Abstract
Impairments in oxygen delivery and consumption can lead to reduced muscle endurance and physical disability. Perfusion, a measure of microvascular blood flow, provides information on nutrient delivery. T2* provides information about relative tissue oxygenation. Changes in these parameters following stress, such as exercise, can yield important information about imbalance between delivery and consumption. In this study, we implemented novel golden angle radial MRI acquisition technique to simultaneously quantify muscle perfusion and T2* at 7T with improved temporal resolution, and demonstrated assessment of spatial and temporal changes in these parameters within calf muscles during recovery from plantar flexion exercise. Nine healthy subjects participated the studies. At rest, perfusion and T2* in gastrocnemius muscle group within calf muscle were 5 ± 2 mL/100 g/min and 21.1 ± 3 ms respectively. Then the subjects performed plantar flexion exercise producing a torque of ~8ft-lb. Immediately after the exercise, perfusion was elevated to 79.3 ± 9 mL/100 g/min and T2* was decreased by 6 ± 3%. The time constants for 50% perfusion and T2* recovery were 54.1 ± 10 s and 68.5 ± 7 s respectively. These results demonstrate successful simultaneous quantification of perfusion and T2* in skeletal muscle using the developed technique.
Similar content being viewed by others
Introduction
Muscle weakness and fatigue are common manifestations of a variety of diseases that decrease mobility such as multiple sclerosis (MS), Parkinson’s disease (PD), and aging1,2,3,4. The underlying causes of muscle weakness and fatigue are not completely understood. It has been shown that impaired cellular energy production plays an important role in muscle fatigue5. Cells require adequate supplies of oxygen (O2) and nutrients for energy production, and deficiency in O2 supply and extraction may reduce cellular energy production required for muscle function. Accordingly, measurements of O2 delivery and microvascular oxygenation are of considerable interest and have the potential to provide useful understanding of the biochemical mechanisms of decreased mobility in disease and the assessment of treatment targets and responses.
Perfusion is the delivery of tissue mass normalized rate of blood, which also accommodates the supply of O2 and other nutrients to the tissue. Quantitative perfusion in skeletal muscle can be measured non-invasively using the arterial spin labeling (ASL) MRI technique. This technique has been used to study muscle perfusion in humans with ischemia- in reperfusion and exercise paradigms6,7. These studies have demonstrated that skeletal muscle perfusion dynamics are capable of providing insights into pathological and physiological functions8,9,10.
Blood oxygenation level-dependent (BOLD) contrast has been used to infer changes in blood oxygenation in skeletal muscle in response to various stimuli11. Muscle BOLD contrast results primarily from changes in the total amount of deoxyhemoglobin in the imaging volume12. The decrease in the deoxyhemoglobin content in a voxel causes a decrease in susceptibility hence increased signal intensity in the gradient echo BOLD MRI images. The BOLD signal largely depends on the changes in T2*. Quantitative T2* maps may provide more specific physiological information about muscle oxygen extraction in response to stimuli.
Oxygen delivery and demand are tightly coupled in exercising muscle and this coupling might be compromised in pathologic state13. Combined measurement of dynamic perfusion and T2* in skeletal muscle has the potential to provide important information about oxidative metabolism and functional deficits. Studies of combined quantification of perfusion and T2* or other markers of tissue oxygenation have been implemented for reactive hyperemia6,14,15, but there has been no demonstration of this technique for submaximal exercise (functional hyperemia) at 7T using radial acquisition. We chose functional hyperemia because it is more physiologically analogous to the demands of daily living than reactive hyperemia. High signal to noise advantage of 7T and low susceptibility to bulk motion due to radial acquisition will allow more robust determination of perfusion and T2* in dynamic studies with higher temporal resolution. Although several challenges, such as magnetic field inhomogeneity, need to be overcome at ultra-high filed studies, but improved SNR and improved contrast at ultra-high field benefits the dynamic measurement of ASL and T2*.
The main goal of this study is to develop and demonstrate the feasibility of a technique to simultaneously determine dynamic changes in perfusion and T2* in calf muscle at improved temporal resolution with an exercise stimulus. High temporal resolution is important for detection of significant changes in these metabolism related parameters following exercise. To accomplish this aim, we developed a novel interleaved golden angle radial MRI pulse sequence and quantified muscle perfusion and T2*. We built an MRI compatible plantar flexion exercise device and demonstrated the assessment of spatial and temporal changes in these parameters in calf muscle during recovery from plantar flexion exercise. Combined measurements can not only reduce experiment time but also several types of information can be obtained with same stimulus.
