Abstract
Herpes simplex labialis (HSL) is a viral disease that affects the perioral region. No guidelines recommending an effective treatment exist. The treatment of HSL with three different products was examined. Herpatch Serum, a film-forming patch, was compared to Compeed Patches, a set of semiocclusive hydrocolloid patches, and Zovirax Cream (ingredient: 5% acyclovir). In this prospective, randomized, examiner-blind study, 180 patients with recurrent HSL were split into three groups (Compeed: n = 60, Herpatch: n = 60, Zovirax: n = 60) and examined within 24 hours of HSL outbreak (DRKS Registration No.: DRKS00007786). The primary endpoint was healing time. The secondary endpoints were the reaction rate and quality of therapy evaluated by the Clinician’s Global Assessment of Therapy (CGAT) and the Subject’s Global Assessment of Therapy (SGAT) (0 = no response; 10 = excellent response), respectively. There was no significant difference among the healing times for the different products. The mean (95% confidence interval) was 9.67 days (9.11–10.22) for Compeed, 9.30 days (8.75–9.85) for Herpatch, and 9.80 days (9.30–10.30) for Zovirax. The reaction rate and quality of therapy (CGAT and SGAT) of Herpatch were significantly higher than those of Compeed and Zovirax. Within the study limitations, Herpatch proved to be an effective, non-antiviral alternative in the treatment of HSL.
Similar content being viewed by others
Introduction
Herpes simplex labialis (HSL) is a worldwide infection of the oral and perioral regions caused by an infection with Herpes Simplex Virus type 1 (HSV-1) or, rarely, Herpes Simplex Virus type 2 (HSV-2). Despite the high prevalence of HSL, the disease has not yet been well characterized. The seroprevalence of HSV-1 in Germany was 78.4% from 2008 until 20111,2. While many infections remain subclinical, other patients suffer from painful recurrent infections.
Following the primary infection with HSV-1, the virus replicates at the site of infection and proceeds to travel retrograde down unmyelinated sensory fibres to the trigeminal ganglion, where it establishes latency3. Interfering triggers such as psychological or physiological stress, UVB radiation, trauma, menstruation, sideropenia or febrile illness can provoke the reactivation of the virus4,5.
The course of disease in recurrent HSL generally involves several stages. Within the precursor stage, pain, tingling, or burning sensations in the affected area may occur. This is followed by the appearance of a macule, turning into a papule and leading to the formation of a vesicle. The vesicle bursts, and the formation of a soft scab is initiated. Subsequently, the soft scab is replaced by a hard scab. Over time, the scab falls off, and the lesion is fully healed without scarring6,7,8. While healing, the process is often accompanied by symptoms such as pain, discomfort or reduced self-esteem6. Complete healing takes seven to ten days7.
The treatment of recurrent HSL turns out to be very difficult and variable. Because of the slight effects of diverse therapies, the infection represents a constant and global public health problem9. Episodic therapy can be used for relief of accompanying symptoms10. Therefore, several topical applications, such as phytotherapeuticals, natural remedies, photodynamic therapy, heat and laser application, as well as antiviral substances, can be provided11,12,13,14,15,16.
The application of antiviral creams such as the Zovirax Cream (Zovirax; Glaxo Wellcome Operations, Barnard Castle, England), is favoured by most patients. Zovirax includes 5% acyclovir as an active ingredient. Acyclovir enters the affected cells and represses viral replication. The cream soothes symptoms such as pain, itching and burning. It is applied five times daily on the lesion and adjoining skin until complete healing occurs. Application should occur on at least four consecutive days but should not exceed 10 days17. Due to the potential for irritation and contact sensitization, the cream should not be applied on the skin if hypersensitivities against the components exist. Systemic toxicology studies were not required since an overdosage of the cream is unlikely because of the minimal exposure18.
An alternative is provided in the Compeed Invisible Cold Sore Patches that include no antiviral ingredient (Compeed; Johnson & Johnson Santé Beauté France SAS, Sézanne, France). The cytotoxicity was tested on fibroblasts. Further studies examined the irritation of the patches on rabbits and the sensitivity on guinea pigs. The outer layer of the patch consists of a semiocclusive polyurethane film, which allows excessive wound exudate to evaporate while keeping the lesion moist, ensuring an optimum moisture level. The patch seals the wound and arranges ideal conditions for wound healing. The patch functions as a shield, protecting surrounding areas from infection. As soon as the first symptoms occur, the patch is placed on the lesion, replaced if required, and worn for 24 hours until complete healing occurs19.
