Abstract
We investigate changes in brain function before and after carpal tunnel release. Magnetoencephalography (MEG), during which we recorded somatosensory evoked cortical magnetic fields (SEFs), and a clinical evaluation were performed before surgery and 6 months after. The distance on the vertical axis between the equivalent current dipoles (ECDs) for the first and third digits before surgery was significantly less than after surgery. There were no significant differences in values between the control participant and patients after surgery. In terms of distal motor latency, there was a negative correlation with the distance. The recovery function of the root mean square (RMS) before surgery for the N20m was less suppressed at 10 ms of ISI in patients, compared to controls. There were no significant differences in the RMS values for patients before and after surgery. Our results indicate that treating peripheral nerve lesions, such as in carpal tunnel release, positively modifies brain function.
Similar content being viewed by others
Introduction
Brain plasticity changes, which can be adaptive or maladaptive, occur following peripheral and central nerve lesions. These changes have been shown in patients with carpal tunnel syndrome (CTS), one of the most common peripheral neuropathies. Research into the plastic changes associated with CTS has primarily used functional magnetic resonance imaging (fMRI)1,2,3,4 and magnetoencephalography (MEG)5,6. Dhond et al.7 have reported that fMRI and MEG results are novel markers of neuroplasticity in CTS and can be used to study central changes that may occur following clinical interventions.
Both morphological and functional brain changes have revealed brain plasticity. In a study of CTS patients, gray matter volume was significantly reduced in the contralesional somatosensory hand area, pulvinar, and frontal pole. In the contralesional somatosensory cortex, it was correlated with median nerve conduction velocity (NCV)1. In addition, cortical thickness in the precentral and postcentral gyri (somatosensory and primary motor hand area) contralateral to the more affected hand was significantly reduced in a CTS-paresthesia subgroup compared with that in a CTS-pain subgroup3.
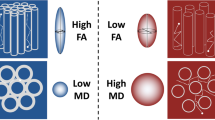
Functionally, a reduced second/third interdigit cortical separation distance in the contralateral primary somatosensory cortex is associated with worse symptomatology (particularly paresthesia), reduced fine motor skill performance, and poorer sensory discrimination accuracy for median nerve innervated digits. Furthermore, primary somatosensory cortex neuroplasticity for median nerve innervated digits in CTS is maladaptive and underlies the functional deficits seen in these patients2.
We previously studied patients with CTS using MEG, which revealed functional changes of neural activity in the somatosensory cortex5. Distances on the vertical axis between the equivalent current dipoles for the stimulation of the first and third digits were shorter in patients than in controls5, in line with a previous report2. In addition, the N20m component from the paired median nerve stimulation recovered earlier in CTS patients than in control participants, suggesting that CTS induced disinhibition or hypersensitivity in the primary somatosensory cortex. The local lesion at the peripheral nerve can be treated by carpal tunnel release. We questioned whether the central nervous system responses that had been modified by a peripheral nerve lesion could be remodified by the treatment. Few studies have measured the brain changes in CTS patients before and after treatment. Therefore, the changes in brain plasticity following carpal tunnel release remain unknown. To address this, we conducted a survey 6 months after carpal tunnel release and investigated the changes in brain function before and after treatment.
Methods
The study was approved by the Ethical Review Committee of Nagoya University. The methods utilized conformed to the applicable regulations and guidelines, and informed consent was obtained from all participants.
Patients and control participants
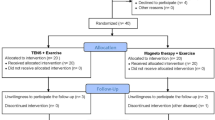
The effect of carpal tunnel release was investigated in 12 hands (6 right, 6 left) of 10 patients (7 female, 3 male; 66.8 ± 11.3 years average age). The control group was compromised of 21 age-matched healthy participants (9 female, 12 male; 68.0 ± 7.4 years mean age).
Two individuals in the experimental group suffered from bilateral CTS. As is common practice, both initially underwent carpal tunnel release on the more severe side only. After the conclusion of the investigation of the initial surgery, the condition of their contralateral hand worsened such that it too was operated on. Therefore, the effect of carpal tunnel release was investigated independently on each side in these two patients.
