Abstract
Human papillomavirus (HPV) infection contributes to most anal cancers and premalignant intraepithelial lesions. This study investigated anal HPV infections and cytological abnormalities among men who have sex with men (MSM). Sociodemographic characteristics and sexual behaviors were collected by using a structured questionnaire. Anal cytological results were examined, and HPV genotyping was performed by the Linear Array HPV Genotyping test. Logistic regression was used to estimate risk factors and their associations with high-risk HPV infection and cytological abnormalities. Among 163 MSM, 101 were seropositive for human immunodeficiency virus (HIV) and 62 were seronegative for HIV. The overall prevalence of HPV was 66.2%. A total of 61.9% and 48.2% of participants had never acquired any of either the quadrivalent or nonavalent vaccine HPV types, respectively. Cytological findings showed 15.3% atypical squamous cells of undetermined significance, 16.6% low-grade squamous intraepithelial lesion, 4.9% atypical squamous cells that cannot exclude high-grade squamous intraepithelial lesion and 17% high-grade squamous intraepithelial lesion. The number of high-risk HPV types was the predominant risk factor for abnormal anal cytology (OR 2.02, 95% CI 1.27–3.24). Infection with high-risk HPV was a significant predictor for cytological abnormality. MSM should be encouraged to obtain the HPV vaccine.
Similar content being viewed by others
Introduction
Human papillomavirus (HPV) is an important cause of sexually transmitted diseases worldwide and is associated with malignant transformations in the squamous epithelium of the anus1. A rising trend in the incidence of anal cancer has been shown in recent years, increasing from 0.8 per 100,000 person-years in 1975 to 1.8 per 100,000 person-years in 2014 in the United States2. The development of anal cancer or pre-cancerous lesions is associated with one’s lifetime number of sexual partners, human immunodeficiency virus (HIV) infection, receptive anal intercourse and anal HPV infection, particularly infection with HPV163,4,5. Moreover, among individuals with anal cancer, nearly 90% of cases are attributable to HPV infection6. A recent meta-analysis also showed that the increased prevalence of HPV is associated with the severity of abnormal anal cytology7.
The incidence of anal cancer among patients with HIV infection is much higher than among the general population (51.4 versus 1.2 per 100,000 person-years)8. HIV infection may attenuate the host’s immune competence, which then worsens the control of anal HPV infections9,10,11. In addition, HIV seropositives have a decreased probability of clearing anal HPV infection and have prolonged anal HPV infections, compared to HIV seronegatives11. The persistent anal HPV infections have been particularly found in high-risk HPV types, which are the predominant risk factors for anal cancer12,13. Thus, HIV infection is considered one of the most important independent risk factors for high-risk anal HPV infection14,15,16,17.
Anal HPV infection is mainly transmitted through anal intercourse, which is usually considered as a major high-risk sexual behavior in men who have sex with men (MSM)18. A previous meta-analysis found that the prevalence of anal HPV infection and epithelial dysplasia among MSM greatly exceeded the prevalence in the cervix among women3. Moreover, among the HIV infected population, the prevalence of any anal HPV type was 96% among MSM, 90% among women and 59% among men who have sex with women, suggesting that the acquisition of anal HPV infection is dependent on sexual behaviors19. However, most of the previous studies were mainly confined to HIV seropositive MSM. Data comparing HPV prevalence among both HIV seropositive and seronegative MSM is limited.
Therefore, this study aimed to evaluate the associations of HPV infection with the risk of abnormal anal dysplasia among MSM. Moreover, the different types or numbers of HPV infections were estimated by stratifying by HIV seronegatives and seropositives.
