Abstract
Acute respiratory failure requiring mechanical ventilation is a major indicator of intensive care unit (ICU) admissions in cirrhotic patients and is an independent risk factor for ICU mortality. This retrospective study aimed to investigate the outcome and mortality risk factors in patients with liver cirrhosis (LC) who required prolonged mechanical ventilation (PMV) between 2006 and 2013 from two databases: Taiwan’s National Health Insurance Research Database (NHIRD) and a hospital database. The hospital database yielded 58 LC patients (mean age: 65.3 years; men: 65.5%). The in-hospital mortality was significantly higher than in patients without LC. Based on the NHIRD database of PMV cases, patients were age-gender matched in a ratio of 1:2 for patients with and without LC. Model for End-Stage Liver Disease (MELD) score was calculated. The mortality was higher in patients with LC (19.5%) than those without LC (18.12%), though not statistically significant (p = 0.0622). Based on the hospital database, risk factor analysis revealed that patients who died had significant higher MELD score than the survivors (18.9 vs 13.7, p = 0.036) and patients with MELD score of >23 had higher risk of mortality than patients with MELD score of ≤23 (adjusted OR:9.26, 95% CI: 1.96–43.8). In conclusion, the in-hospital mortality of patients with high MELD scores who required PMV was high. MELD scores may be useful predictors of mortality in these patients.
Similar content being viewed by others
Introduction
The health burden of liver cirrhosis (LC) has significantly increased worldwide1; it resulted in one million mortalities in 2010 according to the Global Burden of Disease Study 2010 and is estimated to cost 31 million Disability Adjusted Life Years (DALYs)2,3. In Taiwan, liver cirrhosis mortalities jumped from 3723 in the 1980s to 6243 in 2010s1. In patients with previously compensated liver cirrhosis, several conditions such as variceal bleeding, ascites, hepato-renal syndrome, hepatic encephalopathy, hepato-pulmonary syndrome, spontaneous bacterial peritonitis, and severe sepsis may result in unstable clinical conditions that require admission to an intensive care unit (ICU). Once a patient with LC is admitted to the ICU, the mortality rate can range from 34% to 69%4.
Acute respiratory failure that requires mechanical ventilation (MV) is a major indication for the requirement of ICU admission for cirrhotic patients and is an independent risk factor of ICU mortality5,6,7. Although the mortality rate of critically ill patients with LC who need MV is >50%8,9,10, critically ill patients might survive the acute stage in the ICU and enter the difficult stage of being weaned off MV and therefore, may require prolonged mechanical ventilation (PMV). Such patients require a lot of healthcare resources and medical expenses; however, their prognoses are unclear and difficult to assess. Being able to predict whether an LC patient will need PMV and be able to predict their outcomes would allow for healthy mutual communication between physicians, patients, and their family to arrive at a consensus about their post-PMV care plans. Once the outcome can be fully understood and the prognosis can be accurately predicted, physicians can help patients and their families make the best choice regarding the use of PMV. However, investigations focusing on the prognoses and outcomes of patients with LC requiring PMV are scarce. Only one recent study has reported the median survival (0.19 years) and life expectancy (3.59 years) of 1478 LC patients requiring PMV11. Thus, this study aims to investigate the outcome of the cirrhotic patients requiring PMV using two databases – The national health insurance research database (NHIRD) and a hospital-based database. Further, we used detailed information obtained from the hospital-based database to identify risk factors associated with patients’ mortality.
Methods
Patients and study setting
This retrospective study was conducted at Chi Mei Hospital, a 1288 bed tertiary medical center in Tainan City, Taiwan. The hospital has 110 adult intensive care unit (ICU) beds and 16 respiratory care center (RCC) beds. The RCC is prepared to care for difficult-to-wean ICU patients. If the critical patients show improvement including hemodynamic stability without vasoactive agents but required oxygenation, had no acute liver or kidney failure, and appeared not to require any more surgical intervention in the near feature, their in-charge ICU physician considers them eligible for transfer from the RCC.
