriosis-related pelvic pain. In a systematic review with meta-analysis, randomized or nonrandomized controlled studies of conservative endometriosis surgery with or without adjunctive PN were included. Main outcomes were treatment failure (the proportion of women in which surgery failed to adequately resolve midline pain) and the frequency of operative and postoperative complications. A total of 7 studies with 8 group comparisons (3 randomized) representing 503 women (250 PN; 253 Control) were included. Over 34 months median follow-up, crude rates of treatment failure were 15.0% with PN and 40.9% with Controls (risk ratio = 0.43, 95% CI = 0.30 to 0.60, p < 0.001). The risk of postoperative constipation was higher with PN vs. Controls (12.5% vs. 0%, p = 0.024). No treatment group differences were observed for the risk of operative complications (0.6% vs. 0%, p = 0.498), reoperation (4.1% vs. 3.0%, p = 0.758) or urinary incontinence (5.0% vs. 0%, p = 0.195). Overall, in well-selected patients, conservative surgery with adjunctive PN may provide greater relief from midline pain and a similarly low rate of operative complications relative to conservative surgery alone but may increase the risk of constipation postoperatively. However, results were derived from mainly older and lower quality studies. Since then, surgical techniques to treat endometriosis have been improved and the effect of PN observed in prior studies should be confirmed in future studies in women in whom radical excision of deep infiltrating lesions is obtained.
Similar content being viewed by others
Introduction
Endometriosis affects up to 10% of women of reproductive age and is associated with chronic pelvic pain and dysmenorrhea1. Medical management consisting of nonsteroidal anti-inflammatory drugs or hormone-based therapies are first-line treatments for chronic pelvic pain secondary to endometriosis. Despite providing adequate symptom relief in most patients, some women gain only limited or intermittent benefit from medical treatment2,3. Consequently, conservative surgery may be indicated in women with inadequate symptom resolution with medical therapy and who wish to preserve fertility. Pelvic denervation procedures may be used as an adjunct to surgical excision or ablation of endometrial lesions. Presacral neurectomy (PN) involves complete transection of the presacral nerves innervating the uterus, cervix, and proximal fallopian tubes, which is hypothesized to provide relief of chronic midline pelvic pain. The incremental benefit of adjunctive PN to conservative surgery for endometriosis has been explored in previous systematic reviews, but conclusions were mixed4,5. Since these reviews were published over 10 years ago, a reappraisal of existing evidence is warranted. The purpose of this systematic review with meta-analysis was to compare the efficacy and safety of conservative surgery with or without adjunctive PN for relief of chronic pelvic pain due to endometriosis.
Material and Methods
Data sources and searches
We developed and followed a review protocol that adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)6 and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) public database (CRD42019120488; http://www.crd.york.ac.uk/PROSPERO). We searched Medline, Embase, Cochrane Central Register of Controlled Trials, and the Directory of Open Access Journals, with no date or language restrictions, from inception to December 31, 2018 for randomized and nonrandomized controlled studies of conservative endometriosis surgery with or without adjunctive PN using a combination of diagnosis- and treatment-specific keywords. The syntax for Medline searches is provided in Table 1; the syntax for other databases was similar but adapted as necessary. Reference lists of included papers and relevant meta-analyses were manually searched. We also reviewed reports from abstracts and presentations at major gynecological meetings to reduce the risk of publication bias7.
Study selection
Two independent researchers (LM, DF) reviewed titles and abstracts for possible inclusion in the review. Study selection discrepancies between the reviewers were resolved by consensus. Titles and abstracts were initially screened to exclude review articles, commentaries, letters, case reports, and obvious irrelevant studies. Full texts of the remaining articles were retrieved and reviewed. Main inclusion criteria were controlled study of conservative endometriosis surgery with or without adjunctive PN; otherwise identical treatment and follow-up conditions in each group; and at least one reported outcome. Manuscripts published in non-English journals were rewritten in English by a translation service.
