Abstract
Alcohol use disorder (AUD) is a chronic and relapsing disease with a substantial genetic influence. Given the recent discovery of the association of PPM1G methylation with alcohol use disorder (AUD) from a genome-wide methylation study, we sought to verify and extend the previous work of AUD-related impulsivity in a Korean population with AUD. A total of 244 men with AUD were assessed for psychological characteristics and behavioral impulsivity using stop signal task (response inhibition) and Balloon Analog Risk Task (risk-taking). Leukocyte DNA methylation at PPM1G was quantified using pyrosequencing. The effects of PPM1G methylation on severity of problematic drinking measured by Alcohol Use Disorder Identification Test (AUDIT) and multidimensional impulsivity were tested using linear regression analyses. Hypermethylation of PPM1G was significantly associated with risk-taking propensity among men with AUD. No significant association of PPM1G methylation was found to be associated with AUDIT scores and response inhibition. Our findings indicate that altered methylation of PPM1G may influence the impulsive choice of risk-taking in AUD. Further research is required in order to determine the role of PPM1G in the pathophysiology of AUD and multidimensional impulsivity.
Similar content being viewed by others
Introduction
Alcohol use disorder (AUD) is a chronic relapsing disease characterized by excessive alcohol drinking and loss of control over alcohol consumption. Approximately 50% of the risk of AUD can be attributed to genetic factors1. Based on the results from genome-wide association studies of AUD, it is suggested that hundreds of variants with small genetic effects across the genome contribute to the genetic susceptibility of AUD2. In addition to a genetic predisposition, growing evidence supports the theory that environmental factors, such as early life stress, increases vulnerability for the development and psychopathological conditions of AUD3,4. Childhood adversity has been reported to be associated with early initiation of alcohol5 and higher suicidal attempts in patients with AUD6. These findings suggest that the interplay between genes and environment is involved in the pathophysiology of AUD.
Epigenetic modifications such as DNA methylation (reversible modulation of gene expression without changing the DNA sequence), can be key to understanding these gene-environment interactions. A genome-wide DNA methylation study with 18 monozygotic twin pairs discordant for AUD discovered a differentially methylated region in the 3’-protein-phosphatase-1G (PPM1G) gene that is considered to be potentially involved in modulating cortical transmission to the striatum through dephosphorylation of the metabotropic glutamate receptors7. That study also showed that the PPM1G DNA methylation level was associated with PPM1G gene expression, and PPM1G hypermethylation was correlated with an escalation in daily alcohol drinking as well as an impulsivity trait, measured by self-reported impulsivity and brain activity during behavioral inhibition task, in independent adolescent samples7.
Given the recent discovery of an epigenetic association of the PPM1G gene with AUD, we sought to verify and extend the previous work of AUD-related impulsivity in a Korean clinical population with AUD. Since the impulsivity trait, an endophenotype for AUD, is a multifaceted construct8,9, we assessed multidimensional impulsivity using a self-report measure and behavioral tasks, including impulsive action of response inhibition and impulsive choice of risk-taking, and examined their associations with the PPM1G. To ascertain an unbiased effect of the PPM1G, we controlled for the effects of potential confounders such as childhood adversity on epigenetic modulation.
Methods
Participants
A total of 244 male subjects with AUD were included in this study. All participants were recruited from inpatients psychiatric facilities for detoxification and rehabilitation of AUD and assessed after detoxification treatment. Diagnosis of AUD was confirmed by psychiatrists using a structured clinical interview for the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV-TR) criteria and clinical observation. Most recent drinking confirmed by clinician was at least 7 days before study enrollment, and no signs of alcohol intoxication or withdrawal symptoms were observed in any participant on the study day of self-report questionnaire and tasks. Exclusion criteria were: (1) being admitted primarily for another major psychiatric disorder; (2) having an intellectual disability; and (3) having other substance dependencies except tobacco use. In addition, subjects with mood disorders including major depressive disorder based on the DSM-IV-TR criteria and clinician’s careful observation were excluded. Participants were ethnically all Korean. Ethnicity was determined based on self-reported ethnicity and the administrator’s observations. All patients who participated in this study provided written informed consent according to the procedures approved by the Severance Hospital Institutional Review Board (Seoul, Korea), and all protocols were performed in accordance with approved guidelines.
