Abstract
Recent studies have reported that takotsubo syndrome (TTS) patients are suffering from life-threatening arrhythmias. The aim of our study was to understand the short and long-term usefulness of cardiac implantable electronic devices in TTS patients.We constituted a collective of 142 patients in a bi-centric study diagnosed with TTS between 2003 and 2017. The patient groups, divided according to the treatment with (n = 9, 6.3%) or without cardiac devices (n = 133, 93.7%), were followed-up to determine the importance of devices and its complications. One patient was treated with a permanent pacemaker, five patients with a wearable cardioverter defibrillator, two patients with a subcutaneous defibrillator and one patient with a transvenous defibrillator. Regular device check-up was documented in all patients, presenting an ongoing high-degree AV-block. Neither device complications nor life-threatening tachyarrhythmias were documented after acute TTS event. However, patients comprising the device group suffered significantly more often from a highly reduced EF (30 ± 7.7% versus 39.1 ± 9.7%; p < 0.05), cardiogenic shock with use of inotropic agents (66.6% versus 16.6%; p < 0.05) and cardiopulmonary resuscitation (44.4% versus 5.3%; p < 0.05). Our data confirm the usefulness of pacemaker in TTS patients. However, the cardioverter defibrillator including wearable cardioverter defibrillator may not be recommended.
Similar content being viewed by others
Introduction
Takotsubo syndrome (TTS) is characterized by an acute heart failure syndrome and associated with a bevy of adverse events1,2,3,4,5. Four forms of TTS according to affected wall motion changes have been described1,3,6,7,8. Despite the reversibility of TTS recently published data have described a comparable outcome with ACS3,9. The declined outcome is reflected by TTS associated complications including arrhythmias. It has been debated that life-threatening arrhythmias are common in up to 14% of TTS cases and related to QTc interval prolongation10,11,12.The management of arrhythmias in TTS challenges physicians based on the reversible character.
The present study aimed to investigate the role of cardiac implantable electronic devices (CiED) in TTS syndrome and long-term follow-up of its importance and associated complications.
Methods
We recruited 142 patients diagnosed with TTS between January 2003 and September 2017 at the Medical Faculty of Mannheim and University of Frankfurt. The diagnosis TTS was reviewed by two independent experienced cardiologists on the basis of the Mayo Clinic Criteria13,14.
The study protocol received ethics approval from the Ethics Committee of the Medical Faculty Mannheim, University of Heidelberg4. The need for informed consent was waived by the ethics committee. All methods were performed in accordance with the relevant guidelines and regulations.
Cases were divided into two groups according the use of CiED including transient and permanent pacemaker, transvenous ICD, subcutaneous ICD and wearable cardioverter defibrillator or not. CiED was recommended due to the occurrence of life-threatening arrhythmias (encompassing ventricular tachycardia, ventricular fibrillation as well as complete atrioventricular block) and the persistence of reduced ejection fraction (EF) at discharge, all of which were assessed by ECG and echocardiography independently reviewed by two experienced cardiologists prior admission, at admission or during hospital stay. Evaluation the rate of recurrence of life-threatening arrhythmias at short- and long-term was conducted using chart review and medical records.
Different TTS related complications and the outcome of patients including arrhythmias with use of device therapy, thromboembolic events, pulmonary congestion with the need for ventilation, cardiogenic shock and subsequent use of inotropic agents were assessed at TTS event and over follow-up by chart-review and telephone review. The cause of death was evaluated using the above mentioned assessments. Unknown cause of death was defined in cases with unclear cause of death.
Statistics
SPSS statistics 23.0 was used for statistical analysis. Continuous variables with normal distribution and non-continuous variables not normal normal distribution were presented as means ± standard deviation or median with interquartile range, which have been compared using student’s t-test and the Mann–Whitney U-test. A frequency (%) was used for categorical variables and compared using Chi-squared-test or Fisher’s exact test. Statistical significance was defined as a p value ≤ 0.05.
Results
Baseline demographics
We studied the clinical and echocardiographic data of 142 TTS patients. Of these, in 9 (6.3%) patients device implantation was undertaken. The indication for CiED implantation was as following; ventricular fibrillation (n = mp2), torsade de pointes (n = 2), completely atrioventricular-Block (n = 1), and highly reduced EF at discharge (n = 4). The baseline characteristics of patients, who received a CiED are illustrated in Table 1.
