Abstract
Malnutrition is an important risk factor for the development of sarcopenia. Recently, phase angle (PhA) obtained from the bioelectrical impedance analysis is increasingly becoming known as a nutritional status marker and may be considered a good indicator to identify elderly patients at risk of sarcopenia. In this study, we investigated the prevalence of sarcopenia and the relationship between sarcopenia and PhA or body mass index (BMI) as nutritional factors, and evaluated the discrimination performance of these nutritional factors for sarcopenia in 210 kidney transplant recipients. The median age was 55 years and 11.1% had sarcopenia. This prevalence of sarcopenia was lower than previous reports in kidney transplant recipients, maybe because of the differences in sarcopenia definitions and population demographics such as age, sex, race, and comorbidities. Both PhA and BMI were negatively correlated with sarcopenia after adjusting for age, sex, dialysis vintage, time after transplant, presence of diabetes mellitus, hemoglobin, estimated glomerular filtration rate, and the other nutritional factor. The discrimination performance for PhA and BMI had enough power to detect sarcopenia. These results suggest that PhA and BMI can be used in clinical practice to predict sarcopenia in kidney transplant patients.
Similar content being viewed by others
Introduction
Kidney transplantation is the optimal renal replacement therapy for end-stage kidney disease patients, enabling greater longevity and better quality of life compared with dialysis therapy, even for the elderly1,2. Meanwhile, the number of kidney transplants for elderly end-stage kidney disease patients is increasing, with improved graft and patient survivals3,4, consequently contributing to the aging of kidney transplant recipients.
Sarcopenia is a geriatric syndrome characterized by an age-related decline in skeletal muscle mass plus low muscle strength and/or physical performance according to the Asian Working Group for Sarcopenia (AWGS)5. It is associated with adverse clinical outcomes, which include falls, disability, hospital admission, poorer quality of life, and mortality6,7,8,9,10. Primary sarcopenia is caused by aging, while secondary sarcopenia is caused by low activity, malnutrition, and disease (organ failure, inflammatory disease, malignancy, and endocrine disease)11. Although kidney transplant recipients can recover their renal function after transplantation, most of them still have chronic kidney disease (CKD) as well as a gradual decline in renal graft function due to chronic allograft nephropathy. CKD patients are associated with many clinical causes of sarcopenia such as low physical activity, decreased food intake due to anorexia caused by uremic toxins and inflammation, urine and/or dialysate nutrient losses, catabolic and anabolic hormone dysfunction, metabolic acidosis, and chronic inflammation12. Osteoporosis is also a risk factor for sarcopenia, because sarcopenia and osteoporosis share common biological pathways and risk factors13. Therefore, kidney transplant recipients may be high-risk patients for sarcopenia due to risk factors including CKD, aging, and glucocorticoid-induced osteoporosis.
Malnutrition is an important risk factor for the development of sarcopenia11. Several methods are used for the assessment of nutritional status such as body mass index (BMI), which are often used in clinical practice. Recently, phase angle (PhA) is increasingly becoming known as a nutritional status indicator. PhA is a parameter obtained from the bioelectrical impedance analysis (BIA) which has been used as a cell health marker, and is associated with cell membrane integrity, mortality, diet quality, nutritional status, muscle mass, and muscle function14,15,16. Previous reports demonstrated that PhA may be considered a good marker to identify elderly patient at risk of sarcopenia16,17. However, factors associated with sarcopenia in kidney transplant patients remain unknown. The aim of the present study is twofold: firstly, to investigate the prevalence of sarcopenia and the relationship between sarcopenia and PhA or BMI as nutritional factors, and secondly, to evaluate the discrimination performance of these nutritional factors for sarcopenia in kidney transplant recipients.
Results
A total of 210 kidney transplant recipients were enrolled in this study18. The median age was 55 (interquartile range (IQR) 45–66) years, 122 (58%) were male, and 47 (22%) had diabetes mellitus. The median dialysis vintage was 19 (IQR 6–67) months, and the median time after transplant was 85 (IQR 43–135) months. The median BMI and PhA were 22 (IQR 20–25) kg/m2 and 4.8 (4.4–5.3°), respectively. Table 1 shows the demographics, characteristics, and clinical data for the participants, and comparisons between the sarcopenia group (n = 24, 11%) and non-sarcopenia group (n = 186, 89%).