Measurements
The severity of problematic drinking in patients with AUD was assessed using the Alcohol Use Disorders Identification Test (AUDIT)10. Higher AUDIT scores indicated a more harmful drinking behavior. The Korean version of the Barratt Impulsiveness Scale (BIS) was also used to assess participants’ self-reported impulsivity. To evaluate childhood trauma, we used the modified Korean version of the Parent-Child Conflict Tactics Scale (mPCCTS)11 which is based on the Parent-Child Conflict Tactics Scale12. The severity of depressive and anxiety symptoms was assessed using the Beck Depression Inventory (BDI)13 and the Beck Anxiety Inventory (BAI)14. All questionnaires had been validated in the Korean population previously11,15,16,17,18.
Behavioral tasks for impulsive action and impulsive choice
The stop signal task (SST) was used to assess the impulsive action of response inhibition19. The stop-signal reaction time (SSRT) was estimated. A higher SSRT value indicates a worse inhibitory control. In addition, the Balloon Analog Risk Task (BART)20, a computerized decision-making test, was conducted to assess the impulsive choice of risk-taking. Risk-taking propensity was measured by calculating the mean number of pumps in trials during which the balloons did not explode, a higher BART score represents a greater risk-taking propensity.
Pyrosequencing of PPM1G
Venous blood samples were collected in 4 ml EDTA vacutainers and stored at −80 °C prior to analysis. Genomic DNA was isolated from whole blood using the standard techniques. Three cytosine-guanine (CpG) sites in the 3’ untranslated region (UTR) of PPM1G were selected and designed using PSQ Assay Design software (QiagenTM) based on the previous study7. The genomic locations of the three selected CpG sites were as follows: CpG1 (Chr2: 27,604,246; GRCh37), CpG2 (Chr2: 27,604,258; GRCh37), and CpG3 (Chr2: 27,604,271; GRCh37). Pyrosequencing was used for DNA methylation analysis by Genomictree, Inc. The DNA was bisulfite treated and sequencing was performed using the Pyro Gold reagents kit (Qiagen, Hilden, Germany).
Statistical analyses
The SPSS 25.0 software for Windows (SPSS Inc., Chicago, IL, USA) was used for analyses of all data in this study. Descriptive statistical analyses were performed for various variables including demographic, clinical, and epigenetic characteristics of the participants in this study. Multivariable linear regression analyses with the ‘enter method’ were used to test the associations of the PPM1G methylation level with the AUDIT scores and multidimensional impulsivity (self-reported impulsivity; BIS score, impulsive action; SST, and impulsive choice; BART) after adjusting for multiple potential confounders. The regression model included the PPM1G methylation level, childhood trauma (high vs. low), and other demographic and clinical variables (age, duration of AUD, depressive symptoms, and anxiety levels), that may influence the relationship between the PPM1G and AUD-related phenotypes, as independent variables. Childhood trauma exposure was categorized as a binary value, high and low, using a median split of mPCCTS scores. The mean value of methylation levels at the three CpG sites in PPM1G was used for analyses.
Results
Demographic and clinical characteristics
Socio-demographic, clinical characteristics and the methylation level of the PPM1G of the study participants are summarized in Table 1. All participants were men with AUD, and further detailed descriptions are presented in Table 1.
Regression model predicting the severity of problematic drinking and multidimensional impulsivity
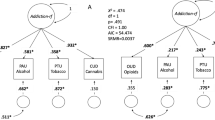
A regression model demonstrated no significant association of the PPM1G with AUDIT scores. Among the potential associated factors selected as independent variables by the regression model, young age, long duration of AUD, higher BDI scores and presence of childhood adversity were significantly associated with higher AUDIT scores (Table S1).
For multidimensional impulsivity, a regression model of impulsive action showed a significant association between PPM1G and risk-taking propensity as measured by the BART (Table 2). In this model, PPM1G methylation explained 3.5% of the variance in risk-taking propensity, indicating small to moderate effect size. Hypermethylation of the PPM1G was correlated with higher risk-taking propensity. On the other hand, a regression model of the BIS score showed no significant association of the PPM1G with self-reported impulsivity trait. In that model, only depressive symptom severity was significantly associated with self-reported impulsivity (Table S2). In addition, a regression model of impulsive choice showed no significant association of the PPM1G with response inhibition by SSRT value (Table S3).
Discussion
The present study examined the role of PPM1G DNA methylation in multidimensional impulsivity among clinical samples with AUD, based on the novel finding of the PPM1G differentially methylated region from a genome-wide DNA methylation study of monozygotic twins discordant for AUD7. Our results demonstrated a significant association between PPM1G hypermethylation and the impulsive choice of risk-taking propensity after adjusting for the possible effects of variable confounders such as childhood adversity on epigenetic changes. When considering that the impulsive choice of risk-taking dramatically increases in early adolescence21 and is known to contribute to increase susceptibility for AUD22, our findings suggest that PPM1G hypermethylation may mediate the effect of high risk-taking in the pathophysiology of AUD.
