Abstract
Prolonged inspiratory to expiratory (I:E) ratio ventilation may improve arterial oxygenation or gas exchange and respiratory mechanics in patients with obesity. We performed a randomised study to compare the effects of the conventional ratio ventilation (CRV) of 1:2 and the equal ratio ventilation (ERV) of 1:1 on arterial oxygenation and respiratory mechanics during spine surgery in overweight and obese patients. Fifty adult patients with a body mass index of ≥25 kg/m2 were randomly allocated to receive an I:E ratio either l:2 (CRV; n = 25) or 1:1 (ERV; n = 25). Arterial oxygenation and respiratory mechanics were recorded in the supine position, and at 30 minutes and 90 minutes after placement in the prone position. The changes in partial arterial oxygen pressure (PaO2) over time did not differ between the groups. The changes in partial arterial carbon dioxide pressure over time were significantly different between the two groups (P = 0.040). The changes in mean airway pressure (Pmean) over time were significantly different between the two groups (P = 0.044). Although ERV provided a significantly higher Pmean than CRV during surgery, the changes in PaO2 did not differ between the two groups.
Similar content being viewed by others
Introduction
The overweight and obese population has increased sharply in recent years1. This is both a concern for general healthcare and a major risk factor for related diseases and perioperative morbidity2. Several studies have revealed that obesity is related to poor postoperative outcomes, such as longer hospital stay, high incidence rates of wound infection, and pulmonary complication3,4,5.
Obesity itself leads to abnormalities of lung mechanics and function. Thus, the obese population has a high incidence of postoperative pulmonary complications resulting from reduced lung compliance, decreased functional residual capacity, and susceptibility to atelectasis formation under general anaesthesia4. Cautious management of mechanical ventilation is necessary in patients with obesity to control these altered respiratory mechanics, which lead to impaired oxygenation and gas exchange during surgery.
Moreover, obesity correlates with an increased risk of intraoperative hypoxaemia6. Numerous studies have focused on methods to improve oxygenation or respiratory mechanics in patients with obesity during the perioperative period5,7,8,9,10, and lung protective strategies have been employed in such patients undergoing general anaesthesia11. Conventionally, high positive end expiratory pressure (PEEP) with the recruit manoeuvre is used to manage impaired oxygenation in patients with obesity during general anaesthesia8. Prolonged inspiratory to expiratory (I:E) ratio ventilation, which is also an effective ventilatory manoeuvre in obese patients undergoing laparoscopic bariatric surgery12,13; this technique improves gas exchange, arterial oxygenation, and respiratory mechanics in patients with acute respiratory distress syndrome or acute lung injury. A prolonged I:E ratio sustains increased alveolar pressure and decreases dead space, consequently improving arterial oxygenation and respiratory function.
Therefore, we hypothesized that prolonged I:E ratio ventilation improves arterial oxygenation and respiratory mechanics in overweight and obese patients undergoing lumbar spine surgery. This randomised study compared the conventional ratio ventilation (CRV) of 1:2 with the equal ratio ventilation (ERV) of 1:1 in terms of their effect on arterial oxygenation and respiratory mechanics during posterior lumbar spine surgery in overweight and obese patients placed in the prone position.
Results
Study population
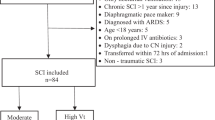
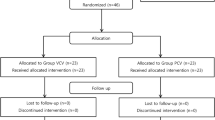
Fifty patients were enrolled in the present study; two dropped out, one in each group, because they were not subjected to the scheduled study protocol (Fig. 1). Demographic variables are shown in Table 1.
Enrolment of patients undergoing lumbar spine surgery. Between November 2016 and October 2018, 54 patients who underwent lumbar spine surgery in our institution were assessed. Four patients did not meet the inclusion criteria and two patients dropped out. Thus, 48 patients were subjected to the study protocol.
Analyses of arterial blood gas
Figure 2 illustrates changes in arterial blood gas during surgery. The changes in arterial pH over time were significantly different between the two groups (P = 0.024). In the ERV group, arterial pH was significantly lower during surgery (P < 0.001), and it was lower at 90 minutes (T90) after placement in the prone position than in the supine position (Tsupine) (P < 0.001). The changes in partial arterial carbon dioxide pressure (PaCO2) over time were significantly different between the two groups (P = 0.040). However, PaCO2 was not significantly changed during surgery in either group. The two groups did not differ in terms of the changes in oxygen partial pressure (PaO2) or alveolar-to-arterial oxygen gradient (D(A-a)O2) over time, although PaO2 was significantly increased and D(A-a)O2 significantly decreased during surgery in both groups (P < 0.001 in both cases).
