Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) with transpapillary metal stenting is the standard palliation method for malignant distal biliary obstruction (MDBO); however, post-ERCP pancreatitis are not uncommon. Endoscopic ultrasonography-guided biliary drainage (EUS-BD) with transmural metal stenting has emerged as an option for primary palliation of MDBO. We compared the efficacy and safety of these procedures as first-line MDBO treatment. We searched for relevant English-language articles in PubMed, Embase, and Cochrane databases. The outcomes of interest were technical success, clinical success, adverse events, stent patency, reintervention rates, and procedure time. Subgroup analysis was performed for patients without duodenal invasion (eg, endoscopically accessible papilla; EUS-choledochoduodenostomy [CDS] vs. ERCP). Ten studies (3 randomized trials and 7 retrospective studies) with 756 patients were included. The cumulative technical and clinical success rates were high for both procedures (EUS-BD: 94.8% [294/310] and 93.8% [286/305], ERCP: 96.5% [386/400] and 95.7% [377/394]). The cumulative adverse event rates were 16.3% (54/331) for EUS-BD and 18.3% (78/425) for ERCP. In subgroup analysis for patients without duodenal invasion, EUS-CDS showed similar cumulative technical and clinical success rate with ERCP (technical success rate, EUS-CDS vs. ERCP: 94.2% [146/155] vs. 97.8% [237/242]; clinical success rate, EUS-CDS vs. ERCP: 94.2% [145/154] vs. 93.0% [225/242]). The cumulative rate of adverse events for EUS-CDS and ERCP was also comparable (15.5% [24/155] for EUS-CDS and 18.6% [45/242] for ERCP). As first-line palliation of MDBO, EUS-BD was similar to ERCP in technical and clinical success and safety; however, larger randomized trials comparing EUS-CDS and ERCP in this setting with endoscopically accessible papilla may be required.
Similar content being viewed by others
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) has gradually evolved to include therapeutic biliary endoscopy since the introduction of endoscopic sphincterotomy in 19741. ERCP-guided stenting across the stricture and through the papilla is the standard palliative treatment for malignant distal biliary obstruction (MDBO). However, ERCP is not always successful and causes various adverse events. ERCP could fail in various situations including duodenal obstruction, surgically altered anatomy, MDBO, and periampullary tumor infiltration. Post-ERCP pancreatitis (PEP) is a major adverse event in ERCP, with an incidence of 3.5% (range, 1.6–15.7%), and can cause death in severe cases2,3. PEP is associated with procedure-related risk factors including difficult cannulation, guidewire passage through the pancreatic duct, and pancreatic injection2.
To date, endoscopic ultrasonography-guided biliary drainage (EUS-BD) has been limited to use in failed ERCP cases. A recent meta-analysis showed better clinical success, fewer adverse events, and lower reintervention rates with EUS-BD than with percutaneous transhepatic biliary drainage (PTBD) as an alternative procedure4. Furthermore, EUS-BD may have several advantages over ERCP. EUS-BD can be easily implemented in patients with duodenal invasion, and procedure-related pancreatitis could be prevented as endoscopists do not manipulate the major papilla during EUS-guided transmural biliary drainage. EUS-BD performed by experts may require a shorter procedure time than ERCP, with use of dedicated devices5. Finally, EUS-BD may show longer stent patency and lower reintervention rates, as the self-expandable metal stent does not need to be placed across the stricture, preventing tumor ingrowth or overgrowth in a metal stent5.
A recent study showed substantially better outcomes with EUS-BD than with ERCP as primary palliation for MDBO5. Recent randomized and prospective studies6,7,8 also showed good results of EUS-BD in patients without duodenal invasion; however, there remains insufficient evidence to suggest EUS-BD as a primary approach5. Therefore, a systematic review and meta-analysis (SRMA) on this subject is needed. We conducted this study to investigate whether EUS-BD is similar to ERCP concerning efficacy and safety in the first-line treatment of MDBO.