Methods
The study was approved by the Auburn University Institutional Review Board (IRB). All experiments were performed in accordance with the IRB guidelines and regulations. Informed consent was provided by each subject prior to participation in the study.
Recruitment
All experiments were done on a Siemens 7T Magnetom (Erlangen, Germany) using a surface coil. Nine healthy volunteers (six females), age = 28 ± 12 years, and weight = 67 ± 8 kg, participated in the study. Inclusion criteria was normal range of motion (> 20°) for ankle joint flexion.
Imaging sequence
Flow alternating inversion recovery (FAIR) is an established ASL method in which slice-selective (SS) and non-selective (NS) inversion pulses are used to acquire tag and control image16. Saturation inversion recovery (SATIR) is a variant of FAIR with short recovery time acquisition, thus allowing for fast dynamic measurements17. The dead time between tagging and acquisition (post labeling delay (PLD)) during perfusion imaging can be used to interleave a gradient echo (GRE) imaging loop to acquire multi-echo images from a slice posterior to the perfusion imaging slice. These multi-echo GRE images are used to quantify T2*. This interleaved approach allows simultaneous measurement of perfusion and T2* with a single scan.
Schematic of pulse sequence is shown in Fig. 1. ASL sequence SATIR was implemented using adiabatic full passage hyperbolic secant inversion pulse for spin tagging with golden angle radial readout (Fig. 1 - slice 1). The PLD was used for interleaved acquisition of T2* data for a slice located 3 cm distally from the perfusion slice (Fig. 1 - slice 2). A multi-echo GRE sequence with radial acquisition was used for T2* mapping. Temporal resolution for perfusion and T2* was approximately 1.3 seconds.
Schematic of pulse sequence and prescription of imaging slices. Pulse sequence consisted of two loops. The outer perfusion loop (top) was acquired with interleaved tagging (SS) and control (NS) adiabatic inversion pulse followed by PLD and radial acquisition of perfusion imaging slice (slice 1). Inner loop consisted of multi-echo GRE pulse sequence implemented during the PLD delay to get multi echo images for T2* calculation. Five echo images were acquired during one outer perfusion loop with echo times = 2.2, 5.0, 7.8, 10.6 and 13.4 ms. Perfusion slice was selected 3 cm proximal to the T2* slice which accounts for the incoming arterial blood flow direction.
Phantom experiment
Initial experiments were done in phantoms to optimize radial image reconstruction at 7T and validate measurements from the new sequence.
Shift estimation and correction
In radial acquisition, the read-out orientation is changed to different angles for each k-space line to acquire a set of radial projections. Gradient imperfection and eddy current effects cause delays in gradient timing and have an angle dependent effect on the projections. This causes the center of acquired projections to shift yielding artifacts in reconstructed images18,19.
We characterized these gradient imperfections in phantoms by collecting projections for x-gradient along angles 0° and 180° and y-gradient along angles 90° and 270°. A delay in gradient timing causes a spatial shift in two projections acquired with opposite gradient polarity. This shift was corrected as described below for x-axis.
Flip one of the 0° and 180° spokes.
-
1.
Take the FT of the magnitude of two spokes.
-
2.
Calculate and plot the phase difference between these two signals. The center of the plot will show a linear phase change due to spatial shift in projections.
-
3.
Fit a linear equation to the phase difference and calculate the slope of that line.
-
4.
Shift along ky = 0 line was calculated from the slope from the equation given by:
\(\Delta {k}_{x}=-\frac{slope\times N}{4\pi }\), where N = no. of samples.
Same procedure is used with 90° and 270° spokes to calculate Δky along kx=0 line. Shift along any arbitrary projection angle ϴ is calculated using20:
Agarose phantoms at 0.5, 1, 2, 3, 4 and 5% concentration were prepared in 50 mL vials to validate perfusion and T2* measurements. The phantoms were prepared by mixing Agarose powder with water, then heated until boiling. New interleaved pulse sequence was used to determine T2* and perfusion and the results were compared to the results from vendor provided multi-echo GRE pulse sequence.