As shown in Fig. 1a, the prevalence of sarcopenia in −39, 40–49, 50–59, 60–69 and 70- age groups were 14.3% (4/28), 8.2% (4/49), 8.5% (4/47), 12.7% (7/55) and 16.1% (5/31), respectively. There was no relationship between age and sarcopenia (p = 0.75). The prevalences of sarcopenia in each CKD stage were the range of 10.8–13.3% regardless of CKD stage as shown in Fig. 1b. Similarly, there was no relationship between CKD stage and sarcopenia (p = 1.00).
Comparisons between the sarcopenia and non-sarcopenia groups
As shown in Table 1, in the sarcopenia group, 16 (67%) were female, which was significantly more than that of the non-sarcopenia group (39%). The median dialysis vintage of the sarcopenia patients was 45 (IQR 14–83) months and longer than that of the non-sarcopenia patients (17 months). The median BMI of the sarcopenia patients was 19 (IQR 17–21) kg/m2, which was significantly lower than that of the non-sarcopenia patients (23 kg/m2). The median PhA of the sarcopenia patients was 4.3 (IQR 3.9–4.6°), which was lower than that of the non-sarcopenia patients (4.8°).
Nutritional factors associated with sarcopenia
The results of multivariable logistic regression analysis evaluating nutritional factors associated with sarcopenia are shown in Table 2. BMI (for IQR difference of 5.2 units, odds ratio (OR) 0.14, 95% confidence interval (CI) 0.05–0.41, p < 0.001) and PhA (for IQR difference of 0.96 units, OR 0.36, 95%CI 0.16–0.82, p = 0.015) were significantly associated with sarcopenia after adjustment for potential confounders. The logistic regression models after penalized were internally validated and the estimated optimism was less than 0.2, indicating that there was no evidence of overfitting.
Figure 2 shows the predicted probability of sarcopenia based on PhA or BMI after adjustment using multivariable logistic regression model. Both PhA and BMI were negatively correlated with sarcopenia.
The predicted probability of sarcopenia based on PhA or BMI. The predicted probability and 95% confidence interval of sarcopenia based on PhA or BMI as nutritional factor after adjustment for age, sex, C-reactive protein, dialysis vintage, time after transplant, diabetes mellitus, hemoglobin, estimated glomerular filtration rate and the other nutritional factor are shown by the black line and the gray band, respectively. PhA, phase angle; BMI, body mass index.
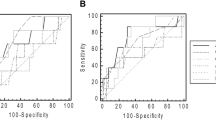
The discrimination performance of nutritional factors for sarcopenia
The area under the bootstrap receiver-operating characteristic curve (AUC-ROC) was 0.83 for BMI and 0.73 for PhA (Table 3). The optimal BMI and PhA cutoff value in order to detect sarcopenia was 20.5 kg/m2 and 4.46° according to the ROC using bootstrap method (Table 3). The area under the precision-recall curve (AUC-PR) was 0.97 for BMI and 0.96 for PhA (Table 3).
Discussion
In this single-center cross-sectional study, we demonstrated that the prevalence of sarcopenia based on the criteria of AWGS was 11.1% and PhA and BMI was negatively correlated with sarcopenia in kidney transplant recipients. PhA ≤ 4.46° and BMI ≤ 20.5 kg/m2 may therefore be used to increase the pretest probability of sarcopenia in kidney transplant recipients.