Methods
Data sources and search strategy
An experienced medical librarian (E.S.) developed the search strategy according to the PRISMA (Preferred Reporting Items for SRMA) guidelines. The literature search was conducted using PubMed, Embase, and the Cochrane Central Register of Controlled Trials for articles published between January 2001 and August 20189. The search terms were combinations of synonyms for biliary obstruction and biliary drainage methods, as follows: (bile duct obstruction or biliary obstruction) and (EUS or endoscopic ultrasound or EUS-guided biliary drainage) and (ERCP or endoscopic retrograde cholangiopancreatography) and (biliary drainage or biliary stent or choledochoduodenostomy [CDS] or hepaticogastrostomy [HGS]). The search was limited to English-language literature.
Inclusion and exclusion criteria
Randomized controlled trials (RCTs) or observational studies comparing EUS and ERCP for MDBO were selected, focusing on either efficacy or safety, or both. The exclusion criteria were (1) case reports, conference reports, editorials, letters, and reviews; (2) animal studies; (3) abstracts and meta-analyses; (4) studies with no comparative data; (5) patients with special characteristics, such as surgically altered anatomy; and (6) other disease entities. Two authors (S.Y.H. and H.S.) independently assessed the eligibility of the searched articles.
Outcome assessment
The primary outcomes were technical success and adverse events for EUS-BD and ERCP. Given the novelty of EUS-BD, we believe that detailed definitions of technical success and adverse events for primary outcomes are warranted5,6. Technical success was defined as placement of the metal stent as planned via ERCP or EUS10. The secondary outcomes were clinical success, stent patency, reintervention rates, and procedure time for EUS-BD and ERCP. Clinical success was defined as resolution of biliary obstruction clinically and as reflected by laboratory parameters, or a 75% decrease in bilirubin level at 4 weeks4.
Data extraction and quality assessment
The following data were extracted: (1) study characteristics (authors, year of study, affiliation, country of origin, study design); (2) patient characteristics (sample size); (3) technical and clinical success rates; (4) adverse events, including procedure-related pancreatitis and bile peritonitis; and (5) stent patency, reintervention rates, and total procedure time. The Cochrane tool for assessing risk of bias was used for RCTs, and the Newcastle-Ottawa scale was used for assessment of observational studies. Two authors (S.Y.H. and H.S.) independently evaluated the quality of the studies, and any disagreement was resolved with consensus of a third or fourth reviewer (D.U.K. and D.H.P.).
Data synthesis and analysis
We performed a random-effects meta-analysis to synthesize the data by pooling the results of RCTs and cohort studies. We used a random-effect model to account for variations across studies, as the subjects or interventions in these studies would have shown some differences. Treatment effect estimates were reported with pooled risk ratios (RRs) and 95% confidence intervals (CIs) for dichotomous outcomes, including technical and clinical success rates, adverse events, reintervention rates, pooled hazard ratios (HRs) and 95% CIs for stent patency, and pooled estimates of weighted mean differences and 95% CIs for total procedure time. We attempted to contact individual investigators and asked them to reanalyze existing data based on statistical parameters in pooled data. We used forest plots for primary and secondary outcomes.
Many of the included patients with duodenal stenosis were “second-line” patients who cannot undergo ERCP. This also causes unnecessary bias away from ERCP, as many patients had duodenal stenosis in the retrospective cohort (for which EUS-BD is most likely to be effective)11.
As usual, EUS-HGS was considered in patients with MDBO and duodenal bulb invasion (e.g., gastric outlet obstruction), periampullary duodenal invasion with compromised duodenal bulb, or surgically altered anatomy. In patients with MDBO and periampullary tumor infiltration with distal duodenal invasion, EUS-CDS was considered first5.
To determine the role of EUS-BD as the routine first-line option for MDBO in patients without duodenal invasion (eg, endoscopically accessible papilla), therefore, a subgroup analysis comparing EUS-CDS and ERCP in this cohort was conducted.
The I2 statistic was used to assess the magnitude of heterogeneity between studies. An I2 of 0% to <25% was considered to indicate no heterogeneity; 25% to <50%, low heterogeneity; 50% to <75%, moderate (substantial) heterogeneity; and 75% to 100%, high (considerable) heterogeneity. The potential risk of publication bias for primary outcomes was evaluated by constructing funnel plots, and asymmetry was assessed using Egger’s test. We used STATA version 11 (StataCorp, College Station, TX, USA) for all analyses.