In vivo study design
After scanner adjustments, perfusion and T2* data were acquired in the calves of the participants at rest. A 1H/31P surface coil (RAPID Biomedical, Rimpar, Germany) with single channel compatible with Siemens Magnetom 7T system was used for the study. The maximum average transmit power of 1H coil was 11.5 W with quadrature RF polarization as per specification. The mean coil dimension of 1H double-loop was 140 mm × 225 mm.
A 6 ms long slice selective (SS) and non-selective (NS) hyperbolic secant adiabatic inversion pulse was used to acquire tag and control images in an interleaved fashion. The inversion efficiency was tested in phantoms as well as in vivo, and a voltage of 500 V was selected for satisfactory inversion slice profile (Figs. S.1 and S.2 in Supplementary Information). Specific common acquisition parameters for perfusion and T2* were: FOV = 192 mm, slice thickness = 5 mm, TR = 1.28 s, flip angle = 15°, bandwidth = 500 Hz/pixel and 64 radial projections. Perfusion PLD = 1 s. TE = 2.2 ms for perfusion and TE = 2.2, 5.0, 7.8, 10.6 and 13.4 ms for GRE sequence.
The subjects then performed 2 minutes of plantar flexion at 0.5 Hz using a home-built MRI compatible exercise device. The knee angle was 0° (aligned with the scanner table) during exercise and the leg was held in place with Velcro straps to prevent bulk motion. The paddle of the device was strapped to an adjustable support with a rubber band and the subjects pushed against the generated resistance. The support position can be adjusted to produce different torques. The torque produced by the subjects in this study was measured to be ~8 ft-lb (~10.8 Nm). A metronome was used to provide audio signal to the volunteers for guiding the ankle plantar flexion exercise protocol. Only slice-selective images were acquired for 3 minutes as participants rested and recovered from exercise, since non-selective acquisitions will interfere with the nearby T2* slice.
It can be shown from SATIR signal derivation17 that
where, MSS and MNS are slice selective and non-selective acquisitions respectively, M0 is the tissue magnetization at equilibrium, T1 is tissue spin-lattice relaxation time constant. As SATIR approach assumes constant T1 for all perfusion values, Eq. (2) shows that, if the signals are corrected for the T2* weighting, the summation of SS and NS signal is approximately constant regardless of the perfusion value. NS value during recovery period can be estimated by subtracting the recovery SS value from the (SS+NS) value at rest. Not acquiring NS images during recovery from exercise results in improved temporal resolution. The recovery NS signal can be estimated using
where MNS,rest and MSS,rest are NS and SS acquisitions respectively at rest, MNS,rec and MSS,rec are NS and SS signals respectively during recovery post-exercise, T2,rest* and T2,rec* are T2* values at rest and during recovery respectively.
Perfusion weighted images were generated from the differences between slice selective and non-selective images at rest. The muscle area activated with high perfusion due to exercise was identified from the perfusion weighted images immediately after exercise. From this muscle activation map a region of interest (ROI) was selected to calculate the perfusion using17
where f is the perfusion (mL/100 g/min), λ is tissue partition coefficient (0.9 mL/g), T is tagging time (or PLD), T1 for tissue is 1.55 sec.21 at 7T. Dynamic change in perfusion was measured as a change from the resting perfusion during the recovery period.
T2* was calculated by fitting a mono-exponential function to the magnitude signal intensity from multi-echo data using
T2* was normalized to the resting T2* values for each individual subject. This was done to account for differences in T2* between subjects due to physiological variances or different shimming.
Results
Phantom experiment
Radial image reconstruction without correction of gradient delay errors showed artifacts (Fig. 2a). Two vials placed on the upper side of a box-shaped phantom were completely missing in the reconstructed image without delay correction. 0° and 180° calibration projections resulted in a sample shift of 0.595 along kx and 90° and 270o projections resulted in a sample shift of 0.696 along ky. In vivo calibration data (Δkx = 0.588 and Δky = 0.689) was similar to that from phantom experiments. The artifacts in the reconstructed image were removed and the vials were visible after accounting for gradient delay errors (Fig. 2b). This same protocol was used for all imaging studies in vivo.
Difference between radial image reconstruction without and with gradient delay error correction. (a) Phantom image shows artifacts without the correction of gradient delay errors. There are two vials on the top that disappear in the reconstructed image. (b) Image after correction for gradient delays.