Data extraction
An initial database was developed, pilot-tested, and refined to ensure consistency with outcomes reported in the literature. Data were independently extracted from eligible studies by two researchers (LM, DF). Data extraction discrepancies between the two researchers were resolved by discussion and consensus. The following variables were recorded in standardized data extraction forms: general manuscript information, patient characteristics (age, disease severity, symptom duration), study characteristics (study design, sample size, surgical access technique, follow-up duration), risk of bias using the Newcastle-Ottawa scale8, pain severity, procedural data (procedure time, procedural blood loss, hospital stay), operative complications, and postoperative complications.
Outcomes
The primary endpoint of this systematic review was treatment failure, defined as the proportion of women in which surgery failed to adequately resolve midline pain, evidenced by continuation or recurrence of moderate or severe pain during follow-up. Secondary outcomes were frequency of operative complications, and postoperative complications including constipation, urinary incontinence, and reoperation.
Data analysis
Women treated with conservative surgery and adjunctive PN were compared to those receiving conservative surgery alone (Controls) with the risk ratio (RR) statistic where a RR > 1 indicated higher risk with PN and a RR < 1 indicated lower risk with PN. For each outcome, the pooled estimate and 95% confidence interval (CI) were calculated. Forest plots were used to illustrate individual study findings and pooled meta-analysis results, when applicable. We used the I2 statistic to estimate heterogeneity of outcomes among studies; a value of 0% represents no heterogeneity and larger values represent increasing heterogeneity9. Significant heterogeneity was defined by a Cochran Q test p < 0.1 or I2 > 50%. When significant heterogeneity was identified, a random effects model was planned; otherwise, a fixed effect model was planned10. Publication bias was visually assessed with funnel plots and quantitatively assessed with Harbord’s test11. A priori, we identified several sensitivity analyses of the primary endpoint, including a subgroup analysis comparing outcomes in randomized vs. nonrandomized studies, meta-regression to explore the influence of follow-up duration on outcomes, and a one-study removed analysis in which we iteratively removed one study at a time to determine whether conclusions were significantly influenced by any single study. We also performed a post hoc analysis comparing primary endpoint results with a fixed effect vs a random effects model. P-values were two-sided with a significance level less than 0.05. Analyses were performed using Stata v14.2 (StataCorp LLC) and Comprehensive Meta-analysis v3.3, (Biostat).
Results
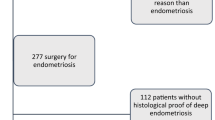
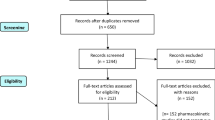
Our initial database search retrieved 145 titles and abstracts; hand searching relevant bibliographies identified 2 additional records. After screening records for inclusion criteria, 40 full-text articles were reviewed for eligibility. Ultimately, 7 studies with 8 group comparisons representing 503 women (250 PN; 253 Control) were included in the meta-analysis. A flow diagram of study identification and selection is shown in Fig. 1.
Women were typically in their early 30 s with moderate or severe (American Fertility Society stage III or IV) endometriosis. Three of eight comparisons were derived from randomly allocated treatment groups, five of eight involved prospective recruitment, and follow-up duration ranged from 13 to 48 months (Table 2). Primary risks of bias among included studies were nonrandomized group assignment and retrospective recruitment. Overall, the risk of bias was high for two comparisons, intermediate for one comparison, and low for five comparisons (Table 3). Additional potential sources of bias related to patient selection criteria, procedural details, and primary outcome definitions are provided in Table 4, which varied considerably among studies.
Procedural data were reported inconsistently and without sufficient detail to warrant meta-analysis. Generally, procedure time was slightly longer (median: 13 minutes; range: 3 to 23 minutes) with PN, blood loss was comparable (range: −4 to 14 cc greater with PN), and hospital stay was comparable (range: 0 to 11 hours shorter with PN).
