Abstract
Selected patients with large vessel occlusions (LVO) can benefit from thrombectomy up to 24 hours after onset. Identifying patients who might benefit from late intervention after transfer from community hospitals to thrombectomy-capable centers would be valuable. We searched for presentation biomarkers to identify such patients. Frequent MR imaging over 2 days of 38 untreated LVO patients revealed logarithmic growth of the ischemic infarct core. In 24 patients with terminal internal carotid artery or the proximal middle cerebral artery occlusions we found that an infarct core growth rate (IGR) <4.1 ml/hr and initial infarct core volumes (ICV) <19.9 ml had accuracies >89% for identifying patients who would still have a core of <50 ml 24 hours after stroke onset, a core size that should predict favorable outcomes with thrombectomy. Published reports indicate that up to half of all LVO stroke patients have an IGR <4.1 ml/hr. Other potentially useful biomarkers include the NIHSS and the perfusion measurements MTT and Tmax. We conclude that many LVO patients have a stroke physiology that is favorable for late intervention, and that there are biomarkers that can accurately identify them at early time points as suitable for transfer for intervention.
Similar content being viewed by others
Introduction
Patients who suffer strokes caused by large vessel occlusions of the anterior circulation (LVOs, viz., terminal internal cerebral artery or middle cerebral artery M1/M2 occlusions) typically will have severe neurological deficits and poor outcomes if not treated1. While they comprise approximately a third of all ischemic strokes, they cause most deaths and poor outcomes. Clinical trials have shown that LVO-stroke patients may be effectively treated with thrombectomy within 6–8 hours2,3,4,5,6,7,8. More recently, the DAWN9 and DEFUSE-310 trials have proven that thrombectomy may be successful up to 24 hours post ictus in carefully selected LVO patients. The widening of the thrombectomy time window presents new opportunities to treat LVO stroke patients; the challenge in community hospitals is to identify patients who will benefit from thrombectomy despite late arrivals or delays due to transfer to intervention-capable centers. We analyzed our cohort of LVO patients who underwent frequent MR imaging over 2 days to identify biomarkers on the admission scan that accurately identify patients likely to have favorable outcomes with thrombectomy despite sustaining significant delays.
Our aim was to identify patient biomarkers measured at first hospital arrival that would predict that the infarct core at 24 hours after stroke onset would be no larger than 50 ml. The time and core size targets are conservative. Most patients in countries in North America, Europe and Japan are well within a 24-hour drive from a thrombectomy-capable center. The ischemic core target volume of 50 ml was based on the data from the prospective thrombectomy clinical trials that used core volumes of less 50 ml6,9 as inclusion criteria, as well as the observation from the HERMES collaboration11 that revealed that patients with final infarcts of <50 ml after thrombectomy had an ~80% probability of living independently at 3 months even when they presented with severe neurological deficits.
Results
MR imaging was performed up to 3 times in the first day and once more at 2 days post ictus in 38 patients with acute anterior circulation LVO ischemic stroke. No patient received thrombolytic therapy or thrombectomy; 18 were treated with normobaric oxygen and 20 with medical air for 8 hours as part of a randomized clinical trial. Demographic and clinical information is displayed in Table 1. Initial MRI scans (MRI-1) were obtained at a mean time after stroke onset of 5.0 hours (range, 1.6–9.5 hours). Subsequent scans (MRI-2, MRI-3 and MRI-4) were acquired at a mean of 11.7 hours (range, 7–15 hours), 1 day (mean 25.8 hours; range, 22–33 hours), and 2 days (mean 49.7 hours; range, 43–57 hours) following stroke onset.
To illustrate the primary imaging data that was used for this study, Fig. 1 shows selected diffusion and perfusion images from a patient with an occlusion of the M1 segment of the left middle cerebral artery. The patient had an initial core volume (ICV) of <50 ml, as revealed by diffusion weighted imaging (DWI), and a much larger volume of abnormal cerebral perfusion. Notably, despite persistence of arterial occlusion and the large perfusion defect, the ischemic core grew slowly over 48 hours and remained <50 ml.