Phantom study
Figure 3 shows six agar phantoms with different concentrations. Perfusion image of the phantom shows noise indicating that the presence of second slice for T2* has no spillover effect on the perfusion slice. Excellent correlation was found between the two T2* values measured by standard multi-echo GRE sequence and new interleaved sequence with r2 = 0.98. The Bland-Altman plot also shows very good agreement between two methods with mean difference = −0.12 ± 1.15.
In vivo
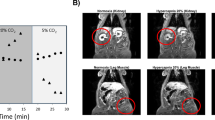
Representative locations of perfusion (slice 1) and T2* (slice 2) are shown in Fig. 4a. At rest, the gastrocnemius muscle has the highest perfusion = 5 ± 2 mL/min/100 g. Sample SS signal time course from gastrocnemius muscle during recovery following plantar flexion exercise is shown in Fig. 5a. As SS, NS, T2* signals were acquired at rest and only SS, T2* were measured during recovery, Eq. (3) was used to estimate the NS signal during recovery period. Finally, Eq. (4) was used to calculate the perfusion. Figure 5b shows the sample perfusion time courses calculated with and without NS acquisition, which manifests that perfusion can be estimated with great accuracy even without the NS acquisition. Figure 4b,c show the perfusion results from plantar flexion exercise. Quantitative perfusion maps are overlaid on the anatomical images indicating the regions of highest change from rest (Fig. 4b). Immediately after exercise, the gastrocnemius muscle showed the highest increase in perfusion. A region of interest (ROI) corresponding to the activated muscle regions identified on the perfusion maps was manually traced on the images and the mean change in perfusion is shown in Fig. 4c. Immediately after exercise, the perfusion in the most activated area of the muscle increased to 79.3 ± 9 mL/min/100 g and decreased slowly to baseline after a relatively fast initial decline during post-exercise rest. Average time constant for 50% perfusion recovery was 54.1 ± 10 s. Figure 6a,b show the synopsis of change in perfusion in different muscle groups – gastrocnemius, soleus and peroneus muscles within calf muscle during recovery from exercise. The perfusion in soleus and peroneus muscles are not affected as much as gastrocnemius muscle due to plantar flexion exercise protocol used in this study.
Two slice locations for perfusion and T2* on calf muscle (a). Slice 1 is perfusion slice and slice 2 is T2* slice. Increased perfusion activated area on corresponding perfusion slice (b) and average perfusion with standard deviation of all the subjects during recovery period from selected ROI (green circle) (c). Decreased T2* activated area on corresponding T2* slice (d) and average relative T2* with standard deviation of all subjects during recovery period from selected ROI (e).
Sample T2* curve fitting from one subject at rest is shown in Fig. S.3 (Supplementary Information). Figure 4d shows overlay of change in T2* after plantar flexion exercise indicating regions of muscle activation. Change in T2* was determined from the difference between the first and last T2* map generated during the recovery period. A region of interest (ROI) was selected to observe the relative change of T2* (normalized by the resting T2*) and is shown in Fig. 4e. T2* decreased by 6 ± 3% immediately after exercise and recovered as the subjects rested. At the end of data acquisition time, T2* did not return to baseline (resting value) and was still off by 2 ± 0.7%. Average time constant for 50% recovery from minimum value to this peak value was 68.5 ± 7 s. Figure 6c,d show the synopsis of change in T2* in different muscle groups- gastrocnemius, soleus and peroneus muscles within calf muscle during recovery from exercise. It shows that T2* of soleus and peroneus muscles are not affected as much as gastrocnemius muscle and return approximately to baseline while gastrocnemius muscle T2* remains elevated by the end of acquisition time. Table 1 shows perfusion and T2* values from the most activated muscle area due to exercise i.e. gastrocnemius muscle of all subjects.