Results
There were 163 MSM enrolled in this study; 101 were HIV seropositive, and 62 were HIV seronegative. Table 1 shows the baseline characteristics of the study participants. The median age among HIV seropositives was 32 years (interquartile range, IQR, 28–38 years old) compared to 29 years (IQR, 26–34 years old) among HIV seronegatives (p = 0.004). HIV seropositives had a higher percentage of smokers than HIV seronegatives (25.7% versus 8.1%, p = 0.010). Among HIV seropositives, 78.2% had undetectable HIV RNA. In addition, the median CD4+ cell count was 551 cells/µl (IQR, 430–730 cells/µl), and the median CD4+ nadir cell count was 251 cells/µl (IQR, 160–379 cells/µl).
All study participants received anal cytology examinations. Figure 1 shows the anal cytology findings. Among our study participants, there were 86 (52.8%) normal cytological findings, 25 (15.3%) atypical squamous cells of undetermined significance (ASCUS), 27 (16.6%) low-grade squamous intraepithelial lesion (LSIL), 8 (4.9%) had atypical squamous cells that cannot exclude high-grade squamous intraepithelial lesion (ASCH) and 17 (10.4%) high-grade squamous intraepithelial lesion (HSIL). When compared to HIV seronegatives, HIV seropositives had a higher frequency of abnormal anal cytology results (p < 0.001). Compared to HIV seronegatives, the prevalence of LSIL (23.8% versus 4.8%, p = 0.003) and HSIL (15.8% versus 1.6%, p = 0.009) were significantly higher among HIV seropositives.
Table 2 shows the baseline characteristics among participants with normal or abnormal anal cytology. Participants with abnormal anal cytology tended to be older, seropositive for HIV and had more receptive anal intercourse within one year (p < 0.05). In addition, participants with abnormal anal cytology showed a prevalence of 23.5% and 17.6% for HPV16 and HPV18 infection, respectively, compared to 5.6% and 2.8% for HPV16 and HPV18 infections among those with normal anal cytology (p < 0.01).
As shown in Table 3, HIV seropositivity and number of detected high-risk HPV showed significant positive associations with anal intraepithelial neoplasia (p < 0.001). On the other hand, the absence of receptive anal intercourse within one year showed negative associations with abnormal anal cytology (p = 0.034). In the multivariate model, only the number of detected high-risk HPV types was significantly associated with abnormal anal cytology, with an adjusted OR of 2.02 (1.27–3.24).
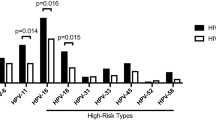
There were 139 (85.3%) participants that had sufficient anal samples for HPV genotyping. Among these men, 81 (58.3%) were HIV seropositive whereas 58 (41.7%) were HIV seronegative. Figure 2 displays the distribution of infection with different HPV types. Among the 37 types of HPV, 66.2% (92/139) of the study participants tested positive for at least one, including 20.9% (29/139) for one HPV type, 13.7% (19/139) for two HPV types, 12.2% (17/139) for three HPV types, 7.2% (10/139) for four HPV types and 12.2% (17/139) for more than four HPV types. Forty-five percent (63/139) had acquired more than one type of anal HPV infection. Multiple HPV infections were more prevalent among HIV seropositives compared to HIV seronegatives (69.1% versus 12.1%, p < 0.001). The overall prevalence of high-risk and low-risk HPV infection was 53.2% (74/139) and 47.5% (66/139), respectively. Compared to HIV seronegatives, HIV seropositives had a significantly higher prevalence of both of high- and low-risk HPV infection types (72.8% versus 25.9%, p < 0.001 for high-risk types and 65.4% versus 22.4%, p < 0.001 for low-risk types). HPV16 (27.0%) and HPV6 (69.7%) were the most common high-risk and low-risk HPV type, respectively. Both were more frequently observed among HIV seropositives than among seronegatives (23.5% versus 1.7%, p < 0.001 for HPV16 and 46.9% versus 13.8%, p < 0.001 for HPV6). We also examined the risk factors associated with high-risk HPV infections (Table 4). In multivariate analyses, HIV seropositivity, having more than five receptive intercourse partners within one year and a history of sexually transmitted diseases within one year were positively associated with high-risk HPV infections (p < 0.05). Similarly, HIV seropositivity was an important associated factor for HPV16 and HPV18 infections with the adjusted OR of 21.3 (2.37–192.40) (p = 0.006) and 13.60 (1.54–120.36) (p = 0.019), respectively. There were 13.7% (19/139) participants without any receptive sexual partner, 56.8% (79/139) participants with one to five receptive sexual partners and 29.5% (41/139) participants with above five receptive sexual partners. There were 43.9% (61/139) participants with a history of sexually transmitted diseases (38.1% with one, 3.6% with two, 0.7% with three, 0.7% with four and 0.7% with five). On the other hand, HIV seropositivity was the only risk factor associated with low-risk HPV infections (OR 7.00, 95% CI 3.07–15.95).