Results
Search results and quality assessment
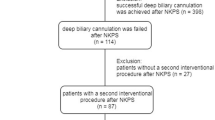
A total 604 articles were identified. The detailed search strategy is described in Supplementary Table 1. After excluding duplicates and irrelevant articles by reviewing abstracts and titles, 171 articles remained. A full-text review was performed, and 161 articles were removed according to the exclusion criteria. The following articles were excluded: (1) studies with no comparative data (n = 68), (2) irrelevant articles that did not include EUS-BD (n = 45), (3) review articles on EUS-BD (n = 27), (4) comparison studies between EUS-BD and another method such as PTBD or surgery (n = 18), and (5) reports with < 5 cases (n = 1). Moreover, 1 article12 was removed as it described enteroscopy-assisted ERCP in patients with surgically altered anatomy and another study was removed as the procedure was performed mostly for benign diseases13. Finally, 10 articles (3 RCTs5,6,7 and 7 retrospective articles11,14,15,16,17,18,19) were included in the meta-analysis (Fig. 1).
Our meta-analysis of 10 studies included 756 patients, of whom 331 underwent EUS-BD and 425 underwent ERCP. Among 220 patients in 3 RCTs, 111 underwent EUS-BD and 109 underwent ERCP. For further analysis, we compared the results of EUS-CDS and ERCP in patients without duodenal invasion. Six studies5,6,7,11,13,16 reported technical/clinical success rates and adverse event rates (including bile peritonitis and pancreatitis) in patients without duodenal invasion. Some articles11,13,16 did not show detailed results. Therefore, we asked the authors of these studies via e-mail for the above-mentioned results. However, some retrospective studies including several cases without duodenal invasion were excluded from our analysis. Among 397 patients without duodenal invasion, 155 underwent EUS-BD and 242 underwent ERCP.
The risk of performance bias was high because none of the RCTs applied blinding of experimental and control procedures. The risk of detection bias was unclear in 1 study; however, the risk of detection bias was low in 2 studies. The risk of reporting, attrition, and selection bias was low in all RCTs. Retrospective articles were assessed with the Newcastle-Ottawa scale; 4 studies showed high quality and 3 showed moderate quality (Supplementary Table 2).
Primary outcomes
Comparison of technical success rates
The overall RR for technical success between EUS-BD and ERCP was 1.01 (95% CI, 0.97–1.06; Q-test p = 0.828, I2 = 0%). There were no significant differences in technical success rates between RCTs and retrospective studies (Fig. 2a). The cumulative technical success rates were high in both procedures (EUS-BD: 94.8% [294/310], ERCP: 96.5% [386/400]). In subgroup analysis for patients without duodenal invasion, EUS-CDS showed similar technical success rates with ERCP (RR, 1.06; 95% CI, 1.00–1.13; Q-test p = 0.973, I2 = 0%) (Fig. 2b). The cumulative technical success rate in patients without duodenal invasion was 94.2% (146/155) for EUS-CDS and 97.8% (237/242) for ERCP.
Comparison of adverse events
The overall RR for adverse events in EUS-BD and ERCP was 1.05 (95% CI, 0.61–1.82; Q-test p = 0.008, I2 = 61.2%) in all studies (Fig. 3a). The cumulative adverse event rate was 16.3% (54/331) for EUS-BD and 18.3% (78/425) for ERCP. However, in RCTs, the adverse event rates for ERCP were relatively high with considerable heterogeneity in each article. In all articles, the adverse events after EUS-BD and ERCP were as follows (EUS-BD [n]:ERCP[n]): cholangitis (17:20), pancreatitis (1:31), cholecystitis (8:13), bile peritonitis (8:0), pneumoperitoneum (3:0), abdominal pain (7:8), bleeding (4:1), stent migration (3:1), perforation (3:1), liver abscess (2:1), fever (0:3), and stent occlusion (0:3). When the incidence rates of procedure-related pancreatitis and bile peritonitis were compared for the 2 methods, there were significantly different results (RR, 0.26; 95% CI, 0.10–0.72, Q-test p = 0.619, I2 = 0% and RR, 5.16; 95% CI, 1.44–18.51; Q-test p = 0.984, I2 = 0%, respectively). The cumulative rate of procedure-related pancreatitis was 0.3% (1/331) for EUS-BD and 7.3% (31/425) for ERCP (Supplementary Fig. 1). The cumulative rate of bile peritonitis was 2.4% (8/331) for EUS-BD and 0% (0/425) for ERCP (Supplementary Fig. 2). There were no severe adverse events in the ERCP group (0%), and there was 1 severe adverse event in the EUS-BD group (1/331, 0.3%). The patient experienced peritoneal stent migration after EUS-guided HGS, and underwent surgical hepaticojejunostomy17.
