Abstract
Cardiovascular disease (CVD) remains the leading cause of death in chronic kidney disease (CKD) patients despite treatment of traditional risk factors, suggesting that non-traditional CVD risk factors are involved. Trimethylamine-N-oxide (TMAO) correlates with atherosclerosis burden in CKD patients and may be a non-traditional CVD risk factor. Serum TMAO concentrations are significantly increased in CKD patients, which may be due in part to increased hepatic flavin monooxygenase (FMO)-mediated TMAO formation. The objective of this work was to elucidate the mechanism of increased FMO activity in CKD. In this study, FMO enzyme activity experiments were conducted in vitro with liver microsomes isolated from experimental CKD and control rats. Trimethylamine was used as a probe substrate to assess FMO activity. The FMO activator octylamine and human uremic serum were evaluated. FMO gene and protein expression were also determined. FMO-mediated TMAO formation was increased in CKD versus control. Although gene and protein expression of FMO were not changed, metabolic activation elicited by octylamine and human uremic serum increased FMO-mediated TMAO formation. The findings suggest that metabolic activation of FMO-mediated TMAO formation is a novel mechanism that contributes to increased TMAO formation in CKD and represents a therapeutic target to reduce TMAO exposure and CVD.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) events are the leading cause of death in chronic kidney disease (CKD) patients despite aggressive treatment of traditional risk factors1, suggesting that non-traditional CVD risk factors may play an important role2,3. Trimethylamine-N-oxide (TMAO) promotes atherosclerosis in preclinical models4, is elevated and associated with CVD in CKD patients5,6,7, and may be a novel non-traditional CVD risk factor8. For instance, we have shown that circulating TMAO concentrations are 30-fold higher in patients with end-stage kidney disease (ESKD) than in the general population and correlate with coronary atherosclerosis burden9. Elevated TMAO concentrations may also directly contribute to fibrosis and non-ischemic heart failure in CKD10,11,12. TMAO concentrations increase disproportionately from Stage 4 to 5 CKD (i.e., 20 μM to 94 μM) compared to Stage 1 to 3 CKD (i.e., 3.3 μM to 10 μM)7,9, strongly implicating formation of TMAO as a contributor to elevated serum TMAO concentrations in advanced CKD. Recently, we demonstrated that enhanced hepatic flavin monooxygenase (FMO)-mediated TMAO formation along with decreased renal clearance contributes to increased TMAO exposure in a mouse model of experimental kidney disease13. However, the mechanism driving increased TMAO formation remained unclear.
Mechanistic evaluation of increased TMAO formation could shed light on novel therapeutic strategies for the prevention of CVD in CKD. In fact, recent studies provide proof of principle that FMO activity is a potential therapeutic target14. In mice, antisense oligonucleotide-mediated knockdown of FMO3 (the primary isoform responsible for TMAO formation in humans) leads to decreases in serum TMAO concentrations and atherosclerosis formation15,16. Therapeutically targeting FMOs may be particularly effective in the setting of increased FMO-mediated TMAO formation as seen in diabetes and CKD13,15,17.
The objective of this study was to elucidate potential mechanisms of increased hepatic FMO-mediated TMAO formation observed in CKD. We accomplished this by conducting FMO enzyme activity experiments with CKD and control rat microsomal fractions. We also investigated potential changes in mRNA and protein expression of FMOs.
Results
Characteristics of CKD and control rats
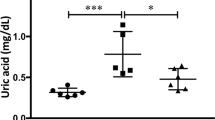
TMAO exposure was compared between CKD and control rats. The median (interquartile range) TMAO concentration in CKD versus control serum was 58 µM (31–102) and 3.4 µM (3.15–5.24), respectively (P = 0.0022; Fig. 1A). Serum creatinine and blood urea nitrogen (BUN) were also higher in CKD rats versus control (P < 0.0001; Fig. 1B).
FMO Activity and Serum TMAO Concentrations in CKD and Control Rats. (A) Serum concentrations of TMAO compared between CKD (n = 6) rats and controls (n = 6). #Serum TMAO concentrations were adjusted for kidney function by dividing individual TMAO concentrations by the corresponding serum creatinine (mg/dL) values. *P < 0.05 for CKD compared to control with a Mann-Whitney test. (B) Biochemical characteristics were compared between CKD (n = 12) and controls (n = 12) with a Student’s t-tests and presented as mean ± SD. (C) Michaelis-Menten plot for the formation of TMAO in rat liver microsomes of both control and CKD rats. Liver microsomal protein (0.5 mg/mL) was incubated with various concentrations of trimethylamine (2.5–1000 µM) for 60 min at 37 °C. Each point represents the mean ± SEM of 6 rats in each group. The parameters were statistically compared with an F-test.