The newly developed Herpatch Serum (Herpatch; Sylphar NV, Deurle, Belgium) is spread on the lesion after the first symptoms of HSL occur, and within a few moments, it forms a transparent physical protective barrier over and around the lesion. Thus, the serum creates a microenvironment that provides optimal conditions for natural healing. Added ingredients such as zinc sulfate, porphyridium polysaccharide, and beta-glucan improve and accelerate wound healing, protect the lesion from drying out and UV radiation, relieve symptoms, strengthen the skin layers, and improve aesthetics20. The toxicological characteristics of the ingredients present in Herpatch suggest no important toxicological effects. Therefore, the serum is considered safe in cases of swallowing and with regard to topical absorption21. Since Herpatch does not include antiviral substances, it presents a potential alternative in the treatment of HSL. To date, Herpatch has not been compared to other products regarding effectiveness. For this reason, Herpatch was compared to Compeed and Zovirax in the following trial.
Methods
Study design and study population
This monocentre study is a prospective, controlled, randomized assessor-blind trial comparing the effectiveness of three products in the treatment of HSL. A total of 180 patients aged between 18 and 65 years with recurrent HSL participated. Within the first 24 hours of HSL outbreak, the patients visited the dental clinic of the University of Witten/Herdecke. The lesion had to present itself as a precursor lesion, macule, papule, vesicle or ulcer. Data were collected from April 2013 until June 2016. Informed consent was obtained from all 180 patients included in this study.
The subjects participating in this study needed to be between 18 and 65 years and were excluded if they showed any painful illnesses of the teeth or gingiva. Most importantly, the outbreak of the HSL could not have occurred more than 24 hours ago.
Subjects were excluded if they showed limited compliance, suffered from severe illnesses, or had taken antibiotics or anti-inflammatory drugs two weeks ahead of participation. Pregnant or breastfeeding females were excluded. Hypersensitivity against the ingredients contained in the products or alcohol or drug abuse were additional exclusion criteria. If the patient had already applied a product for the treatment of HSL on the present lesion or had participated in a different clinical study, the subject was not allowed to participate.
Before the beginning of the trial, the Independent Ethics Committee of the University of Witten/Herdecke permitted (written consent) the execution of this study (Application-No. 94/2012). Additionally, the study was registered at the German Clinical Trials Register (DRKS-No.: DRKS00007786; Registration-Date: 16. June 2015). The methods in this trial were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki for medical research involving humans and its later amendments as well as the principles of Good Clinical Practice.
Study assessment
Throughout the study, several data points were collected by the clinician and the subject. On the initial examination day (day 1), the name, age, and sex of the patient were documented as well as the date and time of the beginning of the trial. Additionally, the characteristics of the HSL lesion were noted: site (upper or lower red of the lip, left or right corner of the mouth, underneath or above the lip), maximum diameter, and lesion stage.
The lesion stage (precursor lesion, macule, papule, vesicle, ulcer, soft scab, hard scab) was classified by the clinician on each examination day. At the end of the observation period (day 10), the clinician, using the Clinician’s Global Assessment of Therapy (CGAT) evaluated the reaction rate (assessment of the speed of effectiveness of the product) and the reaction quality (assessment of the effectiveness of the product). This assessment was taken over from a clinical trial by Karlsmark et al.22.
The subject was accompanied by a patient’s questionnaire that was filled out on each examination day, assessing the following parameters: severity of symptoms (pain, discomfort, itching, burning, tingling, swelling, soreness, vesicle, scab), protection of the lesion, aesthetics, relief of discomfort, and intolerance. At the end of the observation period (day 10), the subject also assessed the reaction rate and reaction quality using the Subject’s Global Assessment of Therapy (SGAT). Additionally, he or she rated the comfort, functionality, handling, and satisfaction of the applied product (Table 1).
Treatment regimen
To ensure that the assessor was properly blinded, the products were randomly packed into nontransparent envelopes. In chronological order, the envelopes were handed out to the subjects.
Within 24 hours of the outbreak of the HSL, the patients were examined, and therapy with the assigned medication was initiated. Subjects were instructed to use the products as recommended on the package insert. Treatment was finished when the lesion was healed or after 10 days, whichever came first.
