Abstract
Idiopathic dilated cardiomyopathy (DCM) is a common cardiomyopathy with the prevalence of 1:250, and at least one-third of all the cases are inherited. Mutations in the TTN gene are considered as the most frequent cause of inherited DCM and cover 10–30% of the cases. The studies were mainly focused on the adult or mixed age group of patients with DCM. The mutation rate in the TTN gene, the characteristics of manifestations and their prognostic significance in childhood have not been studied. To determine TTN mutation rate in children with DCM and the relevance of including this gene in the DNA diagnostic protocol for paediatric DCM, complete clinical and instrumental examination of 36 DCM patients (up to 18 years) with the manifestation of the disease was conducted in specialised cardiology centres. Molecular genetic testing included sequencing of coding and adjacent regulatory regions of the major cardiac TTN isoform N2BA using IonTorrent ™ semiconductor sequencing (for 25 isolated cases) and trio whole exome sequencing (trio WES)on the Illumina platform (for 11 family cases). Our pilot group included 36 probands with DCM diagnosis first established on the basis of the generally accepted criteria at the age of 5 days to 18 years(average age: 6.5 years). The sex ratio (M:F) was 23: 8. There were 25 sporadic DCM cases and 11 cases of familial DCM (at least one of the parents and/or siblings were also diagnosed with DCM). The only likely pathogenic truncating variant p.Arg33703*in the TTN gene (TTNtv) was found in a 16-year-oldmale proband out of 36 (3%). Apparently, TTN-dependent forms of DCMs manifest later at a young (but older than 18 years) or more mature age, and TTN gene cannot be considered as the first-line genetic testing for DCM in the paediatric group, despite several studies have reported a generally high mutation rate in this gene with DCM. Further research is needed to compare the representation of mutations in the TTN gene in different age groups of DCM patients.
Similar content being viewed by others
Introduction
Dilated cardiomyopathy (DCM) is one of the common hereditary diseases, with the prevalence of 1: 250 as estimated by Hershberger et al.1. The annual incidence of this disease in children was 0.57 cases per 100 000 per year overall in the USA alone; DCM detection rate in other countries was also similar2.
DCM may develop under the influence of genetic (primary) or non-genetic (secondary) factors, the frequency of primary forms in the paediatric group of patients reaches 70%2,3. DCM in children is characterised by rapid progression and high mortality4. For paediatric patients, the five-year probability of death or heart transplantation is 46%2. As little is known about the causes, including genetic ones, of DCM in children, the treatment protocols largely represent adapted protocols for the treatment of adult patients, and their effectiveness is limited. For the radical management of progressive heart failure in children and adults, orthotopic heart transplantation (not available in all countries) and mechanical circulatory support devices5 are currently used. It is therefore not surprising that during the medical genetic counselling for this severe and steadily progressive disease, the parents have important questions about verifying the genetic diagnosis, knowing the risk of giving birth to a child with this disease, and the prospects of pre-symptomatic (including prenatal) diagnosis and pre-implantation genetic screening (PGS). However, assisted reproductive treatment can be offered to a family only if the pathogenic mutation has been identified.
Among all primary cardiomyopathies, the approaches to DCM DNA testing are the least developed. In 2011, the expert consensus recommendations for the genetic diagnosis of cardiomyopathies and channelopathies stated that none of the known genes was responsible for >5% of primary DCM cases, there was no protocol for priority DNA testing6. In 2016, ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure pointed out the TTN gene as the most frequent genetic cause of primary DCM7. First, this situation is associated with exceptional genetic diversity of DCM. At least 50 genes have a significant role in DCM development; however, the contribution of each gene to the structure of the disease has not been studied enough8. A small but consistently detectable proportion of mutations was shown only for mutations in the SCN5A and LMNA genes for a particular clinical DCM variant accompanied by atrioventricular (AV) conduction impairment (5–10% each) and the TTN gene6. However, the genetic structure of this disease is poorly studied, and the mutations in each gene are not identified because of the large variety of genes and the absence of frequent mutations. Only with the development of new generation sequencing methods (NGS), large-scale genetic studies of this disease were conducted. The only gene in which mutations account a significant proportion of DCM probands - the TTN gene encoding titin sarcomeric protein.
Before the introduction of NGS methods, the TTN gene was poorly studied because of its large size8. But several studies have shown that mutations in this gene are the leading cause of DCM8,9,10,11,12. According to various estimates, from 10 to 30% of DCM cases are caused by mutations in the TTN gene2,11. The first estimates of the prognostic value of detecting mutations in this gene were performed on several patients with identified mutations. The survival and long-term prognosis of DCM patients may depend on the genetic form of the disease13. In addition, TTN gene mutations have incomplete penetrance, and in DCM patients, a titin mutation is often aggravated by pathogenic variants in other DCM-related genes14.