Changes in arterial blood gas values during surgery. The changes in pH (A) and PaCO2 (B) over time were significantly different between CRV (•, filled circle) and ERV (○, empty circle) groups. PaO2 (C) was significantly higher, whereas D(A-a)O2 (D, alveolar to arterial oxygen tension gradient) was significantly lower in the ERV group than in the CRV group. In the ERV group, PaO2 was significantly higher at T30 and T90 than at Tsupine, whereas there was no difference in the CRV group. CRV = Patients administered 1:2 ratio ventilation; ERV = Patients administered equal ratio ventilation; Tsupine = After induction of anaesthesia in the supine position; T30 and T90 = At 30 and 90 min after placement in the prone positioning, respectively; pH = pH of arterial blood gas analysis; PaO2 = Partial arterial oxygen pressure; PaCO2 = Partial arterial carbon dioxide pressure. *P < 0.05 vs. Tsupine within the group.
Respiratory mechanics
Table 2 lists the patients’ respiratory mechanics during surgery. The changes in peak airway pressure (Ppeak), driving airway pressure (Pdriving), dynamic lung compliance (Cdyn), and static lung compliance (Cstatic) over time were not different between the two groups. While Ppeak was not significantly changed, Pdriving was significantly increased during surgery in both groups (P = 0.008 in the CRV group and P < 0.001 in the ERV group). In both groups, there were significant decreases in Cdyn (P < 0.001 in both cases) and Cstatic (P = 0.025 in the CRV group and P < 0.001 in the ERV group). The changes in mean airway pressure (Pmean) over time were significantly different between the two groups (P = 0.044). Pmean was significantly lower at 30 minutes after in the prone position (T30) and T90 than at Tsupine in the CRV group only (P = 0.001 in both cases).
Haemodynamic signs
The haemodynamic parameters during surgery are listed in Table 3. The changes in mean arterial pressure and heart rate over time were not different between the two groups.
Discussion
The current study, which was expanded from our previous study assessing the effect of prolonged inspiratory ventilation in patients undergoing laparoscopic bariatric surgery13, suggests that ERV does not confer superior arterial oxygenation than CRV during posterior lumbar spine surgery in overweight and obese patients placed in the prone position under general anaesthesia. However, ERV did confer a significantly higher Pmean than CRV during surgery. This was the first study to reveal the impact of prolonged inspiratory ventilation on patients in the prone position.
Postoperative pulmonary complication is one of the main factors determining length of hospital stay and cost burden on patients. Generally, general anaesthesia using muscle paralysis generates impaired pulmonary gas exchange because of alterations in respiratory mechanics and atelectasis formation. Obesity may increase the risk of postoperative pulmonary complications14. Consistent with a previous study13,15, our results showed that PaO2 was significantly higher at T30 and T90 than at Tsupine in the ERV group, and that changes in Pmean were higher in the ERV group than in the CRV group, but this latter effect did not reach statistical significance. ERV improves oxygenation by increasing Pmean and concomitantly reducing Ppeak13. Pmean is related to arterial oxygenation because it is the average alveolar pressure that opens and inflates the alveoli against the elastic recoil of the lungs and chest wall16. An elevated Pmean value induces alveolar recruitment, which improves ventilation perfusion mismatch and blood oxygenation17. Thus, a prolonged I:E ratio sustains an increased alveolar pressure, thus increasing patients’ functional residual capacity18. Although our results do not confirm that ERV is clinically superior to CRV, ERV may be feasible in overweight and obese patients with deteriorated oxygenation during general anaesthesia.
