Abstract
Non-neuronal ATP released from the urothelium in response to bladder stretch is a key modulator of bladder mechanosensation. Whilst non-neuronal ATP acts on the underlying bladder afferent nerves to facilitate sensation, there is also the potential for ATP to act in an autocrine manner, modulating urothelial cell function. The aim of this study was to systematically characterise the functional response of primary mouse urothelial cells (PMUCs) to ATP. PMUCs isolated from male mice (14–16 weeks) were used for live-cell fluorescent calcium imaging and qRT-PCR to determine the expression profile of P2X and P2Y receptors. The majority of PMUCs (74–92%) responded to ATP (1 μM–1 mM), as indicted by an increase in intracellular calcium (iCa2+). PMUCs exhibited dose-dependent responses to ATP (10 nM–1 mM) in both calcium containing (2 mM, EC50 = 3.49 ± 0.77 μM) or calcium free (0 mM, EC50 = 9.5 ± 1.5 μM) buffers. However, maximum iCa2+ responses to ATP were significantly attenuated upon repetitive applications in calcium containing but not in calcium free buffer. qRT-PCR revealed expression of P2X1–6, and P2Y1–2, P2Y4, P2Y6, P2Y11–14, but not P2X7 in PMUCs. These findings suggest the major component of ATP induced increases in iCa2+ are mediated via the liberation of calcium from intracellular stores, implicating functional P2Y receptors that are ubiquitously expressed on PMUCs.
Similar content being viewed by others
Introduction
As the bladder fills, bladder afferents embedded within the detrusor smooth muscle and urothelium provide signals relating the degree of bladder distension into spino-bulbo-spinal reflexes responsible for maintaining continence and supraspinal nuclei for sensory processing1,2. Although there are subtypes of bladder afferents that are considered to be tension receptors, thereby directly transducing bladder stretch into neuronal activation3, a role for adenosine 5′-triphosphate (ATP) released from the urothelium in response to bladder stretch has also been identified in modulating bladder mechanosensation4.
ATP is released from urothelial cells in-vitro and in-vivo in response to cell or bladder stretch5,6,7,8, and significant increases in the levels of urothelial ATP release have been detected in pre-clinical models of spinal cord injury, feline interstitial cystitis, and cyclophosphamide induced cystitis9,10,11,12. Furthermore, enhanced ATP release is also seen from bladder strips isolated from patients with interstitial cystitis/bladder pain syndrome and neurogenic and idiopathic detrusor overactivity13,14,15. The mechanism underlying ATP release from the urothelium has been shown to integrate both traditional vesicular mechanisms9,16, as well as direct release via pannexin and connexin channel proteins17,18. A number of studies, however, have shown that urothelial ATP release is controlled by a rise in intracellular calcium concentrations, with agents that interfere with intracellular calcium entry or the liberation of inositol triphosphate (IP3) able to block stretch induced ATP release9,10,19,20,21,22,23. As ATP is released from urothelial cells during stretch and acts on the underlying afferent nerves, there is also the potential for ATP to act in an autocrine manner, modulating urothelial cell function24,25,26.
Two functional subclasses of membrane bound P2 purinergic receptors (P2X and P2Y) mediate the extracellular actions of ATP27. Functional P2X and P2Y purinergic receptors have been identified in mouse, rat, and guinea pig urothelial cells, as well as human urothelial cell lines26,28,29,30. P2X receptors (P2X1-P2X7) are ionotropic ligand gated ion-channels, which with the exception of P2X7, are characterised by rapid activation and fast inactivation31. P2Y receptors (P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, P2Y14), in contrast, are classic metabotropic G-protein coupled receptors (GPCRs), coupling with Gq/11, Gs and Gi proteins to either activate phospholipase C and release intracellular calcium or bind adenylyl cyclase to modulate cAMP levels27. A range of studies, using various techniques and urothelium from cats, rats, and humans have provided evidence that the urothelium expresses a comprehensive repertoire of purinergic receptor subtypes, including P2X1–7, and P2Y1,2,46,28,29.
The precise role of autocrine purinergic signalling within urothelial cells has yet to be fully determined, however, the maintenance of intracellular calcium homeostasis and further release of neuromodulators is a key consideration. Despite this, only a limited number of studies have systematically explored calcium signalling in urothelial cells. Activation of purinergic receptors upon the urothelium evokes an increase in intracellular calcium which induces acetylcholine release24 as well as auto-feedback to influence ATP release itself13. Uridine 5′-triphosphate (UTP) has also been shown to significantly enhance ATP release via intracellular calcium pathways26,28 indicating that P2Y receptors are an essential component of the urothelial purinergic signalling system.
In this study we provide the first systematic characterisation of extracellular and intracellular calcium contributions to the urothelial response to ATP using primary mouse urothelial cells (PMUCs). Furthermore, we provide the first quantified expression profile of P2X and P2Y receptors in PMUCs and found that intracellular calcium contributes the majority of the functional calcium response to ATP in these cells, implicating P2Y receptors that couple to GPCRs.
Results
Immediately following plating of the PMUCs onto collagen coated coverslips, the cells were randomly dispersed (Fig. 1A). After 30 minutes, the urothelial cells from the same coverslip had migrated to form a continuous single sheet of cells (Fig. 1B). Primary cultures were confirmed to be of urothelial origin through positive staining with the transitional epithelial cell marker cytokeratin 7 (Fig. 1C).