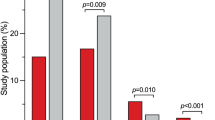
In-hospital complications
Patients treated with CiED suffered more frequently of in-hospital complications; Table 2. Cardiogenic shock was more frequently documented in the CiED group (66.6%) as compared to the non-CiED group (16.6%); p < 0.01. Consequently, the use of positive inotropic drugs was significantly higher in the device group (55.5% versus 16%; p = 0.01). Cardiopulmonary resuscitation (44.4% versus 5.5%; p < 0.01) was significantly more presented in the device group. Patients treated with CiED tended to stay longer in the hospital than patients without CiED treatment (8.3 ± 6.0 versus 4.5 ± 6.0 days; p = 0.07). Other TTS related complications including respiratory support and intubation were similarly documented in both groups.
CiED implantations and follow-up
Pacemaker
One TTS patient presented an apical form. The same patient was admitted to the hospital two years later due to recurrent syncope. Echocardiography and coronary angiography presented a recurrent TTS. This patient received a temporary pacemaker at admission. Due to persistent bradycardia and atrioventricular block III, a permanent pacemaker implantation was done. Regular device check-ups over 8 years presented ongoing bradycardia and AV-block III. No complications have been documented.
Transvenous ICD
One patient was admitted from a referral hospital due to bradycardia and hypoglycemia. One day after admission torsade de pointes has been documented and terminated with a cardioversion (Fig. 1C). A coronary angiography excluded relevant stenosis. However, echocardiography and laevocardiography presented a biventricular TTS form of apical form. CiED implantation was undertaken. Ongoing regular device-follow-up showed no more bradycardia or life-threatening arrhythmia. Additionally no complications have been documented over the follow-up.
Subcutaneous ICD
Subcutaneous ICD (s-ICD) has been implanted in two patients. The first patient was admitted to the hospital for a coloscopy. During coloscopy cardiopulmonary resuscitation because of ventricular fibrillation was required (Fig. 1A). Cardiac MRI, coronary angiography and echocardiography showed a midventricular TTS. Due to recurrent ventricular fibrillation defibrillation was performed eight times. Because of the recurrent ventricular fibrillation ICD implantation was undertaken. During the follow-up of 2 years no complications or life-threatening arrhythmias have been documented.
The second patient was a 22 years old female. The patient was admitted to the hospital due ventricular fibrillation. ECG documentation presented a long QT syndrome. Additionally, an old ECG recorded 4 years ago documented a prolonged QTc interval. There was no family history of sudden cardiac death. In-hospital diagnostics showed a highly reduced EF. Cardiac MRI confirmed an apical TTS form. A recovery of EF has been documented in the hospital. This patient underwent subcutaneous ICD implantation due to a suspected congenital long QT syndrome. Neither complications nor arrhythmias have been documented over 3 months of follow-up.
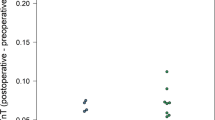
Wearable cardioverter defibrillator
A wearable cardioverter defibrillator was used in five TTS patients due to a highly reduced left ventricular EF. Almost three months later a recovery of EF was documented. However, one female patient (17 year old) underwent an s-ICD implantation due to a suspected congenital long QT-syndrome. No complications or life-threatening arrhythmias have been documented during the follow-up.
Table 3 illustrates a detailed follow-up of TTS treated with CiED.
Discussion
Using our retrospective clinical investigation of 142 TTS patients, we are able to conclude that: (i) the use of CiED in TTS might be safe; (ii) the long-term need for pacemaker in TTS is higher as compared to ICD; (iii) due to the recovery of EF a wearable cardioverter defibrillator might be not required in TTS patients
TTS has been thought to be associated with a favorable prognosis. Recently published data have shown a similar outcome of TTS and ACS. TTS related complications including arrhythmias and acute heart failure have been reported10,11,15. Up to 14% of TTS patients may suffered from lifethreatening arrhythmias and triggered by a QTc interval prolongation. The management of such complication remains challenging physicians due to the reversible character of TTS and absence of risk stratification strategies.
Our study is the largest, to the best of our knowledge, which describes the use of permanent and temporary CiED in TTS.