Discussion
We have demonstrated the feasibility of simultaneous quantification of changes in perfusion and T2* in lower leg following plantar flexion exercise. The sequence was tested and validated in phantoms before in vivo studies. Perfusion measurement without the NS acquisition was also compared with the one measured with the NS acquisition. The temporal resolution of the sequence allowed us to measure dynamic changes in perfusion and T2* as the muscle recovered from the submaximal exercise. We used plantar flexion exercises because it is a simple exercise protocol and physiologically more relevant than reactive hyperemia. The changes in post exercise perfusion and T2* values is in general agreement with values from previous reported studies. This pulse sequence and exercise protocol provides a unique ability to investigate different aspects of muscle metabolic function (i.e., regional perfusion and tissue blood oxygenation). Although some studies reported simultaneous measurement of perfusion and T2* weighted signal at 7T22,23, but none of them measured quantitative T2*. T2* weighted signal, which can also be termed as BOLD signal24,25, is dependent on the change in T2* as well as the initial signal intensity, which is influenced by parameters such as inflow, baseline drifts and changes in T125. Measurement of T2* enables to separate the oxygenation related changes25,26,27. Moreover, the advantage of our current technique compared to the other available techniques is higher temporal resolution, which is vital for measuring notable changes in these metabolism-related parameters following exercise (Fig. 5b), and the fact that radial readout provides more flexibility in quantification of perfusion and T2* as sudden twitch of the subject during measurement of these parameters may result in faulty measurement, which can be overcome by radial readout and the subject feels more comfortable (Fig. S.4 in Supplementary Information).
Exercise increased the blood flow to the stimulated tissue. Perfusion measurement without the NS acquisition was compared with the one measured with NS acquisition from one subject in vivo during recovery following exercise, which shows that our current technique can measure perfusion with excellent accuracy. The muscle perfusion immediately at the end of exercise increased to 79.3 ± 9 mL/min/100 g from a resting value of 5 ± 2 mL/min/100 g. Prior studies with similar exercise protocols reported a peak perfusion in the range of 60 to 84 mL/min/100 g in gastrocnemius muscle7,28,29, in close agreement with our results. The difference in peak perfusion could be due to different work rates during the exercise protocol and selection of ROI. Lower perfusion values have been reported following reactive hyperemia30. This is expected because contraction elicits exercise dependent metabolic demand and increased flow directed to capillaries supplying the metabolically active tissue, whereas during reactive hyperemia the flow is elevated due to reduced vascular resistance caused by ischemia. Perfusion recovery is also in agreement with previous reports with similar exercise protocol28. Another study reported slower recovery of perfusion after exercise29, similar to recovery reported following anaerobic exercise17. It is difficult to speculate the difference in recovery rates between studies since exercise protocol, metabolic state of the tissue under examination or biological differences between study participants may affect the recovery rate.
T2* at 7T is reported to be approximately 22 ms and our resting values are in agreement with previous studies22. However magnetic field inhomogeneity and shim quality will affect the baseline T2*, as another previous study reported shorter T2* of ~17 ms at 7T31. We normalized the post exercise recovery T2* in each subject with the baseline T2* values to eliminate these scanner dependent variations and allow for comparison between subjects. A lower value of T2* is observed immediately after exercise and indicates deoxygenation of activated muscle; i.e., a decrease in venous oxygen saturation. As T2* starts to recover it goes to a peak value of approximately 2% higher than the baseline (resting value). Previous studies reported similar kind of T2* response during recovery following exercise29. This is also in agreement with BOLD studies in which the BOLD signal immediately decreased at the onset of exercise, stayed low during exercise and only recovered when the muscle was allowed to rest at the completion of exercise24. A drop in T2* weighted signal during exercise followed by a rise of the T2* weighted signal before the end of the exercise in gastrocnemius muscle was reported in a previous study, which was probably caused by a falling pH22. This can also be attributed to the fact that two competing factors, increase in flow and oxygen extraction to meet increased metabolic demand due to exercise32,33,34, and rapid decrease in partial oxygen pressure in active muscle35 contribute to the T2* weighted signal change36. Also, activity level can impact T2* weighted signal37 and T2* weighted signal represents all potential contributions to signal loss, including T1 effects, T2 effects and magnetic field inhomogeneities. Following exercise, the perfusion in activated muscle is increased which also affects local blood volume, which is expected to have pronounced effect on BOLD signal. In future with carefully designed exercise paradigms it may be possible to separate the effect of T2* changes due to perfusion and oxygen extraction.