Primary mouse urothelial cells. (A) Light microscope images of PMUCs immediately following isolation and plating on collagen IV coated coverslips, and (B) after 30 minutes in an incubator (37 °C, 95/5% O2/CO2). Cells migrate towards each other forming a cell layer. (C) Representative confocal image of urothelial cells 24 hrs after isolation incubated with both primary (CK7) and secondary antibodies (AF488) and mounted with Prolong Gold Antifade with nuclei staining positive for 4′6-diamidino-2-phenylindole (DAPI). Cells were excited with 495-nm that emits fluorescence at 505- to 534-nm. Scale bar, 20 μm.
Exposure of individual PMUCs to ATP (10 μM) induced a significant rise in intracellular calcium (iCa2+) levels, as reflected by an increase in the fluorescent emissions ratio during continuous application (Fig. 2A). PMUCs responded to ATP with variable sensitivity, but the iCa2+ response was generally characterised by two distinct phases. There was an initial rapid rise in iCa2+ followed by a brief rapid decay, and a more sustained level of iCa2+, which was maintained until ATP was removed and a rapid return to baseline calcium levels was observed (Fig. 2A).
ATP activates urothelial cells. (A) Representative trace of a calcium imaging experiment reveals that ATP (10 μM) is able to induce sustained intracellular calcium entry in PMUCs that returns to baseline following washout. Each coloured line represents an individual urothelial cell from a single experiment. (B) Group data shows urothelial responses to ATP (10 nM–1 mM) are dose dependent with little or no response to 10–100 nM ATP, but sustained intracellular calcium responses to 1 μM, 10 μM, 100 μM, 1 mM (N = 6, n = 37–76 per concentration, Mean ± SEM). (C) Non-linear fit of PMUCs peak response to ATP reveal an EC50 value of 3.49 ± 0.77 µM ATP (N = 6). (D) Less than 20% of PMUCs respond to 10–100 nM ATP, whereas 74–92% of PMUC’s respond to 1 μM to 1 mM ATP.
PMUC iCa2+ responses to ATP were concentration dependent (Fig. 2B,C). Whilst the majority of PMUCs (74–92% of cells/coverslip) respond to high concentrations of ATP (1 μM–1 mM), relatively few (12–20% of cells/coverslip) respond to low concentrations of ATP (10–100 nM) with robust iCa2+ transients (Fig. 2D). Responses to ATP are maximal at 100 μM with no further increases upon application of 1 mM ATP (Fig. 2B,C). The EC50 for ATP evoked iCa2+ responses in urothelial cells was 3.49 ± 0.77 μM.
As ATP release from the urothelium is stimulus dependent, such that increases in bladder stretch would evoke a graded increase in ATP concentrations around urothelial cells, we wanted to test the response of PMUCs to repeated applications of ATP. The rise in iCa2+ during application of ATP returned to baseline immediately following washout. A subsequent dose of ATP at the same concentration to the same cells also initiated a significant rise in iCa2+ (Fig. 3A,B). However, when directly comparing the peak of the 1st and 2nd iCa2+ responses to ATP, we observed that the second response, although robust, was significantly attenuated compared to the first response (Fig. 3C). Furthermore, the kinetics of the intracellular calcium response to ATP were altered, with a significant increase in the time taken to reach peak calcium fluorescence with the second ATP application (Fig. 3D).
PMUCs respond to repeated applications of ATP. (A) ATP (10 μM) evokes a sustained increase in intracellular calcium in PMUCs that rapidly returns to baseline following washout. A second application of ATP also evokes sustained intracellular calcium entry (N = 3, n = 67). (B) Representative trace of PMUC calcium fluorescence shows individual responses to repeated application of ATP (10 μM). Each line represents and individual urothelial cell from a single experiment. (C) The 2nd response to ATP had a significantly lower peak intracellular calcium entry than the 1st response to ATP (0.22 ± 0.01 vs. 0.15 ± 0.007 Rf340/380, N = 3, n = 67 ***P ≤ 0.001, paired Students t-test). (D) The time taken to reach peak intracellular calcium entry is significantly greater during the second response to ATP compared to the first response (15.3 ± 1.4 vs. 19.5 ± 2.4 seconds, N = 3, *P < 0.05, paired Students t-test).
To determine the relative contribution of calcium release from intracellular stores to the PMUC response to ATP, we investigated the response to ATP in a calcium free buffer (Fig. 4). Whilst application of ATP in calcium free buffer evoked a dose dependent increase in iCa2+ above baseline (Fig. 4A), there was a rightward shift in the concentration-response curve to ATP in calcium free buffer and a reduction in the EC50 from 3.49 ± 0.77 μM in 2 mM Ca2+ to 9.5 ± 1.5 μM in 0 mM Ca2+ buffer (Fig. 4A). The time taken to reach peak iCa2+ fluorescence was also significantly increased in calcium free buffer compared to control solution (Fig. 4B). A closer look at the initial kinetics of the urothelial response to ATP in calcium free buffer reveals a significantly slower increase in iCa2+ compared to ATP responses in calcium containing buffer. Because PMUCs took longer to reach peak iCa2+ in response to ATP in calcium free buffer, the characteristic two phase iCa2+ response seen in control experiments was less obvious, instead replaced by a response which did not exhibit an initial sharp peak (Fig. 4C,D). The maximal intracellular calcium response to ATP in the absence of calcium was significantly reduced compared to control 2 mM calcium buffer (Fig. 4E). Moreover, when comparing duplicate applications of ATP in calcium free buffer, we show that maximum iCa2+ responses are not significantly reduced between the 1st and 2nd incubations with ATP (Fig. 4D,E). Additionally, we also observed that the maximal response to ATP in calcium free buffer is similar to the 2nd incubation with ATP in normal calcium buffer (Fig. 4E).
