Abstract
Aim of this study was to establish a simple and highly reproducible physiological circulation model to investigate endovascular device performance. The developed circulation model included a pneumatically driven pulsatile pump to generate a flow rate of 2.7 L/min at 70 beats per minute. Sections from the superficial femoral arteries were used in order to simulate device/tissue interaction and a filter was integrated to analyze periinterventional thromboembolism of white, red and mixed thrombi. The working fluid (3 L) was a crystalloid solution constantly tempered at 36.5 °C. To evaluate the model, aspiration thrombectomy, stent-implantation and thrombectomy with the Fogarty catheter were performed. Usability of the model was measured by the System Usability Scale (SUS) – Score. Histological specimens were prepared and analyzed postinterventional to quantify tissue/device interaction. Moreover, micro- and macroembolism were evaluated for each thrombus entity and each device. Results were tested for normality using the D’Agostino-Pearson test. Statistical comparisons of two groups were performed using the Student’s t-test. All devices were able to remove the occlusions after a maximum of 2 attempts. First-pass-recanalization was not fully achieved for aspiration thrombectomy of mixed thrombi (90.6%), aspiration thrombectomy of red thrombi (84.4%) and stent-implantation in occlusions of red thrombi (92.2%). Most micro- and macroembolism were observed using the Fogarty catheter and after stent-implantation in occlusions of white thrombi. Histological examinations revealed a significant reduction of the vascular layers suggesting vascular damage after use of the Fogarty catheter (327.3 ± 3.5 μm vs. 440.6 ± 3.9 μm; p = 0.026). Analysis of SUS rendered a mean SUS-Score of 80.4 which corresponds to an excellent user acceptability of the model. In conclusion, we describe a stable, easy to handle and reproducible physiological circulation model for the simulation of endovascular thrombectomy including device performance and thromboembolism.
Similar content being viewed by others
Introduction
During the last decade, endovascular recanalization of thrombotic occlusions has achieved greater success through improvement in device technology and the technical abilities of interventionalists1. The extended use of mechanical percutaneous thrombectomy devices like Rotarex® and Angiojet® and the widespread use of various covered and uncovered stent systems marks a new era of interventional percutaneous thrombectomy and expands the scope of action for both arterial and venous disease and both vascular surgeons and vascular interventionalists far beyond the classical surgical thrombectomy2,3. Therefore, all vascular disciplines have made great efforts to establish suitable and standardized circulation models for endovascular training, device testing and experimental studies4,5. But until today, none of these models fulfil the special requirements of simulating percutaneous thrombectomy including thromboembolism, vascular endothelium and different types of thrombi. Most of these described circulation models include plastic replica of the vascular tree and only a few models provide cadaveric vessels with or without a crystalloid solution pumped through the model4,5. Although these models allow the training of basic endovascular procedures, they do not simulate satisfactorily the human vascular system and usually do not allow the sufficient experimental testing of new endovascular devices and new imaging procedures. Moreover, most of these models have never been evaluated or standardized.
Further, a number of issues like postinterventional thromboembolism, vascular endothelium/device interaction, different thrombus entities and large-scale experiments of recanalization could not be investigated sufficiently in groups of large animals or human corpses.
Nevertheless, a standardized and fully evaluated in-vitro circulation model for simulating thrombectomy of thrombotic occlusions/stenosis with different thrombus entities and potential thromboembolism has not been established so far. Ideally, the proposed circulation model should be adapted to the following issues: (I) the model should represent sufficient and reproducible physiological flow conditions with a blood substitute, (II) the model should enable good technical manageability for the interventionalist simulating different segments of the human arterial tree with multilayered vessels with potential for dissection and damage of the vascular endothelium, (III) the model should include different entities of thrombi and periinterventional thromboembolism.