There are a few limitations to the existing study. In order to calculate perfusion, the SATIR approach assumes that the muscle and blood T1 are same17. Measurement of blood and muscle T1 at rest and during recovery post-exercise is not practical. Hence all previous reports using SATIR approach made the assumption that blood and tissue T1 are equal15,17. Different T1 values for muscle (T1 = 1.55 sec)21 and blood (T1 = 2.08 sec)38 have been reported at 7T. Simulation using the reported T1 values for muscle and blood shows that the error introduced in perfusion measurement is not expected to exceed 7%. Another issue of assuming constant T1 throughout the recovery period post-exercise, as implemented by SATIR approach, may affect perfusion estimation as T1 is expected to change due to the change in blood oxygenation levels. The maximum TE for multi echo GRE acquisition should be ≥ T2*. Our maximum TE affected T2* quantification with a maximum error <4%, which was validated in phantom experiment. Also, some recent works showed that muscle metabolic and oxidative capacity varies along the length of the muscle even within the same muscle group39, which was also observed as a gradient in T2* weighted signals between two distal slice locations following exercise23. This suggests that even though the T2* slice should have similar kind of T2* response as the perfusion slice, but there might still be a gradient between the actual numbers. We did not quantify the actual work done during the exercise protocol. Metabolic demand for the tissue provides a feedback signal for increase in blood supply hence it is important to get a measure of work done by the muscles. We also used a surface coil for this study. Since there is no body coil in for 7T, we used the surface coil for both transmit/receive, which compromises the signal to noise from muscle groups at a distance from the coil. A knee coil or other volume coil placed around the calf would improve signal to noise and provide better homogeneous coverage. The plantar flexion device was not compatible with the knee coil due to size restrictions. In future, a new design of the plantar flexion device would allow the study to be conducted with the knee coil. We did not validate the perfusion measurements with an identical ASL sequence without multi-echo GRE loop. This would have required two separate exercise protocols. Difference in the exercise work rate during the two exercise protocols or fatigue can potentially make the comparison difficult. We did test in the phantom that the presence of the multi-echo loop did not affect the perfusion slice data (Fig. 3b). In the present study we evaluated the effect of perfusion loop on the T2* measurements and did not find any evidence that perfusion slice affects the measurement of T2* for at slice 3 cm distal location.
Conclusion
This study demonstrates the ability to simultaneously quantify skeletal muscle perfusion and T2*, both at rest and dynamically during post exercise recovery in calf muscle at 7T using radial acquisition at high temporal resolution. An interleaved golden angle radial acquisition pulse sequence was implemented for the study which helps reduce bulk motion artifacts. The temporal and spatial resolution of the protocol was sufficient to measure changes in metabolism-related parameters post exercise. Regulated plantar flexion exercise isolates the calf muscles and might provide valuable insight into pathophysiological processes independent of impaired heart function. Accordingly, the information provided by this technique may prove to be very valuable in understanding muscle metabolism in healthy subjects as well as patient populations who experience mobility disability such as MS, PD, or older adults. This later observation will be an important next step in this line of research.
References
Finsterer, J. & Mahjoub, S. Z. Fatigue in Healthy and Diseased Individuals. Am J Hosp Palliat Me 31, 562–575, https://doi.org/10.1177/1049909113494748 (2014).
Kluger, B. M., Krupp, L. B. & Enoka, R. M. Fatigue and fatigability in neurologic illnesses Proposal for a unified taxonomy. Neurology 80, 409–416, https://doi.org/10.1212/WNL.0b013e31827f07be (2013).
Heesen, C. et al. Fatigue in multiple sclerosis: an example of cytokine mediated sickness behaviour? J Neurol Neurosur Ps 77, 34–39, https://doi.org/10.1136/jnnp.2005.065805 (2006).
Bakshi, R. Fatigue associated with multiple sclerosis: diagnosis, impact and management. Mult Scler J 9, 219–227, https://doi.org/10.1191/1352458503ms904oa (2003).
Enoka, R. M. & Duchateau, J. Muscle fatigue: what, why and how it influences muscle function. J Physiol-London 586, 11–23, https://doi.org/10.1113/jphysiol.2007.139477 (2008).
Duteil, S. et al. Influence of vascular filling and perfusion on BOLD contrast during reactive hyperemia in human skeletal muscle. Magn Reson Med 55, 450–454, https://doi.org/10.1002/mrm.20760 (2006).
Pollak, A. W. et al. Arterial Spin Labeling MR Imaging Reproducibly Measures Peak-Exercise Calf Muscle Perfusion A Study in Patients With Peripheral Arterial Disease and Healthy Volunteers. Jacc-Cardiovasc Imag 5, 1224–1230, https://doi.org/10.1016/j.jcmg.2012.03.022 (2012).