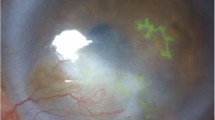
Participation in this study lasted 10 days. On the first day of participation, the subject attended the dental clinic within the first 24 hours of the outbreak of HSL. The inclusion and exclusion criteria were checked. If the patient fulfilled the inclusion criteria, he or she was given a detailed explanation of the reason for and process of the trial. Subsequently, the HSL lesion was documented by taking a photo, noting the stage and site, and measuring the maximum diameter. The patient’s questionnaire and the envelope with the medication were handed out to the participant.
On the 2nd, 4th, 6th, 8th and 10th days, the subject returned at the clinic, and the present stage of the lesion was documented. On the last examination day, the clinician documented the present situation by taking a photo.
Outcome measures
The primary endpoint examines the existence of differences between the three products in terms of healing time. The assessments of the reaction rate and the reaction quality by the clinician (CGAT) and by the subject (SGAT) were defined as the secondary endpoints. The analysis of the patient’s questionnaire was determined as the tertiary endpoint.
Statistical analysis
To produce significant results, the sample size was estimated with the programme G*Power 3.1.9.223. A sample size of 180 patients (60 participants per treatment group) was calculated with a statistical power of 0.8, an alpha error of 0.05, and a 15% drop-out quote with an effect size of 0.5. All data were statistically analysed with the program SPSS 24.0.
The survival curves of the healing time for the primary endpoint were determined using the Kaplan-Meier estimator, and comparisons among the three different treatments were performed by the log-rank test (p < 0.05). All data are fully available without restriction.
The Kolmogorov-Smirnov, Kruskal-Wallis, and Mann-Whitney U tests were used to determine the existence of statistically significant differences among the three tested products regarding the secondary endpoint. After Bonferroni correction, the probability of error p and the level of significance were defined as p = 0.025.
The primary and secondary endpoints were statistically analysed. The tertiary endpoint was analysed descriptively to characterize and provide insight into the overall treatment effects.
Results
Characteristics of study participants and lesions
A total of 180 subjects participated and met the inclusion criteria. There was no drop-out (Fig. 1).
Overall, 81.67% of the subjects were females, and the mean age was 31.46 years (SD: ± 10.79; range: 18–61 years). At the onset, the sizes of the lesion were not significantly different among the three groups. The mean diameter was 0.65 cm. Most of the lesions were located on the upper and lower red of the lip. The locations of the sites showed a similar distribution in all three groups (Table 2).
Healing time
There was no statistically significant difference (log-rank test; p = 0.414) in the healing time among the three products. The mean (95% confidence interval) healing time was 9.67 days (9.11–10.22) for Compeed, 9.30 days (8.75–9.85) for Herpatch and 9.80 days (9.30–10.30) for Zovirax (Fig. 2).
Reaction rate and reaction quality
The reaction rate and reaction quality were evaluated at the end of the therapy by the clinician (CGAT) and the subjects (SGAT) on a scale from 0 to 10 (0 = no response; 10 = excellent response). Both parameters, evaluated by the clinician and subject, were significantly higher for Herpatch compared to Compeed and Zovirax.
The median (25th and 75th percentile) reaction rate (CGAT) of Herpatch was 8.00 (7.25–9.00) and was significantly different (p = 0.001) from that of Compeed, with a median of 7.00 (6.00–8.00), and that of Zovirax, with a median of 7.00 (5.00–8.00). Additionally, the median (25th and 75th percentile) reaction quality (CGAT) showed significantly greater (p = 0.001) for Herpatch, with a median of 8.00 (8.00–9.00), than for Compeed, with a median of 7.00 (6.00–8.00), and for Zovirax, with a median of 7.00 (5.00–8.00) (Fig. 3).
Median (25th and 75th percentile), minimum and maximum of the reaction rate (a) and reaction quality (b) of the product assessed by the clinician (CGAT) at the end of therapy (day 10). Horizontal lines with “***” indicate significant differences between the products, and “†” indicates the lack of a statistically significant difference.
The median (25th and 75th percentile) reaction rate (SGAT) of Herpatch was 8.00 (7.00–9.00) and was significantly different (p = 0.025) from that of Compeed, with a median of 7.00 (5.25–8.00), and that of Zovirax, with a median of 7.00 (4.00–9.00). Additionally, the median (25th and 75th percentile) of the reaction quality (SGAT) was significantly different (p = 0.025) between Herpatch, with a median of 8.00 (7.00–9.00), and Compeed, with a median of 7.00 (5.00–8.00), as well as between Herpatch and Zovirax, with a median of 7.00 (4.00–8.00) (Fig. 4).