All patients with LC transferred to the RCC between 2006 and 2013 were identified from the NHIRD database; patients who required MV for more than three weeks were included in this study. To assess the effects of LC on the outcome of PMV patients, we used a 1:2 ratio of age-sex matched cohort of LC[positive (+)] and LC[negative (–)] patients. The retrospective data were collected on a routine basis and the analysis was carried out retrospectively. Therefore, no informed consent was required, and it was specifically waived off by our Institutional Review Board (IRB). Ethical approval was obtained from Chi Mei Medical Center (IRB 10411-E01). All methods were performed in accordance with the relevant guidelines and regulations. To effectively use MV and reduce the heavy utilization of the ICU, the Taiwan Bureau of National Health Insurance (BNHI) implemented an integrated prospective payment program (IPP) for patients in Taiwan who required PMV in 200011. Based on this policy, PMV patients were required to be transferred to an RCC after an ICU stay of 21 days and to a respiratory care ward after an RCC stay of 42 days11,12,13. The NHIRD database provides detailed information of all insured inpatients and outpatients using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code. Encrypted personal identification was used to protect the identities of the individuals in the database.
Parameters assessed
The medical records of all the LC patients with PMV were retrospectively reviewed and the following information was collected: age, gender, category of previous ICU stay, length of ICU and RCC stays, diagnosis of RCC admission, duration of MV use in ICU and RCC, Acute Physical and Chronic Healthy Evaluation II (APACHE II) score on ICU and RCC admission, serum albumin level, blood urea nitrogen (BUN) level, electrolytes, and serum creatinine level. The severity of LC was determined using the Model for End-Stage Liver Disease (MELD) score based on the result of blood tests upon RCC admission. In-hospital mortality (death due to any cause) was our primary outcome measure.
Statistical Analysis
Continuous variables are expressed as mean ± standard deviation (SD). The significance of the difference between categorical variables and continuous variables between groups was tested using the χ2 test or one-way analysis of variance, respectively. A multivariable logistic regression model was constructed from baseline characteristics and clinical variables with p-values <0.05 as candidates. For determining the final prediction model, the stepwise model-selection procedure (in which all candidate variables were inserted until non-effects entered or the effects were removed by backward elimination) was used to examine the association between predictive variables and the mortality rate using odds ratios (OR) with 95% confidence intervals (95% CI). In addition, we used MELD score of 23 as a cut-off value for further analysis based on a previous study14. All statistical analyses were conducted using SPSS 19 for Windows (IBM, Armonk, NY, USA). Significance was set at p < 0.05.
Results
Outcome of LC patients with PMV
Fifty-eight LC[+] PMV patients (mean age: 65.3 years; men, 65.5%) were identified from the hospital database. Forty-five patients with LC requiring PMV were transferred from the medical ICU to the RCC unit. Pneumonia (50%) and neuromuscular disease (32.8%) were the most frequent causes of RCC admission. The mean length of RCC stay was 16.8 days and the in-hospital mortality was 29.3% (Table 1). The causes of death included sepsis (n = 10), variceal bleeding (n = 3), intracerebral hemorrhage (n = 2), hepatorenal syndrome (n = 1), and hepatic encephalopathy (n = 1). For sepsis-associated mortality, pneumonia was the most common type of infection (n = 5), followed by peritonitis (n = 3), and central venous catheter-related infection (n = 2). Additionally, in two patients, the endotracheal tube was withdrawn for hospice care.
On comparing this population with the age-sex matched cohort from the NHIRD database, we observed that LC[+]patients requiring PMV were more likely to be transferred to the RCC unit from medical ICU, had a longer length of ICU stay, and had decompensated gastrointestinal diseases causing RCC admission, than LC[–] patients; all these were statistically significant (p < 0.05). There were no significant differences between patients with and without LC; these two cohorts had similar outcomes in terms of length of RCC stay and in-hospital mortality.
We identified 6059 LC[+] patients in the NHIRD and 23,806 LC[–] patients who had undergone PMV. Patients with LC in the NHIRD were younger, had more males, and had significantly more HBV and HCV infections (all p < 0.05). The in-hospital mortality was higher among LC[+] patients than among LC[–] patients (p = 0.0049). However, after age and gender matching age and gender, it was seen that patients with LC had higher mortality than those without LC (19.5% vs 18.12%, p = 0.0622) (Table 2).