The basis of CTS diagnosis was a history of dysesthesias at points around the median nerve, as reported previously8. Nerve conduction studies were performed to confirm the diagnosis. Patients whose CTS symptoms were related to trauma, dialysis, rheumatoid arthritis, or neurological disorders were excluded.
For the clinical assessment, we evaluated grip and pinch strength and administered the Hand10, a patient-rated outcome measure to assess hand disorders, just before and 6 months after surgery9,10,11,12. Somatosensory evoked cortical magnetic fields (SEFs) were recorded by MEG on the same schedule.
Magnetoencephalography recording
Signals (0.5 s duration) were recorded using a conventional MEG system as described in our previous study5. A 5,000 Hz sampling frequency and an initial bandpass filter (0.3–2,000 Hz range) were employed. Seventy-five channels of signal data from the hemisphere contralateral to the stimulated nerve were used for recovery function and source analysis.
SEFs following finger stimulation
SEF recordings were taken during stimulation of the first and third digits on the affected hand of CTS patients and on the right hand of control participants. The stimuli were 2 Hz, 0.2 ms square wave pulses randomly delivered to either finger. The intensity was 1.5 times the sensory threshold of each individual5.
Source estimation
To estimate the dipole locations of the initial cortical component of the SEF following stimulation, a single current dipole model was used13. Using SEF signals from each hemisphere, equivalent current dipoles (ECDs) with a goodness-of-fit value of 75% were calculated. A three-dimensional plane was used to express the ECD location and calculate the distance between the locations of the two digits on the vertical (z) axis. The midpoint between the pre-auricular points marked the origin of the coordinate system. The x-axis joined the origin to the nasion, with the nasion in the positive direction. The positive y-axis extended from the origin through the left side, and the positive z-axis extended from the origin through the vertex.
Recovery function
The assessment of the SEF recovery function proceeded as described in previous studies14,15,16. Single or double pulses with interstimulus intervals (ISIs) of 10, 40, 80, or 200 ms were delivered randomly in 0.2 ms durations to the median nerve at the wrist5.
To analyze the recovery function, the SEF evoked by the second of the double stimuli was obtained by subtracting the signal obtained from the single stimulation from that of the double stimulation14,15,16. The root mean square (RMS) of the magnetic field obtained from each hemisphere, as a global field power, was calculated. The N20m component was identified within the latency window of 18–24 ms after stimulation.
Statistical analysis
The distance between the ECD locations was compared using the Tukey-Kramer test. Standardized RMS values were expressed as a function of the ISI. RMS values were also compared in all ISI conditions using the Tukey-Kramer test. Differences were considered statistically significant for p < 0.05.
Results
Clinical outcome
All patients showed an improvement in clinical symptoms after the surgery. The mean Hand10 score significantly improved from 33.7 to 13.7. There were no significant differences in grip strength and pinch power before and after treatment (mean grip strength: 21.4 kg before vs. 19.9 kg after; mean pinch power: 6.3 kg before vs. 6.5 kg after). In this analysis, correlations between MEG measurements and Hand10, grip, or pinch strength were not found.
Source localization of the digits
To localize the representation of the first and third digits, we calculated ECDs using the N20m elicited on stimulation. In the distance between the first and third digits, there were too many patients in whom sensory nerve conduction could not be detected before the operation, yielding no significant differences. However, in terms of distal motor latency before operation, there was a negative correlation with the conduction distance between the first and third digits (−0.46 correlation coefficient; Fig. 1), suggesting that the conduction distance becomes shorter with increasing severity of CTS17.
The distance on the vertical axis between the ECDs for the first and third digits of patients was significantly greater after surgery, compared to that before surgery. Further, there were no significant differences in this value between the patients after surgery and the control participants (4.1 ± 6.0 cm before, 10.9 ± 6.5 cm after, 11.2 ± 3.1 cm controls; Fig. 2).
Distance on the vertical axis (z-axis, from the midpoint between pre-auricular points and vertex) between the equivalent current dipoles (ECDs) for the first and third digits in patients before (Pre) and 6 months after (6 M) operative treatment and control participants (Cont). Each dot indicates a value for each participant. Mean values of the distance were smaller in the patients before operation than those after operation and controls (*p < 0.05, Tukey-Kramer test). The zero value indicates the ECD location of the first digit on the z-axis.