The prevalence of vaccine-preventable HPV types among the 139 MSM is shown in Table 5. There were 86 (61.9%) and 67 (48.2%) participants that had never acquired any of the HPV types included in the quadrivalent or nonavalent HPV vaccine. Among our study participants, none had acquired all four quadrivalent vaccine HPV types or more than four nonavalent vaccine HPV types. There were significantly fewer detected quadrivalent vaccine types in HIV seronegatives than in seropositives (15.5% versus 54.3%, p < 0.001). The same pattern was seen for nonavalent vaccine HPV types (25.9% versus 70.4%, p < 0.001).
Discussion
Anal HPV infection is primarily acquired through sexual exposure, especially via anal intercourse. HPV infection contributes substantially to the risk for anal cancer and squamous intraepithelial lesions. However, there is still limited epidemiological studies investigating the association between anal HPV infection and anal intraepithelial lesions among MSM regardless of their HIV infection status, particularly among the Asian population. The study was conducted in a large medical center which provides substantial healthcare for HIV-seropositives as well as pre- or post-exposure prophylaxis for HIV-seronegatives. Because MSM are considered as a high risk group for HIV infection20,21, the participants enrolled in this study should be representative of most of the MSM in northern Taiwan with considerable generalizability. This study showed that both high- and low-risk anal HPV infections were significantly more prevalent in HIV seropositives than in HIV seronegatives. Individuals with increased numbers of acquired HPV types had increased odds of abnormal anal cytology. However, not many individuals (15.5% of HIV seronegatives and 54.3% of HIV seropositives) were infected with at one or more of the quadrivalent vaccine types (HPV6, 11, 16, 18), suggesting that the HPV vaccine should be advised in these individuals.
We found that the prevalence of anal HPV infection was 85.2% in HIV seropositives and 39.7% in HIV seronegatives. This HPV prevalence is comparable with other studies conducted in Asian countries17,22,23. Among MSM seropositive for HIV, the prevalence of HPV infection was 82.7% in China, 85% in Thailand and 85.3% in Taiwan17,22,23. On the other hand, the prevalence was even higher in Western countries, showing 97% in the United States and 96.3% in Italy24,25. Compared to MSM that were seropositive for HIV, those who were HIV seronegative had consistently lower prevalence of anal HPV infection, which was reported to be 58.5–73.3% and 70% in Asian and Western countries, respectively17,22,23,24,25. Another recent study among MSM of various ethnicities suggested that the estimated global prevalence of anal HPV infection among HIV seropositives and seronegatives was 79% and 47%, respectively26.
In terms of HPV types, the most common types of high-risk genital HPV among HIV seropositive MSM in Taiwan were HPV16 (5.9%), HPV51 (7.9%) and HPV52 (7.2%)20. In Western countries, the most common types was HPV16, with a prevalence of 29.0%27. However, the prevalence of HPV52 was around 10%7,27. Our study found the prevalence of HPV16 and HPV52 to be 23.5% and 17.3%, suggesting that anal HPV52 infection among MSM is more prominent and increasing in Taiwan. A majority of anal cancer was attributed to HPV infections6; nevertheless, the impact of different high-risk HPV types in precancerous lesions on anal cancer has not been clearly identified. The importance of anal HPV52 infection in Taiwan might be worth further investigation.