ATP evokes intracellular calcium responses in calcium free buffer. (A) Dose response of PMUCs to ATP (10 nM–1 mM) in normal calcium containing extracellular buffer (2 mM) and calcium free buffer (0 mM). PMUCs exhibit a dose-dependent increase in intracellular calcium in nominal calcium buffer, but the EC50 to ATP is reduced compared to nominal calcium conditions (3.49 ± 0.77 vs. 9.5 ± 1.5 μM, N = 6, n = 314–360). (B) The time taken for ATP (10 μM) to induce peak intracellular calcium in 0 mM calcium buffer is significantly longer than when cells are exposed to ATP (10 μM) in normal 2 mM calcium buffer (15.3 ± 1.4 s Vs 23.3 ± 1.9 s, N = 3, n = 62 **P ≤0 0.01 unpaired t-test). (C) The initial kinetics of the intracellular calcium response to ATP (10 μM), calculated by linear regression of the initial slope, is dramatically reduced in the absence of extracellular calcium 0.022 ± 0.0025 Vs 0.0058 ± 0.0007015 dRf/dTime (s) (N = 3, n = 67, n = 62). (D) In calcium free buffer, ATP (10 μM) evokes a sustained increase in intracellular calcium in PMUC’s that rapidly returns to baseline following removal of ATP. A second application of ATP in calcium free buffer evokes a sustained intracellular calcium entry (N = 3, n = 62). (E) Peak evoked intracellular calcium responses to 10 μM ATP were significantly reduced in calcium free buffer (0.22 ± 0.01 vs. 0.17 ± 0.01 Rf340/380, N = 3, n = 67, n = 62 ***P ≤ 0.001; one-way ANOVA with Tukey’s post-hoc multiple comparisons). Peak evoked intracellular calcium responses were not significantly reduced during duplicate applications of ATP (10 μM) in calcium free buffer (0.17 ± 0.01 vs. 0.16 ± 0.007 Rf340/380, N = 3, n = 62, ns P ≥ 0.05; one-way ANOVA with Tukey’s post-hoc multiple comparisons).
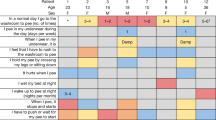
Membrane bound P2X and P2Y purinoceptors mediate the response to extracellular ATP27. Using qRT-PCR we show that PMUCs express almost the complete repertoire of purinergic P2 receptors, with the exception of P2X7 which was below the level of detection (Fig. 5). When comparing the expression of P2 receptors relative to the expression of P2Y1, we identified that P2X2 is the most ubiquitously expressed P2X receptor. The P2Y1 receptor was the highest expressed P2Y receptor, followed by P2Y2.
Urothelial cells express P2X and P2Y receptors: PMUCs express P2X and P2Y receptors. mRNA for P2X1-P2X6, and P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, and P2Y14 was expressed in PMUC’s. P2X7 transcript was below the detection limit (bdl) of the PCR assay. Data presented as expression relative to P2Y1 (N = 3).
Discussion
Extracellular responses to ATP are mediated by two functional subclasses of membrane bound P2 purinergic receptors, P2X and P2Y. P2X receptors (P2X1-P2X6) are ionotropic ligand gated ion-channels which show marked desensitisation following rapid activation31. P2Y receptors (P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, P2Y14), in contrast, are GPCRs, mediating effects via intracellular signalling pathways27. Data from the current study provide a number of novel findings that have implications for understanding the autocrine signaling of the bladder urothelium in response to ATP.
In this study we provide the first quantitative expression profile of P2X and P2Y receptors of the urothelium. We found the most significant expression of P2X2, P2X4, P2Y1 and P2Y2, as well as lesser expression of other purinergic receptor subtypes including P2Y6. There are many benefits in the use of PMUC’s versus a known urothelial cell line, however, a small possibility exists that our PMUC culture is not 100% pure. Nonetheless, our dissection and culture has been refined to ensure the highest purity, and this technique has been used extensively for the purpose of characterising functional urothelial responses5,8,30. In addition, our immunostaining for CK7 indicates that our PMUC culture is pure and our data is largely consistent with previous reports of urothelial purinergic receptor expression28,29,32,33. P2X7 mRNA was not detected in our study, consistent with a lack of expression in human urothelium29. P2X7 is predominantly expressed on cells of hematopoietic lineage as well as glial cells, Schwann cells and astrocytes34. An immunohistochemistry study of cat urothelium, has previously revealed significant P2X7 staining throughout the basal and apical layers of the urothelium6, however, more recent studies have identified the urothelium is prone to non-specific adsorption of antibodies35,36. To ultimately determine the precise molecular architecture of the purinergic receptors expressed on the urothelium, a comprehensive analysis using multiple complementary techniques, including qPCR, western blot, immunohistochemistry and in-situ hybridization will be required.
