Abstract
There is limited information on the association of overweight and obesity with cardiac remodeling in elderly population. Therefore, we investigated whether overweight and obesity are associated with cardiac geometric structures and function in Chinese elderly. A total of 1183 hospitalized patients (aged 65–99 years) with primary hypertension were collected retrospectively in a cross-sectional study, and divided into underweight, normal weight, overweight and obesity patient groups according to their body mass index (BMI). Cardiac echocardiographic parameters were compared between the groups. BMI was 17.2 ± 1.2, 21.4 ± 1.2, 25.1 ± 1.2, 30.2 ± 2.6 kg/m2 in underweight, normal weight, overweight and obesity groups respectively. Aortic and left atrial diameter, interventricular septal and left ventricular (LV) posterior wall thickness, LV end-diastolic and end-systolic diameter, and indexed LV mass, and prevalence of E/A reversal were higher, while LV ejection fraction and fractional shortening were lower in elderly with overweight or obesity, as compared with whose with underweight or normal weight separately (All P < 0.05). However, multivariable regression analysis showed that overweight and obesity are independently related to increased LV wall thickness, end-diastolic diameter and mass (All P < 0.05). In conclusions, this study demonstrates that overweight and obesity are associated with increased LV wall thickness, end-diastolic diameter and mass in Asian elderly.
Similar content being viewed by others
Introduction
A U-shaped association between body mass index (BMI) and mortality exists in elderly population1,2. The mortality rate has been higher in underweight elderly patients than those with normal bodyweight1,2,3. Unexpectedly, a study has shown that the mortality is lower in elderly with overweight or mild moderate obesity than whose with normal bodyweight4, although overweight and obese patients usually have comorbidities such as hypertension, type 2 diabetes mellitus and dyslipidemia than whose with normal bodyweight5,6. This phenomenon is widely known as obesity paradox5. However, unhealthy obesity has been associated with increased all-cause mortality among elderly subjects5. The morbid obesity is related to higher prevalence of hypertension, diabetes and dyslipidemia, which could be associated with major adverse cardiovascular consequences in elderly patients. Nevertheless, the study on detailed associations of overweight and obesity with cardiac structures and function is still limited in elderly Asian population. Therefore, we collected data on Chinese elderly patients with primary hypertension in a cross-sectional study in order to investigate the relationship of overweight and obesity to cardiac remodeling and function.
Methods
Patients
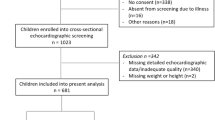
One thousand one hundred eighty-three hospitalized elderly (aged 65 to 99 years, 538 males, 645 females) with primary hypertension were collected retrospectively from April 2014 to March 2018 in a cross-sectional study. The hypertensive patients with or without comorbidities were treated with antihypertensive drugs or/and lifestyle modification. Among them, 98 subjects were firstly diagnosed with primary hypertension; 103 subjects were treated only with lifestyle modification. Hypertension criteria included an average untreated casual systolic blood pressure (SBP) ≥ 140 mm Hg or diastolic blood pressure (DBP) ≥ 90 mm Hg at clinical visits7,8. Type 2 diabetes mellitus (DM) was defined by fasting plasma glucose (FPG) ≥ 7 mmol/L or 2 hours postprandial plasma glucose (PPG) ≥ 11.1 mmol/L in oral glucose tolerance test; Moreover, plasma insulin concentration is normal or increased in the subjects9. Fatty liver was diagnosed by color doppler ultrasound. Gout was considered when there were arthralgia, arthritis and hyperuricemia or gouty tophus. Coronary heart disease (CHD) was considered when there was a history of coronary revascularization, coronary angiographic or electrocardiographic evidences of myocardial infarction or ischemia accompanied by anti-anginal medications. Stroke was based on the history and computer tomographic or magnetic resonance imaging relevant evidences. Chronic obstructive pulmonary disease (COPD) was diagnosed by a history of chronic cough with sputum and pulmonary obstructive ventilation dysfunction. Data was collected retrospectively from the First Affiliated Hospital of Chongqing Medical University, Chongqing, China. The study was approved by the ethics committee of the institution. However, the institutional ethics committee waived the need for patients’ written informed consent for this retrospective analysis of clinically acquired data.