MSM and increased numbers of acquired high-risk HPV types were found to significantly increase the risk for anal atypical squamous lesions in recent reports19,21,28,29. On the other hand, a meta-analysis suggested that HPV16 infection, but not the number of acquired high-risk HPV types was associated with increased risk for anal cancer7. This may be due to the fact that the study included different populations, such as HIV seropositive male and female patients regardless of their sexual orientation7.
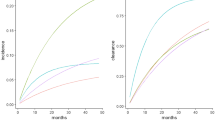
In our study, we found that the prevalence of high-risk HPV infection, including HPV16, HPV31, HPV51, HPV56, HPV58 and HPV68, increased with the severity of abnormal anal cytological findings. The prevalence of high-risk HPV was 35.2% for normal anal cytology, 68.9% for LSIL and ASCUS and 78.3% for ASCH and HISL. These findings are consistent with previous reports7,27. Interestingly, among those with high-risk HPV infection, the numbers of detected high-risk HPV types also increased with the severity of abnormal anal cytology. The median numbers of detected high-risk HPV infections was 0 (IQR, 0–1) for individuals with normal anal cytology, 1 (IQR, 0–2.5) for ASCUS, 1.5 (IQR, 1–3) for LSIL, and 2 (IQR, 1–3) for ASCH and HSIL. Notably, HIV serostatus was also significantly positively associated with HPV infection. HIV seropositives who are immunosuppressed may be more prone to persistent HPV infection, therefore increasing their risk for anal cancer17,20. However, given the multitude of HPV types, the impact of multiple HPV infections on anal dysplasia needs further investigation in large-scale studies.
Most anal cancers or precancerous HSIL among MSM are attributed to HPV infection, especially infection via anal intercourse6,18,28,30,31. Strategies for primary prevention of HPV infection are crucial for the control of anal dysplasia or anal cancer among MSM. Our study found fewer detected quadrivalent or nonavalent vaccine HPV types among HIV seronegatives than among HIV seropositives. Moreover, 61.9% of our study population did not yet acquire any of the HPV types covered in quadrivalent vaccines (HPV6/11/16/18). Thus, this study suggests that there is still a substantial proportion of MSM that may benefit from HPV vaccination. Therefore, increasing awareness of HPV vaccines may be a practical strategy for prevention among MSM, as HPV vaccines have also been suggested for MSM in previous studies21,32.
There are limitations to this study that should be considered. Due to its cross-sectional design, it may be difficult to infer causality, since we could not establish causal temporality. Although we found that HIV seropositivity was associated with acquisition of both low-risk and high-risk HPV types, it was not clear whether HIV infection preceded the HPV infection or not. It is possible that individuals with HIV infection were unable to clear HPV because of impaired immunity. On the other hand, there is also the possibility that individuals with HPV infection may be more sexually active, therefore making them more vulnerable to HIV infections. Lastly, due to the heterogeneity in HPV types, larger sample sizes are needed to further elucidate the influence of specific HPV types or number of anal HPV infections on abnormal anal cytological lesions.
In conclusion, we found a high prevalence of anal dysplasia and HPV infection among MSM regardless of their HIV serostatus. Individuals with increased numbers of HPV infections had stronger associations with anal dysplasia. In addition, there were still a substantial number of MSM who had not yet acquired any of the HPV types that are preventable by vaccines. Therefore, MSM should be advised to receive HPV vaccinations.