Material and Methods
Development of the circulation model
To achieve a physiological circulation model of the human arterial tree, a mechanical volume-controlled pulsatile pump (modified 7025 Rodent Ventilator; Ugo Basile, Gemonio, Italy) was used to generate a flow rate of 2.7 L/min at 70 beats per minute and with a peak flow at 3.3 L/min (Fig. 1a,b). Sections from the human superficial femoral artery (SFA) were provided by voluntary donors undergoing transfemoral amputation and were then transferred into an acrylic resin-based model of the femoropopliteal section (ELASTRAT, Geneva, Switzerland).
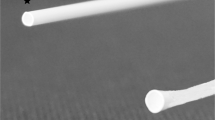
Schematic representation (a) and downsized visualization (b) of the circulation model: (1) replaceable section for the (c) vascular-phantom or the whole arterial tree, (2) filter for collecting thromboembolism, (3) warm water supply, (4) pneumatically driven pulsatile pump. The working fluid (3 L) consisted of a crystalloid solution (60% glucose solution). Depiction of the vacular phantom used for the evaluation of device/tissue interaction.
After extraction all vessels were examined sonographically within the circulation model. High grade stenosis (>50%) as well as occluded vessels and/or plaque ruptures were removed from the study. The extracted vessels had a standard length of 60 mm and a vessel diameter of 6.38 ± 3.17 mm. To fix and stabilize the thrombus position within the vascular phantom, a simple ligature of the extracted vessel was performed (standardized via Hegar probe) in central position of the extracted vessel (Fig. 1c). The Hegar probe defined a standardized residual lumen (5 mm) of the vascular phantom in order to guarantee both a stable thrombus position and an unhindered passage of the endovascular devices. Thrombus position and residual vascular lumen was verified sonographically under flow conditions.
The working fluid (3 L) consisted of a crystalloid solution (60% glucose solution). Alternatively, in former experiments we have also used a suspension of water and whole blood at a volume ratio of 1:3 in order to simulate long-term lysis with pharmacological agents and imaging procedures for intraluminal navigation6. The working fluid was constantly tempered at 36.5 °C by warm water supply. Temperature and intraluminal pressure of the model were constantly measured via an arterial pressure (D19 KT Display; GE Medical Systems, Chicago, USA and DPT-6000 pressure-set; CODAN Critical care GmbH, Forstinning, Germany) and temperature probe (Testo 108; Testo SE and Co KGaA, Lenzkirch, Germany). Periinterventional thromboembolism was determined by collecting micro- and macroembolism in a filter from an extracorporeal circulation system (Schleicher und Schüll, Düren, Germany).
Experimental protocol
This feasibility study serves to develop and evaluate an in-vitro circulation model for studying endovascular thrombectomy including device/tissue interaction and periinterventional thromboembolism (Fig. 1a,b). Therefore, four endovascular trained surgeons evaluated the model and performed aspiration thrombectomy (n = 8/each investigator), thrombectomy with a Fogarty catheter (n = 8/each investigator) and stent-implantation (n = 8/each investigator). All experiments were performed in a hybrid-operation room. Usability of the model was measured by the System Usability Scale (SUS) - Score, as previously described7.
To evaluate potential dissection and/or damage of the vascular endothelium, histological samples were taken and the number of micro- and macroembolisms were analyzed. To evaluate the basic functionality of the model, intraluminal pressure and temperature measurement was continuously performed via an arterial pressure system (D19 KT Display; GE Medical Systems, Chicago, USA and DPT-6000 pressure-set; CODAN Critical care GmbH, Forstinning, Germany) and a temperature probe (Testo 108; Testo SE and Co KGaA, Lenzkirch, Germany). The Studies have been approved by the local ethical committee of the University Medical Center Schleswig-Holstein, Kiel, Germany (protocol identification: D513/19). This research was in compliance with the Helsinki Declaration and informed written consent was obtained from all donors/participants.