Hypermethylation at the PPM1G region on chromosome 2 has been reported to be associated with lower mRNA levels of PPM1G in adolescent non-clinical samples7, although we did not examine the mRNA expression in this study. The previous finding indicates that PPM1G methylation levels influence PPM1G expression and protein levels. PPM1G is a member of the human protein phosphatase 2C (PP2C) family which has been implicated in cellular survival and stress response23,24. Studies in animals and in vitro work suggested a role of the PPM1G in regulating cell cycle progression and cellular stress response pathways23. Although little is known about the biological functioning of the PPM1G in humans, there is some indirect evidence suggesting a relationship between the PPM1G and AUD-related phenotypes. The region of chromosome 2p14‐2q14.3 has been linked to various psychiatric conditions including AUD and suicidal attempts, related to impulsivity and behavioral disinhibition25,26,27. A genetic study with polymorphisms across chromosome 2 in a case-control sample for alcoholism showed a significant association of rs2384629, a genetic polymorphism on the PPM1G gene, with combined AUD and suicide attempts or conduct phenotypes25. This suggests a genetic role of the PPM1G in AUD-related impulsivity. Ruggeri et al. reported a significant association of PPM1G hypermethylation with self-reported impulsivity measured by impulsivity-related subscales of the Substance Use Risk Profile Scale (SURP). This association was significant even after controlling for the possible genotype effects of polymorphisms covering the PPM1G locus of methylation status. Although the biological function of the PPM1G remained unclear, these findings suggest that the PPM1G may play a role in the pathophysiology of AUD, possibly through the impulsivity trait, an endophenotype for AUD.
Among our regression models predicting severity of problematic drinking or multidimensional impulsivity, the PPM1G methylation level was significant only for the impulsive choice of risk-taking, not for AUDIT scores, self-reported impulsivity, or impulsive action of behavioral inhibition using the stop signal task. Lack of significant association between PPM1G and AUDIT scores in the present study seemed to be consistent with the previous negative finding of alcohol exposure severity in non-clinical adolescents7. However, our sample consisted entirely of chronic alcohol-dependent patients with relatively high AUDIT scores. Therefore, the relationship between PPM1G methylation and severity of AUD needs to be confirmed in a cohort that includes the entire spectrum of AUDIT scores. For impulsivity, there was some discrepancy of self-reported impulsivity and behavioral inhibition between our study and Ruggeri’s results. However, direct comparison may be difficult due to a variety of differences including demographic factors such as age, sex, and ethnicity, clinical characteristics (e.g. clinical vs. non-clinical), measurements of impulsive action and choice, as well as the used self-report tools (e.g. BIS vs. SURP). Because impulsivity is a complex and multidimensional construct in nature8,9, comprehensive measure of multidimensional impulsivity would be beneficial to enhance the determination of the genetic effects on trait impulsivity and brain response related to impulsivity as an endophenotype for AUD.
Although biological mechanisms modulating methylation status of PPM1G is unknown, recent research suggests that excessive alcohol use can induce epigenetic dysregulation in human and rodent brains through alteration of the DNA methylation dynamics such as changes in DNA-methyltransferase (DNMT) expression and activity28,29. A postmortem brain study of bipolar disorder and schizophrenia suggested that chronic alcohol abuse has an effect on number of DNMT 1 mRNA-positive neurons29. Further research is needed to elucidate the biological mechanisms underlying regulation of DNA methylation of PPM1G.
There are several limitations to this study. First, we did not recruit healthy controls, as our main purpose was to examine epigenetic influence of PPM1G on quantitative AUD-related traits such as impulsivity among individuals with AUD. Future case control studies with healthy controls may help understand disease-specific methylation changes of PPM1G and their role in AUD. In addition, when considering sex differences in alcohol use and alcohol-related problems30, our findings in male patients may have limited application to female patients with AUD. Second, our study with a cross-sectional design restricts the ability to reveal a causal link of PPM1G methylation with the AUD-related impulsivity trait. Ruggeri et al.’s finding of a significant association of PPM1G hypermethylation with the escalation of daily alcohol drinking between ages 14 and 16 in non-clinical adolescents supports the possibility that PPM1G hypermethylation may be a vulnerable marker for developing AUD, rather than a consequence of AUD. Future longitudinal research is warranted in order to establish the direction of causality in their relationship. Third, we did not consider the effect of some potential confounders, including heterogeneity in white blood cell composition31 and cigarette smoking32,33, that may contribute to inter-individual variability in DNA methylation. In particular, since smoking can induce epigenetic modifications, the possible effect of smoking on DNA methylation should be considered in future studies. Fourth, since we cannot measure DNA methylation levels directly in the brain during clinical studies, we assumed that the DNA methylation pattern of PPM1G in peripheral leukocytes reflects the PPM1G methylation pattern in brain. Although DNA methylation is tissue-specific, there is some evidence suggesting that patterns of peripheral DNA methylation or mRNA expression reflect changes in brain tissues34,35. In addition, peripheral PPM1G methylation levels have been reported to be associated with brain activity during the impulsive action task of the SST7. However, it is still questionable whether peripheral DNA methylation could serve as surrogates for DNA methylation in the brain. Finally, the present sample size may be limited to detect an association between DNA methylation levels at a given CpG site and a complex phenotype controlled by many genes with very small effect. Therefore, a study with a larger number of samples with stronger statistical power is needed to confirm the present findings.