Stiermaier et al. has described a higher in-hospital and one-year mortality rate of TTS patients associated with life-threatening arrhythmias including ventricular fibrillation, ventricular tachycardia and complete atrioventricular block11. It has been reported that one patient was treated by ICD implantation and one patient was discharged with a wearable cardioverter defibrillator. Follow-up did not record any relevant arrhythmias16. Here we report about the use of wearable cardioverter-defibrillator in 5 patients and s-ICD in 2 patients. No arrhythmias have been documented over long-term follow-up. One young patient treated with a wearable cardioverter defibrillator has undergone an s-ICD due to a congenital long QT. All these data suggest a consensus that cardioverter defibrillator including wearable cardioverter defibrillator are not recommended in TTS patients. The higher vulnerability of myocardial muscle to develop ventricular arrhythmias at TTS event might be explained by oedema2. Another important trigger for ventricular arrhythmias is the acquired long-QT syndrome. Long QT syndrome is associated with sudden cardiac death. Recently published data of a TTS model using induced pluripotent stem cells showed that estradiol attenuates the acquired long-QT syndrome17, consistent with the clinical observation that TTS occurs frequently in postmenopausal women. Of note, in our current study, we found a concomitant long QT syndrome and TTS at the same time. Both patients were young. Therefore, a congenital channelopathy should be evaluated using family screening and genetic screening.
Cardiac arrest could be in presented in TTS patients in absence of QT prolongation. The main mechanism for this finding might be related to catecholamine toxicity. In other cases TTS might be the results of cardiac arrest and cardiopulmonary resuscitation18.
The reversible character of wall motion abnormality of TTS may explain the uncertain value of cardioverter defibrillators (ICD and wearable life-vest) as showed in our study19. In contrast, our findings in one patient with permanent pacemaker showed that a permanent device might be required in TTS patients with bradycardia or atrioventricular block. Our data are comparable with the study of Stiermaier et al. on the use of pacemaker in TTS patients.
The ongoing susceptibility to fatal bradyarrhythmias in TTS patients after index-event and lower-susceptibility to fatal tachyarrhythmias after the acute TTS event might be explained by the recommended medication (beta-blockers) at discharge. Beta-blockers suppress ventricular tachyarrhythmias, but nervertheless decrease the heart rate and might be the cause for permanent pacing of pacemakers. We have recently presented in our TTS model that beta-blockers shorten the action potential duration consisting with a shortening of QT-interval and reducing the arrhythmia risk.
Study limitations
This study is a bi-centric retrospective case series study with a low number of patients and without a comparative control group. Therefore the non-significant comparison values of baseline characteristics should be evaluated with caution. Magnetic resonance imaging was not performed systematically to find a possible interaction between remnant edema and/or inflammation and life-threatening arrhythmias. The use of electrophysiology work-up to stratify the risk of ventricular tachyarrhythmias in TTS patients was not evaluated.
Conclusions
Permanent CiED implantation might be recommended in cases of bradyarrhythmias. The use of temporary and permanent cardioverter defibrillator is not recommended in TTS patients. More data on management of life-threatening arrhythmias are necessary to provide a general recommendation.
References
Dote, K., Sato, H., Tateishi, H., Uchida, T. & Ishihara, M. [Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol 21, 203–214 (1991).
Eitel, I. et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 306, 277–286, https://doi.org/10.1001/jama.2011.992 (2011).
Templin, C. et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 373, 929–938, https://doi.org/10.1056/NEJMoa1406761 (2015).
El-Battrawy, I. et al. Prevalence, Clinical Characteristics, and Predictors of Patients with Thromboembolic Events in Takotsubo Cardiomyopathy. Clin Med Insights Cardiol 10, 117–122, https://doi.org/10.4137/CMC.S38151 (2016).
El-Battrawy, I., Borggrefe, M. & Akin, I. Atrial fibrillation as a risk factor for worse outcome in acute coronary syndrome. Int J Cardiol 246, 53, https://doi.org/10.1016/j.ijcard.2017.05.065 (2017).
Ghadri, J. R. et al. Differences in the Clinical Profile and Outcomes of Typical and Atypical Takotsubo Syndrome: Data From the International Takotsubo Registry. JAMA Cardiol 1, 335–340, https://doi.org/10.1001/jamacardio.2016.0225 (2016).
Suzuki, K. et al. An atypical case of “Takotsubo cardiomyopathy” during alcohol withdrawal: abnormality in the transient left ventricular wall motion and a remarkable elevation in the ST segment. Intern Med 43, 300–305 (2004).