Generation of different thrombus entities and preparation of the intraluminal thrombus
As previously reported, thrombi were made in the Chandler loop under standardized conditions8,9. Venous blood was taken from five voluntary, healthy male donors and haematologic testing was performed prior to blood sampling including testing for Von Willebrand disease, haemophilia, the factor V Leiden mutation and thrombophilia diagnosis. A polymeric vessel-phantom was used to obtain standardized thrombus dimensions (length = 30 mm, diameter = 6 mm) from the Chandler loop. A series of former experiments and pretests (n = 150) was performed to secure an adequate reproducibility of the thrombi6. The thrombi were extracted, measured and immediately transferred into the circulation model.
Red thrombi (agglutinative thrombi) were generated by using human full blood, white thrombi (precipitation thrombi) were generated by using human plasma and mixed thrombi (white and red) were generated by using human full blood and plasma at a volume ratio of 1:110.
Endovascular procedures
Four endovascular trained surgeons evaluated the model and performed the endovascular procedures in the circulation model. An introduction sheet was inserted proximal and the thrombotic occlusion was passed via a 0.035 inch guide wire (Terumo GmbH Germany, Eschborn, Germany) in order to perform simple aspiration thrombectomy, stent-implantation (Abbott, Chicago, USA; Absolut Pro Vascular self-expanding stent, 6 × 40 mm) and thrombectomy via Fogarty catheter (Edwards Lifesciences, Irvine, USA; Over-the-wire Fogarty catheter). Afterwards all interventionalists answered the SUS questionnaire and evaluated the handling of the model.
Analysis of thromboembolism
Micro- and macroembolism were collected in a post-occlusion filter (Schleicher und Schüll, Düren, Germany) distal of the simulated thrombus. After each recanalization maneuver, the post-occlusion filter was checked for embolized thrombus fragments by a blinded observer via microscope. Fragments > = 1 mm (macroemboli) and <1 mm (microemboli) were separately counted.
Histological analysis
Six proximal, mean and distal vessel specimens were routinely fixed in 4% formalin solution and embedded in paraffin. Paraffin-embedded vascular tissue sections (4 μm) were then stained with hematoxylin-eosin (HE) to define the intimal and medial layers by light microscopy. The intima-media-thickness was quantified in ten random vascular sections by an image analyzer (Samba 2000®; North Sioux City, Iowa, USA).
Statistical analysis
All values are expressed as mean ± standard deviation (SD). Categorical variables are presented as frequency distributions (n) and percentages (%). Data were analyzed with Graph Pad Prism version 5.01 for Windows (GraphPad Software; San Diego, California, USA) and tested for normality using the D’Agostino-Pearson test. Statistical comparisons of two groups were performed using the Student’s t-test. A p-value < 0.05 was considered as significant.
Results
Performance of endovasculare procedures and usability of the circulation model
Endovascular recanalization was achieved in 92 out of the 96 maneuvers. Four maneuvers failed because of mishandling of the model (n = 2) and the device (n = 2). All devices (aspiration catheter, Fogarty catheter, self-expanding stent) were able to remove or eliminate (stent implantation) the thrombus after a maximum of 2 attempts (Fig. 2). First-pass-recanalization was not fully achieved for aspiration thrombectomy of mixed clots (90.6%), aspiration thrombectomy of red thrombi (84.4%) and stent-implantation in occlusion of red thrombi (92.2%), as presented in Tables 1–3. The evaluation of the circulation model rendered a mean SUS-Score of 80.4 which corresponds to a percentile rank of 90% and therefore an excellent acceptability range/adjective rating7. Mean intraluminal pressure was 83.5 mm/Hg ± 4.32 and temperature was 36.43 C ± 2.23 measured at six different time points during the experiments.
Representative imaging of thrombectomy performed in the circulation model. Performance of stent-implantation (a) in the region of the thrombotic occlusion. Performance of thrombectomy with the Fogarty catheter (b). Red arrows mark the position of the replaceable vascular section. Red asterisks show the position of the stent respectively the Fogarty catheter.
Analysis of thromboembolism
Micro- and macroembolism occur in all endovascular maneuvers except aspiration thrombectomy of red thrombi (Tables 1–3). Most micro- and macroembolism were observed using the Fogarty catheter (n = 11) and stent-implantation (n = 9) in occlusions of white thrombi (Tables 1–3; Fig. 3).