Recovery function
We divided the patients into two groups based on whether sensory nerve conduction was detectable before the operation. In terms of recovery function (10 ms), the mean was 0.46 in the undetectable group (7 hands) and 0.73 in the measurable moderate severity group (5 hands), with the latter being significantly higher (p < 0.05). The mean VAS scores in these two groups were 31.9 and 66.8, respectively (p < 0.05), indicating more severe pain in the moderate severity group.
The RMS before surgery for the N20m was less suppressed at 10 ms of ISI in patients, when compared with that in controls (p < 0.05, Figs. 3 and 4). There were no significant differences in the RMS values for patients before and after surgery (Fig. 3). The values were also not significantly different between patients and control participants concerning the hand contralateral to that operated on (Fig. 4).
Recovery function of the relative value of the root mean square (RMS) for the N20m following median nerve stimulation at various inter-stimulus intervals (ISIs) on the side operated on in the patients. The RMS value following single stimulation (Single) is expressed as 1.0. The RMSs before (Pre) and 6 months after (6 M) operative treatment in the affected hands and the right hand in the controls (Cont). The mean RMS value at 10 ms of ISI was less suppressed in the Pre condition, compared to the control (*p < 0.05, Tukey-Kramer test).
Recovery function of the relative value of the root mean square (RMS) for the N20m following median nerve stimulation at various inter-stimulus intervals (ISIs) on the side not operated on in the patients. The RMS value following single stimulation (Single) is expressed as 1.0. The RMSs before (Pre) and 6 months after (6 M) and the right hand in the controls (Cont). The mean RMS value at 10 ms of ISI was less suppressed in the Pre and 6 M conditions, compared to the control (*p < 0.05, Tukey-Kramer test).
Discussion
Many technologies are available to assess brain function including fMRI, positron emission tomography, near-infrared spectroscopy, electroencephalography, and MEG. A particular strength of MEG is that it allows measurement of the magnetic field of the brain caused by the electrical activity of nerves without being affected by extra-cerebral tissues18. We previously reported neural function in the brain using a MEG system to elucidate the pathology of intractable pain and nerve disorders5,16. CTS causes dysfunction at the peripheral nerve; however, neural signals modified at the peripheral nerve lesion can affect the neural response in the brain5,19. In this study, we conducted MEG measurement in patients with CTS before and after surgical treatment to assess any remodeling of neural activity in the brain.
All patients responded well to treatment as evidenced by their Hand10 scores. In comparison to the preoperative distance between ECDs for the first and third digits, the postoperative distance increased, approaching those of health individuals. The increment of the distance between receptive fields for the two fingers indicated that neural activity for spatial discrimination between the fingers after the treatment functionally improved, reaching a level similar to that seen in the controls. On the other hand, the recovery function, which reflects disinhibition or hypersensitivity of the central nervous system following the median nerve stimulation, was not significantly changed by surgical treatment, although a slight shift of the value to the control was observed.
We found two series of neural activities modified by CTS. These plastic changes in the receptive field and recovery function could be interpreted as adaptive or maladaptive. Changes in the receptive fields for the first and third fingers were remodified by 6 months after treatment with improvement of CTS symptoms. The evidence suggests that the change in the receptive fields modified by CTS was maladaptive plasticity in the brain that resulted in poor spatial discrimination between fingers.
The recovery function was not correlated with the clinical symptoms 6 months after surgical treatment. One interpretation might be that the inhibitory/disinhibitory neural activity modified by CTS took longer than 6 months for remodification. Alternatively, disinhibitory neural activity may have been a compensatory adaptive plastic change amplifying neural signals from the peripheral nerve affected by CTS. The disinhibition might have remained until functional repair of the peripheral nerve was completed.
We examined the results of NCV and MEG in this study. Our findings suggested that the conduction distance between the first and third digits might have become shorter with increasing severity of CTS. In other words, the more severe the condition, the more diminished the sensation becomes, which is consistent with the observations in actual clinical practice. More interestingly, there was a larger difference in the recovery function at 10 ms between the moderate severity group and the control group, compared to the difference between the severe group and the control group. This may be because, in the moderate severity group, remodeling in the brain aims to increase the sensitivity through a disinhibitory action on the recovery function and adaptive change; this may be less likely to occur in severe cases, where the patients can no longer feel pain.