Ischemic core volume growth rates in patients with ICA, M1 & M2 occlusions
Table 2 displays the average ischemic lesion growth in LVO patients grouped by initial infarct core volume (ICV). The highest average growth occurred during the initial period between stroke onset and the time of the first imaging. In all groups, the second period (~5–12 hours) the average growth of the core was less than 10% of the initial period. The lesion growth during the other periods was also much lower than the initial period for all groups. Infarct core growth is nonlinear:
linear regression resulted in a poor correlation coefficient between lesion volumes and time (R2 < 0.6); conversely, correlation coefficients were high (R2 ≥ 0.96) between lesion volumes and the natural logarithm of time, suggesting logarithmic growth of the ischemic core over 2 days.
Temporal Ischemic core volume changes in patients with ICA and M1 occlusions
Figure 2 displays the changes in ischemic core volumes, grouped by baseline infarct core volumes in the 7 patients with distal ICA and 17 patients with M1 occlusions. Patients with small initial infarct cores (<50 ml) at baseline had slower core growth compared to patients with large baseline cores (>100 ml).
Biomarkers of slow progressors likely to benefit from delayed thrombectomy
Our goal was to identify the biomarkers that identify patients that have such slow growth of infarct cores that they may be amenable to successful thrombectomy up to 1 day after onset. Other researchers, most notably the Pittsburgh group12, have emphasized the importance of slow progressors and their management. Here we adopt a practical definition of slow progressors as patients with an infarct core of appropriate size to be amenable to successful thrombectomy up to 1 day after onset. We used a target ischemic core size of <50 ml at the time of the 1-day scan to identify these patients. This conservative core target of 50 ml was based on the data from the prospective clinical trials that used core volumes of less than 50 ml6,9 as inclusion criteria, as well as the observation from the HERMES collaboration11 that patients with final infarcts of <50 ml after thrombectomy had an ~80% probability of living independently at 3 months irrespective of initial symptom severity.
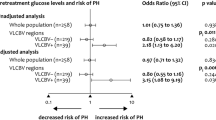
Receiver operator characteristic (ROC) analyses were performed to find the best biomarkers of treatable slow progressors in the 24 patients with ICA and M1 occlusions. We compared key characteristics of our patient group with the control cohorts from the DEFUSE3 and DAWN thrombectomy clinical trials (Table 3). All of the variables are similar to trial control groups with the exception of a lower proportion of female patients in our cohort. Admission variables that were evaluated included NIHSS, admission infarct core volume (ICV), initial infarct core growth rate (IGR), mean transit time volume, Tmax volume, and the diffusion/perfusion mismatch. Figure 3 displays an ROC graph showing the sensitivity versus the false positive rate for predicting the <50 ml target volume at 24 hours for 3 of these variables at the time of presentation. More details of the ROC analyses are shown in Table 4. IGR and ICV were equivalent as the best performing markers with the highest sensitivities and the lowest false positive rates. Both had areas under the curve (AUC) of 0.97 or better as well as 89% sensitivity and 100% specificity for the specific criteria of <4.1 ml/hr (IGR) and <19.9 ml (ICV).
Receiver operator characteristic (ROC) curves of variables predicting ischemic core volumes <50 ml one day after stroke onset. Data is from the 24 patients with an ICA or M1 occlusion identified on CT or MR angiography. For clarity of presentation, the only variables included in this graph ischemic stroke initial growth rate (IGR), NIH Stroke Scale (NIHSS), and diffusion/perfusion mismatch (MM).
Discussion
Patients with potentially severe strokes caused by an occlusion of a major cerebral artery but with a favorable physiology have small infarct cores that grow slowly and are likely to be excellent candidates for thrombectomy despite significant time delays. This finding comes from a cohort of LVO patients who were part of a clinical trial that assessed the value of normobaric oxygen (NBO). While NBO was not shown to be effective13, the study design included multiple MRI scans over a short time and resulted in the unique observations described here. Using a target ischemic core volume of 50 ml at 24 hours, we found that that the best biomarkers of such a favorable physiology are an infarct core growth rate of <4.1 ml/hr or an initial infarct core volume of <19.9 ml.
We chose 50 ml target volume after considering a report from the HERMES collaboration (that combined data from 7 thrombectomy trials) that indicated a 50 ml final infarct volume after thrombectomy results in a high probability of excellent long-term outcomes despite the severity of presenting symptoms11. Our targets are not meant to be prescriptive. Other target volumes may be better. For example, ROC analysis of a 70 ml target revealed 90%/100% sensitivity/specificity for an IGR <5.2 ml. Suitable volumes may be even larger if there is less eloquence of the tissue at risk, and investigations of larger target volumes in patients with lower NIHSS may also be very useful. The assessment at 24 hours is also somewhat arbitrary, and was only used because that is the outer time limit of the successful trials published to date. It is very likely that there will be patients that will benefit from treatment beyond 24 hours.