Histological analysis
Specimens of arteries were stained with HE to examine potential dissection and damage of the vascular layers. No macroscopic dissection was observed in the current experiments. The intima-media-thickness did not differ significantly after aspiration, thrombectomy and stent-implantation. However, histological examination revealed significant vascular lesions of tunica intima and media after using the Fogarty catheter (327.3 ± 3.5 μm vs. 440.6 ± 3.9 μm; p = 0.026; Supplement 1).
Discussion
Endovascular procedures have marked a new era of vascular medicine during the last two decades11,12. Accordingly, endovascular methods have also been performed to recanalize thrombotic occlusions by mechanic thrombectomy or stent-implantation but until today no suitable in-vitro model for the simulation of thrombotic occlusions and thromboembolism is available4,5. Most of the so far described in-vitro models allow the basic training of endovascular procedures and simple experimental testing but they do not simulate satisfactorily the human vascular tree and circulation system. Therefore, these models usually do not allow the sufficient experimental testing of new endovascular devices respectively new imaging procedures including catheter handling, thromboembolism and injury of the vascular layers.
In contrast, animal models can offer a physiological circulation, however the size of most animal vessels is too small for many devices being introduced to human arteries. Larger mammals like pigs and sheep could simulate the human arterial tree, but experiments with these animals are subjected to major logistic challenges, ethical concerns and great expense4,13. Moreover, a number of issues like postinterventional thromboembolism, vascular endothelia/device interaction, different thrombus entities and large-scale experiments of vascular recanalization cannot be investigated sufficiently in groups of large animals.
The reproducible model featured in this study provides a physiological circulation, easy access for the interventionalist, simulation of vascular-tissue/device interactions and analysis of periinterventional thromboembolism due to different thrombus entities. Accordingly, the analysis of the SUS-score originally created to provide a simple assessment of technical procedures, revealed a high acceptability range and support our hypothesis of high user acceptance7. All participating investigators attested an excellent technical performance and acceptability range of the circulation model. Therefore, the model should be easily reproducible and usable for other researches in the vascular field.
The basic functionality (temperature, blood pressure) of the circulation system was assessed at six time points during the evaluation experiments and the reproducibility and stability of the model was particularly high (SD <10%). The pilot experiments showed that complete first-pass-recanalization was achieved for all devices except aspiration thrombectomy of mixed and red thrombi which corresponds to the consistence of the different thrombus entities. Agglutinative “red” thrombi are composed of cellular deposits and feature a more rigid surface whereas “white” precipitation thrombi grow out of the plasmatic components with a softer structure. Consequently, the pilot experiments showed that micro- and macroembolism differed between the three methods of thrombectomy and also between the three types of thrombi reflecting that the choice of the vascular tool and composition of the thrombus impact significantly thromboembolism.
One major objective of the current study was to establish a model which enables the investigation of tissue/device interaction under physiological conditions. Histological specimens were prepared after the experiments and revealed that only the use of the Fogarty catheter was associated with significant damage of the vascular layer which is supported by the findings of former studies for mechanical thrombectomy14.
Therefore, the model also provides differentiated results of device performance which seems necessary as development in vascular imaging provides, in the future, more precise assessment of thrombus localization and composition and market offers the clinician a bewildering number of vascular tools15,16.
In conclusion the here developed circulation model which can be easily established and employed by other groups offers three major benefits: (I) a stable, easy to handle and reproducible physiological circulation for the simulation of endovascular access (II) a cadaveric vascular tree/vascular interposition for studying the influence of endovascular tools on the vascular layer; and (III) the possibility to simulate agglutinative thrombotic occlusions or precipitation thrombi and easy assessment of perioperative thromboembolism.
References
Goktay, A. Y. & Senturk, C. Endovascular Treatment of Thrombosis and Embolism. Adv. Exp. Med. Biol. 906, 195–213 (2016).