The present study showed that PhA was negatively correlated with sarcopenia in kidney transplant recipients. PhA is a parameter calculated from reactance and resistance, which are measured by BIA. Reactance expresses the capacity of cell membranes to store energy and is positively correlated with not only the quantity of cells but also the integrity of cell membranes in the body. Resistance expresses the volume of water compartments and is negatively correlated with the quantity of body fluids. Thus, PhA is regarded as a nutritional status indicator15. It is also an excellent predictor of morbidity and mortality in HIV, kidney disease, cancer, and geriatric patients19,20,21,22. Basile C et al. reported that PhA was positively correlated with muscle strength and mass in elderly patients16. Kilic MK et al. demonstrated that PhA was negatively correlated with sarcopenia and the optimal PhA cutoff value to detect sarcopenia was ≤4.55° in the elderly17. This result was almost the same as our results in kidney transplant recipients. However, Dos Reis AS et al. showed that PhA was associated with only handgrip strength (HGS), and not with other sarcopenia components and sarcopenia in kidney transplant recipients23. They divided kidney transplant recipients into two groups according to the first PhA tercile and investigated the association of PhA with sarcopenia and sarcopenia components. The difference between their PhA value (5.8° for women and 6.2° for men) and our optimal PhA cutoff value (4.46°) may explain the difference in the results between the two studies.
Our study showed that BMI was also negatively correlated with sarcopenia in kidney transplant recipients. It is well known that BMI is associated with sarcopenia24,25,26. The sarcopenia diagnostic criteria have components such as skeletal muscle mass index (SMI) and HGS adjusted for BMI27. Landi F et al. reported that BMI higher than 21 kg/m2 had significantly lower odds for sarcopenia than BMI lower than 21 kg/m2 (OR 0.76; 95% CI 0.64–0.90)24. Senior HE et al. demonstrated that BMI was negatively correlated with sarcopenia25. Kim H et al. showed that BMI lower than 21.0 kg/m2 was significantly associated with the development of sarcopenia in a longitudinal study26. Our study revealed that the optimal BMI cutoff value in order to detect sarcopenia was 20.5 kg/m2. Sarcopenia can coexist with obesity, and this state is referred to as sarcopenic obesity28. BMI combined with PhA may therefore be useful for the detection of sarcopenia in kidney transplantation.
Because the accuracy of the ROC may be uncertain due to the imbalanced data, we added the AUC-PR results. Although the criteria of threshold based on the PR curve is ambiguous even if the threshold based on the ROC was used, the precision was 0.9 or higher and recall was 0.7 or higher. Therefore, we believe that it can be well classified using the threshold of the ROC. Moreover, the AUC values for PhA and BMI had enough power to detect sarcopenia. These results suggested that BMI and PhA are beneficial factors in clinical practice to identify sarcopenia patients in kidney transplant recipients.
The percentage of kidney transplant recipients with sarcopenia was 11.1% in this study population, whose median age was 55 (IQR 46–66) years. Several reports have been made on the prevalence of sarcopenia in kidney transplant recipients, ranging from 11.8 to 49.6%22,29,30. Ozkayar N et al. reported that 34 out of 166 (20.5%) kidney transplant recipients, with a mean age of 37.9 ± 11.9 years, had sarcopenia based on only HGS29. Yanishi M et al. reported that 6 out of 51 (11.8%) kidney transplant recipients, with a mean age of 46.2 ± 12.8 years, had sarcopenia based on the AWGS criteria30. Dos Reis AS et al. reported that 64 out of 129 (49.6%) kidney transplant recipients, with a mean age was 47.8 ± 11.8 years, had sarcopenia based on the EWGSOP1 criteria23. This wide range of sarcopenia prevalence kidney transplant recipients may owe to the differences in sarcopenia definitions and population demographics such as age, sex, race, and comorbidities. In another kidney transplant population in which 50.3% had sarcopenia based on the EWGSOP1 criteria, 19%, 39%, 1.6%, and 5.5% were diagnosed as sarcopenia by the EWGSOP2 criteria defined as HGS + SMI, HGS + appendicular skeletal muscle mass (ASM), five times sit to stand (5STS) + SMI, and 5STS + ASM, respectively31. The prevalence of sarcopenia is known to increase with the degree of renal function impairment32,33. Moon SJ et al. reported that 5.6% of their study population, 11,625 subjects aged 40 years or older, had sarcopenia, and according to the stage of CKD, the prevalence of sarcopenia was 4.3%, 6.3%, and 15.4% in CKD 1, 2, and 3–5, respectively33. However, in our kidney transplant patients, the prevalence of sarcopenia was 11.1%, 10.4%, and 11.4% in CKD 1, 2, and 3–5, respectively, and renal graft function was not associated with sarcopenia.