The reliable identification of LVO slow progressors could greatly expand the use of thrombectomy, and more widely apply the lessons from the recent DAWN9 and DEFUSE-310 thrombectomy trials that treated patients up to 24 hours after onset. The substantial number of slow progressors is largely explained by collateral physiology that typically produces logarithmic growth of the ischemic core as documented in this study. In animal stroke models, the ischemic core also grows in a logarithmic fashion14. Documentation of this type of growth in patients has lacked empirical validation. Wheeler et al.15 suggested logarithmic infarct growth rates in LVO patients using only 2 imaging data points: baseline and 1-week core volumes. Because 4 imaging studies were performed over 2 days, we are able to validate logarithmic-type growth, and explain on our prior observation of apparent ischemic core stability in LVO patients16. We found that most of the core growth occurred within the first 6 hours, with less than 10% further growth over remainder of the first day. Comparison of line fits of core volume with respect to time or the natural logarithm of time favored logarithmic growth.
Our findings beg the question of what proportion of all LVO stroke patients are slow progressors. A review of published studies of patients with LVO that included IGR measurements suggests that a large proportion have growth rates below 4.1 ml/hr and are slow progressors as we have defined them here (Table 5). Taken together, the published evidence from nearly 700 LVO patients suggest that up to half of LVO patients are slow progressors. If this is confirmed, the targeted thrombectomy of slow progressors has the potential to substantially reduce the deaths, severe disabilities and costs due to stroke.
The very high variability of lesion growth in LVO patients is best explained by differences in the collateral circulation17,18,19,20. Slow progressors must have robust collateral circulations that persist for long periods. An important consideration is whether slow progressor LVO patients will still need thrombectomy after a long delay or will spontaneous recanalization make the procedure unnecessary. We found that only 13% of slow progressors with ICA or M1 occlusions had favorable functional outcomes at 3 months, similar to the control cohorts in the DAWN and DEFUSE-3 thrombectomy clinical trials. Not undergoing thrombectomy for such occlusions is clearly hazardous, even in slow progressors, because the arterial occlusion may persist for a long period and the advantageous collateral physiology may diminish and ultimately collapse.
There may be more practical but still effective alternatives to MRI for the identification of LVO patients that are slow progressors. Our ROC analyses (Table 4) hint at several approaches, and there may be others. This is important because patients may present at centers without an available MRI. One alternative may be CT perfusion. We found that the MR perfusion measurement MTT performed well, and it is likely that a CT perfusion MTT measurement would be similarly effective. Additionally, while not tested in this study, perfusion CT estimates of the ischemic core may be effective. A marker that does not rely on imaging is the NIHSS score of <16 in patients with ICA/M1 occlusions: about 90% of slow progressors would be identified, with a false positive rate would be 3 out of 10. A different NIHSS target might be chosen for a higher specificity, but with a lower sensitivity. For example, an NIHSS ≤9 is 100% specific and 63% sensitive. There are likely other effective imaging biomarkers that may derived from CT perfusion, CT angiography, and possibly even noncontrast CT data.
An important strength of this study is that it documented the natural history of ischemic core evolution, without confounders such as thrombolytic use or thrombectomy, which has rarely been done previously20. A possible limitation is the relatively small number of patients that were studied. However, the fact that each patient was scanned multiple times makes our findings robust. A cross sectional study designed to reveal the findings described here would likely require several hundred patients. There is the potential confound of NBO therapy on the NBO-treated arm; however, there was no significant difference between the NBO and room air treated groups on any imaging variable that was measured including outcomes13. In any case, prospective studies are needed to determine the value of imaging biomarkers in making triage decisions for transport of patients for thrombectomy.