Using live cell calcium imaging, we have systematically characterised the functional response of primary mouse urothelial cells to ATP, revealing a key role for intracellular calcium stores in urothelial ATP responses. Consistent with our observations, a number of previous studies have shown functional responses to ATP in isolated urothelial cells from mouse, rat, and guinea pig26,28,29,30. In the current study, the urothelial response to ATP was characterised by a rapid rise in intracellular calcium, followed by sustained intracellular levels of calcium in the presence of the agonist. Following duplicate applications of sub-maximal ATP, and in a calcium free extracellular solution, the magnitude and kinetics of ATP evoked responses were altered. As the repeat sub-maximal doses of ATP were applied with only a short washout period, it is possible that the changes in the observed response are due to alterations in the function of urothelial purinergic receptors responsible for calcium influx. As P2X receptors undergo rapid desensitisation, it is likely that the reduction in response that we observed during duplicate application of ATP in calcium containing buffer is due to a desensitisation of these P2X receptors. P2X receptors also exhibit rapid activation kinetics, with direct influx of cations across the electrochemical gradient responsible for intracellular calcium influx. We, like others, found significant expression of the P2X2 receptor in the urothelium6,37,38, as well as expression of P2X1,3,4,5,6 which have also previously been identified within the urothelium6,37,38,39. Therefore, if these receptors are desensitised we would expect, and in this study observed, an increase in the time taken to reach peak intracellular calcium during a second application of ATP. Furthermore, the obvious differences in the rate of intracellular calcium rise that occurred in calcium free, compared to calcium containing buffer further implicate P2X receptors in the initial fast component of intracellular calcium influx in response to ATP. The relative abundance of P2X2 over other P2X receptors suggests this receptor may be a key integrator of this response, however, in a somewhat related function, P2X4 mediates ATP-induced calcium influx in response to fluid shear stress in human vascular endothelium40 and its role in urothelial evoked calcium influx cannot be currently ruled out. The P2X receptor isoforms mediating this initial ATP response requires further elucidation. Together these data support a mechanism whereby liberation of intracellular calcium via a slower G-protein coupled mechanism involving inositol triphosphate (IP3)41, rather than direct influx across the electrochemical gradient, may be responsible for the intracellular calcium influx in response to repeated applications of ATP27. P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, couple to phospholipase C and the liberation of intracellular calcium via IP3 and we, like others, identified the expression of these P2Y receptor subtypes within the urothelium6,26,28.
In further support of a P2Y mediated ATP response in the urothelium, we identified that ATP evoked increases in intracellular calcium persist even when cells are superfused in a calcium free extracellular solution. Removal of extracellular calcium from the perfusion buffer isolates the GPCR mediated P2Y receptor response from the ionotropic P2X component of calcium influx42, and thus provides additional evidence that a large proportion of the urothelial response to ATP is mediated by the liberation of calcium from intracellular stores rather than through membrane bound calcium channels. In addition, with repeated applications of ATP in the absence of extracellular calcium, there was no reduction in peak response or obvious change in response profile. In rat cultured urothelial cells, UTP, an agonist of P2Y receptors, has been shown to stimulate intracellular calcium rises via a phospholipase C-linked mechanism which was unaffected by extracellular calcium but significantly attenuated by store depletion26,28. Our study also provide some insight into the mechanisms responsible for urothelial calcium conductance. In normal calcium containing buffer, our data suggests extracellular calcium conductance provides the initial fast component of the intracellular calcium response to ATP, likely via non-selective P2X receptor cation channels, corroborating computational modelling and functional studies of urothelial cell calcium signalling that implicated extracellular channel currents43,44. During duplicate applications of ATP in calcium free buffer we observe calcium responses that are of equivalent magnitude in the first and second application, as well as a rapid return to baseline following ATP removal. These data suggest that after removal of ATP as a stimulus, intracellular calcium is not lost in significant amounts into the extracellular space and that intracellular calcium is rapidly and efficiently sequestered back into the endoplasmic reticulum for future use.
The ability of urothelial cells to respond to continuous or repeated stimuli with an increase in intracellular calcium, the known stimulus for distension evoked ATP release from the urothelium22,23, is essential to the proposed physiological role of urothelial signalling during bladder distension. The importance of ATP in providing autocrine modulation of intracellular calcium levels within the urothelium is implicated by the role of intracellular calcium, via the liberation of IP3, in mediating stretch evoked ATP release19,22,23, the ability of ATP to induce ATP release13, and the multitude of interactions that ATP has been proposed to mediate in the sub-urothelium relating to mechanosensitivity17,27,45,46,47. Thus, a mechanism by which the actions of ATP and its metabolites are able to mediate further ATP release could be an additional mechanism contributing to the enhancement in reflex bladder activity observed in a number of bladder disorders. Indeed, ATP release is enhanced from bladder strips isolated from neurogenic and idiopathic detrusor overactivity patients, as well as IC/BPS patients13,14,15, and an increased urinary content of ATP is observed in women with OAB48. Whilst this ATP is likely to be acting on underlying bladder afferent nerves49,50, bladder sensations could be further modified by autocrine actions of ATP on urothelial cells.
The presence of ectonucleotides in the urothelial layer51, which have the ability to breakdown ATP to adenosine-5′-diphosphate, a potent agonist of P2Y1, and results showing that both ADP and UTP are able to stimulate release of ATP52, have all provided further credibility to the theory that P2Y receptors have an essential role in urothelial function and ATP release. Intriguingly, the ATP metabolite adenosine, acting through P1 receptors has been shown to inhibit further ATP release and this was proposed to be through inhibition of intracellular calcium liberation19. A systematic assessment of the contribution of purinergic receptors in the response to ATP will be an important area for future investigation.
These results have shown for the first time that the major component of ATP induced increases in urothelial intracellular calcium are via the liberation of calcium from intracellular stores, implicating but not confirming functional P2Y receptors. In addition, these results provide the first complete expression profile of P2X and P2Y receptors on PMUCs. The control of urothelial intracellular calcium levels is a necessary factor in ATP release, and ATP release is an essential component in the control of micturition within the bladder.
Methods
The methods described have been used in previous studies and were performed as previously described5,8,53. Comprehensive details of the methods are provided to account for any minor variations in protocol.