FMO activity in CKD and control rats
The potential mechanism of altered FMO-mediated TMAO formation in CKD was assessed by comparing enzyme kinetic parameters observed in CKD rat liver microsomes with control rat microsomes. The Vmax (i.e., the maximal rate at which the enzyme catalyzes the reaction) for TMAO formation was increased by 25% in CKD versus control (651.4 ± 18 versus 522.7 ± 22 pmol/mg protein/minute, P < 0.0001; Fig. 1C). The Km value (i.e., substrate concentration at half the maximum velocity) was not different between groups (16.3 ± 2.3 versus 11.3 ± 2.5 μM, P = 0.15).
Gene and protein expression
In order to evaluate whether any changes in FMO activity were due to changes in gene or protein regulation, hepatic FMO mRNA and protein expression were assessed (Fig. 2A). No change in Fmo1 or Fmo3 mRNA was observed in CKD versus control. The positive control Cyp(Cytochrome P450)-3a2 was downregulated in CKD versus control (P < 0.0001). Ahr (aryl-hydrocarbon receptor) was upregulated in CKD versus control (P < 0.05) but Arnt (aryl hydrocarbon receptor nuclear translocator) and Cyp1a2 were not.
mRNA and Protein Expression. (A) mRNA expression of hepatic drug metabolism enzymes and related genes (Fmo3, Fmo1, Arnt, Ahr, Cyp1a2, Cyp3a2 and Actb) in control and CKD rats. Hepatic mRNA levels were normalized to β-Actin and expressed relative to the controls using absolute quantification. Experiments were conducted in duplicates, and results are presented as mean ± SD of 12 rats in each group. *P < 0.05 and **P < 0.001 compared with control by Student’s t-tests. (B) Protein expression of drug metabolism enzymes and related proteins (FMO3, AhR, CYP1A2, CYP3A2 and β-Actin) in control and CKD rat livers. The densitometry units of protein expression were normalized to that of β-Actin. The results are presented as mean ± SD of 12 rats in each group. The lower panel represents blots of six control and six CKD rats. *P < 0.05 and **P < 0.001 compared with control by Student’s t-tests. The corresponding full-length blots are presented in Supplementary Figures 2–5.
FMO3, CYP1A2, AhR and CYP3A2 protein expression is presented in Fig. 2B. Decreases in AhR (P < 0.01) and CYP3A2 (P < 0.001) but no change in FMO3 and CYP1A2 protein expression were observed in CKD versus control.
Metabolic activation and inhibition of FMO
An atypical kinetic reaction known as metabolic activation was explored as a potential mechanism of increased FMO activity. Concentration-dependent increases of up to 4-fold in metabolic activation were observed with octylamine as a positive activation control (P < 0.0001; Fig. 3A). L-arginine was evaluated to identify potential representative endogenous compounds responsible for activation; up to a 1.4-fold increase in metabolic activation was observed in the presence of L-arginine (P < 0.0001; Fig. 3B). FMO-mediated TMAO formation was decreased by 58% (P < 0.0001; Fig. 3C) in the presence of the FMO inhibitor methimazole. Lastly, FMO activity was determined in the presence 5–20% ultra-filtered human serum to assess whether solutes retained in ESKD can activate FMO enzymes. TMAO formation velocity was increased up to 3-fold with uremic serum compared to 1.9-fold with healthy control serum (P < 0.0001; Fig. 4).
Metabolic Activation and Inhibition of FMO. Michaelis-Menten plot for the formation of TMAO in rat liver microsomes in the presence of increasing concentrations of (A) octylamine and (B) L-arginine. Liver microsomal protein (0.5 mg/mL) was incubated with various concentrations of trimethylamine (2.5–1000 µM) for 60 min at 37 °C in the presence of either octylamine (0.01–2 mM) or L-arginine (0.5 and 2 mM). Each point represents the mean of at least 3 replicates at each trimethylamine concentration in each group. The parameters were statistically compared with an F-test. Note that P value represents a comparison of Vmax for each octylamine or L-arginine concentration versus control. (C) FMO-mediated TMAO formation was also assessed in the presence of the FMO inhibitor methimazole. Liver microsomal protein (0.5 mg/mL) was incubated with 50 µM of trimethylamine for 60 min at 37 °C in the presence of 1 mM of methimazole. Each point represents the mean ± SD of 5 replicates. *P < 0.001for treatment group compared to control by Student’s t-test.