In conclusion, ischemic core initial growth rates of <4.1 ml/hr and ischemic core volumes of <19.9 ml are excellent biomarkers for selecting LVO patients that are likely to benefit from transfer to thrombectomy-capable stroke centers despite a substantial delay. These biomarkers are effective because of the characteristic physiological logarithmic growth of the ischemic core. Published accounts suggest that up to half of all LVO stroke patients meet these criteria. Other biomarkers based on CT imaging or NIHSS may be more practical and more widely applicable, although they are somewhat less effective. These observations herald an opportunity to treat many more severe ischemic stroke patients with thrombectomy by transporting patients identified with suitable biomarkers to have a favorable physiology.
Methods
Patient selection and evaluation
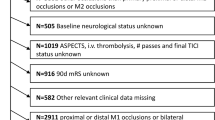
This study was compliant with the Health Insurance Portability and Accountability Act (HIPAA) and was approved by Partners Human Research Committee / Massachusetts General Hospital institutional review board (IRB). The data are from the Normobaric Oxygen Therapy (NBO) in Acute Ischemic Stroke Trial, in which all methods were carried out in accordance with relevant guidelines and regulations and that informed consent was obtained from all participants or, if participants are under 18, from a parent and/or legal guardian. (see http://clinicaltrials.gov/show/NCT00414726 for the complete trial inclusion and exclusion criteria). We included patients who met the following criteria: 1) MR imaging including a DWI scan showing acute ischemic injury; 2) CT angiography (CTA) or MR angiography (MRA) of the head demonstrating a proximal anterior circulation artery occlusion (i.e. terminal ICA and/or proximal MCA (M1 and/or M2 origin); 3) three or more MRIs performed within ~2 days of stroke onset. Of the 60 subjects who underwent serial MRI in the clinical trial, 38 met inclusion criteria for this analysis. For patients whose stroke onset was not witnessed, onset time was estimated as midway between last seen well and first seen with stroke symptoms21. National Institutes of Health Stroke Scale (NIHSS) scores were recorded at all time points, and the modified Rankin Scale (mRS) was recorded 3 months after admission, by investigators blinded to MRI lesions and treatment assignment. A favorable outcome was defined as living independently (mRS score of 2 or less) at 3 months.
Imaging techniques
MRI scans were obtained at admission and repeated after ~12 hours, ~1 day and ~2 days after onset using a clinical 1.5-T (General Electric, Waukesha, Wisconsin) MRI system. Sagittal T1, axial DWI, Fluid-attenuated inversion recovery (FLAIR) T2, and gradient-echo sequences were performed at each time point. In addition, head MRA was obtained with the first three MRI scans.
DWI were acquired using the following median values: field of view of 220 mm, 25 slices, thickness of 5 mm, gap of 1 mm, TR of 5 seconds, TE of 85.3 ms, acquisition matrix 128 × 128, and with b = 0 s/mm2 and b = 1000 s/mm2 in at least 6 diffusion-gradient directions. Isotropic DWI and apparent diffusion coefficient (ADC) maps were calculated using techniques previously described22. FLAIR imaging were performed with a fast-spin echo sequence, with the following median values: 10 s TR, 145 ms TE, 2200 ms TI, 256 × 192 matrix, 220 mm FOV, 25 5 mm slices with 1 mm gap. Gradient-echo T2* imaging median values included TR/TE of 817/25 ms, 20° flip angle, 256 × 192 matrix, 220 mm FOV, 25 5 mm thick slices and 1 mm gap. Perfusion MRI data were acquired using the following median values: field of view of 220 mm, 15 slices, thickness of 5 mm, gap of 1 mm, TR of 1.5 seconds, TE of 40 ms, flip angle 60 degrees, acquisition matrix 128 × 128. 80 data points were acquired using gradient-echo echo planar imaging readout. Mean-transit time (MTT) and Tmax (time at which the tissue response function reached maximum value) perfusion maps were calculated using automated oscillation index regularized deconvolution23.
The 3D time-of-flight MRA consisted of a 7cm-thick slab positioned over the circle of Willis. The median imaging parameters were TR/TE = 36/6.8 ms, 25° flip-angle, 180 mm FOV, 320 × 192 matrix, 101 axial images, 1.4-mm-thick with 0.7-mm overlap. The MRA source images were post-processed into maximum intensity projection images.
CT angiography was performed using multi-detector scanners (GE Medical Systems, Milwaukee, WI) from the vertex to the aortic arch following injection of 65–140 ml of a nonionic contrast agent (Isovue; Bracco Diagnostics, Princeton, NJ) at a rate of 3 to 4 ml/s. The median parameters were 1.25-mm slice thickness, 220 mm reconstruction diameter, 120 kV, and 657 mA.