Median (25th and 75th percentile), minimum and maximum of the reaction rate (a) and reaction quality (b) of the product assessed by the subject (SGAT) at the end of therapy (day 10). Horizontal lines with “***” indicate significant differences between the products, and “†” indicates a lack of a statistically significant difference.
Accompanying symptoms and product features
All tested products were well tolerated and showed no serious adverse events. The development of symptoms showed a similar distribution in all three groups. While pain, discomfort, itching, burning, tingling, swelling, and blisters occurred primarily at the beginning of therapy, the appearance of soreness and crusts increased until the end of the treatment. All symptoms were rated on a scale from 0 to 10 (0 = no symptoms; 10 = severe symptoms) (Fig. 5).
The assessment of product features was performed on a 0 to 10 scale. The highest ratings of lesion protection (0 = no protection; 10 = high protection), aesthetics (0 = poor aesthetics; 10 = high aesthetics), and relief of discomfort (0 = no relief; 10 = high relief) were achieved with Herpatch use. However, Herpatch led to the most intolerances (0 = tolerant; 10 = intolerant), such as dried lips or redness. The assessment of comfort (0 = no comfort; 10 = high comfort), functionality (0 = poor functionality; 10 = high functionality), handling (0 = hard handling; 10 = easy handling), and satisfaction (0 = no satisfaction; 10 = high satisfaction) were more in favour of Herpatch (Fig. 6).
Discussion
Within this monocentre, randomized, assessor-blind study, the effectiveness of three different products in the treatment of HSL was evaluated in a total of 180 patients. In this study cohort, the sex ratio was in favour of females (81.67%). This can be explained by the higher prevalence of clinically manifested orofacial herpes simplex in females than in males24,25,26. In addition, the number of females working at the University of Witten/Herdecke is higher than the number of males. Due to the high number of participants in this single study, we included the patients as soon as HSL occurred, leading to a higher number of enrolled females. Comparable studies also did not consider the unbalanced proportion of male to female participants in the recruitment22,27,28. This can be considered a limitation of this study, but the advantage of this study is the high number of participants. The mean age of the participants is comparable to that of a study from Senti et al., with a mean of 32.6 years. They included patients from 18 to 50 years of age29. Clinical trials with a minimum age of 18 result in a higher mean age30,31,32. Participation lasted 10 days, which is equal to that of comparable studies22,33,34. Other studies have defined longer periods of observation of up to 22 days35,36,37. An extended observation span allows the monitoring of lesions with a longer healing time but might lead to a negative impact on the recruitment and compliance of patients. Treatment was initiated in the first 24 hours of the outbreak of the lesion. Within this time, the prodromal lesion turns into a vesicle38. Gross and Braun observed a vesicle on the first examination day in 88% of the patients. Because of the high prevalence of vesicles, this early lesion stage was considered the beginning of the evaluation of the healing time33.
The healing time of HSL lesions treated with Herpatch was comparable to that of lesions treated with Compeed and with Zovirax (primary endpoint). The differences among Herpatch, Compeed and Zovirax were small and not statistically significant. Herpatch contains several ingredients that provide perfect conditions for wound healing, while the Compeed semiocclusive hydrocolloid dressing promotes moist wound healing and reduces crusting19,20. Both products do not influence the viral replication cycle. Only Zovirax includes an antiviral agent (5% acyclovir)17. Application of this substance at an early prodromal stage leads to an inhibition of the viral replication of HSV-1 in the host cell39. The early prodromal stage generally presents with subclinical symptoms that are usually imperceptible to the patient. A delayed application of acyclovir at a later stage does not influence the healing time36,40.