Metabolic Activation of FMO-mediated TMAO Formation by Human Serum. Michaelis-Menten plots for the formation of TMAO in rat liver microsomes in the presence of increasing percentages of (A) human uremic serum and (B) healthy control serum. Liver microsomal protein (0.5 mg/mL) was incubated with various concentrations of trimethylamine (2.5–1000 µM) for 60 min at 37 °C in the presence of serum (5–20%). Each point represents the mean of at least 3 replicates at each trimethylamine concentration in each group. The parameters were statistically compared with an F-test. Note that P value represents a comparison of Vmax for each percent ultra-filtered serum group versus control.
Discussion
We show for the first time that metabolic activation of hepatic FMOs leads to increased formation of the non-traditional CVD risk factor TMAO, which may contribute to dramatically elevated serum concentrations in CKD rats. These findings corroborate our clinical observations of significantly elevated systemic TMAO concentrations in patients with advanced CKD and provide a novel mechanism for our recent observations of enhanced FMO-mediated TMAO formation in experimental CKD9,13.
Mechanistically, metabolic activation of FMO enzymes by uremic solutes may contribute to increased TMAO formation in CKD. In fact, metabolic activation likely contributes to the increased systemic exposure of TMAO observed in CKD, evidenced by disproportionate increases of serum TMAO in advanced CKD relative to earlier stages of CKD. For instance, TMAO serum concentrations are increased 16-fold in CKD rats (Fig. 1B), and 30-fold in ESKD patients compared to controls9. The Vmax of TMAO formation was increased by 25% (P < 0.0001; Fig. 1A) in CKD versus control tissue in the isolated microsomal incubation experiments. However, no changes in FMO gene or protein expression (Fig. 2A,B) were observed, suggesting that increased FMO activity was unrelated to changes in expression. The latter finding is inconsistent with our previous observations in mice, in which gene expression changes may partially explain differences in FMO activity13, but is not unexpected given well-known species differences in FMO3 regulation in mice compared to rats and humans18. For instance, FMO3 expression is also profoundly decreased by testosterone in mice but this effect is less clear in rats and humans19,20. Therefore, the current experimental rat model may better reflect FMO3 regulation and metabolic activity observed in humans with CKD. Furthermore, changes in FMO3 mRNA and protein expression often do not correlate with serum TMAO exposure, suggesting that alternative mechanisms such as metabolic activation may regulate FMO activity21. Nevertheless, current and previous findings collectively indicate that FMO-mediated TMAO formation is increased in CKD, and our present data suggest that it is mechanistically driven by metabolic activation.
Metabolic activation was elicited with octylamine, L-arginine, and uremic and healthy control serum. The up to 4-fold increase in Vmax in the presence of octylamine clearly demonstrates that FMO-mediated TMAO formation can be activated (Fig. 3A)14. The increased metabolic activation with human uremic serum versus healthy control serum suggests that increased concentrations of uremic solutes retained in uremic serum elicit greater metabolic activation (Fig. 4A). Although the potential effector compounds remain unknown, the endogenous solute L-arginine elicits activation (Fig. 3B), and other structurally similar endogenous substances may behave in a similar manner. Interestingly, L-arginine serum concentrations are similar in CKD and healthy patients22, and it is possible that L-arginine is contributing to the metabolic activation observed with healthy control serum (Fig. 4B).
Metabolic activation is an atypical kinetic reaction. Activation of FMO-mediated TMAO formation indicates that ‘effector’ compounds are eliciting structural or electrostatic changes in the FMO catalytic site23. In fact, FMO enzymes can be activated by a broad range of effector compounds that are known uremic retention solutes, including primary amines, guanidine derivatives and small peptides14,24,25. In CKD, these compounds may deposit and accumulate in liver tissue, specifically in the microsomal fraction where they can act as FMO effectors26,27, and this may explain the present findings of metabolic activation and increased TMAO formation in experimental CKD28,29,30,31,32.
In accordance with enzyme kinetic principles, the increased Vmax resulting from metabolic activation of FMOs would result in a corresponding increase in TMAO formation when substrate (trimethylamine) concentrations exceed the relatively low Km value (enzyme affinity for substrate) of approximately 28 µM for FMO3 enzymes33. In this scenario, the reaction is rate limited and not substrate/supply limited, such that any increase in Vmax leads to a corresponding increase in TMAO formation. Trimethylamine concentrations can exceed this Km value in humans considering trimethylamine production is approximately 50 mg/day, especially after a precursor-nutrient rich meal34,35,36. Furthermore, FMO3 gene polymorphisms are associated with increased TMAO concentrations, indicating that FMO-mediated TMAO formation is not supply limited17. Overall, these data support a novel biologically plausible mechanism involving metabolic activation that increases the Vmax of FMO-mediated TMAO formation and contributes to well documented increases in systemic concentrations of TMAO in CKD patients.