Among 8 group comparisons, crude rates of treatment failure were 15.0% (35/234) with PN and 40.9% (96/235) with Controls over 34 months median follow-up. Heterogeneity in the treatment failure rate among studies was small to moderate (I2 = 38%, p = 0.130). In fixed effects meta-analysis, the risk of treatment failure was lower with PN vs. Controls (RR = 0.43, 95% CI = 0.30 to 0.60, p < 0.001), representing a 57% risk reduction (Fig. 2). Funnel plot asymmetry was not evident and quantitative assessment did not indicate publication bias (p = 0.078). The treatment benefit of PN was maintained in a subgroup analysis that separately evaluated results among randomized (RR = 0.54, 95% CI = 0.35 to 0.84, p = 0.006) and nonrandomized (RR = 0.29, 95% CI = 0.17 to 0.50, p < 0.001) studies. In meta-regression, the benefit of PN persisted over a 42-month postoperative period. At 1-year follow-up, treatment failure rates were 8.8% with PN and 25.3% with Controls. Thereafter, annualized treatment failure rates were 5.9% per year with PN and 15.5% per year with Controls (p = 0.034) (Fig. 3). Results of the one-study removed analysis suggested that the meta-analysis conclusions were not significantly influenced by any single study. Specifically, the risk of treatment failure remained lower with PN vs. Controls following removal of each study one at a time from the meta-analysis, with the RRs ranging from 0.31 to 0.46 (all p < 0.001). Finally, the risk of treatment failure was comparable when applying a random effects meta-analysis model (RR = 0.37, 95% CI = 0.23 to 0.60, p < 0.001).
Forest plot of the risk of treatment failure comparing conservative surgery with or without presacral neurectomy. The risk ratio and 95% confidence interval are plotted for each study. The pooled risk ratio (diamond apex) and 95% confidence interval (diamond width) is calculated using a fixed effects model. Pooled risk ratio >1 suggests higher risk with presacral neurectomy. Pooled risk ratio <1 suggests lower risk with presacral neurectomy. Fixed effects risk ratio: 0.43 (95% CI: 0.30, 0.60; p < 0.001). I2 = 38%, p = 0.130. PN = presacral neurectomy; CON = Controls.
Meta-regression of the influence of follow-up duration on the risk of treatment failure comparing conservative surgery with or without presacral neurectomy. The risk of treatment failure at 1-year follow-up was 8.8% with conservative surgery and presacral neurectomy (PN) and 25.3% with conservative surgery alone (Control). Thereafter, the annualized risk of treatment failure was 5.9% per year with PN and 15.5% per year with Control (p = 0.034). Plotted values represent the regression line that spans the range of follow-up durations among studies included in the meta-analysis.
Among 6 group comparisons, crude rates of operative complications were 0.6% with PN and 0% with Controls (p = 0.498). In the only study in which an operative complication was reported12,13, a single patient treated with PN experienced significant bleeding from the middle sacral vein that was successfully managed with bipolar electrocauterization. Limited results were available for the remaining complications, which were each reported in only one or two studies. The risk of postoperative constipation was higher with PN vs. Controls (12.5% vs. 0%, p = 0.024). No treatment group differences were observed in the risk of reoperation (4.1% vs. 3.0%, p = 0.758) or urinary incontinence (5.0% vs. 0%, p = 0.195) (Table 5). Each patient with postoperative urinary incontinence was treated with antimuscarinics, which resulted in only slight symptom improvement. Heterogeneity was not observed for any reported complication (all I2 = 0%).
Discussion
Recurrence of pelvic pain is common following conservative surgery for endometriosis14,15, a finding that was confirmed in this systematic review and meta-analysis. We found that adjunctive PN may provide greater relief from endometriosis-related midline pain and a similarly low rate of operative complications compared to conservative surgery alone but may increase the risk of constipation postoperatively.
The main finding of this review was that adjunctive PN reduced the risk of treatment failure relative to conservative surgery alone. This finding was upheld in subgroup and sensitivity analyses and was not influenced by significant heterogeneity or publication bias. A statistically significant reduction in the risk of treatment failure with PN was identified in only 4 of 8 comparisons, which was likely attributable to the small sample sizes of individual studies. After pooling results from all studies, there was a large and consistent treatment benefit attributable to PN such that the number of women needed to treat with PN in order to prevent one treatment failure (i.e. number needed to treat) was 4. That more than 50% of women treated with conservative surgery alone experienced pain recurrence by 3 years underscores the clinical importance of these results.