We excluded patients with secondary hypertension due to glomerulonephritis, pyelonephritis, aldosteronism, vascular diseases and glucocorticoid use. The patients with primary hypertension coexisting senile degenerative cardiac valvular disease, congenital heart disease or whose treated with bariatric surgery were also excluded.
Assessment of body mass index
BMI = body weight kg/(height m)2. Underweight, normal weight, overweight and obesity were respectively diagnosed according to World Health Organization criteria for Asian populations, as considering that overweight and obese Asian people are more susceptible to cardiovascular diseases10. Underweight refers BMI < 18.5 kg/m2. Normal weight: 23 kg/m2 < BMI ≥ 18.5 kg/m2. Overweight: 27.5 kg/m2 < BMI ≥ 23 kg/m2. Obesity: BMI ≥ 27.5 kg/m210.
Measurement of blood glucose, lipids, uric acid, creatinine and eGFR
Plasma glucose and glycated hemoglobin (HbA1c) concentrations were determined by hexokinase method and high performance liquid ion exchange chromatography respectively. Total cholesterol (TC), high density lipoprotein cholesterol (HDL-C) and triglyceride (TG) were determined by cholesterol oxidase, magnesium sulfate precipitation and three-color methods respectively. Low density lipoprotein cholesterol (LDL-C) was calculated by TC - HDL-C - (TG/2.19). Plasma uric acid and creatinine concentrations were determined by uricase and enzyme methods respectively. eGFR (estimated glomerular filtration rate) was calculated by following equations. For male, serum creatinine (Scr) > 80 μmol/L: eGFR = 141 · (Scr μmol/L/88.4/0.9)−1.209 · 0.993Age years; Scr ≤ 80 μmol/L: eGFR = 141 · (Scr μmol/L/88.4/0.9)−0.411 · 0.993Age years. For female, Scr > 62 μmol/L: eGFR = 144 · (Scr μmol/L/88.4/0.7)−1.209 · 0.993Age years; Scr ≤ 62 μmol/L: eGFR = 144 · (Scr μmol/L/88.4/0.7)−0.329 · 0.993Age years11.
Measurement of cardiac structure and function by echocardiography
According to American Society of Echocardiology leading-edge method, transthoracic color doppler echocardiographic studies were performed and read by experienced cardiologists in a single core laboratory in our hospital, with a Vivid echocardiographic system (General Electric Co., Fairfield, CT, USA), which was equipped with a 3.5-MHz sector scan transducer12,13. Two-dimensional–guided M-mode measurement of right ventricular diameter (RVD), aortic diameter (AOD), interventricular septal thickness (IVST), left ventricular (LV) posterior wall thickness (LVPWT) and end-diastolic diameter (LVEDD) were examined at end-diastole from the parasternal long-axis view; Left atrial diameter (LAD) and LV end-systolic diameter (LVESD) were measured at end-systole from the parasternal long-axis view; LV mass (LVM) g = (0.80 · 1.04 · ((LVEDD mm + IVST mm + LVPWT mm)3 - (LVEDD mm)3) + 0.6) · 0.001; LVMI g/m2.7 = LVM g/(height m)2.7; LV peak early (E) and late (A) filling velocities were measured. E/A reversal prevalence, LV ejection fraction (LVEF) and fractional shortening (LVFS) were examined8,12,13.