Several studies on brain function changes after other orthopedic surgeries have been performed20,21,22. Changes in the brain following contralateral cervical 7 nerve transfer for brachial plexus injury have been reported21,22. Furthermore, transhemispheric transposition of activated brain cortices is associated with the recovery of motor and sensory functions in ipsilesional upper limbs in patients with contralateral cervical 7 nerve transfer21. Resting-state MRI showed that interhemispheric functional connectivity of the primary motor cortex increased and the inter-hemispheric functional connectivity between the supplementary motor areas reduced bilaterally in patients with CTS22. However, these studies reveal brain function after treatment.
Although there are several studies comparing brain function before and after acupuncture treatment for CTS23,24,25, the longitudinal changes associated with surgical treatment of CTS are unknown. Ma et al.6 used task-dependent fMRI and electromyography assessment before and after surgery to assess CTS changes. They found that CTS patients had decreased activation in the postcentral gyrus, inferior frontal lobe, superior frontal lobe, and parahippocampal gyrus 6 months after surgery. In this study, we used MEG to evaluate plasticity changes before and after carpal tunnel release surgery. We found indexes of brain plasticity change that remained up to 6 months after surgery. To use these MEG and fMRI indexes6, we suggest that a new method of treatment evaluation should be developed. Our results show the importance of a neurorehabilitation-based approach to treat not only the diseased site but also the central nervous system. In the future, we plan to evaluate clinical improvement using brain functional analysis.
There are some limitations in this study. First, we had a small number of participants. Similar numbers have been used in previous studies, however, and were considered statistically acceptable. Second, we evaluated changes in plasticity 6 months before and after surgery. This evaluation period matches a previous study6; although recovery of function may have been different had we evaluated other periods. Third, the correlation of Hand10 scores, grip strength, and pinch strength with MEG measurements could not be obtained in this analysis. This was not unexpected, as it is well known that clinical data and patient-rated outcome measures do not correlate with electrodiagnostic severity in CTS26. Lastly, there is a possibility that the findings might be an epiphenomenon of the surgical intervention. However, because the procedure only involves a small incision with local anesthesia, it is unlikely that any associated epiphenomena might last for the 6 months between our measurement times.
In summary, the distance on the vertical axis between the ECDs for the first and third digits improved 6 months after carpal tunnel release. However, there were only slight changes in the recovery function of the RMS for the N20m 6 months after surgery. Our results suggest that treating peripheral nerve lesions, such as in carpal tunnel release, positively modifies brain function. We reveal a more complete understanding of the pathophysiology of CTS that incorporates a neurorehabilitative approach targeting the adaptive and maladaptive changes in the brain.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Maeda, Y. et al. Altered brain morphometry in carpal tunnel syndrome is associated with median nerve pathology. Neuroimage Clin. 2, 313–319 (2013).
Maeda, Y. et al. Functional deficits in carpal tunnel syndrome reflect reorganization of primary somatosensory cortex. Brain. 137, 1741–1752 (2014).
Maeda, Y. et al. Primary somatosensory/motor cortical thickness distinguishes paresthesia-dominant from pain-dominant carpal tunnel syndrome. Pain. 157, 1085–1093 (2016).
Lu, Y. C. et al. Local and extensive neuroplasticity in carpal tunnel syndrome: A resting-state fMRI study. Neurorehabil Neural Repair. 31, 898–909 (2017).
Iwatsuki, K. et al. Recovery function of somatosensory evoked brain response in patients with carpal tunnel syndrome: A magnetoencephalographic study. Clin Neurophysiol. 127, 2733–2738 (2016).
Ma, H. et al. A longitudinal fMRI research on neural plasticity and sensory outcome of carpal tunnel syndrome. Neural Plast. 2017, 5101925 (2017).
Dhond, R. P. et al. Spatio-temporal mapping cortical neuroplasticity in carpal tunnel syndrome. Brain. 135, 3062–3073 (2012).
Iwatsuki, K. et al. Comparative responsiveness of the Hand 20 and the DASH-JSSH questionnaires to clinical changes after carpal tunnel release. J Hand Surg Eur. 39, 145–51 (2014).