In subgroup analysis for patients without duodenal invasion, EUS-CDS showed similar adverse event rates with ERCP (RR, 0.78; 95% CI, 0.48–1.29; Q-test p = 0.321, I2 = 14.7%) (Fig. 3b). The cumulative rate of adverse events was 15.5% (24/155) for EUS-CDS and 18.6% (45/242) for ERCP. The cumulative rate of procedure-related pancreatitis was 0% (0/155) for EUS-CDS and 8.7% (21/242) for ERCP. The cumulative rate of bile peritonitis was 2.6% (4/155) for EUS-CDS and 0% (0/242) for ERCP. Evaluation with Egger’s regression test did not detect any obvious asymmetric distribution or small-study effect (p = 0.646); however, the funnel plot showed slight publication bias, owing to the small number of studies included and the moderate heterogeneity (Supplementary Fig. 3). The trim and fill method was used to adjust for publication bias, and the corrected RR in 12 studies was 0.801 (95% CI, 0.446–1.441) (Supplementary Fig. 4)20.
Secondary outcomes
Short-term results
Comparison of clinical success rate and procedure time: The overall RR for clinical success between EUS-BD and ERCP was 1.01 (95% CI, 0.96–1.06; Q-test p = 0.620, I2 = 0%) (Fig. 4a). The cumulative clinical success rates were high in both procedures (EUS-BD: 93.8% [286/305], ERCP: 95.7% [377/394]). In subgroup analysis for patients without duodenal invasion, EUS-CDS showed similar clinical success rates with ERCP (RR, 0.99; 95% CI, 0.93–1.05; Q-test p = 0.644, I2 = 0.0%) (Fig. 4b). The cumulative clinical success rate in patients without duodenal invasion was 94.2% (145/154) for EUS-CDS and 93.0% (225/242) for ERCP. When compared for procedure time, the overall standard mean difference was −5.35 (95% CI, −11.81 to 1.10; Q-test p = 0.000, I2 = 81.2%) in favor of EUS-BD (Supplementary Fig. 5). The mean procedure time of EUS-BD was 8.31–43 min and that of ERCP was 13.1–52.6 min. Although there was no statistical significance, EUS-BD had a shorter procedure time (by about 5 min).
Mid-/long-term results
Reintervention rate and stent patency. The reintervention rate was compared between EUS-BD and ERCP with an overall RR of 0.82 (95% CI, 0.48–1.41; Q-test p = 0.059, I2 = 50.6%) (Supplementary Fig. 6). The incidence of reintervention for EUS-BD was 19.4% (38/196) and that for ERCP was 25.9% (78/291). Comparison of stent patency between procedures revealed an overall HR of 0.74 (95% CI, 0.35–1.56; Q-test p = 0.006, I2 = 69.4%) (Supplementary Fig. 7). EUS-BD had a tendency toward lower reintervention rates and longer stent patency than ERCP; however, there was no statistically significant difference between them.
Discussion
This meta-analysis showed comparable results for EUS-BD and ERCP in relieving MDBO. Furthermore, EUS-CDS showed similar clinical and technical success and overall adverse event profiles with lower rates of procedure-related pancreatitis compared with ERCP in the subgroup without duodenal invasion.
EUS-BD was initially reported in 2001 by Giovannini et al., who performed CDS with a plastic stent21. It has begun to replace PTBD as a rescue method in patients with ERCP failure. A recent meta-analysis4 reported that EUS-BD has better results in terms of success rate, adverse event rates, and reintervention rate than PTBD. One meta-analysis22 of EUS-BD methods (HGS vs. CDS) compared success rates and adverse events in studies published before and after 2013. Increased success rates and decreased adverse events were observed in studies published after 2013. These findings may be due to improvements of EUS-BD accessories, better procedure organization, and greater endoscopist experience.