Factors predicting in-patient mortality of LC[+] patients requiring PMV
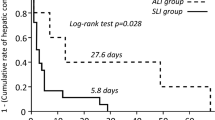
Among the 58 LC[+] patients requiring PMV, 17 patients suffered from in-hospital mortality. No significant difference was observed between survivors and those who died in terms of age, sex, category of transferred ICU, length of stay in ICU and RCC, APACHE II score upon ICU and RCC admission, diagnosis of RCC admission, and laboratory findings (all p > 0.05). However, we did observe that those who died showed significantly higher MELD scores than the survivors (18.9 vs 13.7, p = 0.036) (Table 3), and the higher MELD scores was associated with a higher probability for mortality (Figs. 1 and 2). As reported in a previous study14, we used 23 as the cut-off value of MELD score for further analysis and observed that patients with MELD ≥ 23 had higher risk of mortality than patients with MELD < 23 (adjusted odds ratio [OR]: 9.26, 95% confidence interval [CI]: 1.96–43.8) (Table 4).
Discussion
Using the two databases– hospital-based and NHIRD-based, this study investigated the outcome of LC patients requiring PMV. Initially, we found that the overall mortality of this population was 29.3% and 19.5% in the hospital-based and NHIRD-based investigations, respectively. Although mortality rates of LC[+] patients were higher than those of LC[–] patients, the differences were not significant. The lack of significant survival differences between the cirrhotic and non-cirrhotic cohort maybe because we included patients even with mild LC in this study. In the hospital-based cohort, 29.3% of the total LC patients had MELD score less than 10 which indicated less severe liver cirrhosis and the mortality of this subgroup being lower than patients with a MELD score greater than 10. In addition, we also observed that patients who died had a higher MELD score than the survivors (18.9 vs 13.7). To resolve this issue, we further analyzed the data to identify the risk factor of mortality among LC patients; we only found one prognostic factor - MELD score which was significantly associated with mortality among this specific population. The usefulness of the MELD score in predicting the outcome of cirrhosis patients in various conditions has been demonstrated in previous studies14,15,16,17; however, to the best of our knowledge, our study is the first to show that MELD scores can be associated with mortality in cirrhosis patients requiring PMV. Moreover, by using 23 as a cutoff for MELD score based on a previous study14, we observed that patients with a MELD score of ≥ 23 had a higher risk of mortality than patients with MELD of <23. In summary, the findings of this study indicate that not all LC patients requiring PMV had significantly higher mortality compared to those without LC; patients with severe LC (with higher MELD scores) showed significant association with higher mortality than those with mild LC (lower MELD scores).
Knowing the prognostic factors and being able to predict the outcome of LC[+] patients requiring PMV is important for hepatologists, patients, and patients’ families to have better communication and to arrive at a consensus about the patient’s care plans. More than 20% of the patients requiring PMV are more likely to be near the end of their life and some of them may prefer palliative care to preserve the quality of life rather than prolonging their life expectancy by receiving life-sustaining therapy including PMV. Our findings can help us to better understand the outcome of LC patients on PMV and provide important information about the prognosis of this specific population. Further, it suggests that patients with severe LC on PMV are associated with poor outcome and palliative care may be recommended for these patients.
Our study has a few limitations. First, we measured only the in-hospital mortality rate. We did not assess the patient outcomes post-discharge; thus, we are unable to provide data on long-term outcomes, e.g., the one-year survival rate. In addition, we did not evaluate patients’ quality of life. Further studies are needed to clarify these issues. Second, the number of patients from the single hospital-based setting was limited; therefore, our findings cannot be generalized to patients in other hospitals or countries. However, our study did use another large-scale NHIRD database through which we enrolled many patients. Findings from both the databases were similar; thus, the results should remain representative of this specific population. Third, LC[+] severity was only available in the hospital-based setting, but not in the NHIRD. In addition, because some subjective assessments of LC severity in Child classification, such as ascites and hepatoencephalopathy were not available in this retrospective study, we used MELD scores which provided an objective assessment of the disease severity. Finally, due to the retrospective nature of this study, some bias may have confounded our analysis.