In the present study, we evaluated renal graft function using the CKD-EPI 2012 equation combined with serum creatinine and serum cystatin C. Serum creatinine is affected by muscle mass or protein intake, while serum cystatin C is affected by inflammation or immunosuppression therapy. eGFR (estimated glomerular filtration rate) calculated using the CKD-EPI 2012 equation combined with creatinine and cystatin C may therefore be appropriate for the assessment of renal function in the elderly as well as in kidney transplant recipients34,35,36.
After adjustment for potential confounders, nutritional markers were associated with sarcopenia, while age and renal graft function were not in our kidney transplant patients. These results suggest that the impact of nutrition on sarcopenia is greater than that of aging or renal dysfunction in kidney transplant recipients. A low protein diet is recommended for kidney transplant recipients, because high protein intake may lead to damage to their renal grafts. However, an excessive low protein diet may lead to a decrease in the quality of life and to mortality in kidney transplant recipients, especially the elderly, so that it might be necessary to reconsider nutritional therapies for kidney transplant recipients.
Our study has several limitations. First, we could not reveal a causal relationship between sarcopenia and nutritional markers because of the cross-sectional design of our study. Second, this study was performed in a single center in Japan, and these results should not be generalized to subjects of other races or nationalities. Third, we evaluated muscle mass without CT and MRI, which are the gold standards.
In conclusion, our results showed that PhA and BMI may be beneficial factors in clinical practice to identify sarcopenia in kidney transplant recipients.
Patients and Methods
Study design and participants
A single-center cross-sectional study was conducted at Osaka City University Hospital between October 2018 and February 2019. The inclusion criteria were (1) clinical stability (defined as no hospitalization needed since the last check-up or within a month) and (2) more than a year post-transplant, while the exclusion criteria were (1) refusal to participate in this study, (2) missing data on diagnostic criteria for sarcopenia, and (3) not first kidney transplant (4) abnormal hydration status, which is <69 or >75% of total body water/lean mass. This study was approved by the Ethics Committee of Osaka City University Graduate School of Medicine (No. 3859). All patients provided written informed consent for participation in the study, and all the procedures were in accordance with the Helsinki Declaration of 2000.
Sarcopenia diagnosis
Sarcopenia was diagnosed by low muscle mass and either low muscle strength or low physical performance according to the AWGS criteria5. Low muscle strength was defined as HGS <26 kg for males and <18 kg for females. Low muscle mass was defined as SMI <7.0 kg/m2 for males and <5.7 kg/m2 for females. Low functional capacity was defined as gait speed <0.8 m/s.
Muscle strength and physical performance measurements
Gait speed was measured by the time to walk 10 m, and the average time of two trials was taken. HGS was measured on both hands alternately twice, with a Smedley hand-held dynamometer at a standing position with elbow in full extension, and the best of the two attempts were recorded. All gait speed and HGS were measured by the same single observer.
Bioimpedance measurements
The ASM, total body water, lean mass, and PhA were measured by BIA using the InBody S10 (InBody Co, Ltd., Seoul, Korea), which has a tetrapolar eight-point tactile electrode system and six different frequencies (1 kHz, 5 kHz, 50 kHz, 250 kHz, 500 kHz, 1000 kHz). Measurements were taken while the patients laid flat on a bed in the supine position with their limbs away from the body midline. Reactance and resistance were measured at 50 kHz. PhA was calculated according to the following formula: PhA [°] = arctangent (reactance/resistance)*(180/π)37. SMI was calculated as ASM in kilograms divided by height in meters squared.
Biochemical measurements
Blood samples were drawn in the morning after overnight fasting. Hemoglobin, C-reactive protein, fasting blood glucose, hemoglobin, HbA1c, serum creatinine, serum cystatin C were measured using the JCA-BM6070 (JEOL Ltd., Tokyo, Japan) automatic biochemical analyzer.