However, treatment efficacy with PN must be balanced against the possibility of complications. The risk of constipation was higher in women receiving PN (12.5% vs. 0%). Among women reporting constipation, 73% reported symptom resolution with medical treatment, while the remaining 27% reported persistent symptoms, representing 3.4% of all women treated with PN. While these results were only reported in 2 studies12,13,16, the finding of increased constipation risk with PN is in agreement with previous studies17. While urinary incontinence is another known risk of PN, we did not identify statistical differences between groups for this complication. However, this analysis was underpowered to detect clinically meaningful differences between groups since urinary incontinence was reported in only one study12,13. Therefore, while results of this review do not provide evidence that PN increases urinary incontinence risk, this possibility cannot be discounted given the lack of outcome reporting among included studies. Importantly, women with endometriosis often suffer from bowel- and bladder-related symptoms preoperatively and it is unclear whether the data reported here represent pre-existing or new diagnoses. Although the reported intra- and post-operative complication rate was limited, under-reporting cannot be excluded as inconsistent complication reporting is common in the surgical literature18.
It is important to compare the results of the current review with those of prior systematic reviews of PN. In a Cochrane review published in 2005, Proctor and colleagues4 included one randomized trial of conservative surgery with or without adjunctive PN19 in their meta-analysis. They excluded the study of Tjaden et al.20 due to small sample size, and the randomized trial of Zullo et al.12,13 was not yet published. In a 2007 systematic review with meta-analysis, Latthe et al.5 included the same three randomized trials as in the current review, but their analysis evaluated pain at distinct time points, none of which were reported in all three trials. Therefore, the current systematic review is the only report to pool pain data from all randomized trials. Further, we supplemented this evidence with data from five nonrandomized controlled studies. Lastly, we performed subgroup, sensitivity, and meta-regression analyses to explore the robustness of study conclusions and the influence of potential confounders. In this respect, the current research is the most comprehensive and contemporary systematic review on the clinical utility of PN in women with endometriosis.
Despite the benefit of PN observed in this study, it is important to recognize that this is a technically challenging procedure with attendant risks of significant bleeding from the adjacent venous plexus. The surgery must be performed carefully and meticulously in order to prevent injury to major vessels and the right ureter, which delineate the lateral border of the dissection. In the current study, significant operative bleeding was reported in 1 (0.6%) woman treated with PN, with no other reports of operative complications. The single complication, sacral hemorrhage, represents the most common complication of PN17. Surgical experience with PN among surgeons in the included studies was unclear, but it is plausible that the incremental pain reductions and low complication rates with PN in this meta-analysis may have been realized among experienced practitioners. Future studies aimed to quantify the learning curve associated with PN are warranted. It is also important to note that, despite surgeon experience, adjunctive PN may not be appropriate in all women. Appropriate patients are those who report midline pain of at least 6 months duration that is refractory to medical management. Midline pelvic pain is most responsive to uterine denervation procedures21 whereas women with primarily lateral component pain typically show little improvement12,13. Aside from patient selection factors, neuroanatomic variability of the presacral space and failure to completely transect all presacral nerves are potential causes of reduced efficacy. While pre-existing constipation or urinary dysfunction are not absolute contraindications to PN, women with these diagnoses should be carefully informed of the potential for exacerbation of symptoms following surgery. Ultimately, the decision to undergo PN should be made following patient-physician shared decision-making that carefully considers medical history, physician operative experience, complication risk, and future fertility desires.