Methods
Study design and subjects
This cross-sectional study was conducted in a tertiary medical center, Taipei Veterans General Hospital in northern Taiwan. Males at least 20 years of age who reported having regular sex with men in the past 6 months were enrolled from March, 2015 to July, 2016. The MSM who were HIV seropositive were recruited from outpatient clinics during their regular follow-ups. On the other hand, the MSM who were seronegative for HIV were recruited from voluntary HIV testing clinics. These men were confirmed as HIV-negative by Western blot using the recomline HIV-1 & HIV-2 IgG (Mikrogen GmbH, Neuried, Germany) or HIV viral load examination using cobas HIV-1 (Roche Diagnostics, Mannheim, Germany). Participants with a history of anal cancer or abnormal anal cytology were excluded. All methods in this study were carried out in accordance with the principles of the Declaration of Helsinki. This study was approved by the Institution Review Board of Taipei Veterans General Hospital. All of the study subjects provided informed consent.
Data collection
Study subjects were interviewed at study entry using a structured questionnaire (Supplementary questionnaire). The information collected included demographic characteristics (age, educational levels and income), smoking status, partnership (single or fixed partner), sexual behavior within 1 year, HPV vaccination status and history of sexually transmitted diseases. Clinical data on HIV infection at study entry was obtained by medical chart review with a standardized form. Data on HIV viral load, CD4+ cell count and nadir CD4+ cell count was abstracted.
Anal specimen collection for cytology and HPV genotyping
At the enrollment visit, well-trained health-care professionals sampled anal specimens from all participants using LIBO Specimen Collection and Transport Swab (LIBO Medical Products Inc., New Taipei City, Taiwan) with 5 cm insertion into the anal canal and a slow 360-degree rotating extraction. The swab was then shaken in SurePath liquid-based cytology fluid (Becton, Dickinson and Company, NJ, USA). The anal cytology slides were screened and labeled by cytotechnologists first then interpreted by two cytopathologists separately blinded for HIV or HPV infection status. Slides with discordant interpretations were reviewed again under a multi-head microscope for agreements. The cytological results were interpreted according to the Bethesda System terminology as negative, ASCUS, LSIL, ASCH and HSIL33. The remaining samples were sent for HPV genotyping using the Linear Array HPV Genotyping test (Roche Molecular Systems, Inc., Pleasanton, CA), per the manufacturer’s instructions. Briefly, the target DNA was first amplified using polymerase chain reaction. Then, the nucleic acid was hybridized to identify 37 anal HPV DNA genotypes, including high-risk types (16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68 and 82) and low-risk types (6, 11, 40, 42, 54, 61, 70, 72, 81 and CP6108)34. The Human ß-globin gene was used as a primer for internal control.
Statistical analysis
We compared baseline characteristics between HIV seropositive and seronegative MSM and tested differences in categorical variables using Chi-squared or Fisher’s exact tests, while continuous variables using Student-t or Mann-Whitney U tests. We then used logistic regression models to estimate the associations of baseline characteristics (age, HIV seropositivity, receptive anal intercourse, detectable HPV) with intraepithelial neoplasia. In addition, we also investigated possible risk factors associated with high-risk or low-risk HPV types. Odds ratios (ORs) with 95% confidence intervals (CIs) were obtained from the logistic regressions. Two-tailed tests were used to determine statistical significance and a value of p < 0.05 was considered significant. All statistical analyses were performed using SPSS software version 20 (SPSS INC, Chicago, IL, USA).
References
Beckmann, A. M. et al. Human papillomavirus infection and anal cancer. Int. J. cancer 43, 1042–1049 (1989).
Sclafani, F. & Rao, S. Systemic Therapies for Advanced Squamous Cell Anal Cancer. Curr. Oncol. Rep. 20, 53, https://doi.org/10.1007/s11912-018-0698-6 (2018).
Machalek, D. A. et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol. 13, 487–500, https://doi.org/10.1016/S1470-2045(12)70080-3 (2012).
Islami, F., Ferlay, J., Lortet-Tieulent, J., Bray, F. & Jemal, A. International trends in anal cancer incidence rates. Int. J. Epidemiol. 46, 924–938, https://doi.org/10.1093/ije/dyw276 (2017).