Data collection
The demographics (age, sex), characteristics (dialysis vintage, time after transplant, transplantation type, presence of diabetes mellitus) and clinical data (hemoglobin, C-reactive protein, fasting blood glucose, hemoglobin, HbA1c, serum creatinine, serum cystatin C) were collected from electronic medical records. Body weight and height were measured wearing light clothing and without shoes, and BMI was calculated as weight in kilograms divided by height in meters squared. eGFR was calculated using the CKD-EPI 2012 equation combined with serum creatinine and serum cystatin C34.
Statistical analysis
Categorical variables were expressed as count and percentage, and continuous variables were expressed as median and IQR. Categorical variables were compared using chi-squared test, and continuous variables were compared using Mann-Whitney U-test.
For primary analysis, to assess the relationship between sarcopenia and PhA or BMI as nutritional factors, the multivariable logistic regression model was used with adjustment for age, sex, C-reactive protein, dialysis vintage, time after transplant, diabetes mellitus, hemoglobin, eGFR and the other nutritional factor (for sarcopenia, non-sarcopenia = 0 and sarcopenia = 1). To avoid overfitting, the regression model was limited to two nutritional factors and 8 covariates, and penalized maximum likelihood estimation was performed to allow shrinkage for effect of each variable. The selection of covariates was made a priori according to expert opinion and previous literature, namely age37,38, sex38, C-reactive protein39,40, diabetes mellitus41,42, dialysis vintage42, time after transplant, hemoglobin43, and eGFR31. Long-term use of immunosuppressive agents including steroids and calcineurin inhibitors has a negative effect on the muscles of kidney transplant recipients44,45. Optimism assesses the magnitude of overfitting of logistic regression model (a value less than 0.2 is considered as good), and was calculated using C-statistics by 150 times of bootstrap sampling.
For secondary analysis, the discrimination performance for sarcopenia was assessed by AUC-ROC and AUC-PR. We reported bootstrap bias-corrected AUC as the validated measure of the predictive performance of each nutritional factor. The sensitivity and specificity were calculated by using the best cut-off score for the nutritional factors with the Youden index for the ROC. The statistical analyses were performed using R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided p < 0.05 was considered statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are available in the figshare repository https://doi.org/10.6084/m9.figshare.7992851.
References
Laupacis, A. et al. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 50, 235–242 (1996).
Wolfe, R. A. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 341, 1725–1730 (1999).
Matas, A. J. et al. OPTN/SRTR 2013 Annual Data Report: kidney. Am. J. Transplant. 15(Suppl 2), 1–34 (2015).
Yagisawa, T., Mieno, M., Yoshimura, N., Yuzawa, K. & Takahara, S. Current status of kidney transplantation in Japan in 2015: the data of the Kidney Transplant Registry Committee, Japanese Society for Clinical Renal Transplantation and the Japan Society for Transplantation. Ren. Replace. Ther. 2, 68 (2016).
Chen, L. K. et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 15, 95–101 (2014).
Landi, F. et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin. Nutrition. 31, 652–658 (2012).
da Silva Alexandre, T., de Oliveira Duarte, Y. A., Ferreira Santos, J. L., Wong, R. & Lebrão, M. L. Sarcopenia according to the european working group on sarcopenia in older people (EWGSOP) versus Dynapenia as a risk factor for disability in the elderly. J. Nutr. Health Aging. 18, 547–553 (2014).
Woo, J., Leung, J. & Morley, J. E. Defining sarcopenia in terms of incident adverse outcomes. J. Am. Med. Dir. Assoc. 16, 247–252 (2015).
Beaudart, C. et al. Quality of life and physical components linked to sarcopenia: The SarcoPhAge study. Exp. Gerontol. 69, 103–110 (2015).
Landi, F. et al. Sarcopenia and mortality among older nursing home residents. J. Am. Med. Dir. Assoc. 13, 121–126 (2012).
Cruz-Jentoft, A. J. et al. European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 39, 412–423 (2010).
Kim, J. C., Kalantar-Zadeh, K. & Kopple, J. D. Frailty and protein-energy wasting in elderly patients with end stage kidney disease. J. Am. Soc. Nephrol. 24, 337–351 (2013).