Kato, K., Sakai, Y., Ishibashi, I. & Kobayashi, Y. Transient focal left ventricular ballooning: a new variant of Takotsubo cardiomyopathy. Eur Heart J Cardiovasc Imaging 16, 1406, https://doi.org/10.1093/ehjci/jev218 (2015).
Redfors, B. et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction - A report from the SWEDEHEART registry. Int J Cardiol 185, 282–289, https://doi.org/10.1016/j.ijcard.2015.03.162 (2015).
Madias, C. et al. Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm 8, 555–561, https://doi.org/10.1016/j.hrthm.2010.12.012 (2011).
Stiermaier, T. et al. Prevalence and Clinical Significance of Life-Threatening Arrhythmias in Takotsubo Cardiomyopathy. J Am Coll Cardiol 65, 2148–2150, https://doi.org/10.1016/j.jacc.2015.02.062 (2015).
Stiermaier, T. et al. Incidence, determinants and prognostic relevance of cardiogenic shock in patients with Takotsubo cardiomyopathy. Eur Heart J Acute Cardiovasc Care, https://doi.org/10.1177/2048872615612456 (2015).
Madhavan, M. & Prasad, A. Proposed Mayo Clinic criteria for the diagnosis of Tako-Tsubo cardiomyopathy and long-term prognosis. Herz 35, 240–243, https://doi.org/10.1007/s00059-010-3339-x (2010).
Prasad, A., Lerman, A. & Rihal, C. S. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 155, 408–417, https://doi.org/10.1016/j.ahj.2007.11.008 (2008).
El-Battrawy, I. et al. Incidence and Prognostic Relevance of Cardiopulmonary Failure in Takotsubo Cardiomyopathy. Sci Rep 7, 14673, https://doi.org/10.1038/s41598-017-15327-3 (2017).
Stiermaier, T. et al. Management of arrhythmias in patients with Takotsubo cardiomyopathy: Is the implantation of permanent devices necessary? Heart Rhythm, https://doi.org/10.1016/j.hrthm.2016.06.013 (2016).
El-Battrawy, I. et al. Estradiol protection against toxic effects of catecholamine on electrical properties in human-induced pluripotent stem cell derived cardiomyocytes. Int J Cardiol 254, 195–202, https://doi.org/10.1016/j.ijcard.2017.11.007 (2018).
Ghadri, J. R. et al. International Expert Consensus Document on Takotsubo Syndrome (Part II): Diagnostic Workup, Outcome, and Management. Eur Heart J 39, 2047–2062, https://doi.org/10.1093/eurheartj/ehy077 (2018).
Migliore, F. et al. Incidence and management of life-threatening arrhythmias in Takotsubo syndrome. Int J Cardiol 166, 261–263, https://doi.org/10.1016/j.ijcard.2012.09.107 (2013).
Author information
Authors and Affiliations
Contributions
Ibrahim El-Battrawy, Julia W. Erath, Siegfried Lang, Xiaobo Zhou, Uzair Ansari, Martin Borggrefe and Ibrahim Akin designed the research and wrote the paper; Ibrahim El-Battrawy, Ibrahim Akin, Thorsten Gietzen, Uzair Ansariand Michael Behnes performed the clinical research; Ibrahim El-Battrawy, Siegfried Lang, Xiaobo Zhou, Julia W. Erath, Thorsten Gietzen and Ibrahim Akin analyzed data.
Corresponding author
Ethics declarations
Competing interests
Julia W. Erath reports receiving consultant fees, travel support and lecture fees from ZOLL Medical, travel grants from Bayer Vital, St. Jude Medical/Abbott, Novartis and lecture fees from Servier and Bayer and was a fellow of the Boston Scientific heart rhythm fellowship program.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Battrawy, I., Erath, J.W., Lang, S. et al. Takotsubo syndrome and cardiac implantable electronic device therapy. Sci Rep 9, 16559 (2019). https://doi.org/10.1038/s41598-019-52929-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52929-5
This article is cited by
-
Takotsubo pathophysiology and complications: what we know and what we do not know
Heart Failure Reviews (2023)
-
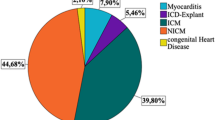
Real life experience with the wearable cardioverter-defibrillator in an international multicenter Registry
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.