Wilkinson, J. R. et al. The rising incidence of anal cancer in England 1990–2010: a population-based study. Colorectal Dis. 16, O234–239, https://doi.org/10.1111/codi.12553 (2014).
de Martel, C., Plummer, M., Vignat, J. & Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 141, 664–670, https://doi.org/10.1002/ijc.30716 (2017).
Lin, C., Franceschi, S. & Clifford, G. M. Human papillomavirus types from infection to cancer in the anus, according to sex and HIV status: a systematic review and meta-analysis. Lancet Infect. Dis. 18, 198–206, https://doi.org/10.1016/S1473-3099(17)30653-9 (2018).
Patel, P. et al. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992–2003. Ann. Intern. Med. 148, 728–736 (2008).
de Pokomandy, A. et al. Prevalence, clearance, and incidence of anal human papillomavirus infection in HIV-infected men: the HIPVIRG cohort study. J. Infect. Dis. 199, 965–973, https://doi.org/10.1086/597207 (2009).
Sobhani, I. et al. Anal carcinoma: incidence and effect of cumulative infections. AIDS 18, 1561–1569 (2004).
Critchlow, C. W. et al. Effect of HIV infection on the natural history of anal human papillomavirus infection. AIDS 12, 1177–1184 (1998).
Frisch, M. et al. Variants of squamous cell carcinoma of the anal canal and perianal skin and their relation to human papillomaviruses. Cancer Res. 59, 753–757 (1999).
Daling, J. R. et al. Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer 101, 270–280, https://doi.org/10.1002/cncr.20365 (2004).
Somia, I. K. A. et al. Prevalence of and risk factors for anal high-risk HPV among HIV-negative and HIV-positive MSM and transgender women in three countries at South-East Asia. Med. 97, e9898, https://doi.org/10.1097/MD.0000000000009898 (2018).
Nowak, R. G. et al. Prevalence of Anal High-Risk Human Papillomavirus Infections Among HIV-Positive and HIV-Negative Men Who Have Sex With Men in Nigeria. Sex. Transm. Dis. 43, 243–248, https://doi.org/10.1097/OLQ.0000000000000431 (2016).
Muller, E. E. et al. The prevalence of human papillomavirus infections and associated risk factors in men-who-have-sex-with-men in Cape Town, South Africa. BMC Infect. Dis. 16, 440, https://doi.org/10.1186/s12879-016-1706-9 (2016).
Phanuphak, N. et al. Anal human papillomavirus infection among Thai men who have sex with men with and without HIV infection: prevalence, incidence, and persistence. J. Acquir. Immune Defic. Syndr. 63, 472–479, https://doi.org/10.1097/QAI.0b013e3182918a5a (2013).
de Martel, C. et al. Cancers attributable to infections among adults with HIV in the United States. AIDS 29, 2173–2181, https://doi.org/10.1097/QAD.0000000000000808 (2015).
Conley, L. et al. Factors associated with prevalent abnormal anal cytology in a large cohort of HIV-infected adults in the United States. J. Infect. Dis. 202, 1567–1576, https://doi.org/10.1086/656775 (2010).
Cheng, S. H., Chu, F. Y., Lin, Y. S. & Hsueh, Y. M. Influence of age and CD4+ T cell counts on the prevalence of genital human papillomavirus infection among HIV-seropositive men who have sex with men in Taiwan. J. Med. Virol. 84, 1876–1883, https://doi.org/10.1002/jmv.23413 (2012).
Cheng, S. H., Chu, F. Y., Wang, C. C. & Hsueh, Y. M. Screening and risk factors for anal cancer precursors in men infected with HIV in Taiwan. J. Med. Virol. 86, 193–201, https://doi.org/10.1002/jmv.23825 (2014).
Li, X. et al. Anal HPV/HIV co-infection among Men Who Have Sex with Men: a cross-sectional survey from three cities in China. Sci. Rep. 6, 21368, https://doi.org/10.1038/srep21368 (2016).