In summary, the present study illustrated that the hypermethylation of PPM1G was significantly associated with the impulsive choice of risk-taking propensity, not the severity of problematic alcohol drinking, in a male Korean clinical population with AUD. The present finding supports the conclusion that the altered methylation status of PPM1G influences the pathophysiology of AUD, possibly through the impulsivity trait of risk-taking. Further prospective research is required in order to determine the role of PPM1G in the pathophysiology of AUD and multidimensional impulsivity.
Change history
18 June 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Verhulst, B., Neale, M. C. & Kendler, K. S. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol. Med. 45, 1061–1072, https://doi.org/10.1017/S0033291714002165 (2015).
Deak, J. D., Miller, A. P. & Gizer, I. R. Genetics of alcohol use disorder: a review. Curr. Opin. Psychol. 27, 56–61, https://doi.org/10.1016/j.copsyc.2018.07.012 (2019).
Enoch, M. A. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology 214, 17–31, https://doi.org/10.1007/s00213-010-1916-6 (2011).
Zimmermann, U. S., Blomeyer, D., Laucht, M. & Mann, K. F. How gene-stress-behavior interactions can promote adolescent alcohol use: the roles of predrinking allostatic load and childhood behavior disorders. Pharmacol. Biochem. Behav. 86, 246–262, https://doi.org/10.1016/j.pbb.2006.09.024 (2007).
Rothman, E. F., Edwards, E. M., Heeren, T. & Hingson, R. W. Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics 122, e298–304, https://doi.org/10.1542/peds.2007-3412 (2008).
Roy, A. Distal risk factors for suicidal behavior in alcoholics: replications and new findings. J. Affect. Disord. 77, 267–271 (2003).
Ruggeri, B. et al. Association of Protein Phosphatase PPM1G With Alcohol Use Disorder and Brain Activity During Behavioral Control in a Genome-Wide Methylation Analysis. Am. J. Psychiatry 172, 543–552, https://doi.org/10.1176/appi.ajp.2014.14030382 (2015).
Congdon, E. & Canli, T. The endophenotype of impulsivity: reaching consilience through behavioral, genetic, and neuroimaging approaches. Behav. Cogn. Neurosci. Rev. 4, 262–281, https://doi.org/10.1177/1534582305285980 (2005).
Salvatore, J. E. Gottesman, II & Dick, D. M. Endophenotypes for Alcohol Use Disorder: An Update on the Field. Curr. Addict. Rep. 2, 76–90, https://doi.org/10.1007/s40429-015-0046-y (2015).
Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R. & Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction 88, 791–804 (1993).
Kim, M. & Lee, E. The influence of abused childhood experiences, exposure to suicide and exposure to suicide news on suicidal thought among adolescents: the mediating role of goal instability. Korean J. Youth Stud. 18, 403–429 (2011).
Straus, M. A., Hamby, S. L., Finkelhor, D., Moore, D. W. & Runyan, D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child. Abuse Negl. 22, 249–270 (1998).
Beck, A. T., Steer, R. A. & Carbin, M. G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 8, 77–100 (1988).
Steer, R. A. & Beck, A. T. Beck Anxiety Inventory. 23–40 (1997).
Hahn, H. M. et al. A Standardization Study of Beck Depression Inventory in Korea. J. Korean Neuropsych. Assoc. 25 (1986).
Lee, B. O., Lee, C. H., Lee, P. G., Choi, M. J. & Namkoong, K. Development of Korean Version of Alcohol Use Disorders Identification Test(AUDIT-K):Its Reliability and Validity. J. Korean Acad. addiction psychiatry 4, 83–92 (2000).
Lee, H. The Operation Guide of Impulsiveness Test. Seoul: Korea Guidance (1992).
Yook, S. P. & Kim, Z. S. A clinical study on the Korean version of Beck Anxiety Inventory: comparative study of patient and non-patient. Korean. J. Clin. Psychol. 16, 185–197 (1997).