Statistical analysis
Continuous parameters were expressed as mean values ± standard deviation (SD). The statistical differences were evaluated by one-way ANOVA, followed, in case of significance, by a two-side LSD test for multiple comparisons including between overweight and underweight or normal weight groups, and between obesity and underweight or normal weight groups. Categorical data were summarized as percentages and compared using Chi-square test. Pearson univariate linear correlation and logistic multivariate regression models were utilized for data analysis. Statistical analysis was performed by SPSS 22.0 software package (IBM Company, Chicago, Illinois 60606, USA). A 2-tailed value of P < 0.05 was considered to be statistically significant.
Results
Clinical characteristics
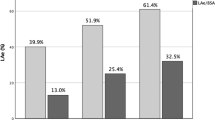
The study included 1183 hypertensive patients with mean age and BMI (SD) of 79 ± 7 years and 24.5 ± 3.8 kg/m2 respectively. The male sex, BMI, prevalence of hypertension, dyslipidemia and type 2 DM, plasma glucose, HbA1c, fatty liver markers, uric acid, cigarette smoking, alcohol drinking, and the use of medications were higher in overweight patients as compared with underweight or normal weight patients (All P < 0.05, Tables 1–2). Consistently, the above mentioned parameters have increased in the obese patients as compared with the underweight or normal weight patients, as shown in the Tables 1–2. BMI was correlated positively with male sex, hypertension, type 2 DM, plasma glucose, HbA1c, dyslipidemia, fatty liver, gout, uric acid, cardiac functional class, cigarette smoking, alcohol drinking, and use of medications respectively (All P < 0.05, Tables 1–2).
Cardiac LV structure and function
Echocardiographic parameters were also compared between overweight and underweight or normal weight patients. The results showed that AOD, LV wall thickness, diameter and mass, and the prevalence of E/A reversal were increased; whereas LVEF and LVFS were decreased in patients with overweight (All P < 0.05, Table 3). The respective comparisons between obese and underweight or normal weight patients showed that AOD, LAD, LV wall thickness, diameter and mass, and the prevalence of E/A reversal were increased; but LV function was decreased in patients with obesity (All P < 0.05, Table 3). BMI was directly related to echocardiographic parameters including AOD, LAD, LV wall thickness, diameter, mass and the prevalence of E/A reversal; Meanwhile it was inversely related to LVEF and LVFS (All P < 0.05, Table 3).
Multivariable adjusted regression analysis showed that BMI was not related to sex, age, cigarette smoking, alcohol drinking, hypertension, diabetes, dyslipidemia, fatty live and gout (All P > 0.05, Table 4). However, BMI was directly associated only with LV wall thickness, end-diastolic diameter and mass (All P < 0.05, Table 4).
Discussion
The present study shows that overweight and obesity were associated with increased LV wall thickness, dimension and mass in the hypertensive elderly Asian population. The results remained consistent, after adjustment of many variables including sex, age, hypertension, diabetes, dyslipidemia, gout, use of cigarette smoking and alcohol drinking.
Overweight and obesity may be the most important lifestyle-related factors involving in cardiovascular morbidity and mortality in elderly14,15,16. Previous studies showed that overweight and obese older people are susceptible to cardiovascular diseases in Asian populations14,15. Our study showed that even slightly increased BMI was associated with unwanted cardiac remodeling. On the other hand, it has suggested that overweight and obesity with cardiac remodeling could be prevented through beneficial lifestyle modification and bariatric surgery17,18.
Through its linking with the occurrence of other metabolic syndrome components, obesity is closely related to atherosclerotic cardiovascular disease and consequent hemodynamic alteration as well as cardiac structural change and dysfunction19. The pathophysiological mechanisms underlying the overweight- and obesity- LV remodeling may be multifactorial. With increments in adipose tissue and its vascular bed size in the case of overweight or obesity, as a compensatory mechanism, the sympathetic and renin-angiotensin-aldosterone (RAA) systems are activated to drive cardiovascular system overload for meeting the metabolic demands of extra adipose tissue. Long-standing overweight leads to cardiac volume- and pressure-overload, and higher cardiac output and blood pressure via activation of sympathetic and RAA systems, consequently causing myocardial fibrosis, ventricular maladaptive hypertrophy and enlargement with cardiac dysfunction, and increase of cardiovascular events and mortality20.