Heller, S. et al. Percutaneous Mechanical Thrombectomy Using Rotarex® S Device in Acute Limb Ischemia in Infrainguinal Occlusions. Biomed. Res. Int. 2362769 (2017).
Das, S., Das, N., Serota, H. & Vissa, S. A retrospective review of patients with massive and submassive pulmonary embolism treated with AngioJet rheolytic thrombectomy with decreased complications due to changes in thrombolytic use and procedural modifications. Vascular. 26(2), 163–168 (2018).
Garrett, J. R. A human cadaveric circulation model. J. Vasc. Surg. 33(5), 1128–1130 (2001).
Jansen, S., Cowie, M., Linehan, J. & Hamdorf, J. M. Fresh frozen cadaver workshops for advanced vascular surgical training. ANZ J. Surg. 84(11), 877–880 (2014).
Rusch, R. et al. Development of a new catheter prototype for laser thrombolysis under guidance of optical coherence tomography (OCT): validation of feasibility and efficacy in a preclinical model. J. Thromb. Thrombolysis. 43(3), 352–360 (2017).
Brooke, J. SUS: a retrospective. Journal of usability studies. 8(2), 29–40 (2013).
Diamond, S. L. Engineering design of optimal strategies for blood clot dissolution. Annu. Rev. Biomed. Eng. 1, 427–461 (1999).
Slee, J. B., Alferiev, I. S., Levy, R. J. & Stachelek, S. J. The use of the ex vivo 316 Chandler Loop Apparatus to assess the biocompatibility of modified polymeric blood 317 conduits. J. Vis. Exp. 20, (90) (2014).
Byrnes, J. R. & Wolberg, A. S. Red blood cells in thrombosis. Blood. 130(16), 1795–1799 (2017).
Dominguez, A. III, Bahadorani, J., Reeves, R., Mahmud, E. & Patel, M. Endovascular therapy for critical limb ischemia. Expert Rev. Cardiovasc. Ther. 13(4), 429–444 (2015).
Mustapha, J. A., Diaz-Sandoval, L. J. & Saab, F. Innovations in the endovascular management of critical limb ischemia: retrograde tibiopedal access and advanced percutaneous techniques. Curr Cardiol. Rep. 19(8), 68 (2017).
Long, C. A. et al. An endovascular model of ischemic myopathy from peripheral arterial disease. J. Vasc. Surg. 66(3), 891–901 (2017).
Turk, A. S., Siddiqui, A. H. & Mocco, J. A comparison of direct aspiration versus stent retriever as a first approach (‘COMPASS’): protocol. J. Neurointerv. Surg. 10(10), 953–957 (2018).
Feng, J. & Jing, Z. Development History of Endovascular Surgery and Devices. Endovascular Surgery and Devices. PP 3–7 (2018).
Kim, J., Park, J. E., Nahrendorf, M. & Kim, D. E. Direct thrombus imaging in stroke. J. Stroke. 18(3), 286–296 (2016).
Acknowledgements
We like to thank Katharina Hess for helping with the preparation of the histological specimen and Marijana Mikkelsen for helping with the illustration.
Author information
Authors and Affiliations
Contributions
R.R., J.T., S.A., R.B. designed the circulation model. R.R. and R.B. designed all experiments. M.A., L.H., M.R., A.H., J.P.S., R.R., T.P., J.C. evaluated and analyzed the usability of the circulation model. M.R. and R.R. performed and analyzed the histological stainings. All authors interpreted results, contributed to the manuscript and prepared the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rusch, R., Trentmann, J., Hummitzsch, L. et al. Feasibility of a circulation model for the assessment of endovascular recanalization procedures and periprocedural thromboembolism in-vitro. Sci Rep 9, 17356 (2019). https://doi.org/10.1038/s41598-019-53607-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-53607-2
This article is cited by
-
Experimental Evaluation of the Effectiveness of Aspiration-Based Techniques to Treat Different Types of Acute Thromboembolic Occlusions in the Femoropopliteal Vascular System Using an In Vitro Flow Model
CardioVascular and Interventional Radiology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.