Animals
The University of Sheffield Animal Care Committee (UK) approved experiments involving animals under a project license issued in accordance with the UK Animals (Scientific Procedures) Act 1986. Adult (14–16 weeks) C57BL/6J male mice were used in this study. Mice were group housed (5 mice/cage) in specific housing rooms within a temperature-controlled environment of 22 °C and a 12:12 hr light-dark cycle. Mice had free access to food and water at all time. All experiments were performed on cells isolated from mice that were humanely euthanized by cervical dislocation in accordance with the guidelines set-out by the UK Animals Act 19865,8.
Isolation of primary mouse urothelial cells (PMUCs)
Culture of primary mouse urothelial cells was performed as previously described5,8,30. Following cervical dislocation, bladders were excised from the mouse, dissected in sterile PBS and pinned urothelial side up in a SYLGARD™ coated dish. The bladder was incubated with 2.5 mg/ml Dispase dissolved in modified Eagle’s medium (MEM) media (Gibco) containing 1% antibiotic-antimycotic (PSF) solution (Gibco) and 0.7% Hepes (1 M) for 3 hrs at room temperature (21 °C). Cells were gently scraped from the urothelium using a blunt scalpel and dissociated in 0.025% trypsin-EDTA (Invitrogen) at 37 °C for 10 mins using gentle trituration with a Pasteur pipette at 5 and 10 minutes. The cell suspension was resuspended in MEM with 10% Fetal Bovine Serum (FBS) before centrifugation (15 min, 1,500 rpm, 4 °C). The MEM + FBS was aspirated and the cell pellet was resuspended in fresh keratinocyte serum free media (KSFM; Invitrogen) before being plated on collagen (IV) (Sigma-Aldrich) coated coverslips. Coverslips were left for 4 h in an incubator at 37 °C and 5% CO2 before flooding with KSFM (2 ml/well).
Calcium imaging of cultured urothelial cells
Calcium imaging of PMUC’s was performed as previously described5,8. Cultured urothelial cells (20–24 hrs) attached to coverslips were loaded with 2 μM Fura-2-acetoxymethyl ester (Fura-2AM; Sigma Aldrich) for 15 minutes in the dark at 37 °C. Coverslips were then placed in a washing well containing KSFM media at 37 °C for 15 minutes before being washed in HEPES buffer (Composition in mM (NaCl 142, NaHCO3 5, HEPES 10, Glucose 16, KCL 2, CaCl2 2, MgCl2 1, 0.1% BSA, 310 mOsm) at room temperature for 15 minutes before imaging. Coverslips containing cells were transferred to a perfusion chamber mounted on an inverted microscope (Axiovert S100 TV, Zeiss, Cambridge, UK) equipped with a 20x oil immersion objective (Zeiss). Cells were continually superfused with external HEPES solution at a rate of approximately 1.5 mL/min. Cells were alternately illuminated at 340 and 380 nm with a 20 msec exposure time (Polychrome IV, TILL Photonics, Munich, Germany). Emitted light was passed through a 510 nm band pass filter and collected by a 512B Cascade CCD camera (Photometrics, Tucson, AZ) and images were acquired at 0.5 Hz. MetaMorph imaging software (Molecular Devices, Sunnyvale, CA) was used to analyse all calcium imaging experiments.
Calcium imaging protocol
Cells for experiments carried out in normal calcium (2 mM) containing buffer were exposed to an individual concentration of ATP (10 nM–1 mM) for 60 seconds via continual perfusion. If a second dose of ATP was to be applied, a 3-minute washout with HEPES was allowed, followed by ATP at the same concentration for a further 60 seconds. Individual cells were easily discriminated based on fluorescent intensity under the microscope. For experiments in calcium free (0 mM) HEPES (Composition in mM (NaCl 142, NaHCO3 5, HEPES 10, Glucose 16, KCL 2, MgCl2 3, 0.1% BSA, 310 mOsm), recordings were started in calcium containing HEPES and switched to continual perfusion with calcium free HEPES during the recording period for two minutes prior to addition of ATP to ensure a complete switch in solution.
Immunohistochemistry of cultured urothelial cells
Immunohistochemistry and microscopy of cultured urothelial cells was performed as previously described5. Urothelial cells were labeled for transitional epithelium using monoclonal antibody cytokeratin 7 (CK7) (OV-TL 12/30; ThermoFisher). The details of the primary antibody used are in Table 1. Coverslips were washed with 0.1 M phosphate-buffered saline (PBS) three times and fixed with ice-cold 4% PFA at 4 °C for 45 minutes. Coverslips were washed with saponin 0.05% (Sigma-Aldrich) + 2% FBS in 0.1 M PBS (SF-PBS) to remove excess PFA and permeabilise cell membranes. Nonspecific binding of secondary antibodies was blocked with 3% bovine serum albumin diluted in 0.05% SF-PBS (Sigma-Aldrich) for 1 h. Coverslips were incubated with primary antisera and diluted in SF-PBS overnight (28 h) at 4 °C. Sections were then washed 3x in PBS and incubated in the dark for 2 h at room temperature with secondary antibody conjugated to Alexa Fluor. Cells were then washed in SF-PBS before mounting in Prolong Gold Antifade with DAPI (ThermoFisher Scientific) and coverslipped. Slides were allowed to dry for 24 h before visualization.