Grozinger, G. et al. Perfusion measurements of the calf in patients with peripheral arterial occlusive disease before and after percutaneous transluminal angioplasty using MR arterial spin labeling. J Magn Reson Imaging 40, 980–987, https://doi.org/10.1002/jmri.24463 (2014).
Wu, W. C. et al. Skeletal muscle microvascular flow in progressive peripheral artery disease: assessment with continuous arterial spin-labeling perfusion magnetic resonance imaging. J Am Coll Cardiol 53, 2372–2377, https://doi.org/10.1016/j.jacc.2009.03.033 (2009).
Englund, E. K. et al. Multiparametric assessment of vascular function in peripheral artery disease: dynamic measurement of skeletal muscle perfusion, blood-oxygen-level dependent signal, and venous oxygen saturation. Circ Cardiovasc Imaging 8, https://doi.org/10.1161/CIRCIMAGING.114.002673 (2015).
Elder, C. P., Cook, R. N., Chance, M. A., Copenhaver, E. A. & Damon, B. M. Image-Based Calculation of Perfusion and Oxyhemoglobin Saturation in Skeletal Muscle During Submaximal Isometric Contractions. Magnet Reson Med 64, 852–861, https://doi.org/10.1002/mrm.22475 (2010).
Donahue, K. M. et al. Simultaneous gradient-echo/spin-echo EPI of graded ischemia in human skeletal muscle. J Magn Reson Imaging 8, 1106–1113, https://doi.org/10.1002/jmri.1880080516 (1998).
Oliveira, M. F. et al. Does impaired O-2 delivery during exercise accentuate central and peripheral fatigue in patients with coexistent COPD-CHF? Frontiers in Physiology 5, ARTN 514 10.3389/fphys.2014.00514 (2015).
Lebon, V., Carlier, P. G., Brillault-Salvat, C. & Leroy-Willig, A. Simultaneous measurement of perfusion and oxygenation changes using a multiple gradient-echo sequence: application to human muscle study. Magn Reson Imaging 16, 721–729, https://doi.org/10.1016/s0730-725x(98)00088-5 (1998).
Englund, E. K. et al. Combined measurement of perfusion, venous oxygen saturation, and skeletal muscle T-2* during reactive hyperemia in the leg. J Cardiovasc Magn R 15, Artn 70 10.1186/1532-429x-15-70 (2013).
Kim, S. G. & Tsekos, N. V. Perfusion imaging by a flow-sensitive alternating inversion recovery (FAIR) technique: application to functional brain imaging. Magn Reson Med 37, 425–435, https://doi.org/10.1002/mrm.1910370321 (1997).
Raynaud, J. S. et al. Determination of skeletal muscle perfusion using arterial spin labeling NMRI: Validation by comparison with venous occlusion plethysmography. Magnet Reson Med 46, 305–311, https://doi.org/10.1002/mrm.1192 (2001).
Peters, D. C., Derbyshire, J. A. & McVeigh, E. R. Centering the projection reconstruction trajectory: reducing gradient delay errors. Magn Reson Med 50, 1–6, https://doi.org/10.1002/mrm.10501 (2003).
Block, K. & Uecker, M. Simple method for adaptive gradient-delay compensation in radial MRI. In Proccedings of 19th Annual Meeting of ISMRM, Qubec, Canada (2011).
Armstrong, T. et al. Free-breathing liver fat quantification using a multiecho 3D stack-of-radial technique. Magn Reson Med 79, 370–382, https://doi.org/10.1002/mrm.26693 (2018).
Jordan, C. D., Saranathan, M., Bangerter, N. K., Hargreaves, B. A. & Gold, G. E. Musculoskeletal MRI at 3.0 T and 7.0 T: A comparison of relaxation times and image contrast. Eur J Radiol 82, 734–739, https://doi.org/10.1016/j.ejrad.2011.09.021 (2013).
Schewzow, K. et al. Dynamic ASL and T2-weighted MRI in exercising calf muscle at 7 T: a feasibility study. Magn Reson Med 73, 1190–1195, https://doi.org/10.1002/mrm.25242 (2015).
Niess, F. et al. Interleaved P-31 MRS/H-1 ASL for analysis of metabolic and functional heterogeneity along human lower leg muscles at 7T. Magnet Reson Med, https://doi.org/10.1002/mrm.28088 (2019).