Although activation of FMOs leads to increased TMAO formation in this experimental model of CKD, this requires validation in humans. We and several other investigators have reported elevated concentrations of trimethylamine and/or TMAO in CKD patients (Supplementary Table S1)5,7,9,37, but to date the potential mechanisms are unclear. Decreased renal clearance undoubtedly contributes to elevated serum TMAO concentrations38, although the relative contribution is unclear and likely minimal in the setting of advanced kidney disease. Additionally, the observations that systemic TMAO concentrations increase disproportionately in advanced CKD relative to earlier stages of CKD9, and that hemodialysis is relatively ineffective at lowering systemic exposure of TMAO (i.e., evidenced by pre-dialysis concentrations)39, despite high intradialytic clearance37,40, support the premise that TMAO formation is increased in CKD. It has been postulated that TMAO production is not changed in ESKD patients receiving chronic hemodialysis, and that the extraordinarily increased concentrations in these patients are due partly to the inability of hemodialysis to provide clearances of the magnitude achieved by tubular secretion40. While the latter point is valid, TMAO concentrations rise disproportionately even in non-dialyzed Stage 4 CKD patients with residual kidney function and presumably residual secretory clearance. One possible explanation is that the loss of secretory clearance in ESKD is outweighed by a simultaneous increase in TMAO production leading to the increased systemic exposure observed. Lastly, though decreased nonrenal clearance also may impact the systemic exposure of substrates predominantly cleared by the pathway in question41, TMAO undergoes little nonrenal clearance42, so this is unlikely to explain the increases in systemic exposure observed as kidney disease progresses. Overall, high systemic TMAO exposure is likely due to a combination of decreased renal clearance43, and increased TMAO production in kidney disease.
There are several limitations of the current study. Post-translational modifications like phosphorylation may affect enzyme activity and this was not evaluated. The microbiome plays an integral role in the production of trimethylamine, the FMO substrate that is metabolized into TMAO, and we did not explore how it is changed in CKD or whether any changes are associated with altered TMAO formation. It is also possible that the potential effector compounds may be derived from dietary nutrients. The patients that contributed the uremic and healthy serum were not on a controlled diet, which may have influenced the metabolic activation results. In addition, serum from other donors was not evaluated to replicate these findings. There are hundreds of known uremic retention solutes that accumulate in CKD and future work is necessary to determine the potential effector compounds that may activate FMO-mediated TMAO formation44. Future in vitro and in vivo studies will evaluate FMO enzyme activity in the presence of individual solutes (i.e., TMAO, urea, primary amines, guanidine derivatives, etc.). Lastly, therapeutically targeting FMO3 function by partial inhibition may not induce the undesirable symptoms of trimethylaminuria observed in patients with inactive FMO3 enzymes35, but this should be carefully evaluated.
In conclusion, we show for the first time that metabolic activation of hepatic FMOs leads to increased formation of the non-traditional CVD risk factor TMAO. These data provide important mechanistic insight into the function of hepatic FMOs, as metabolic activation may contribute to the elevated TMAO concentrations observed as kidney function declines. FMO-mediated metabolism may be a therapeutic target to decrease TMAO exposure and thereby lower rates of CVD in patients with CKD.
Methods
Chemical reagents
Trimethylamine hydrochloride, TMAO, NADPH, magnesium chloride, tris (hydroxymethyl) aminomethane (Trizma® base), Trizma® hydrochloride, n-octylamine, methimazole, L-arginine and formic acid ( ≥ 95%) were purchased from Sigma-Aldrich (St. Louis, MO). Deuterated internal standard (d9-trimethylamine N-oxide) was purchased from Cambridge Isotopes (Cambridge, MA, USA). Optima LC–MS grade water, acetonitrile, and methanol was purchased from Fisher Scientific (Pittsburgh, PA). Taqman® primers used for mRNA quantification were purchased from Applied Biosystems (Foster City, CA). All fluorescent antibodies were purchased from Abcam (Cambridge, MA) (Codes: ab2769, ab8226, ab22717, ab126790, ab195627, ab186693 and ab175774).
Experimental model
Male Sprague-Dawley rats (Charles River, Saint-Charles, PQ, Canada) that weighed 200 to 300 g were fed standard rat chow and water ad libitum on a 12-hour light/dark cycle. Control rats were pair-fed matching amounts of standard rat chow consumed by CKD rats. The Canadian Council on Animal Care guidelines were observed for care and use of laboratory animals. The experimental protocol was authorized by the Maisonneuve-Rosemont Hospital Research Centre Animal Care Committee. Experimental CKD was surgically induced by first performing a 2/3rd nephrectomy of the left kidney followed 7 days later by a complete right nephrectomy, as previously described45. Control rats underwent to two sham laparotomies. Rats were sacrificed 42 days after the initial surgery and livers were immediately harvested and stored at −80 °C.