Excessive fat from adipose tissues accumulates in vessels, leading to arterial stiffness and hypertension21; as adipose accumulates in respiratory tract, it mechanically impairs pulmonary ventilation. Resultantly, hypoventilation, obstructive sleep apnea, hypoxia, hypercapnia and respiratory acidosis can then occur22. This chronic hypoxia and hypercapnia cause sympathetic-RAA system activation, vasoconstriction and hypertension with consequent overweight- or obesity-related cardiac geometric remodeling and dysfunction20,22. Additionally, accumulated adipose tissue can secrete RAA components, which can activate sympathetic and RAA systems, leading to adverse cardiac dysfunction23,24.
The present study has demonstrated that both overweight and obesity are directly related to LV wall thickness, LV dilation and mass in elderly25. Our results are in line with other studies, which have confirmed that overweight and obesity predominantly resulted in LV concentric hypertrophy25,26. Besides these findings, our study also replenished that overweight and obesity are independently related to LV enlargement and larger LV mass in elderly. Although the overweight- and obesity-associated LV enlargement has not been consistently related to LV systolic dysfunction26, it may lead to cardiac remodeling and LV diastolic dysfunction27,28. Previous epidemiological evidence has also indicated that higher body weight could provide protection against adverse cardiac events in elderly population, which is reflecting so called as obesity paradox27,29. However, obesity with significant cardiac remodeling has been associated with an increased risk of cardiac death16,20.
Nevertheless, our study suggested that overweight and obesity are not associated with dilation of right ventricle and left atrium and LV function. The underlying causes could be explained as follows: LV geometric alterations were mild and may not cause dilation of right ventricle and left atrium and LV dysfunction30. Left atrial dimension was evaluated by anteroposterior diameter, although left atrial volume has been used as a measure of left atrial size. During previous years, left atrial volume was not routinely assessed in clinical practice, and therefore this data was not available from our medical records. Secondly, LV diastolic dysfunction was defined by E/A reversal31, which may not precisely reflect LV diastolic dysfunction.
The major limitation of the present study is that the data was obtained from a cross-sectional study. Although multivariable adjusted regression analyses were performed, the effects of other possible confounding factors should be taken into consideration. Therefore, large prospective studies would be needed to reconfirm the observed findings. The study was carried on hypertensive elderly, its results should be cautiously extrapolated to normotensive elderly.
In conclusion, overweight and obesity are related to echocardiographic findings such as increased LV wall thickness, dilation and mass in elderly. These LV changes can be detected easily by cardiac echocardiography in real life clinical practice.
References
Harris, T. et al. Body mass index and mortality among nonsmoking older persons: the Framingham Heart Study. J. Am. Med. Assoc. 259, 1520–1524 (1988).
Tanaka, S. et al. Body mass index and mortality among Japanese patients with type 2 diabetes: pooled analysis of the Japan diabetes complications study and the Japanese elderly diabetes intervention trial. J. Clin. Endocrinol. Metab. 99, E2692–2696, https://doi.org/10.1210/jc.2014-1855 (2014).
Batsis, J. A. et al. Body mass index and risk of adverse cardiac events in elderly patients with hip fracture: a population-based study. J. Am. Geriatr. Soc. 57, 419–426, https://doi.org/10.1111/j.1532-5415.2008.02141.x (2009).
Liu, Z. M., Tse, L. A., Chan, D., Wong, C. & Wong, S. Y. S. Dietary sugar intake was associated with increased body fatness but decreased cardiovascular mortality in Chinese elderly: an 11-year prospective study of Mr and Ms OS of Hong Kong. Int. J. Obes. 42, 808–816, https://doi.org/10.1038/ijo.2017.292 (2018).