Lin, C. C. et al. Human papillomavirus prevalence and behavioral risk factors among HIV-infected and HIV-uninfected men who have sex with men in Taiwan. Med. 97, e13201, https://doi.org/10.1097/MD.0000000000013201 (2018).
Nyitray, A. G. et al. Prevalence of and Risk Factors for Anal Human Papillomavirus Infection in a Sample of Young, Predominantly Black Men Who Have Sex With Men, Houston, Texas. J. Infect. Dis. 217, 777–784, https://doi.org/10.1093/infdis/jix617 (2018).
Ucciferri, C. et al. Prevalence of anal, oral, penile and urethral Human Papillomavirus in HIV infected and HIV uninfected men who have sex with men. J. Med. Virol. 90, 358–366, https://doi.org/10.1002/jmv.24943 (2018).
Marra, E., Lin, C. & Clifford, G. M. Type-specific anal human papillomavirus prevalence among men, according to sexual preference and HIV status: a systematic literature review and meta-analysis. J. Infect. Dis., https://doi.org/10.1093/infdis/jiy556 (2018).
Combes, J. D. et al. Prevalence and Risk Factors for Anal Human Papillomavirus Infection in Human Immunodeficiency Virus-Positive Men Who Have Sex with Men. J. Infect. Dis. 217, 1535–1543, https://doi.org/10.1093/infdis/jiy059 (2018).
Palefsky, J. M. et al. High incidence of anal high-grade squamous intra-epithelial lesions among HIV-positive and HIV-negative homosexual and bisexual men. AIDS 12, 495–503 (1998).
Palefsky, J. M. et al. Anal squamous intraepithelial lesions in HIV-positive and HIV-negative homosexual and bisexual men: prevalence and risk factors. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 17, 320–326 (1998).
Silverberg, M. J. et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin. Infect. Dis. 54, 1026–1034, https://doi.org/10.1093/cid/cir1012 (2012).
Diamond, C., Taylor, T. H., Aboumrad, T., Bringman, D. & Anton-Culver, H. Increased incidence of squamous cell anal cancer among men with AIDS in the era of highly active antiretroviral therapy. Sex. Transm. Dis. 32, 314–320 (2005).
King, E. M. et al. Human papillomavirus DNA in men who have sex with men: type-specific prevalence, risk factors and implications for vaccination strategies. Br. J. Cancer 112, 1585–1593, https://doi.org/10.1038/bjc.2015.90 (2015).
Nayar, R. & Wilbur, D. C. The Bethesda system for reporting cervical cytology: definitions, criteria, and explanatory notes. (Springer, (2015).
Coutlee, F. et al. Enhanced detection and typing of human papillomavirus (HPV) DNA in anogenital samples with PGMY primers and the Linear array HPV genotyping test. J. Clin. Microbiol. 44, 1998–2006, https://doi.org/10.1128/JCM.00104-06 (2006).
Acknowledgements
This work was supported by the Ministry of Science and Technology (MOST 107-2314-B-075-071) in Taiwan.
Author information
Authors and Affiliations
Contributions
M.-H.L., P.-F.W., S.W.-W.K. and J.-F.H. were involved in conceiving this study and data acquisition. M.-H.L. and S.W.-W.K. contributed to experiment design and data interpretation. P.-F.W., C.S., S.-J.C., L.-Y.L, S.-S.C. and C.-R.L. performed the experiments and contributed to data analysis. M.-L.H. and P.-F.W. contributed to manuscript drafting. J.-F.H., C.S. and C.-R.L. contributed to the supervision of this investigation. All of the authors critically revised this manuscript for important intellectual content and approved the final version submitted for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, PF., Hang, JF., Strong, C. et al. Anal human papillomavirus and its associations with abnormal anal cytology among men who have sex with men. Sci Rep 10, 3165 (2020). https://doi.org/10.1038/s41598-020-59967-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59967-4
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.