Image analysis
DWI abnormalities were outlined visually using both the DWI and ADC maps from the same time-point. Tmax lesions were outlined visually with knowledge of DWI and ADC, while MTT abnormalities were outlined visually with knowledge of DWI, ADC and Tmax maps. Analysts blinded to treatment assignment, time-point and clinical information performed all outlines. All outlines were performed using semi-automated, open-source software (Display, Montreal Neurologic Institute, Montreal). Lesion growth was calculated as the Infarct core volume divided by the time in hours from last seen well or from the prior measurement.
Statistical analysis
All values are reported as percentage, mean (standard error), or median. Mann-Whitney, Kruskal-Wallis, ANOVA, or Friedman Test, as appropriate, was used to assess changes in lesion volumes across the 4 time points. Correlation analyses were performed between DWI volumes and time as well as between DWI volumes and natural logarithm of time. Simple and multivariable regression analyses were used to assess the relationship of clinical and imaging variables measured at the time of admission with functional outcomes at 3 months. P-values of less than 0.05 were considered statistically significant. Receiver operator characteristic (ROC) analyses were performed to evaluate the sensitivity and specificity of presenting variables. Analyses described were performed using MedCalc version 14.8.1 and SPSS statistical software (release 20.0 for Windows; SPSS, Chicago, IL). ROC analyses were performed using MedCalc.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gonzalez, R. G. et al. Good outcome rate of 35% in IV-tPA-treated patients with computed tomography angiography confirmed severe anterior circulation occlusive stroke. Stroke; a J. Cereb. circulation 44, 3109–3113, https://doi.org/10.1161/STROKEAHA.113.001938 (2013).
Berkhemer, O. A. et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 372, 11–20, https://doi.org/10.1056/NEJMoa1411587 (2015).
Campbell, B. C. et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N. Engl. J. Med. 372, 1009–1018, https://doi.org/10.1056/NEJMoa1414792 (2015).
Goyal, M. et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N. Engl. J. Med. 372, 1019–1030, https://doi.org/10.1056/NEJMoa1414905 (2015).
Jovin, T. G. et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N. Engl. J. Med. 372, 2296–2306, https://doi.org/10.1056/NEJMoa1503780 (2015).
Saver, J. L. et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N. Engl. J. Med. 372, 2285–2295, https://doi.org/10.1056/NEJMoa1415061 (2015).
Bracard, S. et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 15, 1138–1147, https://doi.org/10.1016/S1474-4422(16)30177-6 (2016).
Muir, K. W. et al. Endovascular therapy for acute ischaemic stroke: the Pragmatic Ischaemic Stroke Thrombectomy Evaluation (PISTE) randomised, controlled trial. J. Neurol. Neurosurg. Psychiatry 88, 38–44, https://doi.org/10.1136/jnnp-2016-314117 (2017).
Nogueira, R. G. et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 378, 11–21, https://doi.org/10.1056/NEJMoa1706442 (2018).
Albers, G. W. et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 378, 708–718, https://doi.org/10.1056/NEJMoa1713973 (2018).
Boers, A. M. M. et al. Association of follow-up infarct volume with functional outcome in acute ischemic stroke: a pooled analysis of seven randomized trials. J. Neurointerv Surg. 10, 1137–1142, https://doi.org/10.1136/neurintsurg-2017-013724 (2018).
Rocha, M. & Jovin, T. G. Fast Versus Slow Progressors of Infarct Growth in Large Vessel Occlusion Stroke: Clinical and Research Implications. Stroke; a J. Cereb. circulation 48, 2621–2627, https://doi.org/10.1161/STROKEAHA.117.017673 (2017).
Singhal, A. & Investigators, P. S. Serial MRI Findings in a Phase 2B Clinical Trial of Normobaric Oxygen Therapy (NBO) in Acute Ischemic Stroke (AIS). Neurol. 80(suppl), S42.001 (2013).
Bardutzky, J. et al. Perfusion and diffusion imaging in acute focal cerebral ischemia: temporal vs. spatial resolution. Brain Res. 1043, 155–162, https://doi.org/10.1016/j.brainres.2005.02.073 (2005).