The statistical analysis of the reaction rate and the reaction quality showed statistically significant differences between Herpatch and Compeed as well as between Herpatch and Zovirax, both in favour of Herpatch. Karlsmark et al. evaluated the same parameters without assessing statistically significant differences between Compeed and Zovirax22. Hydrocolloid wound dressings such as the Compeed patches promote re-epithelialization and reduce inflammatory responses41,42. However, in this clinical trial, the patch had to be removed several times due to the patch margins peeling off. This was caused particularly by liquids such as saliva, food or drinks or by facial expressions. The peeled-off margins led to discomfort and caused the patient to renew the patch. With every replacement, already formed crusts were torn off with the patch, causing pain while promoting primary wound healing. Accompanying symptoms such as pain, tingling, swelling, or burning were also assessed in comparable trials43,44. The duration and intensity of symptoms were rated and showed comparable distributions independent of the applied product. This evaluation is important to prove the effective impact of treatment on healing.
Creams for topical application, such as Zovirax, wear off quickly while eating or drinking. For this reason, topical creams do not persist for an adequate time on the lesion and need to be reapplied every three to four hours45. This leads to a higher rating of unsatisfaction, which was also shown in comparable clinical studies46. Skulason et al. also assessed the aesthetics of a transparent gel compared to that of a white cream. Most patients preferred the gel because of its high aesthetic qualities3. Subjects treating recurrent HSL with Herpatch indicated high comfort, good aesthetics, easy use of application and overall high satisfaction with the product.
In this study, three disparate materials were compared. Double blinding would have minimized the risk of bias47. Because of the use of three different materials, conducting a double-blinded study under true conditions would have been challenging. To ensure objective assessments, the clinician was blinded, and the evaluation of healing time by the clinician was determined as the primary endpoint. The reaction rate and reaction quality were defined as secondary endpoints.
Finally, it is important to mention that this clinical trial did not include a placebo group. The comparison of an antiviral substance to a placebo can prove the positive characteristics of the antiviral compound. While Zovirax leads to an active antiviral treatment, Herpatch and Compeed only contain ingredients for the relief of symptoms. The antiviral effect and benefits of acyclovir have been shown in several studies, where placebo led to severe symptoms while healing48,49. Nevertheless, a comparable study also observed no significant differences regarding the healing time between Zovirax and Compeed22. Additionally, studies using a placebo showed false results because of the placebo’s ingredients, leading to a comparable healing time as an acyclovir cream36,50. For these reasons, the inclusion of a placebo group was waived.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supporting materials.
References
Korr, G. et al. Decreasing seroprevalence of herpes simplex virus type 1 and type 2 in Germany leaves many people susceptible to genital infection: time to raise awareness and enhance control. BMC Infect. Dis. 17, 471 (2017).
Darai, G., Handermann, M., Sonntag, H. G., Tidona, C. & Zöller, L. In Lexikon der Infektionskrankheiten des Menschen (Third Edition) (ed. Gholamreza Darai) 388–91 (Springer, 2009).
Skulason, S., Holbrook, W. P., Thormar, H., Gunnarsson, G. B. & Kristmundsdottir, T. A study of the clinical activity of a gel combining monocaprin and doxycycline: a novel treatment for herpes labialis. J. Oral. Pathol. Med. 41, 61–67 (2012).
Arduino, P. G. & Porter, S. R. Herpes Simplex Virus Type 1 infection: overview on relevant clinico-pathological features. J. Am. Acad. Dermatol. 37, 107–121 (2008).
Diebold, S. & Overbeck, M. Soft Tissue Disorders of the Mouth. Emerg. Med. Clin. N. Am. 37, 55–68 (2019).
Dreno, B., Malkin, J. E., Saiag, P. & Batuji-Garin, S. Patient´s profile, burden of disease and quality of life in recurrent herpes labialis: a survey conducted in USA and France. J. Eur. Acad. Dermatol. 26, 1458–1460 (2012).
McCarthy, J. P., Browning, W. D., Teerlink, C. & Veit, G. Treatment of herpes labialis: comparison of two OTC drugs and untreated controls. J. Esthet. Restor. Dent. 24, 103–109 (2012).
Browning, W. D. & McCarthy, J. P. A case series: herpes simplex virus as an occupational hazard. J. Esthet. Restor. Dent. 24, 61–66 (2012).
Raborn, G. W. & Grace, M. G. Recurrent herpes simplex labialis: selected therapeutic options. J. Can. Dent. Assoc. 69, 498–503 (2003).
Tubridy, E., Kelsberg, G. & St. Anna, L. Clinical Inquiry: which drugs are most effective for recurrent herpes labialis?. J. Fam. Pract. 63, 104–105 (2014).
Patora, J. & Klimek, B. Flavonoids from lemon balm (Melissa officinalis L., Lamiaceae). Acta Pol. Pharm. 59, 139–143 (2002).