Microscopy
Fluorescence was visualized with a confocal laser scanning microscope (Leica TCS SP8X; Leica Microsystems, Wetzlar, Germany). Images (1,024 × 1,024 pixels) were obtained using a X63 lens (software zoom X1.3) X60 oil immersion objective, and sequential scanning (4- to 5-line average). Separation of fluorophores was achieved using white line laser tuned to 495-nm excitation and 505- to 534-nm emission detection settings for AF-488 and 405-nm excitation and 425- to 475-nm emission detection settings for DAPI. Confocal settings were optimized to reduce background staining by adjusting the white light laser intensity, emission window (as described above), and amplifier gain [726.7 offset: X0.07 (AF488); 10 offset: X0.1 (DAPI)]. These settings were saved and used for all imaging5.
qRT-PCR of urothelial cells
Following isolation of PMUC, cells were incubated at 37 °C in KSFM media for 24 hrs. mRNA from PMUC’s was isolated (RNAeasy minikit, Qiagen) and cDNA was synthesized by reverse transcription using superscript III (Invitrogen) from mRNA following the manufacturers protocol. cDNA was amplified by PCR for 35 cycles (Research Rotor-Gene 6000 real time thermocycler; Corbett-Qiagen) with forward and reverse primers (Table 2) and iQSYBR Green Master Mix (Biorad). Primers were designed as exon spanning with a product size of between 98–207 bp and Tm°C of less than 65 °C (Table 2). All PCR reactions were made up to a total of 25 μl, cyclic conditions were set at: 95 °C for 12 minutes as an initial hold stage followed by 40 cycles of 95 °C for 30 s, 59 °C for 30 s, 72 °C for 30 s, followed by a melt curve of 0.5 °C increments every 30 seconds from 72–95 °C. All samples were assayed in triplicate in the same plate. The relative amount of a target gene was calculated by the 2−ΔΔCt method using β-actin as a housekeeping gene.
Data analysis and statistics
PMUCs intracellular calcium flux was calculated as a ratio between the fluorescent signal at 340/380 nm (e.g. Rf 340/380) for responding cells. All data are presented as Mean ± SEM. Initial slope for urothelial activation kinetics was calculated using a linear regression of time from ATP application to max peak (Rf340/380). For qRT-PCR expression, levels of each target gene were calculated relative to the housekeeping gene, β-actin, and represented relative of P2Y1 receptor expression. Statistical analysis was carried out using either paired or un-paired Student’s t-test as appropriate. Statistical significance was confirmed at P < 0.05 using GraphPad Prism 7 software. (N = number of mice, n = number of cells)53.
Data availability
The datasets generated during and/or analysed during the study are available from the corresponding author on reasonable request.
References
Spencer, N. J. et al. Identifying unique subtypes of spinal afferent nerve endings within the urinary bladder of mice. Journal of Comparative Neurology 526, 707–720, https://doi.org/10.1002/cne.24362 (2018).
Fowler, C. J., Griffiths, D. & de Groat, W. C. The neural control of micturition. Nature reviews. Neuroscience 9, 453–466, https://doi.org/10.1038/nrn2401 (2008).
Grundy, L., Erickson, A. & Brierley, S. M. Visceral Pain. Annual Review of Physiology 81, null, https://doi.org/10.1146/annurev-physiol-020518-114525 (2019).
de Groat, W. C. & Yoshimura, N. Afferent nerve regulation of bladder function in health and disease. Handbook of experimental pharmacology, 91–138, https://doi.org/10.1007/978-3-540-79090-7_4 (2009).
Grundy, L. et al. NKA enhances bladder-afferent mechanosensitivity via urothelial and detrusor activation. American Journal of Physiology-Renal Physiology 315, F1174–F1185, https://doi.org/10.1152/ajprenal.00106.2018 (2018).
Birder, L. A. et al. Alterations in P2X and P2Y purinergic receptor expression in urinary bladder from normal cats and cats with interstitial cystitis. American Journal of Physiology-Renal Physiology 287, F1084–F1091, https://doi.org/10.1152/ajprenal.00118.2004 (2004).
Mansfield, K. J. & Hughes, J. R. Effect of inflammatory mediators on ATP release of human urothelial RT4 cells. Biomed Res Int 2014, 182862–182862, https://doi.org/10.1155/2014/182862 (2014).
Grundy, L., Daly, D. M., Chapple, C., Grundy, D. & Chess-Williams, R. TRPV1 enhances the afferent response to P2X receptor activation in the mouse urinary bladder. Scientific Reports 8, 197, https://doi.org/10.1038/s41598-017-18136-w (2018).
Birder, L. A. et al. Feline interstitial cystitis results in mechanical hypersensitivity and altered ATP release from bladder urothelium. American Journal of Physiology-Renal Physiology 285, F423–F429, https://doi.org/10.1152/ajprenal.00056.2003 (2003).
Smith, C. P., Vemulakonda, V. M., Kiss, S., Boone, T. B. & Somogyi, G. T. Enhanced ATP release from rat bladder urothelium during chronic bladder inflammation: effect of botulinum toxin A. Neurochemistry International 47, 291–297, https://doi.org/10.1016/j.neuint.2005.04.021 (2005).
Khera, M., Somogyi, G. T., Kiss, S., Boone, T. B. & Smith, C. P. Botulinum toxin A inhibits ATP release from bladder urothelium after chronic spinal cord injury. Neurochemistry International 45, 987–993, https://doi.org/10.1016/j.neuint.2004.06.001 (2004).
Smith, C. P. et al. Botulinum toxin type A normalizes alterations in urothelial ATP and NO release induced by chronic spinal cord injury. Neurochemistry International 52, 1068–1075, https://doi.org/10.1016/j.neuint.2007.11.006 (2008).
Sun, Y. & Chai, T. C. Augmented extracellular ATP signaling in bladder urothelial cells from patients with interstitial cystitis. American Journal of Physiology - Cell Physiology 290, C27–C34, https://doi.org/10.1152/ajpcell.00552.2004 (2005).