This meta-analysis has certain limitations pertaining to the quality of studies available for analysis that may influence interpretation. Heterogeneity in study design and surgical techniques was observed, which may confound data interpretation. We were unable to determine the influence of surgical access (laparoscopy vs. laparotomy) in treatment outcomes due to the small number of studies available for analysis. Inclusion of data from nonrandomized studies may have introduced bias into the results. Indeed, most included studies were classified as intermediate or high risk of bias. However, study design differences did not impact overall conclusions since pain relief with PN persisted when analyzing only randomized trials. There was also considerable variation in the completeness of data reported among studies such that only weak conclusions can be derived from outcomes that were reported in few studies. Patient selection criteria and surgeon experience were under-reported and, therefore, generalizability of these results may be limited. Further, the bulk of the results of this review were derived from older studies that utilized laparotomy. Yet, contemporary surgical management of endometriosis-related pain involves laparoscopic techniques that allow a more radical excision of endometriotic lesions with better long-term outcomes. Despite the fact that scientific reports on PN have decreased over the last decade, PN is widely promoted by specialized endometriosis treatment centers as a relatively safe and efficacious adjunct to conservative surgery, a conclusion which is debatable based on numerous factors including surgeon experience and limited evidence derived from studies with unclear generalizability to current practice. It seems there may be a lack of concordance of the role of PN between scientific reports and in clinical practice at specialized centers where PN is aggressively promoted. Given the relative paucity of controlled studies on PN despite its continued use in clinical practice, additional randomized trials and high-quality nonrandomized studies with long-term follow-up are encouraged to better characterize the benefits and harms associated with this procedure.
Conclusion
In well-selected patients, conservative surgery with adjunctive PN may provide greater relief from midline pain and a similarly low rate of operative complications relative to conservative surgery alone but may increase the risk of constipation postoperatively. Main limitations of this review included unclear generalizability of results due to under-reporting of patient selection criteria, surgeon experience, and complications, as well as relatively short follow-up duration in a young patient population. Further, results were derived from mainly older and lower quality studies. Since then, surgical techniques to treat endometriosis have been improved and the effect of PN observed in prior studies should be confirmed in future studies in women in whom radical excision of deep infiltrating lesions is obtained.
Data availability
The underlying data informing this meta-analysis will be made available upon reasonable request.
References
Eskenazi, B. & Warner, M. L. Epidemiology of endometriosis. Obstet Gynecol Clin North Am 24, 235–258 (1997).
Becker, C. M., Gattrell, W. T., Gude, K. & Singh, S. S. Reevaluating response and failure of medical treatment of endometriosis: a systematic review. Fertil Steril 108, 125–136, https://doi.org/10.1016/j.fertnstert.2017.05.004 (2017).
National Institute for Health and Care Excellence. Endometriosis: diagnosis and management, https://www.nice.org.uk/guidance/ng73/evidence/full-guideline-pdf-4550371315 (2017).
Proctor, M. L., Latthe, P. M., Farquhar, C. M., Khan, K. S. & Johnson, N. P. Surgical interruption of pelvic nerve pathways for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev, CD001896, https://doi.org/10.1002/14651858.CD001896.pub2 (2005).
Latthe, P. M., Proctor, M. L., Farquhar, C. M., Johnson, N. & Khan, K. S. Surgical interruption of pelvic nerve pathways in dysmenorrhea: a systematic review of effectiveness. Acta Obstet Gynecol Scand 86, 4–15, https://doi.org/10.1080/00016340600753117 (2007).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151, W65-94, doi:0000605-200908180-00136 (2009).
Cook, D. J. et al. Should unpublished data be included in meta-analyses? Current convictions and controversies. JAMA 269, 2749–2753 (1993).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25, 603–605, https://doi.org/10.1007/s10654-010-9491-z (2010).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560, https://doi.org/10.1136/bmj.327.7414.557 (2003).
Lau, J., Ioannidis, J. P. & Schmid, C. H. Quantitative synthesis in systematic reviews. Ann Intern Med 127, 820–826 (1997).
Harbord, R. M., Egger, M. & Sterne, J. A. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 25, 3443–3457, https://doi.org/10.1002/sim.2380 (2006).
Zullo, F. et al. Effectiveness of presacral neurectomy in women with severe dysmenorrhea caused by endometriosis who were treated with laparoscopic conservative surgery: a 1-year prospective randomized double-blind controlled trial. Am J Obstet Gynecol 189, 5–10 (2003).
Zullo, F. et al. Long-term effectiveness of presacral neurectomy for the treatment of severe dysmenorrhea due to endometriosis. J Am Assoc Gynecol Laparosc 11, 23–28 (2004).