Kurimoto, S. et al. Development and validation of a ten-item questionnaire with explanatory illustrations to assess upper extremity disorders: favorable effect of illustrations in the item reduction process. J Orthop Sci. 16, 737–744 (2011).
Kurimoto, S. et al. Favorable effects of explanatory illustrations attached to a self-administered questionnaire for upper extremity disorders. Qual Life Res. 22, 1145–1149 (2013).
Nishizuka, T., Iwatsuki, K., Kurimoto, S., Yamamoto, M. & Hirata, H. Efficacy of a forearm band in addition to exercises compared with exercises alone for lateral epicondylitis: a multicenter, randomized, controlled trial. J Orthop Sci. 22, 289–294 (2017).
Nishizuka, T. et al. Favorable responsiveness of the Hand10 questionnaire to assess treatment outcomes for lateral epicondylitis. J Hand Surg Asian Pac 23, 205–209 (2018).
Sarvas, J. Basic mathematical and electromagnetic concepts of the biomagnetic inverse problem. Phys Med Biol. 32, 11–22 (1987).
Hoshiyama, M. & Kakigi, R. Two evoked responses with different recovery functions in the primary somatosensory cortex in humans. Clin Neurophysiol. 112, 1334–1342 (2001).
Hoshiyama, M. & Kakigi, R. New concept for the recovery function of short-latency somatosensory evoked cortical potentials following median nerve stimulation. Clin Neurophysiol. 113, 535–541 (2002).
Goto, S. et al. Disinhibitory shift of recovery curve of somatosensory-evoked response in elderly: a magnetoencephalographic study. Clin Neurophysiol. 126, 1228–1233 (2015).
Park, K. M., Shin, K. J., Park, J., Ha, S. Y. & Kim, S. E. The usefulness of terminal latency index of median nerve and f-wave difference between median and ulnar nerves in assessing the severity of carpal tunnel syndrome. J Clin Neurophysiol. 31, 162–168 (2014).
Iwatsuki, K., Hoshiyama, M., Oyama, S., Shimoda, S. & Hirata, H. Magnetoencephalographic evaluation for the myoelectric hand prosthesis with tacit learning system. NeuroRehabilitation. 44, 19–23 (2019).
Yoshida, A. et al. Upper extremity disability is associated with pain intensity and grip strength in women with bilateral idiopathic carpal tunnel syndrome. NeuroRehabilitation. 44, 199–205 (2019).
Grooms, D. R. et al. Neuroplasticity associated with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 47, 180–189 (2017).
Kakinoki, R. et al. Motor and sensory cortical changes after contralateral cervical seventh nerve root (CC7) transfer in patients with brachial plexus injuries. J Hand Surg Asian Pac. 22, 138–149 (2017).
Yu, A. et al. Functional connectivity of motor cortical network in patients with brachial plexus avulsion injury after contralateral cervical nerve transfer: a resting-state fMRI study. Neuroradiology. 59, 247–253 (2017).
Napadow, V. et al. Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome. Pain. 130, 254–266 (2007).
Napadow, V. et al. Somatosensory cortical plasticity in carpal tunnel syndrome treated by acupuncture. Hum Brain Mapp. 28, 159–171 (2007).
Maeda, Y. et al. Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain. 140, 914–927 (2017).
Trybus, M., Koziej, M., Belka, M., Bednarek, M. & Banach, M. The Polish version of the Boston Carpal Tunnel Questionnaire: Associations between patient-rated outcome measures and nerve conduction studies. J Plast Reconstr Aesthet Surg. 72, 924–932 (2019).
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number 15K10400 and 19K09647.
Author information
Authors and Affiliations
Contributions
K.I., M.H. and H.H. performed this study and wrote the draft. K.I., T.S., A.Y. and H.H. registered the patients. K.I. and T.S. designed this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iwatsuki, K., Hoshiyama, M., Yoshida, A. et al. A magnetoencephalographic study of longitudinal brain function alterations following carpal tunnel release. Sci Rep 9, 19776 (2019). https://doi.org/10.1038/s41598-019-56190-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56190-8
This article is cited by
-
Altered brain function and structure in carpal tunnel syndrome: a systematic review and meta-analysis of structural and functional brain imaging
Brain Structure and Function (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.