Previous researches were mainly focused on the adult or mixed age group of patients with DCM15. Only a few studies investigated the spectrum of mutations in the paediatric and adolescent groups of patients16. The TTN mutation rate, the characteristics of manifestations and their prognostic significance in childhood were not thoroughly studied.
Aim
The aim of the study was to determine the TTN mutation rate in paediatric patients with DCM and to assess the relevance of the inclusion of this gene into the DNA diagnostics protocol.
Materials and Methods
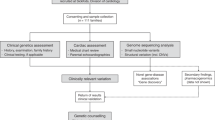
Complete clinical and instrumental examination of the patients were performed in accordance with diagnostic protocol at the specialised cardiology and cardiac surgery centres and departments where children with DCM were diagnosed and/or observed. Genetic counselling and molecular genetic research were performed in accordance with the principles of the Declaration of Helsinki, informed consent for genetic testing was given by the parents or guardians of the minor patients. The informed consent included DNA diagnostics and using the results of the study for publishing. The results do not violate the confidentiality of patients and could not be used to identify them.
Molecular genetic analysis was conducted on the DNA extracted from the venous blood samples or from paraffin blocks (in three cases, DNA testing was performed post- mortem) with standard reagent kits. For 25 probands (sporadic cases, the only patient in family), sequencing of coding and adjacent regulatory regions of major cardiac TTN isoform N2BA using IonTorrent ™ semiconductor sequencing was performed.
For 11 probands (family cases) and their parents, trio whole exome sequencing (trio WES) on the Illumina platform was performed. Capillary Sanger re-sequencing was performed for the fragments with low coverage and for the confirmation of the identified genetic variants.
All genetic variants annotated by original software were analysed with open bioinformatics tools.
We used PolyPhen, Mutation Taster, SIFT, FATHMM, HSF, Cardio Classifier and Atlas of Cardiac Genetic Variation Database (https://www.cardiodb.org)17,18,19,20,21,22.
For primary analysis of sequencing results we used IGV (Interactive Genomic Viewer), and variant tables were created by IonRep software23. Every variant found was proof-checked in online genome browser (UCSC browser) and variant databases (dnSNP, gnomAD)24,25,26. Genetic variant with the frequency >1% was not considered as potentially pathogenic. Human Splicing Finder and NetGene2 were used to assess the potential impact on splicing27,28.
Ethical approval
This study was performed in accordance with the 1964 Helsinki declaration, its later amendments and local ethics committee.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Results and Discussion
The study group included 36 probands diagnosed with DCM first established on the basis of the generally accepted criteria at the age of 5 days to 18 years (in one case, DCM with the left ventricular non-compaction was diagnosed prenatally at the period of 30 weeks of gestation); the average age was 6.5 years. The sex ratio (M:F) was 23: 8. There were 25 sporadic DCM cases and 11 cases of familial DCM (at least one of the parents and/or siblings was also diagnosed with DCM). Clinical phenotype of patients at the time of the first consultation is summarized in the Table 1 (supplementary).
On the basis of the published reports of a significant (up to 30%) frequency of pathogenic genetic variants in the TTN gene3,8 that lead to shortened protein isoform development, we were expected to detect at least 6–8 mutations in the examined group. However, the only one truncating variant p.Arg33703* was found in a cohort of patients with paediatric DCM.
The carrier of this variant was diagnosed with DCM at 16 years. The main complaint was palpitation caused by PVC. The left ventricle (LV) was slightly enlarged (EDD (end diastolic volume) LV 57 mm) with decreased ejection fraction (EF LV 45%), but the tolerance to the physical exercise was preserved. This variant was also found in the proband’s mother (41 y.o.) with syncope, DCM, heart failure (NYHA IV), pulmonary hypertension, supraventricular and ventricular arrhythmia (Fig. 1A).
(A) Stop-gain variant carrier family tree. I.2–41 y.o., DCM, Heart failure (HF) NYH III-IV; II.1–16 y.o., DCM, HF NYH II; Mut* - c.101107 C > T (p.Arg33703Ter). (B) Fragment of the Sanger sequencing chromatogram with heterozygous C > T substitution. (C) Titin protein scheme and its alignment with the regions of the sarcomere. p.Arg33703Ter location is shown.
This is a heterozygous variant ENST00000589042.1:c.101107 C > T p.Arg33703* located at exon 359 in the IC isoform (exon 308 for N2BA isoform) (Fig. 1B,C). This variant is extremely rare (MAF 0,00001797 in the gnomAD) and is registered in the dbSNP database (rs766265889); however, no clinical data are available. Exon 359 translates within the M-disc of the sarcomere and encodes 9 domains (Ig-like 142–148, fibronectin-type III 132 and protein kinase domains). The exon is asymmetric, and its PSI (Proportion Spliced In) is 100% in DCM patients. rs766265889 has two entries in ClinVar database (one of which is our submission), and there are a number of other truncating variants mapped in exon 359 with p.Asp33700fs as the most closely located (https://www.cardiodb.org/titin/titin_exon.php?id=359). The location of the exon within M-disc, its large size and multi-domain composition, asymmetry and PSI allows us to treat p.Arg33703Ter as a likely pathogenic finding, but the exact role of the p.Arg33703Ter has to be elucidated.