Fedele, L., Bianchi, S., Zanconato, G., Bettoni, G. & Gotsch, F. Long-term follow-up after conservative surgery for rectovaginal endometriosis. Am J Obstet Gynecol 190, 1020–1024, https://doi.org/10.1016/j.ajog.2003.10.698 (2004).
Seo, J. W., Lee, D. Y., Yoon, B. K. & Choi, D. The age-related recurrence of endometrioma after conservative surgery. Eur J Obstet Gynecol Reprod Biol 208, 81–85, https://doi.org/10.1016/j.ejogrb.2016.11.015 (2017).
Liu, K. J. et al. [Effectiveness and safety of laparoscopic presacral neurectomy in treating endometriosis-associated pain]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 33, 485–488 (2011).
Chen, F. P. & Soong, Y. K. The efficacy and complications of laparoscopic presacral neurectomy in pelvic pain. Obstet Gynecol 90, 974–977 (1997).
Martin, R. C. 2nd, Brennan, M. F. & Jaques, D. P. Quality of complication reporting in the surgical literature. Ann Surg 235, 803–813, https://doi.org/10.1097/00000658-200206000-00007 (2002).
Candiani, G. B., Fedele, L., Vercellini, P., Bianchi, S. & Di Nola, G. Presacral neurectomy for the treatment of pelvic pain associated with endometriosis: a controlled study. Am J Obstet Gynecol 167, 100–103 (1992).
Tjaden, B., Schlaff, W. D., Kimball, A. & Rock, J. A. The efficacy of presacral neurectomy for the relief of midline dysmenorrhea. Obstet Gynecol 76, 89–91 (1990).
Gambone, J. C. et al. Consensus statement for the management of chronic pelvic pain and endometriosis: proceedings of an expert-panel consensus process. Fertil Steril 78, 961–972 (2002).
Garcia, C. R. & David, S. S. Pelvic endometriosis: infertility and pelvic pain. Am J Obstet Gynecol 129, 740–747 (1977).
Polan, M. L. & DeCherney, A. Presacral neurectomy for pelvic pain in infertility. Fertil Steril 34, 557–560 (1980).
Puolakka, J., Kauppila, A. & Ronnberg, L. Results in the operative treatment of pelvic endometriosis. Acta Obstet Gynecol Scand 59, 429–431 (1980).
Buttram, V. C. & Reiter, R. C. In Surgical treatment of the infertile female 89-147 (Williams & Wilkins, 1985).
Malinak, L. R. Operative management of pelvic pain. Clin Obstet Gynecol 23, 191–200 (1980).
Rock, J. & Jones, H. Reparative and reconstructive surgery of the female generative tract. (Williams and Wilkins, 1983).
Rosenhein, N. B. & Rock, J. Surgery in the retroperitoneal space. (JB Lippincott, 1988).
Perry, C. P. & Perez, J. The role for laparoscopic presacral neurectomy. J Gynecol Surg 9, 165–168, https://doi.org/10.1089/gyn.1993.9.165 (1993).
Acknowledgements
The authors thank David Fay, PhD for assistance with data extraction and verification, and Xiaorui Ji for foreign language translation services.
Author information
Authors and Affiliations
Contributions
Conceived and designed the analysis: Larry E. Miller, Ruemon Bhattacharyya, Valerie M. Miller. Collected the data: Larry E. Miller. Performed the analysis: Larry E. Miller. Wrote first draft: Larry E. Miller. Provided critical review and manuscript revisions: Ruemon Bhattacharyya, Valerie M. Miller. Final approval of the submitted paper: Larry E. Miller, Ruemon Bhattacharyya, Valerie M. Miller.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miller, L.E., Bhattacharyya, R. & Miller, V.M. Clinical Utility of Presacral Neurectomy as an Adjunct to Conservative Endometriosis Surgery: Systematic Review and Meta-Analysis of Controlled Studies. Sci Rep 10, 6901 (2020). https://doi.org/10.1038/s41598-020-63966-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63966-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.