O’Brien, E. C. et al. Association of body mass index and long-term outcomes in older patients with non-ST-segment-elevation myocardial infarction: results from the CRUSADE Registry. Circ. Cardiovasc. Qual. Outcomes 7, 102–109, https://doi.org/10.1161/CIRCOUTCOMES.113.000421 (2014).
Weiss, A., Boaz, M., Beloosesky, Y., Kornowski, R. & Grossman, E. Body mass index and risk of all-cause and cardiovascular mortality in hospitalized elderly patients with diabetes mellitus. Diabet. Med. 26, 253–259, https://doi.org/10.1111/j.1464-5491.2009.02672.x (2009).
Committee of cardiocerebrovascular diseases of Gerontological Society of China. [Chinese expert consensus on the diagnosis and treatment of hypertension in the elderly (2017)]. Zhonghua Nei Ke Za Zhi 56, 885-893, https://doi.org/10.3760/cma.j.issn.0578-1426.2017.11.024 (2017).
Peng, J. et al. Association of left atrial enlargement with ventricular remodeling in hypertensive Chinese elderly. Echocardiography 34, 491–495, https://doi.org/10.1111/echo.13484 (2017).
Zhao, Q., Laukkanen, J. A., Li, Q. & Li, G. Body mass index is associated with type 2 diabetes mellitus in Chinese elderly. Clin. Interv. Aging 12, 745–752, https://doi.org/10.1111/echo.13484 (2017).
W.H.O. Expert Consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163, https://doi.org/10.1016/S0140-6736(03)15268-3 (2004).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1–39 e14, https://doi.org/10.1016/j.echo.2014.10.003 (2015).
Marwick, T. H. et al. Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). Eur. Heart J. Cardiovasc. Imaging 16, 577–605, https://doi.org/10.1093/ehjci/jev076 (2015).
Fan, H. et al. Abdominal obesity is strongly associated with cardiovascular disease and its risk factors in elderly and very elderly community-dwelling Chinese. Sci. Rep. 6, 21521, https://doi.org/10.1038/srep21521 (2016).
Chuang, S. Y., Hsu, Y. Y., Chen, R. C., Liu, W. L. & Pan, W. H. Abdominal obesity and low skeletal muscle mass jointly predict total mortality and cardiovascular mortality in an elderly asian population. J. Gerontol. A Biol. Sci. Med. Sci. 71, 1049–1055, https://doi.org/10.1093/gerona/glv192 (2016).
Aune, D., Schlesinger, S., Norat, T. & Riboli, E. Body mass index, abdominal fatness, and the risk of sudden cardiac death: a systematic review and dose-response meta-analysis of prospective studies. Eur. J. Epidemiol. 33, 711–722, https://doi.org/10.1007/s10654-017-0353-9 (2018).
Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the obesity society. J. Am. Coll. Cardiol. 63, 2985–3023, https://doi.org/10.1016/j.jacc.2013.11.004 (2014).
Shin, S. H. et al. Beneficial effects of bariatric surgery on cardiac structure and function in obesity. Obes. Surg. 27, 620–625, https://doi.org/10.1007/s11695-016-2330-x (2017).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet 384, 766–781, https://doi.org/10.1016/S0140-6736(14)60460-8 (2014).
Lascaris, B. et al. Cardiac structure and function before and after bariatric surgery: a clinical overview. Clin. Obes. 8, 434–443, https://doi.org/10.1111/cob.12278 (2018).
Iancu, M. E., Copaescu, C., Serban, M. & Ginghina, C. Favorable changes in arterial elasticity, left ventricular mass, and diastolic function after significant weight loss following laparoscopic sleeve gastrectomy in obese individuals. Obes. Surg. 24, 364–370, https://doi.org/10.1007/s11695-013-1097-6 (2014).