Reginster, J. Y., Beaudart, C., Buckinx, F. & Bruyère, O. Osteoporosis and sarcopenia: two diseases or one? Curr. Opin. Clin. Nutr. Metab. Care. 19, 31–36 (2016).
Chertow, G. M., Lazarus, J. M., Lew, N. L., Ma, L. & Lowrie, E. G. Bioimpedance norms for the hemodialysis population. Kidney Int.; (1997 Dec).(6):1617–1621 (1997 Dec).
Lukaski, H. C. Evolution of bioimpedance: a circuitous journey from estimation of physiological function to assessment of body composition and a return to clinical research. Eur. J. Clin. Nutr. 67, S2–9 (2013).
Basile, C. et al. Phase angle as bioelectrical marker to identify elderly patients at risk of sarcopenia. Exp. Gerontol. 58, 43–46 (2014).
Kilic, M. K. et al. Association of Bioelectrical Impedance Analysis-Derived Phase Angle and Sarcopenia in Older Adults. Nutr. Clin. Pract. 32, 103–109 (2017).
Kosoku A. et al. Sarcopenia characteristics, bioimpedance measurements and clinical data on kidney transplant recipients. figshare. Dataset. https://doi.org/10.6084/m9.figshare.8799158 (2019).
Ott, M. et al. Bioelectrical impedance analysis as a predictor of survival in patients with human immunodeficiency virus infection. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 9, 20–25 (1995).
Chertow, G. M., Jacobs, D. O., Lazarus, J. M., Lew, N. L. & Lowrie, E. G. Phase angle predicts survival in hemodialysis patients. J. Ren. Nutr. 7, 204–207 (1997).
Gupta, D. et al. Bioelectrical impedance phase angle as a prognostic indicator in breast cancer. BMC Cancer. 8, 249 (2008).
Wirth, R., Volkert, D., Rösler, A., Sieber, C. C. & Bauer, J. M. Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Arch. Gerontol. Geriatr. 51, 290–294 (2010).
Dos Reis, A. S., Santos, H. O., Limirio, L. S. & de Oliveira, E. P. Phase Angle Is Associated With Handgrip Strength but Not With Sarcopenia in Kidney Transplantation Patients. J. Ren. Nutr. 29, 196–204 (2019).
Landi, F. et al. Prevalence and risk factors of sarcopenia among nursing home older residents. J. Gerontol. A Biol. Sci. Med. Sci. 67, 48–55 (2012).
Senior, H. E., Henwood, T. R., Beller, E. M., Mitchell, G. K. & Keogh, J. W. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 82, 418–423 (2015).
Kim, H. et al. Incidence and predictors of sarcopenia onset in community-dwelling elderly Japanese women: 4-year follow-up study. J. Am. Med. Dir. Assoc. 16(85), e1–8 (2015).
Studenski, S. A. et al. The FNIH sarcopenia project: rationale, study description, conference recommendations,. Final. estimates. J. Gerontol. A Biol. Sci. Med. Sci. 69, 547–558 (2014).
Stenholm, S. et al. Sarcopenic obesity: definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care. 11, 693–700 (2008).
Ozkayar, N. et al. Evaluation of sarcopenia in renal transplant recipients. Nephrourol. Mon. 6, e20055 (2004).
Yanishi, M. et al. Factors Associated With the Development of Sarcopenia in Kidney Transplant Recipients. Transpl. Proc. 49, 288–292 (2017).
Limirio, L. S., Santos, H. O., Dos Reis, A. S. & de Oliveira, E. P. (Dis) Agreement between the first and the recent European consensus on definition and diagnosis for sarcopenia in kidney transplant patients. Eur J Clin Nutr. In press, https://doi.org/10.1038/s41430-019-0535-5.
Foley, R. N., Wang, C., Ishani, A., Collins, A. J. & Murray, A. M. Kidney function and sarcopenia in the United States general population: NHANES III. Am. J. Nephrol. 27, 279–286 (2007).