Wheeler, H. M. et al. The growth rate of early DWI lesions is highly variable and associated with penumbral salvage and clinical outcomes following endovascular reperfusion. Int. J. stroke: Off. J. Int. Stroke Soc. 10, 723–729, https://doi.org/10.1111/ijs.12436 (2015).
Gonzalez, R. G. et al. Stability of large diffusion/perfusion mismatch in anterior circulation strokes for 4 or more hours. BMC Neurol. 10, 13, https://doi.org/10.1186/1471-2377-10-13 (2010).
Christoforidis, G. A., Mohammad, Y., Kehagias, D., Avutu, B. & Slivka, A. P. Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR Am. J. Neuroradiol. 26, 1789–1797, http://www.ajnr.org/content/26/7/1789.long (2005).
Liebeskind, D. S. Collaterals in acute stroke: beyond the clot. Neuroimaging Clin N. Am. 15, 553–573, x, https://doi.org/10.1016/j.nic.2005.08.012 (2005).
Hakimelahi, R. et al. Time and diffusion lesion size in major anterior circulation ischemic strokes. Stroke; a J. Cereb. circulation 45, 2936–2941, https://doi.org/10.1161/STROKEAHA.114.005644 (2014).
Vagal, A. et al. Collateral Clock Is More Important Than Time Clock for Tissue Fate. Stroke; a J. Cereb. circulation 49, 2102–2107, https://doi.org/10.1161/STROKEAHA.118.021484 (2018).
Maas, M. B. & Singhal, A. B. Unwitnessed stroke: impact of different onset times on eligibility into stroke trials. J. stroke Cerebrovasc. diseases: Off. J. Natl Stroke Assoc. 22, 241–243, https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.08.004 (2013).
Sorensen, A. G. et al. Human acute cerebral ischemia: detection of changes in water diffusion anisotropy by using MR imaging. Radiology 212, 785–792, https://doi.org/10.1148/radiology.212.3.r99se24785 (1999).
Copen, W. A. et al. Exposing hidden truncation-related errors in acute stroke perfusion imaging. AJNR Am. J. Neuroradiol. 36, 638–645, https://doi.org/10.3174/ajnr.A4186 (2015).
Olivot, J. M. et al. Impact of Initial Diffusion-Weighted Imaging Lesion Growth Rate on the Success of Endovascular Reperfusion Therapy. Stroke; a J. Cereb. circulation 47, 2305–2310, https://doi.org/10.1161/STROKEAHA.116.013916 (2016).
Desai, S. M., Rocha, M., Jovin, T. G. & Jadhav, A. P. High Variability in Neuronal Loss Time is Brain, Requantified. Stroke; a J. Cereb. circulation 50, 34–37 (2019).
Acknowledgements
The following founding sources are provided by authors, NIH-NINDS R01NS051412 (ABS, GSS, SS, OW), P50NS051343 (ABS, GSS, SS, OW), R21NS077442 (ABS), R21-NS085574 (ABS), U10 -NS086729 (ABS), R01NS059775 (OW), and R01NS063925 (OW). Current address for Dr. Gisele S Silva is Dept. of Neurology, Hospital Israelita Albert Einstein, São Paulo, Brazil.
Author information
Authors and Affiliations
Contributions
A.B.S. and R.G.G. conceived and designed the study. R.G.G. wrote the first draft. G.S.S., J.H., S.S. and O.W. did the analysis. All authors contributed to the interpretation of the results. ABS is integrity guarantor.
Corresponding author
Ethics declarations
Competing interests
Dr. Wu reports personal fees from Penumbra, Inc. All other authors declare no competing interests beyond funding sources delineated in the acknowledgements.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
González, R.G., Silva, G.S., He, J. et al. Identifying Severe Stroke Patients Likely to Benefit From Thrombectomy Despite Delays of up to a Day. Sci Rep 10, 4008 (2020). https://doi.org/10.1038/s41598-020-60933-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60933-3
This article is cited by
-
Low baseline ischemic water uptake is directly related to overestimation of CT perfusion-derived ischemic core volume
Scientific Reports (2022)
-
Development and clinical application of a deep learning model to identify acute infarct on magnetic resonance imaging
Scientific Reports (2022)
-
How can imaging in acute ischemic stroke help us to understand tissue fate in the era of endovascular treatment and cerebroprotection?
Neuroradiology (2022)
-
Late Thrombectomy in Clinical Practice
Clinical Neuroradiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.