Shah, R. V. et al. Obesity and sleep apnea are independently associated with adverse left ventricular remodeling and clinical outcome in patients with atrial fibrillation and preserved ventricular function. Am. Heart J. 167, 620–626, https://doi.org/10.1016/j.ahj.2014.01.002 (2014).
Borghi, F., Seva-Pessoa, B. & Grassi-Kassisse, D. M. The adipose tissue and the involvement of the renin-angiotensin-aldosterone system in cardiometabolic syndrome. Cell Tissue Res. 366, 543–548, https://doi.org/10.1007/s00441-016-2515-6 (2016).
Lambert, E. A., Straznicky, N. E., Dixon, J. B. & Lambert, G. W. Should the sympathetic nervous system be a target to improve cardiometabolic risk in obesity? Am. J. Physiol. Heart Circ. Physiol. 309, H244–258, https://doi.org/10.1152/ajpheart.00096.2015 (2015).
Woodiwiss, A. J. et al. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am. J. Hypertens. 21, 1144–1151, https://doi.org/10.1038/ajh.2008.252 (2008).
Turkbey, E. B. et al. The impact of obesity on the left ventricle: the Multi-Ethnic Study of Atherosclerosis (MESA). J.A.C.C. Cardiovasc. imaging 3, 266–274, https://doi.org/10.1016/j.jcmg.2009.10.012 (2010).
Abel, E. D., Litwin, S. E. & Sweeney, G. Cardiac remodeling in obesity. Physiol. Rev. 88, 389–419, https://doi.org/10.1152/physrev.00017.2007 (2008).
Powell, B. D., Redfield, M. M., Bybee, K. A., Freeman, W. K. & Rihal, C. S. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am. J. Cardiol. 98, 116–120, https://doi.org/10.1016/j.amjcard.2006.01.063 (2006).
Mariscalco, G. et al. Body mass index and mortality among adults undergoing cardiac surgery: a nationwide study with a systematic review and meta-analysis. Circulation 135, 850–863, https://doi.org/10.1161/CIRCULATIONAHA.116.022840 (2017).
Litwin, S. E. Cardiac remodeling in obesity: time for a new paradigm. J.A.C.C. Cardiovas. imaging 3, 275–277, https://doi.org/10.1016/j.jcmg.2009.12.004 (2010).
Laukkanen, J. A., Kurl, S., Eranen, J., Huttunen, M. & Salonen, J. T. Left atrium size and the risk of cardiovascular death in middle-aged men. Arch. Intern. Med. 165, 1788–1793, https://doi.org/10.1001/archinte.165.15.1788 (2005).
Acknowledgements
This study was supported by the natural science research fund of Chongqing Science & Technology Commission in Chongqing City, China (CSTC, No. 2007BB5276), the medical science & technology research fund of Health Bureau of Chongqing City, China (No. 04-2-154 and No. 2009-2-290) and the grant from National Key Clinical Specialties Construction Program of China (No. [2013]544).
Author information
Authors and Affiliations
Contributions
G.L. contributed to the study conception, experiment design and protocols and research fund raising. C.L.,L.H., Q.Z., J.Z. and X.Z. carried out experiments and data collection. G.L. statistically analyzed and interpreted experimental results. G.L. and J.A.L. drafted, reviewed, revised and finalized the manuscript. Finally, all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, C., Li, G., Laukkanen, J.A. et al. Overweight and obesity are associated with cardiac adverse structure remodeling in Chinese elderly with hypertension. Sci Rep 9, 17896 (2019). https://doi.org/10.1038/s41598-019-54359-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-54359-9
This article is cited by
-
Phospho-ablation of cardiac sodium channel Nav1.5 mitigates susceptibility to atrial fibrillation and improves glucose homeostasis under conditions of diet-induced obesity
International Journal of Obesity (2021)
-
Low body mass is associated with reduced left ventricular mass in Chinese elderly with severe COPD
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.