Kumar, V., Chapple, C. R., Rosario, D., Tophill, P. R. & Chess-Williams, R. In vitro release of adenosine triphosphate from the urothelium of human bladders with detrusor overactivity, both neurogenic and idiopathic. European Urology 57, 1087–1092, https://doi.org/10.1016/j.eururo.2009.11.042 (2010).
Kumar, V., Chapple, C. R., Surprenant, A. M. & Chess-Williams, R. Enhanced adenosine triphosphate release from the urothelium of patients with painful bladder syndrome: a possible pathophysiological explanation. The Journal of Urology 178, 1533–1536, https://doi.org/10.1016/j.juro.2007.05.116 (2007).
Knight, G. E., Bodin, P., De Groat, W. C. & Burnstock, G. ATP is released from guinea pig ureter epithelium on distension. American journal of physiology. Renal physiology 282, F281–288, https://doi.org/10.1152/ajprenal.00293.2000 (2002).
Beckel, J. M. et al. Pannexin 1 channels mediate the release of ATP into the lumen of the rat urinary bladder. The Journal of physiology 593, 1857–1871, https://doi.org/10.1113/jphysiol.2014.283119 (2015).
Sengiku, A. et al. Circadian coordination of ATP release in the urothelium via connexin43 hemichannels. Scientific Reports 8, 1996, https://doi.org/10.1038/s41598-018-20379-0 (2018).
Dunning-Davies, B. M., Fry, C. H., Mansour, D. & Ferguson, D. R. The regulation of ATP release from the urothelium by adenosine and transepithelial potential. BJU International 111, 505–513, https://doi.org/10.1111/j.1464-410X.2012.11421.x (2013).
Collins, V. M. et al. OnabotulinumtoxinA significantly attenuates bladder afferent nerve firing and inhibits ATP release from the urothelium. BJU International 112, 1018–1026, https://doi.org/10.1111/bju.12266 (2013).
Hanna-Mitchell, A. T. et al. Effect of botulinum toxin A on urothelial-release of ATP and expression of SNARE targets within the urothelium. Neurourology and Urodynamics, n/a-n/a, https://doi.org/10.1002/nau.22508 (2013).
Matsumoto-Miyai, K., Kagase, A., Murakawa, Y., Momota, Y. & Kawatani, M. Extracellular Ca2+ regulates the stimulus-elicited ATP release from urothelium. Autonomic Neuroscience 150, 94–99, https://doi.org/10.1016/j.autneu.2009.05.253 (2009).
Matsumoto-Miyai, K. et al. Store-operated Ca2+ entry suppresses distention-induced ATP release from the urothelium. American Journal of Physiology - Renal Physiology 300, F716–F720, https://doi.org/10.1152/ajprenal.00512.2010 (2011).
Hanna-Mitchell, A. T. et al. Non-neuronal acetylcholine and urinary bladder urothelium. Life Sciences 80, 2298–2302, https://doi.org/10.1016/j.lfs.2007.02.010 (2007).
Birder, L. A. Urothelial signaling. Autonomic Neuroscience 153, 33–40, https://doi.org/10.1016/j.autneu.2009.07.005 (2010).
Sui, G. et al. Purinergic and muscarinic modulation of ATP release from the urothelium and its paracrine actions. American Journal of Physiology - Renal Physiology 306, F286–F298, https://doi.org/10.1152/ajprenal.00291.2013 (2014).
Burnstock, G. Purinergic signalling. Br J Pharmacol 147(Suppl 1), S172–S181, https://doi.org/10.1038/sj.bjp.0706429 (2006).
Chopra, B. et al. Expression and function of rat urothelial P2Y receptors. American Journal of Physiology - Renal Physiology 294, F821–F829, https://doi.org/10.1152/ajprenal.00321.2006 (2008).
Shabir, S. et al. Functional expression of purinergic P2 receptors and transient receptor potential channels by the human urothelium. American Journal of Physiology - Renal Physiology 305, F396–F406, https://doi.org/10.1152/ajprenal.00127.2013 (2013).
Everaerts, W. et al. Functional characterization of transient receptor potential channels in mouse urothelial cells. American Journal of Physiology - Renal Physiology 298, F692–F701, https://doi.org/10.1152/ajprenal.00599.2009 (2010).
North, R. A. Molecular physiology of P2X receptors. Physiological Reviews 82, 1013–1067, https://doi.org/10.1152/physrev.00015.2002 (2002).
Timóteo, M. A. et al. ATP released via pannexin-1 hemichannels mediates bladder overactivity triggered by urothelial P2Y6 receptors. Biochemical Pharmacology 87, 371–379, https://doi.org/10.1016/j.bcp.2013.11.007 (2014).
Liu, M. et al. Epigallocatechin gallate attenuates interstitial cystitis in human bladder urothelium cells by modulating purinergic receptors. Journal of Surgical Research 183, 397–404, https://doi.org/10.1016/j.jss.2012.11.041 (2013).
Skaper, S. D., Debetto, P. & Giusti, P. The P2X7 purinergic receptor: from physiology to neurological disorders. The FASEB Journal 24, 337–345, https://doi.org/10.1096/fj.09-138883 (2010).
Yu, W. & Hill, W. G. Defining protein expression in the urothelium: a problem of more than transitional interest. American Journal of Physiology - Renal Physiology 301, F932–F942, https://doi.org/10.1152/ajprenal.00334.2011 (2011).
Everaerts, W. et al. Where is TRPV1 expressed in the bladder, do we see the real channel? Naunyn-Schmied Arch Pharmacol 379, 421–425, https://doi.org/10.1007/s00210-008-0391-7 (2009).