Al-Waili, N. S. Topical honey application vs. acyclovir for the treatment of recurrent herpes simplex lesions. Med. Sci. Monit. 10, 94–98 (2004).
Honarmand, M., Farhadmollashahi, L. & Vosoughirahbar, E. Comparing the effect of diode laser against acyclovir cream for the treatment of herpes labialis. J. Clin. Exp. Dent. 9, 729–732 (2017).
Arduino, P. G. & Porter, S. R. Oral and perioral herpes simplex virus type 1 (HSV-1) infection: review of its management. Oral Dis. 12, 254–270 (2006).
Lotufo, M. A. et al. “Efficacy of photodynamic therapy on the treatment of herpes labialis: a systematic review”. Photodiagnosis Photodyn. Ther. (2019).
Zupin, L. et al. Antiviral properties of blue laser in an in vitro model of HSV-1 infection. Microbiol. Immunol. (2018).
Glaxo Operations UK. ZOVIRAX Labialis, 50 mg/g, Crème Aciclovir (Package Insert) (2012).
U.S. Food and Drug Administration. ZOVIRAX (acyclovir) cream 5% for topical use - Reference ID: 3481551 (2014).
Johnson & Johnson. Compeed Herpesbläschen-Patch (Package Insert) (2011).
Sylphar NV. Herpatch - herpes cold sore serum (Package Insert) (2017).
Sylphar NV. Clinical Evaluation Report of the medical device Herpatch Serum (2017).
Karlsmark, T., Goodman, J. J., Drouault, Y., Lufrano, L. & Pledger, G. W. Randomized clinical study comparing Compeed cold sore patch to acyclovir cream 5% in the treatment of herpes simplex labialis. J. Eur. Acad. Dermatol. 22, 1184–1192 (2008).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A. G. Statistiacal power analysis using G*Power 3.1: Test for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160 (2009).
Malvy, D. et al. Epidemiology of orofacial herpes simplex virus infections in the general population in France: results of the HERPIMAX study. J. Eur. Acad. Dermatol. 21, 1398–1403 (2007).
Pica, F. & Volpi, A. Public awareness and knowledge of herpes labialis. J. Med. Virol. 84, 132–137 (2012).
QuickStats. Age-Adjusted Trends in the Prevalence of Herpes Simplex Virus Type 1 (HSV-1) and Herpes Simplex Virus Type 2 (HSV-2) Among Adolescents and Adults Aged 14-49 Years - United States,1999-2000 Through 2015-2016. Morb. Mortal. Wkly Rep. 67, 203 (2018).
Van Vloten, W. A., Swart, R. N. & Pot, F. Topical acyclovir therapy in patients with recurrent orofacial herpes simplex infections. J. Antimicrob. Chemother. 12, 89–93 (1983).
Jautová, J. et al. Lip creams with propolis special extract GH 2002 0.5% versus aciclovir 5.0% for herpes labialis (vesicular stage): Randomized, controlled double-blind study. Wien. Med. Wochenschr. 169, 193–201 (2019).
Senti, G. et al. A Randomized, Double-Blind, Placebo-Controlled Study to Test the Efficacy of Topical 2-Hydroxypropyl-Beta-Cyclodextrin in the Prophylaxis of Recurrent Herpes Labialis. Dermatology 226, 247–252 (2013).
Raborn, G. W. et al. Effective treatment of herpes simplex labialis with penciclovir cream: combined results of two trials. J. Am. Dent. Assoc. 133, 303–309 (2002).
Spruance, S. L. et al. Acyclovir cream for treatment of herpes simplex labialis: results of two randomized, double-blind, vehicle-controlled, multicenter clinical trials. Antimicrob. Agents Chemother. 46, 2238–2243 (2002).
Spruance, S. L. et al. High-dose, short-duration, early valacyclovir therapy for episodic treatment of cold sores: results of two randomized, placebo-controlled, multicenter studies. Antimicrob. Agents Chemother. 47, 1072–1080 (2003).
Gross, G. & Braun, D. Efficacy and tolerability of topical foscarnet sodium in treatment of herpes labialis: Results of post-marketing surveillance. Hautarzt 57, 40–46 (2006).