PaO2 significantly increased over time in both the ERV and CRV groups, perhaps because the patients were placed in the prone position. Numerous studies have demonstrated that the prone position can improve oxygenation in pneumonia, acute respiratory distress syndrome, and acute lung injury19,20,21. Pelosi et al. also reported that the prone position resulted in improved lung compliance, a rise of functional residual capacity, and improved oxygenation in obese patients under elective general anaesthesia22. A rise in functional residual capacity was also seen after placement of the patients in the prone position, perhaps because there was decreased cephalad pressure on the diaphragm and changes in the gravitational ventilation/perfusion gradient23. The improved oxygenation also results from movement of the diaphragm, because, compared with the supine position, the prone position leads to greater excursion in the posterior diaphragm in regions where atelectasis formation and ventilation/perfusion mismatch are most severe during general anaesthesia; furthermore, pulmonary perfusion is more uniformly distributed in the prone position24. We assumed that the prone position improves oxygenation during general anaesthesia, regardless of which mechanical ventilatory manoeuvre is used, and further study is required to confirm our results.
Prolonged I:E ratio ventilation and prone positioning improve ventilation/perfusion heterogeneity to produce efficient gas exchange25,26. In contrast with some studies, our data showed that PaCO2 was increased in the intraoperative period. We permitted the study practitioners to manage the respiratory rate and maintain an end-tidal carbon dioxide tension (EtCO2) level between 33 and 36 mmHg. This may have created bias. Additional studies are needed to verify the actual impact of ERV on gas exchange.
The present study had some limitations. Firstly, even though we used a randomisation plan generator, the mean body mass index (BMI) of the ERV group was higher than that of the CRV group. Despite this statistical deficiency, ERV did not confer better arterial oxygenation than CRV in patients in the prone position in the present study. In one study by Kendale and Blitz, an increase in BMI correlated with an increase in intraoperative hypoxaemia risk6. Therefore, in the present study, the mean BMI of both groups may have affected arterial oxygenation during the study period. Secondly, our study group did not include morbidly obese patients whose BMI was more than 35.0 kg/m2; the purpose of the study was to investigate the effect of prolonged I:E ratio ventilation in overweight and obese patients. Hence, a supplemental study examining prolonged I:E ratio ventilation during spine surgery should be performed in morbidly obese patients.
In conclusion, ERV conferred lower peak inspiratory pressure and higher mean airway pressure than CRV in overweight and obese patients undergoing posterior lumbar spine surgery in the prone position under general anaesthesia. Therefore, ERV may reduce the airway pressure increase in overweight and obese patients undergoing spinal surgery in the prone position. Even though ERV did not confer better arterial oxygenation than CRV in the present study, ERV may be feasible in overweight or obese patients during general anaesthesia. Further study is needed to confirm the impact of ERV on oxygenation in patients with elevated BMI undergoing spine surgery in the prone position.
Methods
Subjects
This study was approved by the institutional Ethics Committee (Gachon University Gil Medical Center Institutional Review Board 2016–211, Incheon, Korea) and registered at the US Clinical Trials Registry (NCT02961920). After obtaining written informed consent, we assessed 54 patients scheduled for lumbar spine surgery in our institution between November 2016 and October 2018. Fifty adult patients with an ASA physical status of I or II and a BMI of ≥25 kg/m2 were enrolled the study. Patients were excluded if they had severe pulmonary disease (history of chronic obstructive pulmonary disease, asthma, bronchopleural fistula, or pneumothorax), haemodynamic instability, and/or hypovolaemia. The enrolled patients were randomly allocated according to a predetermined sequence to receive an I:E ratio of either 1:2 (CRV; n = 25) or 1:1 (ERV; n = 25). One researcher in our institution who was not involved in the present study generated the allocation sequence without blocking using a randomisation plan generator (http://www.randomisation.com). This study was performed in accordance with relevant guidelines and regulations, including the CONSORT guidelines (Fig. 1).
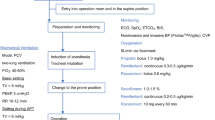
Anaesthesia
To induce anaesthesia, intravenous propofol (1.5 mg/kg) and rocuronium (0.8 mg/kg) were administered. Volume-controlled mechanical ventilation was applied, with a tidal volume of 10 mL per ideal body weight (kg), an I:E ratio of 1:2 or 1:1, depending on the group allocation, and no external PEEP. To maintain the EtCO2 level between 33 and 36 mmHg during surgery, the respiratory rate was adjusted. To maintain anaesthesia, sevoflurane was used, with an end-tidal concentration of 2–2.5% by volume and a bispectral index score between 40 and 60. Rocuronium (0.2 mg/kg) was injected every hour. The inspired oxygen fraction (FiO2) was 0.4, using oxygen and air. Radial artery catheterization was conducted to allow repeated blood sampling and continuous blood pressure monitoring.