Conclusions
The in-hospital death rate of severe LC[+] patients who required PMV was high and MELD scores may be useful indicators for predicting mortality in this population.
References
Mokdad, A. A. et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 12, 145 (2014).
Murray, C. J. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380, 2179–2223 (2012).
Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380, 2095–2128 (2012).
Saliba, F., Ichai, P., Levesque, E. & Samuel, D. Cirrhotic patients in the ICU: prognostic markers and outcome. Curr. Opin. Crit. Care. 19, 154–160 (2013).
Levesque, E., Saliba, F., Ichai, P. & Samuel, D. Outcome of patients with cirrhosis requiring mechanical ventilation in ICU. J. Hepatol. 60, 570–578 (2014).
Shawcross, D. L. et al. The impact of organ dysfunction in cirrhosis: survival at a cost? J. Hepatol. 56, 1054–1062 (2012).
Levesque, E. et al. Prospective evaluation of the prognostic scores for cirrhotic patients admitted to an intensive care unit. J. Hepatol. 56, 95–102 (2012).
Shellman, R. G., Fulkerson, W. J., DeLong, E. & Piantadosi, C. A. Prognosis of patients with cirrhosis and chronic liver disease admitted to the medical intensive care unit. Crit. Care Med. 16, 671–678 (1988).
Rabe, C. et al. Does intubation really equal death in cirrhotic patients? Factors influencing outcome in patients with liver cirrhosis requiring mechanical ventilation. Intensive Care Med. 30, 1564–1571 (2004).
Zimmerman, J. E., Wagner, D. P., Seneff, M. G., Becker, R. B., Sun, X. & Knaus, W. A. Intensive care unit admissions with cirrhosis: risk-stratifying patient groups and predicting individual survival. Hepatology. 23, 1393–1401 (1996).
Su, J., Lin, C. Y., Chen, P. J., Lin, F. J., Chen, S. K. & Kuo, H. T. Experience with a step-down respiratory care center at a tertiary referral medical center in Taiwan. J. Crit. Care. 21, 156–161 (2006).
Hung, T. C., Lai, Y. F., Tseng, C. W., Hong, Y. H. & Shi, H. Y. Trend analysis of hospital resource utilization for prolonged mechanical ventilation patients in Taiwan: a population-based study. Respir. Care. 58, 669–675 (2013).
Liu, C. J. et al. Impact of Taiwan’s integrated prospective payment program on prolonged mechanical ventilation: a 6-year nationwide study. Respir. Care. 58, 676–682 (2013).
Oberkofler, C. E. et al. Model of end stage liver disease (MELD) score greater than 23 predicts length of stay in the ICU but not mortality in liver transplant recipients. Crit. Care. 14, R117 (2010).
Tsui, T. Y., Scherer, M. N., Schnitzbauer, A. A., Schlitt, H. J. & Obed, A. Adult living donor liver transplantation: body mass index and MELD score of recipients are independent risk factors for hospital mortality. Langenbecks Arch, Surg. 394, 235–241 (2009).
Siniscalchi, A. et al. Pretransplant model for end-stage liver disease score as a predictor of postoperative complications after liver transplantation. Transplant. Proc. 41, 1240–1242 (2009).
Saab, S. et al. MELD score predicts 1-year patient survival post-orthotopic liver transplantation. Liver Transpl. 9, 473–476 (2003).
Author information
Authors and Affiliations
Contributions
K.C. Cheng and C.M. Chen, the guarantor of this manuscript, C.C. Lai, K.L. Tseng, S.R. Chiang, K.S. Chan, C.M. Chao and S.C. Hsing contributed to the conception and design of the study, C.H. Ho, and K.L. Tseng analyzed and interpreted the data, C.C. Lai, and K.C. Cheng drafted the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lai, CC., Tseng, KL., Ho, CH. et al. Outcome of liver cirrhosis patients requiring prolonged mechanical ventilation. Sci Rep 10, 4980 (2020). https://doi.org/10.1038/s41598-020-61601-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-61601-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.