Band, G. P., Van Der Molen, M. W. & Logan, G. D. Horse-race model simulations of the stop-signal procedure. Acta psychologica 112, 105–142 (2003).
Lejuez, C. W. et al. Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART). J. Exp. psychology. Appl. 8, 75–84 (2002).
Braams, B. R., van Duijvenvoorde, A. C., Peper, J. S. & Crone, E. A. Longitudinal changes in adolescent risk-taking: a comprehensive study of neural responses to rewards, pubertal development, and risk-taking behavior. J. Neurosci. 35, 7226–7238, https://doi.org/10.1523/JNEUROSCI.4764-14.2015 (2015).
Dougherty, D. M. et al. Behavioral Impulsivity and Risk-Taking Trajectories Across Early Adolescence in Youths With and Without Family Histories of Alcohol and Other Drug Use Disorders. Alcohol. Clin. Exp. Res. 39, 1501–1509, https://doi.org/10.1111/acer.12787 (2015).
Foster, W. H., Langenbacher, A., Gao, C., Chen, J. & Wang, Y. Nuclear phosphatase PPM1G in cellular survival and neural development. Developmental dynamics: an. Off. Publ. Am. Assoc. Anatomists 242, 1101–1109, https://doi.org/10.1002/dvdy.23990 (2013).
Lu, G. & Wang, Y. Functional diversity of mammalian type 2C protein phosphatase isoforms: new tales from an old family. Clin. Exp. Pharmacol. Physiol. 35, 107–112, https://doi.org/10.1111/j.1440-1681.2007.04843.x (2008).
Dick, D. M. et al. Evidence for genes on chromosome 2 contributing to alcohol dependence with conduct disorder and suicide attempts. Am. J. Med. Genet. B Neuropsychiatr. Genet 153B, 1179–1188, https://doi.org/10.1002/ajmg.b.31089 (2010).
Foroud, T. et al. Alcoholism susceptibility loci: confirmation studies in a replicate sample and further mapping. Alcohol. Clin. Exp. Res. 24, 933–945 (2000).
Dick, D. M. et al. A genome-wide screen for genes influencing conduct disorder. Mol. Psychiatry 9, 81–86, https://doi.org/10.1038/sj.mp.4001368 (2004).
Bonsch, D. et al. Lowered DNA methyltransferase (DNMT-3b) mRNA expression is associated with genomic DNA hypermethylation in patients with chronic alcoholism. J. neural Transm. 113, 1299–1304, https://doi.org/10.1007/s00702-005-0413-2 (2006).
Guidotti, A. et al. DNA methylation/demethylation network expression in psychotic patients with a history of alcohol abuse. Alcoholism: Clin. Exp. Res. 37, 417–424 (2013).
Schulte, M. T., Ramo, D. & Brown, S. A. Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin. Psychol. Rev. 29, 535–547, https://doi.org/10.1016/j.cpr.2009.06.003 (2009).
Reinius, L. E. et al. Differential DNA methylation in purified human blood cells: implications for cell lineage and studies on disease susceptibility. PloS One 7 (2012).
Jia, Y.-F. et al. Differential SLC1A2 promoter methylation in bipolar disorder with or without addiction. Front. Cell. Neurosci. 11, 217 (2017).
Lee, K. W. & Pausova, Z. Cigarette smoking and DNA methylation. Front. Genet. 4, 132 (2013).
Masliah, E., Dumaop, W., Galasko, D. & Desplats, P. Distinctive patterns of DNA methylation associated with Parkinson disease: identification of concordant epigenetic changes in brain and peripheral blood leukocytes. Epigenetics 8, 1030–1038 (2013).
Zhubi, A. et al. An upregulation of DNA-methyltransferase 1 and 3a expressed in telencephalic GABAergic neurons of schizophrenia patients is also detected in peripheral blood lymphocytes. Schizophr. Res. 111, 115–122 (2009).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (NRF-2018R1A2B2007714). The funding source did not give any influences on the study design, data collection, analysis and interpretation of data, the writing of the report and the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
S.K. and J.K. conceived and planned the study. S.K. and S.H. contributed to data collection and management. C.P., H.K. and J.K. performed the statistical analyses and interpreted the findings. C.P., J.K. and S.K. wrote the manuscript. H.K. provided scientific input and helped edit the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, C.I., Kim, H.W., Hwang, S.S. et al. Association of PPM1G methylation with risk-taking in alcohol use disorder. Sci Rep 10, 5490 (2020). https://doi.org/10.1038/s41598-020-62504-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62504-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.