Study design
Standard monitoring during anaesthesia included continuous electrocardiography, systemic arterial pressure, heart rate, EtCO2, and peripheral oxygen saturation. We measured intraoperative respiratory mechanics, including peak airway pressure (Ppeak), mean airway pressure (Pmean), plateau airway pressure, and PEEP using the anaesthesia machine (S/5 Avance anaesthetic machine, GE Healthcare, Madison, WI, USA). We also measured arterial blood gas at three time-points: 10 minutes after anaesthesia induction, Tsupine, T30 and T90. We calculated Pdriving, Cdyn, and Cstatic from respiratory data, and D(A-a)O2 from arterial gas analysis data. Pdriving was defined as the difference between plateau airway pressure and PEEP. Cdyn and Cstatic were calculated using the following formulas: tidal volume/(Ppeak − PEEP) and tidal volume/Pdriving, respectively. Alveolar oxygen tension was calculated using the following formula: FiO2(PB − 47 mmHg) − (PaCO2/0.8), where PB is the barometric pressure (760 mmHg).
Statistical analysis
A previous study reported that, during CRV with an inspired oxygen fraction of 0.4, the mean value (standard deviation) of partial arterial oxygen pressure (PaO2) was 181 (28) mmHg in obese patients after placement in the prone position22. We assumed a mean PaO2 difference of 15% between the CRV and ERV groups. With an α-value of 0.05 and a statistical power of 90%, a sample size of 23 patients was required for each group. Anticipating a 10% drop out rate, we recruited 50 patients.
Continuous variables are expressed as mean ± standard deviation, and categorical variables as number of patients (%). Continuous variables were analysed using the Student’s t-test or Mann–Whitney U test. Categorical variables were analysed using Fisher’s exact test. Serial changes in respiratory variables and haemodynamic changes were analysed using repeated measures ANOVA, followed by Bonferroni correction27. After analysing the group × time interaction, we reanalysed serial changes in respiratory variables in each group using repeated measures ANOVA followed by Bonferroni correction. SPSS 21.0 (SPSS Inc., Chicago, IL) was used for statistical analyses.
Clinical trial number
NCT02961920 (Date of registration: November 11 2016) https://clinicaltrials.gov/ct2/show/NCT02961920?term=NCT02961920&rank=1.
Data availability
All data generated or analysed during this study are available from the corresponding author upon reasonable request.
References
Gupta, V. et al. Safety of Aesthetic Surgery in the Overweight Patient: Analysis of 127,961 Patients. Aesthetic surgery journal 36, 718–729 (2016).
Sood, A. et al. The Effect of Body Mass Index on Perioperative Outcomes After Major Surgery: Results from the National Surgical Quality Improvement Program (ACS-NSQIP) 2005–2011. World journal of surgery 39, 2376–2385 (2015).
Patel, N. et al. Obesity and spine surgery: relation to perioperative complications. Journal of neurosurgery. Spine 6, 291–297 (2007).
Wysham, W. Z. et al. Obesity and perioperative pulmonary complications in robotic gynecologic surgery. American journal of obstetrics and gynecology 213, 33.e31–33.e37 (2015).
Maia, L. A., Silva, P. L., Pelosi, P. & Rocco, P. R. M. Controlled invasive mechanical ventilation strategies in obese patients undergoing surgery. Expert review of respiratory medicine 11, 443–452 (2017).
Kendale, S. M. & Blitz, J. D. Increasing body mass index and the incidence of intraoperative hypoxemia. Journal of clinical anesthesia 33, 97–104 (2016).
Bluth, T. et al. Protective intraoperative ventilation with higher versus lower levels of positive end-expiratory pressure in obese patients (PROBESE): study protocol for a randomized controlled trial. Trials 18, 202 (2017).
Imber, D. A. et al. Respiratory Management of Perioperative Obese Patients. Respiratory care 61, 1681–1692 (2016).
Xie, P., Li, Z. & Tian, Z. The optimal combination of mechanical ventilator parameters under general anesthesia in obese patients undergoing laparoscopic surgery. Journal of clinical anesthesia 34, 290–294 (2016).