Recently, several retrospective and randomized studies comparing ERCP and EUS-BD as first-line options for relieving MDBO have been published5,6,7,11,14,15,16,17,18. The technical and clinical success rates and adverse events were comparable between the procedures. However, the sample size of each study may be underpowered23.
A summary of meta-analysis results with separate pooling of RCTs and retrospective studies is shown in Table 1. This meta-analysis revealed similar technical and clinical success rates for EUS-BD and ERCP (technical: 94.8% vs. 96.5%, clinical: 93.8% vs. 95.7%). The results were similar and highly homogeneous in RCTs and retrospective studies.
In cases of biliary obstruction without duodenal invasion (eg, endoscopically accessible papilla), EUS-CDS showed similar technical and clinical success rate with ERCP (technical success rate, EUS-CDS vs. ERCP: 94.2% vs. 97.8%; clinical success rate, EUS-CDS vs. ERCP: 94.2% vs. 93.0%). Duodenal invasion was found in 13–20% of patients with pancreatic or biliary tract cancer24, and duodenal invasion is an important cause of failure to access the ampulla with duodenoscopy, especially in duodenal obstruction proximal to or involving the ampulla. EUS-BD does not need to pass the duodenum, and many cases of biliary obstruction with duodenal invasion were located below the superior duodenal angle or the second portion of the duodenum. In this circumstance, EUS-BD was predicted to have better success rates than ERCP in duodenal invasion.
For EUS-BD to serve as a primary method, there should be meaningful results in comparison with ERCP in the absence of duodenal invasion. Our results showed comparable outcomes between EUS-CDS and ERCP in the subgroup without duodenal invasion. Furthermore, EUS-CDS is more advantageous with respect to adverse event profiles such as PEP even if there is no bile leak compared with ERCP stenting. EUS-BD has potential benefit especially in preoperative biliary drainage because it can prevent PEP, which is a major cause of delay during the preoperative period. Further, some studies proved that preoperative EUS-CDS causes no significant problem in the surgical procedure7,25. Given that relatively few patients with accessible papilla underwent EUS-CDS and ERCP in previous studies, further larger RCT comparing EUS-CDS with a dedicated device and ERCP-guided transpapillary stenting for resectable pancreatic cancer with accessible papilla may be warranted, to determine whether EUS-CDS for preoperative biliary drainage has a potential benefit in preventing PEP and to determine its clinical impact on surgical outcomes compared with ERCP-guided transpapillary stenting.
A recent multicenter study5 revealed that EUS-BD has longer stent patency, fewer reinterventions, and shorter procedure times than ERCP for the primary palliation of MDBO. The authors attributed these results to the use of dedicated devices and substantial endoscopist experience. Dedicated stent introducers such as DEUS (Standard Sci Tech, Seoul, South Korea) and Hot-Axios (Boston Scientific, Natick, MA, USA) provided improved clinical results by simplifying the complex steps of EUS-BD26. Recently, there have been reports on the usefulness of lumen-apposing metal stent in EUS-CDS8,25. The use of these new devices could result in better success rates and lower adverse event rates. Oh et al.27 reported that substantial endoscopist experience in EUS-HGS contributed to shorter procedure time, as well as increased success and decreased adverse event rates. Given the technical feasibility of EUS-CDS compared with EUS-HGS, EUS-CDS with a dedicated device may gain popularity for primary palliation of MDBO, as a viable alternative to ERCP, in the near future. Furthermore, EUS-BD resulted in relatively longer stent patency despite tumor progression because a self-expandable metallic stent is not placed across the stricture site28.
A direct comparison of adverse events for EUS-BD and ERCP may be difficult because there are many such circumstances and the spectrum of adverse events differs among studies. Our study showed similar overall cumulative adverse event rates for EUS-BD and ERCP (16.3% vs. 18.3%). Bile peritonitis was a major concern in EUS-BD, whereas procedure-related pancreatitis was a major concern in ERCP. In EUS-BD, the incidence of bile peritonitis was 2.4%, and 1 patient had a severe adverse event due to stent migration. In ERCP, the overall incidence of procedure-related pancreatitis was 7.3%, with no severe adverse events. However, bile peritonitis associated with EUS-BD may be reduced by the use of dedicated devices for EUS-BD5. PEP may be related to morbidity, mortality, and prolonged hospitalization. Although there have been various efforts to prevent PEP, it still occurs29,30. Thus, from the viewpoint of the higher incidence and difficult management of PEP compared with bile peritonitis, EUS-BD with dedicated devices for the prevention of bile peritonitis may be preferred as the first-line procedure for patients with a high risk for PEP.