Generally, deletions leading to a frameshift result in a premature termination codon and are considered pathogenic by default. But the clinical interpretation of genetic variants found in the TTN gene is very complex because of the enormous size of the protein and the objective difficulty of performing functional analysis of mutations, and also the high frequency of occurrence of premature termination codons and mutation splicing in healthy population, which reaches 2–3%1,8. It has been shown that the clinical effect of mutations, even leading to premature termination codons and changes in splicing sites, strongly depends on which domain of the protein they affect. Currently, the focus is on genetic variants with a more unambiguous effect on the protein – splicing mutations and nonsense mutations.
The bioinformatics research showed that the pathogenicity of a variant in the TTN gene depends on how widely the exon with the mutation is represented in all isoforms of the protein and which domain it affects15. Pathogenic mutations are grouped by gene segments corresponding to specific structures in the protein molecule in the composition of the sarcomere12. A significant portion of premature termination codons qualified as pathogenic are localised in the C-terminal domain of the cardiac-specific isoforms and translating within A-disc or M-disc of the sarcomere12,29.
The results of this study were somewhat unexpected: a single mutation in the TTN gene was detected in patients with DCM diagnosed before the age of 18 years. These data can only partly be explained by the limited size of the sample or ethnic characteristics of the Russian group of patients. Our results are consistent with those of D. Fatkin et al., where only a small number of TTNtv are found in the group of 82 children with DCM including one de novo mutation16.
The structure of the genetic causes of DCM is different at different ages. Apparently, TTN-dependent forms of DCM manifest later, at a young (but over 18 years) or at a more mature age. Data on the genotype–phenotype correlation with DCM are insufficient. Studies on the mid-term survival of DCM patients showed that mutations in the TTN gene are not associated with deterioration in the prognosis compared with other patients with DCM15. Data have shown that patients with TTN-mediated DCM have a better prognosis compared with LMNA-dependent cardiomyopathy considering the rate of heart failure progression and the high risk of life-threatening ventricular arrhythmias28,30,31. However, in all the cases, the discussion was about the examined groups of patients with the average age of clinical manifestation of DCM at 40–50 years13,16,30 which, compared with the paediatric group, is certainly a better prognosis.
Conclusion
The absence of pathogenic substitutions in patients with DCM manifestation at an age less than 18 years indicates the possibility of the existence of different genetic causes of DCM in different age groups. In addition, this suggests a more favourable course of TTN-mediated forms of DCM compared to childhood forms of the disease. The pathogenic role of the TTN mutations should be assessed with caution. From the results of this study, the TTN gene cannot be considered as a first-line genetic test for DCM in the paediatric group, despite several studies have reported a generally high mutation rate in this gene with DCM. Further research is needed to compare the representation of TTN mutations in different age groups of patients with DCM.
References
Hershberger, R. E., Hedges, D. J. & Morales, A. Dilated cardiomyopathy: the complexity of a diverse genetic architecture. Nat Rev Cardiol. 10(9), 531–47 (2013).
Rusconi, P. et al. For the Pediatric Cardiomyopathy Registry Investigators. Differences in Presentation and Outcomes between Children with Familial Dilated Cardiomyopathy and Children with Idiopathic Dilated Cardiomyopathy: A Report from the Pediatric Cardiomyopathy Registry Study Group. Circ Heart Fail. 10(2), e002637 (2017).
Maron, B. J. et al. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 113(14), 1807–16 (2006).
Bollen, I. A. E. et al. Cardiomyocyte hypocontractility and reduced myofibril density in end-stage pediatric cardiomyopathy. Front Physiol. 8, 1103 (2017).
Everitt, M. D. et al. Recovery of echocardiographic function in children with idiopathic dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. J Am Coll Cardiol. 63(14), 1405–13 (2014).
Ackerman, M. J. et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm 13(8), 1077–109 (2011).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 18(8), 891–975 (2016).
Herman, D. S. et al. Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med. 366(7), 619–28 (2012).
Dellefave, L. & McNally, E. M. The genetics of dilated cardiomyopathy. Curr Opin Cardiol. 25(3), 198–204 (2010).
Gigli, M. et al. A Review of the Giant Protein Titin in Clinical Molecular Diagnostics of Cardiomyopathies. Front Cardiovasc Med. 3, 21 (2016).
Verdonschot, J. A. J. et al. Titin cardiomyopathy leads to altered mitochondrial energetics, increased fibrosis and long-term lifethreatening arrhythmias. Eur Heart J. 39(10), 864–873 (2018).