Muller, M. D. et al. Muscle oxygenation during dynamic plantar flexion exercise: combining BOLD MRI with traditional physiological measurements. Physiol Rep 4, https://doi.org/10.14814/phy2.13004 (2016).
Ledermann, H. P. et al. Blood oxygenation level-dependent magnetic resonance imaging of the skeletal muscle in patients with peripheral arterial occlusive disease. Circulation 113, 2929–2935, https://doi.org/10.1161/Circulationaha.105.605717 (2006).
Schulte, A. C., Speck, O., Oesterle, C. & Hennig, J. Separation and quantification of perfusion and BOLD effects by simultaneous acquisition of functional I-0- and T-2*-parameter maps. Magnet Reson Med 45, 811–816, https://doi.org/10.1002/mrm.1109 (2001).
Speck, O. & Hennig, J. Functional imaging by I-0- and T-2*-parameter mapping using multi-image EPI. Magnet Reson Med 40, 243–248, https://doi.org/10.1002/mrm.1910400210 (1998).
Wray, D. W. et al. Multiparametric NMR-Based Assessment of Skeletal Muscle Perfusion and Metabolism During Exercise in Elderly Persons: Preliminary Findings. J Gerontol a-Biol 64, 968–974, https://doi.org/10.1093/gerona/glp044 (2009).
Englund, E. K. et al. Simultaneous measurement of macro- and microvascular blood flow and oxygen saturation for quantification of muscle oxygen consumption. Magnet Reson Med 79, 846–855, https://doi.org/10.1002/mrm.26744 (2018).
Englund, E. K. et al. Combined measurement of perfusion, venous oxygen saturation, and skeletal muscle T2* during reactive hyperemia in the leg. J Cardiovasc Magn Reson 15, 70, https://doi.org/10.1186/1532-429X-15-70 (2013).
Towse, T. F. et al. Comparison of muscle BOLD responses to arterial occlusion at 3 and 7 Tesla. Magnet Reson Med 75, 1333–1340, https://doi.org/10.1002/mrm.25562 (2016).
Cain, S. M. & Chapler, C. K. O-2 Extraction by Canine Hindlimb during Alpha-Adrenergic Blockade and Hypoxic Hypoxia. J Appl Physiol 48, 630–635 (1980).
Kingvanvlack, C. E., Curtis, S. E., Mewburn, J. D., Cain, S. M. & Chapler, C. K. Role of Endothelial Factors in Active Hyperemic Responses in Contracting Canine Muscle. J Appl Physiol 79, 107–112 (1995).
Schaffartzik, W. et al. Effect of Reduced Hemoglobin Concentration on Leg Oxygen-Uptake during Maximal Exercise in Humans. J Appl Physiol 75, 491–498 (1993).
Poole, D. C. & Richardson, R. S. Determinants of oxygen uptake - Implications for exercise testing. Sports Med 24, 310–322 (1997).
Li, Z. J. et al. Dynamic characteristics of T2*-weighted signal in calf muscles of peripheral artery disease during low-intensity exercise. Journal of Magnetic Resonance Imaging 46, 40–48, https://doi.org/10.1002/jmri.25532 (2017).
Stacy, M. R. et al. Comparison of regional skeletal muscle tissue oxygenation in college athletes and sedentary control subjects using quantitative BOLD MR imaging. Physiological Reports 4, UNSP e12903 10.14814/phy2.12903 (2016).
Zhang, X. et al. In vivo blood T(1) measurements at 1.5 T, 3 T, and 7 T. Magn Reson Med 70, 1082–1086, https://doi.org/10.1002/mrm.24550 (2013).
Boss, A. et al. Oxidative capacity varies along the length of healthy human tibialis anterior. J Physiol-London 596, 1467–1483, https://doi.org/10.1113/Jp275009 (2018).
Author information
Authors and Affiliations
Contributions
Experiments, data analysis and manuscript preparation: S.Z.M.; Supervision of the study, experiments, edited the manuscript and conceived the study: A.B.; Edited the manuscript and conceived the study: T.S.D., R.W.M., L.B.G., A.N.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmud, S.Z., Gladden, L.B., Kavazis, A.N. et al. Simultaneous Measurement of Perfusion and T2* in Calf Muscle at 7T with Submaximal Exercise using Radial Acquisition. Sci Rep 10, 6342 (2020). https://doi.org/10.1038/s41598-020-63009-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-63009-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.