Our study has some limitations. First, some results had high heterogeneity owing to the different analysis methods in some articles. Second, the definitions of outcomes were unclear in some studies although we contacted the corresponding authors to ask for details. Third, only 3 RCTs with relatively small numbers of cases were included. Most patients were enrolled in retrospective studies, which had a weak, heterogeneous methodology compared with RCTs. Especially, 1 study enrolled patients with failed ERCP in the EUS-BD group11. These data may have diluted the results of RCTs. Fourth, in this analysis, various methods of EUS-BD, including HGS and CDS, were used. Fifth, with recent developments in chemotherapy and best supportive care, patients now have better survival chances than before. However, in this analysis, most data were short-term results and long-term data were lacking. Further studies are needed to determine whether EUS-BD is appropriate for long-term survivors.
In summary, EUS-BD has technical and clinical success rates similar to those of ERCP. The adverse event rates were also similar despite different adverse event entities in the primary palliation of MDBO. EUS-BD showed a significantly lower incidence of PEP but a higher incidence of bile peritonitis than ERCP. In patients without duodenal invasion, EUS-CDS was similar to ERCP in terms of technical/clinical success rates and adverse event profiles in the first-line palliation of MDBO. Given the few randomized trials and the heterogeneous methodology of retrospective studies in this SRMA, further larger randomized trials comparing EUS-CDS with a dedicated device and ERCP for the primary treatment of MDBO in patients with endoscopically accessible papillae at the setting of preoperative biliary drainage or palliation may be required.
References
Kawai, K. et al. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc 20, 148–151 (1974).
Dumonceau, J. M. et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - updated June 2014. Endoscopy 46, 799–815, https://doi.org/10.1055/s-0034-1377875 (2014).
Anderson, M. A. et al. Complications of ERCP. Gastrointest Endosc 75, 467–473 (2012).
Sharaiha, R. Z. et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc 85, 904–914 (2017).
Paik, W. H. et al. EUS-Guided Biliary Drainage Versus ERCP for the Primary Palliation of Malignant Biliary Obstruction: A Multicenter Randomized Clinical Trial. Am J Gastroenterol 113, 987–997 (2018).
Park, J. K. et al. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc (2018).
Bang, J. Y., Navaneethan, U., Hasan, M., Hawes, R. & Varadarajulu, S. Stent placement by EUS or ERCP for primary biliary decompression in pancreatic cancer: a randomized trial (with videos). Gastrointest Endosc 88, 9–17 (2018).
Tsuchiya, T. et al. Long-term outcomes of EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction: a prospective multicenter study. Gastrointest Endosc 87, 1138–1146 (2018).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151, W65–94 (2009).
Park, D. H. et al. EUS-guided biliary drainage with one-step placement of a fully covered metal stent for malignant biliary obstruction: a prospective feasibility study. Am J Gastroenterol 104, 2168 (2009).
Dhir, V. et al. Multicenter comparative evaluation of endoscopic placement of expandable metal stents for malignant distal common bile duct obstruction by ERCP or EUS-guided approach. Gastrointest Endosc 81, 913–923 (2015).
Khashab, M. A. et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: an international comparative study. Endosc Int Open 4, E1322 (2016).
Nakai, Y. et al. Indications for endoscopic ultrasonography (EUS)‐guided biliary intervention: Does EUS always come after failed endoscopic retrograde cholangiopancreatography? Dig Endosc 29, 218–225 (2017).
Tonozuka, R., Itoi, T., Sofuni, A., Itokawa, F. & Moriyasu, F. Endoscopic double stenting for the treatment of malignant biliary and duodenal obstruction due to pancreatic cancer. Dig Endosc 25, 100–108 (2013).
Hamada, T. et al. Transmural biliary drainage can be an alternative to transpapillary drainage in patients with an indwelling duodenal stent. Dig Dis Sci 59, 1931–1938 (2014).