Franaszczyk, M. et al. Titin truncating variants in dilated cardiomyopathy —prevalence and genotype-phenotype correlations. PLoS One. 12(1), e0169007 (2017).
Tobita, T. et al. Genetic basis of cardiomyopathy and the genotypes involved in prognosis and left ventricular reverse remodeling. Sci Rep. 8(1), 1998 (2018).
Haas, J. et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J. 36(18), 1123–35 (2015).
Tayal, U. et al. Phenotype and clinical outcomes of titin cardiomyopathy. J Am Coll Cardiol. 70(18), 2264–74 (2017).
Fatkin, D. et al. Titin truncating mutations: A rare cause of dilated cardiomyopathy in the young. Progress in Pediatric Cardiology 40, 41–45 (2016).
Roberts, A. M. et al. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci. Transl. Med. 7, 270ra6, https://www.cardiodb.org/titin/index.php (2015).
Sunyaev, S. R., Adzhubei, I. & Jordan, D. M. Predicting Functional Effect of Human Missense Mutations Using PolyPhen-2. Curr Protoc Hum Genet. Jan; 0 7: Unit7.20, https://omictools.com/polyphen-tool (2013).
Schwarz, J. M., Cooper, D. N., Schuelke, M. & Seelow, D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat Methods. Apr; 11(4):361–2, http://www.mutationtaster.org/ (2014).
Ngak-Leng, S. et al. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Research, Volume 40, Issue W1, 1 July, Pages W452–W457, https://sift.bii.a-star.edu.sg/ (2012).
Shihab, H. A. et al. Predicting the Functional, Molecular and Phenotypic Consequences of Amino Acid Substitutions using Hidden Markov Models. Hum. Mutat. 34, 57–65, http://fathmm.biocompute.org.uk/ (2013).
Whiffin, N. et al. CardioClassifier: disease- and gene-specific computational decision support for clinical genome interpretation. Genetics in Medicine volume 20, pages 1246–1254, https://www.cardioclassifier.org/ (2018).
Robinson, J. T. et al. Integrative Genomics Viewer. Nature Biotechnology 29, 24–26 https://igv.org/ (2011).
Kent, W. J. et al. The human genome browser at UCSC. Genome Res. Jun 12(6), 996–1006, https://genome.ucsc.edu/index.html (2002).
Sherry, S. T. et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. Jan 1;29(1):308–11, https://www.ncbi.nlm.nih.gov/snp/ (2001).
Karczewski, K. J. et al. Variation across 141,456 human exomes and genomes reveals the spectrum of loss-of-function intolerance across human protein-coding genes. bioRxiv Jan.28, https://doi.org/10.1101/531210v3, https://gnomad.broadinstitute.org (2019).
Desmet, F. O. et al. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acid Research, http://www.umd.be/HSF3/ (2009)
Hebsgaard, S. M. et al. Splice site prediction in Arabidopsis thaliana DNA by combining local and global sequence information, Nucleic Acids Research Vol. 24, No. 17, 3439–3452. http://www.cbs.dtu.dk/services/NetGene2/ (1996).
Gerull, B. et al. Identification of a novel frameshift mutation in the giant muscle filament titin in a large Australian family with dilated cardiomyopathy. J. Mol. Med. 84, 478–83 (2006).
Tayal, U. et al. Truncating variants in titin independently predict early arrhythmias in patients with dilated cardiomyopathy. J Am Coll Cardiol Lett. 69(19), 2466–8 (2017).
Taylor, M. et al. Genetic variation in titin in arrhythmogenic right ventricular cardiomyopathy – overlap syndromes. Circulation. 124(8), 876–85 (2011).
Acknowledgements
This study was supported by grant of Russian Research Foundation 16-15-10421.
Author information
Authors and Affiliations
Contributions
S. Dzemeshkevich – project supervision, patients selection, clinical evaluation and follow-up, manuscript editing and proof outline. A. Dombrovskaya - clinical evaluation of patients, manuscript editing. N. Kotlukova – patients selection, clinical evaluation and follow-up. A. Bukaeva and V.Kaimonov – NGS sequencing, discussing the data. A. Bukaeva and I. Povolotskaya – bioinformatic analysis, genetic data processing. V. Mikhailov – writing the manuscript, Sanger resequencing, cascade familial screening, pooling the data together, preparing the illustrations. E. Zaklyazminskaya – designing the study, writing the manuscript, patients selection, genetic counseling, proof outline.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zaklyazminskaya, E., Mikhailov, V., Bukaeva, A. et al. Low mutation rate in the TTN gene in paediatric patients with dilated cardiomyopathy – a pilot study. Sci Rep 9, 16409 (2019). https://doi.org/10.1038/s41598-019-52911-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52911-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.