Korzhuk, A. et al. High-Frequency Percussive Ventilation Rescue Therapy in Morbidly Obese Patients Failing Conventional Mechanical Ventilation. Journal of intensive care medicine, 885066618769596 (2018).
Xu, L., Shen, J. & Yan, M. The effect of pressure-controlled inverse ratio ventilation on lung protection in obese patients undergoing gynecological laparoscopic surgery. Journal of anesthesia 31, 651–656 (2017).
Mousa, W. F. Equal ratio ventilation (1:1) improves arterial oxygenation during laparoscopic bariatric surgery: A crossover study. Saudi J Anaesth 7, 9–13 (2013).
Jo, Y. Y., Kim, J. Y., Park, C. K., Chang, Y. J. & Kwak, H. J. The Effect of Ventilation Strategy on Arterial and Cerebral Oxygenation During Laparoscopic Bariatric Surgery. Obes Surg 26, 339–344 (2016).
Reinius, H. et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 111, 979–987 (2009).
Kim, M. S. et al. The impact of two different inspiratory to expiratory ratios (1:1 and 1:2) on respiratory mechanics and oxygenation during volume-controlled ventilation in robot-assisted laparoscopic radical prostatectomy: a randomized controlled trial. Canadian journal of anaesthesia = Journal canadien d’anesthesie 62, 979–987 (2015).
Marcy, T. W. & Marini, J. J. Inverse ratio ventilation in ARDS. Rationale and implementation. Chest 100, 494–504 (1991).
Zavala, E. et al. Effect of inverse I:E ratio ventilation on pulmonary gas exchange in acute respiratory distress syndrome. Anesthesiology 88, 35–42 (1998).
Kim, W. H. et al. Prolonged inspiratory time produces better gas exchange in patients undergoing laparoscopic surgery: A randomised trial. Acta anaesthesiologica Scandinavica 57, 613–622 (2013).
Kallet, R. H. A Comprehensive Review of Prone Position in ARDS. Respiratory care 60, 1660–1687 (2015).
Du, Y. et al. [Meta analysis of observing prone position ventilation role in the oxygenation of severe pneumonia patients]. Zhonghua wei zhong bing ji jiu yi xue 30, 327–331 (2018).
Kim, W. Y. & Hong, S. B. Sepsis and Acute Respiratory Distress Syndrome: Recent Update. Tuberculosis and respiratory diseases 79, 53–57 (2016).
Pelosi, P. et al. Prone positioning improves pulmonary function in obese patients during general anesthesia. Anesthesia and analgesia 83, 578–583 (1996).
Lamm, W. J., Graham, M. M. & Albert, R. K. Mechanism by which the prone position improves oxygenation in acute lung injury. American journal of respiratory and critical care medicine 150, 184–193 (1994).
Krayer, S., Rehder, K., Vettermann, J., Didier, E. P. & Ritman, E. L. Position and motion of the human diaphragm during anesthesia-paralysis. Anesthesiology 70, 891–898 (1989).
Johnson, N. J., Luks, A. M. & Glenny, R. W. Gas Exchange in the Prone Posture. Respiratory care 62, 1097–1110 (2017).
Yadav, M., Reddy, E. P., Sharma, A., Kulkarni, D. K. & Gopinath, R. The Effect of Position on PaCO2 and PETCO2 in Patients Undergoing Cervical Spine Surgery in Supine and Prone Position. Journal of neurosurgical anesthesiology 29, 298–303 (2017).
Lee, Y. What repeated measures analysis of variances really tells us. Korean journal of anesthesiology 68, 340–345 (2015).
Author information
Authors and Affiliations
Contributions
K.M.K., J.C. and H.K. designed the study and wrote the manuscript. J.C. and S.B.K. performed data collection. D.L. and W.J. performed data management and interpreted data. K.M.K., J.C., S.B.K. and H.K. analysed data and prepared the manuscript. All authors have seen the original study data, reviewed the data analysis, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, K.M., Choi, J.J., Lee, D. et al. Effects of ventilatory strategy on arterial oxygenation and respiratory mechanics in overweight and obese patients undergoing posterior spine surgery. Sci Rep 9, 16638 (2019). https://doi.org/10.1038/s41598-019-53194-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-53194-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.