Kawakubo, K. et al. Endoscopic ultrasound-guided choledochoduodenostomy vs. transpapillary stenting for distal biliary obstruction. Endoscopy 48, 164–169 (2016).
Hamada, T. et al. International study of endoscopic management of distal malignant biliary obstruction combined with duodenal obstruction. Scand J Gastroenterol 53, 46–55 (2018).
Yamao, K. et al. Outcomes of endoscopic biliary drainage in pancreatic cancer patients with an indwelling gastroduodenal stent: a multicenter cohort study in West Japan. Gastrointest Endosc (2018).
Nakai, Y. et al. Prospective multicenter study of primary EUS-guided choledochoduodenostomy using a covered metal stent. Endoscopic ultrasound (2018).
Duval, S. & Tweedie, R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 95, 89–98 (2000).
Giovannini, M. et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 33, 898–900 (2001).
Wang, K. et al. Assessment of efficacy and safety of EUS-guided biliary drainage: a systematic review. Gastrointest Endosc 83, 1218–1227 (2016).
Leonardo Frazzoni, L. F. Alberto Larghi. EUS-guided biliary drainage versusERCP for the primary treatment ofmalignant distal biliary obstruction:time for a large randomized study. Gastrointest Endosc 88, 571–572 (2018).
Conio, M., Demarquay, J.-F., De Luca, L., Marchi, S. & Dumas, R. Endoscopic treatment of pancreatico-biliary malignancies. Crit Rev Oncol Hematol 37, 127–135 (2001).
Anderloni, A. et al. Single-stage EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction. Gastrointest Endosc (2018).
Park, D. H. et al. Feasibility and safety of a novel dedicated device for one‐step EUS‐guided biliary drainage: A randomized trial. J Gastroenterol Hepatol 30, 1461–1466 (2015).
Oh, D. et al. Optimal biliary access point and learning curve for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting. Therap Adv Gastroenterol 10, 42–53 (2017).
Hara, K. et al. Endoscopic ultrasonography-guided biliary drainage: Who, when, which, and how? World J Gastroenterol 22, 1297 (2016).
Elmunzer, B. J. et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med 366, 1414–1422 (2012).
Choudhary, A. et al. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc 73, 275–282 (2011).
Acknowledgements
The authors thank Nakai Y. (University of Tokyo, Tokyo, Japan), Kawakubo K. (Hokkaido University, Sapporo, Japan), and Dhir V. (Asian Cancer Institute, Mumbai, India) for providing additional data from their studies.
Author information
Authors and Affiliations
Contributions
Study concept and design: Do Hyun Park, Dong Uk Kim. Acquisition of data: Sung Yong Han, Hoonsub So, Euisoo Shin. Statistical analysis and interpretation of data: Seon-Ok Kim, Sung Yong Han. Drafting of the manuscript: Sung Yong Han, Hoonsub So, Dong Uk Kim, Do Hyun Park. Critical revision: Dong Uk Kim, Do Hyun Park. Approval of the final draft submitted: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Han, S.Y., Kim, SO., So, H. et al. EUS-guided biliary drainage versus ERCP for first-line palliation of malignant distal biliary obstruction: A systematic review and meta-analysis. Sci Rep 9, 16551 (2019). https://doi.org/10.1038/s41598-019-52993-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52993-x
This article is cited by
-
Role of Endoscopic Ultrasound in the Management of Pancreatic Cancer
Indian Journal of Surgical Oncology (2024)
-
Pancreaticoduodenectomy after bilirubin adsorption for distal cholangiocarcinoma with severe obstructive jaundice refractory to repeat preoperative endoscopic biliary drainage: a case report
Clinical Journal of Gastroenterology (2024)
-
Role of therapeutic endoscopic ultrasound in gastrointestinal malignancy- current evidence and future directions
Clinical Journal of Gastroenterology (2022)
-
Multicenter study of lumen-apposing metal stents with or without pigtail in endoscopic ultrasound-guided biliary drainage for malignant obstruction—BAMPI TRIAL: an open-label, randomized controlled trial protocol
Trials (2022)
-
EUS-Guided Versus ERCP-Guided Biliary Drainage for Primary Treatment of Distal Malignant Biliary Obstruction
Current Treatment Options in Gastroenterology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.