Studeny, S., Torabi, A. & Vizzard, M. A. P2X2 and P2X3 receptor expression in postnatal and adult rat urinary bladder and lumbosacral spinal cord. Am J Physiol Regul Integr Comp Physiol 289, R1155–R1168, https://doi.org/10.1152/ajpregu.00234.2005 (2005).
Svennersten, K., Hallén-Grufman, K., de Verdier, P. J., Wiklund, N. P. & Poljakovic, M. Localization of P2X receptor subtypes 2, 3 and 7 in human urinary bladder. BMC Urol 15, 81–81, https://doi.org/10.1186/s12894-015-0075-9 (2015).
Sun, Y. & Chai, T. C. Up-regulation of P2X3 receptor during stretch of bladder urothelial cells from patients with interstitial cystitis. J Urol 171, 448–452, https://doi.org/10.1097/01.ju.0000099660.46774.3c (2004).
Yamamoto, K., Korenaga, R., Kamiya, A. & Ando, J. Fluid Shear Stress Activates Ca2+ Influx Into Human Endothelial Cells via P2X4 Purinoceptors. Circulation Research 87, 385–391, https://doi.org/10.1161/01.RES.87.5.385 (2000).
von Kügelgen, I. Pharmacological profiles of cloned mammalian P2Y-receptor subtypes. Pharmacology & Therapeutics 110, 415–432, https://doi.org/10.1016/j.pharmthera.2005.08.014 (2006).
Dong, X. et al. P2Y receptors mediate Ca2+ signaling in duodenocytes and contribute to duodenal mucosal bicarbonate secretion. Am J Physiol Gastrointest Liver Physiol 296, G424–G432, https://doi.org/10.1152/ajpgi.90314.2008 (2009).
Appleby, P. A., Shabir, S., Southgate, J. & Walker, D. Cell-type-specific modelling of intracellular calcium signalling: a urothelial cell model. J R Soc Interface 10, 20130487–20130487, https://doi.org/10.1098/rsif.2013.0487 (2013).
Wu, C., Gui, G. P. & Fry, C. H. Intracellular Ca2+ regulation and electrophysiolgical properties of bladder urothelium subjected to stretch and exogenous agonists. Cell Calcium 49, 395–399, https://doi.org/10.1016/j.ceca.2011.03.008 (2011).
Nakagomi, H. et al. Urothelial ATP exocytosis: regulation of bladder compliance in the urine storage phase. Scientific reports 6, 29761–29761, https://doi.org/10.1038/srep29761 (2016).
Takezawa, K., Kondo, M., Nonomura, N., Shimada, S. & Urothelial, A. T. P. Signaling: what is its role in bladder sensation? Neurourol Urodyn 36, 966–972, https://doi.org/10.1002/nau.23099 (2017).
Birder, L. A. et al. How does the urothelium affect bladder function in health and disease? ICI-RS 2011. Neurourol Urodyn 31, 293–299, https://doi.org/10.1002/nau.22195 (2012).
Silva-Ramos, M. et al. Urinary ATP may be a dynamic biomarker of detrusor overactivity in women with overactive bladder syndrome. PLoS ONE 8, e64696, https://doi.org/10.1371/journal.pone.0064696 (2013).
Cockayne, D. A. et al. Urinary bladder hyporeflexia and reduced pain-related behaviour in P2X3-deficient mice. Nature 407, 1011–1015 (2000).
Vlaskovska, M. et al. P2X3 knock-out mice reveal a major sensory role for urothelially released ATP. The Journal of Neuroscience 21, 5670–5677 (2001).
Yu, W., Robson, S. C. & Hill, W. G. Expression and distribution of ectonucleotidases in mouse urinary bladder. PLoS ONE 6, e18704, https://doi.org/10.1371/journal.pone.0018704 (2011).
Mansfield, K. J. & Hughes, J. R. P2Y receptor modulation of ATP release in the urothelium. Biomed Res Int 2014, 830374–830374, https://doi.org/10.1155/2014/830374 (2014).
Grundy, L. Non-Neuronal ATP: Regulation of Release and action in the bladder. Doctoral Thesis, Bond University, Gold Coast, Australia (2014).
Acknowledgements
The majority of the work contained in this manuscript appears within the Doctoral Thesis of Dr. Luke Grundy entitled Non-Neuronal ATP: Regulation of Release and Action in the Bladder (Bond University, Gold Coast, Australia, 2014). S.M.B. is a National Health and Medical Research Council of Australia (NHMRC) R.D. Wright Biomedical Research Fellow (APP1126378). Work funded in part by NHMRC Australia Project Grants (#1139366 and #1140297 to S.M.B.).
Author information
Authors and Affiliations
Contributions
L.G. performed the experiments, analysed data, and prepared the manuscript. L.G., R.C.W., D.J.S., and D.G. designed the research study and obtained funding. All authors contributed essential scientific input and corrections to the manuscript during preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chess-Williams, R., Sellers, D.J., Brierley, S.M. et al. Purinergic receptor mediated calcium signalling in urothelial cells. Sci Rep 9, 16101 (2019). https://doi.org/10.1038/s41598-019-52531-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52531-9
This article is cited by
-
TGR5 agonists induce peripheral and central hypersensitivity to bladder distension
Scientific Reports (2022)
-
Exploring the Therapeutic Potential of Targeting Purinergic and Orexinergic Receptors in Alcoholic Neuropathy
Neurotoxicity Research (2022)
-
Hypersensitivity of bladder low threshold, wide dynamic range, afferent fibres following treatment with the chemotherapeutic drugs cyclophosphamide and ifosfamide
Archives of Toxicology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.