Sacks, S. L. et al. Clinical efficacy of topical docosanol 10% cream for herpes simplex labialis: A multicenter, randomized, placebo-controlled trial. J. Am. Acad. Dermatol. 45, 222–230 (2001).
Evans, T. G. et al. Double-blind, randomized, placebo-controlled study of topical 5% acyclovir-1% hydrocortisone cream (ME-609) for treatment of UV radiation-induced herpes labialis. Antimicrob. Agents Chemother. 46, 1870–1874 (2002).
Spruance, S. L. et al. Early, patient-initiated treatment of herpes labialis with topical 10% acyclovir. Antimicrob. Agents Chemother. 25, 553–555 (1984).
Semprini, A. et al. Kanuka honey versus aciclovir for the topical treatment of herpes simplex labialis: a randomised controlled trial. BMJ Open 9 (2019).
Fatahzadeh, M. & Schwartz, R. A. Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management. J. Am. Acad. Dermatol. 57, 737–763 (2007).
Doerr, H. W. & Gerlich, W. In Medizinische Virologie: Grundlagen, Diagnostik, Prävention und Therapie viraler Erkrankungen (Second Edition) (Hans W. Doerr) 17-43, 149-153, 653-660 (Thieme Verlag, 2010).
Spruance, S. L. et al. Treatment of recurrent herpes simplex labialis with oral acyclovir. J. Infec.t Dis. 161, 185–190 (1990).
Junker, J. P. E., Kamel, R. A., Caterson, E. J. & Eriksson, E. Clinical Impact Upon Wound Healing and Inflammation in Moist, Wet, and Dry Environments. Adv. Wound Care 2, 348–356 (2013).
Wei, L. The application of moist dressing in treating burn wound. Open Med. 10, 452–456 (2015).
Khemis, A. et al. Evaluation of the efficacy and safety of a CS20(R) protective barrier gel containing OGT compared with topical aciclovir and placebo on functional and objective symptoms of labial herpes recurrences: a randomized clinical trial. J. Eur. Acad. Dermatol. 26, 1240–1246 (2012).
Arenberger, P., Arenbergerova, M., Hladikova, M., Holcova, S. & Ottillinger, B. Comparative Study with a Lip Balm Containing 0.5% Propolis Special Extract GH 2002 versus 5% Aciclovir Cream in Patients with Herpes Labialis in the Papular/Erythematous Stage: A Single-blind, Randomized, Two-arm Study. Curr. Ther. Res. Clin. E. 88, 1–7 (2018).
Tang, W. & Bhushan, B. Adhesion, friction and wear characterization of skin and skin cream using atomic force microscope. Colloids Surf. B 76, 1–15 (2010).
Zschocke, I., Reich, C., Zielke, A., Reitmeier, N. & Reich, K. Silica gel is as effective as acyclovir cream in patients with recurrent herpes labialis: results of a randomized, open-label trial. J. Dermatol. Treat. 19, 176–181 (2008).
Carson, C. F., Ashton, L., Dry, L., Smith, D. W. & Riley, T. V. Melaleuca alternifolia (tea tree) oil gel (6%) for the treatment of recurrent herpes labialis. J. Antimicrob. Chemother. 48, 450–451 (2001).
Chen, F. et al. Efficacy and safety of nucleoside antiviral drugs for treatment of recurrent herpes labialis: a systematic review and meta-analysis. J. Oral Pathol. Med. 46, 561–568 (2017).
Petti, S. & Lodi, G. The controversial natural history of oral herpes simplex virus type 1 infection. Oral Dis. 25, 1850–1865 (2019).
Shaw, M. et al. Failure of acyclovir cream in treatment of recurrent herpes labialis. BMJ Open 291, 7–9 (1985).
Acknowledgements
We thank Sylphar (Deurle, Belgium) for the funding of the materials, compensation for the participants, etc.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.B., S.Z. Data curation: M.B. Formal analysis: M.B., H.B. Investigation: H.B., A.W. Methodology: M.B., S.Z., V.G. Project administration: M.B., V.G. Supervision: M.B., V.G., S.Z. Validation: M.B., V.G. Writing (original draft preparation): H.B., A.W. Writing (review and editing): M.B. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Boes, H., Goulioumis, V., Wechsler, A. et al. Clinical Study on the Effectiveness of Three Products in the Treatment of Herpes Simplex Labialis. Sci Rep 10, 6465 (2020). https://doi.org/10.1038/s41598-020-63530-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63530-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.