Moon, S. J., Kim, T. H., Yoon, S. Y., Chung, J. H. & Hwang, H. J. Relationship between Stage of Chronic Kidney Disease and Sarcopenia in Korean Aged 40 Years and Older Using the Korea National Health and Nutrition Examination Surveys (KNHANES IV-2, 3, and V-1, 2), 2008-2011. PLoS One. 10, e0130740 (2015).
Inker, L. A. et al. CKD-EPI Investigators. Estimating glomerular filtration rate from serum creatinine and cystatin C. N. Engl. J. Med. 367, 20–29 (2012).
Masson, I. et al. GFR estimation using standardized cystatin C in kidney transplant recipients. Am. J. Kidney Dis. 61, 279–284 (2013).
Fan, L. et al. Comparing GFR Estimating Equations Using Cystatin C and Creatinine in Elderly Individuals. J. Am. Soc. Nephrol. 26, 1982–1989 (2015).
Norman, K., Stobäus, N., Pirlich, M. & Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis-clinical relevance and applicability of impedance parameters. Clin. Nutr. 31, 854–861 (2012).
Kim, H. et al. Sarcopenia: Prevalence and associated factors based on different suggested definitions in community-dwelling older adults. Geriatr. Gerontol. Int. 16, 110–122 (2016).
Mochizuki, T., Yano, K., Ikari, K. & Okazaki, K. Sarcopenia-associated factors in Japanese patients with rheumatoid arthritis: A cross-sectional study. Geriatr. Gerontol. Int. 19, 907–912 (2019).
Bano, G. et al. Inflammation and sarcopenia: A systematic review and meta-analysis. Maturitas. 96, 10–15 (2017).
Han, P. et al. Prevalence and Factors Associated With Sarcopenia in Suburb-dwelling Older Chinese Using the Asian Working Group for Sarcopenia Definition. J. Gerontol. A Biol. Sci. Med. Sci. 71, 529–535 (2016).
Ren, H., Gong, D., Jia, F., Xu, B. & Liu, Z. Sarcopenia in patients undergoing maintenance hemodialysis: incidence rate, risk factors and its effect on survival risk. Ren. Fail. 38, 364–371 (2016).
Hirani, V. et al. Low Hemoglobin Concentrations Are Associated With Sarcopenia, Physical Performance, and Disability in Older Australian Men in Cross-sectional and Longitudinal Analysis: The Concord Health and Ageing in Men Project. J. Gerontol. A Biol. Sci. Med. Sci. 71, 1667–1675 (2016).
Dasarathy, S. Posttransplant Sarcopenia: An Underrecognized Early Consequence of Liver Transplantation. Dig. Dis. Sci. 58, 3103–3111 (2013).
Klein, G. L. The effect of glucocorticoids on bone and muscle. Osteoporos. Sarcopenia. 1, 39–45 (2015).
Acknowledgements
The authors appreciate the support of Kuwabara Nobuyuki and Norihiko Kumada at Osaka City University Hospital, for their data collection help.
Author information
Authors and Affiliations
Contributions
A.K. and J.U. designed the study, and A.K. wrote the initial draft of the manuscript. A.K. and T.I. contributed to analysis and interpretation of data, and assisted in the preparation of the manuscript. All other authors have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kosoku, A., Uchida, J., Nishide, S. et al. Association of sarcopenia with phase angle and body mass index in kidney transplant recipients. Sci Rep 10, 266 (2020). https://doi.org/10.1038/s41598-019-57195-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-57195-z
This article is cited by
-
Association of phase angle with sarcopenia and muscle function in patients with COPD: a case-control study
BMC Pulmonary Medicine (2024)
-
Association of phase angle with sarcopenia in chronic musculoskeletal pain patients: a retrospective study
Journal of Orthopaedic Surgery and Research (2023)
-
Frailty and sarcopenia in older kidney transplant recipients: a cross-sectional study
European Geriatric Medicine (2023)
-
A Combined Assessment Method of Phase Angle and Skeletal Muscle Index to Better Predict Functional Recovery after Acute Stroke
The Journal of nutrition, health and aging (2022)
-
Neutrophil–lymphocyte Ratio and C-Reactive Protein Levels are not Associated with Strength, Muscle Mass, and Functional Capacity in Kidney Transplant Patients
Inflammation (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.