Determination of FMO activity
Metabolic activity of hepatic FMOs was assessed with isolated microsomes of control (n = 6) and CKD (n = 6) rat livers. Specifically, trimethylamine was used as a probe substrate of FMO enzymes, and formation rate of TMAO was used as a surrogate measurement of FMO activity. Hepatic microsomes (i.e., the liver fraction containing FMOs) were isolated by differential ultra-centrifugation as previously described46. Incubation times and microsomal protein concentrations were optimized to achieve linear formation of TMAO in the experiments. Microsomal incubations using 0.5 mg/mL of microsomal protein in 0.02 M Tris-HCl buffer (pH 7.4) containing 1 mM nicotinamide adenine dinucleotide phosphate (NADPH), as an essential cofactor, and 5 mM magnesium chloride (MgCl2) were conducted for each rat. The microsomal incubations were pre-warmed in the presence of NADPH for 3 minutes at 37 °C. To start the reaction, 3 μL of increasing concentrations of trimethylamine (2.5, 5, 10, 25, 50, 100, 200, 500, 1000 μM) was added, and microsomes were incubated for 60 min at 37 °C. Final reaction volumes were 300 μL. Each trimethylamine incubation experiment (i.e., each concentration) was conducted in duplicate (CKD vs. healthy control). Negative controls omitting NADPH and trimethylamine were assessed for all incubations. Reactions were stopped by adding 300 μL of ice-cold methanol. TMAO was quantified by ultra-performance liquid chromatography tandem mass spectrometry (LC-MS/MS) as we reported previously47.
mRNA analysis
RNA isolation and real-time quantitative polymerase chain reaction (RT-qPCR) were conducted as recommended by MIQE guidelines48. Total RNA was extracted from homogenized liver tissue from n = 12 CKD and n = 12 control rats, using QiaShredder and RNeasy Mini Kit (Qiagen, Valencia, CA). RNA purity (260/280 ratios ranging from 1.8 to 2.0) and concentrations were determined by measuring the optical density at 260 nm and 280 nm using NanoDrop (ThermoFisher Scientific, Waltham, MA). cDNA was then prepared using SuperScript III reverse transcriptase (Invitrogen, San Diego, CA) with 1 μg of total RNA and random hexamers. Fmo3, Fmo1, Arnt, Ahr, Cyp1a2, Cyp3a2 and Actb (β-Actin) genes were quantified by RT-qPCR with Applied Biosystems 7500 Fast Real-Time PCR System (Foster City, CA) using Taqman® Gene Expression Master Mix (Applied Biosystems, Foster City, CA) and Taqman® specific primers. Template and reverse transcriptase controls were not included in every reaction. Ahr and Arnt were selected because the aryl-hydrocarbon receptor (AhR) signaling pathway may be activated in CKD and partially regulate FMO expression49,50. Hepatic mRNA concentrations were normalized to Actb and expressed relative to the controls using absolute quantification.
Western blot analysis
The protein expression of hepatic FMO3, CYP1A2, CYP3A2, AHR and β-Actin was determined with fluorescent Western blotting. Homogenized liver tissue from n = 12 CKD and n = 12 control rats (30 μg total protein) were separated by 4–15% Mini Protean TGX (Bio-Rad, Hercules, CA) gel electrophoresis and transferred onto PVDF membranes. Transferred membranes were blocked for 1 hour at room temperature using Odyssey Blocking Buffer. Membranes were incubated at 4 °C overnight with specific primary antibodies diluted in 50:50 blocking buffer and TBS- 0.1% Tween (TBST) (1:1000–2500 mouse monoclonal anti- β-Actin, CYP1A2 and AhR; 1:1000 polyclonal rabbit anti- FMO3 and CYP3A2). Membranes were washed four times for 10 minutes with TBST and then for one hour with 50:50 blocking buffer and TBST. Membranes were then incubated for 1 hour in fluorescent secondary antibodies at room temperature (1:20000 donkey anti-rabbit; or 1:10000 donkey anti-mouse). Finally, membranes were washed with TBST, and antibody binding was measured by a LI-COR fluorescent reader (Lincoln, NE) detection system. CYP1A2 and CYP3A2 were selected as controls because their expression in experimental CKD is unchanged and decreased, respectively51. Specificity was assessed by incubating blots that were loaded with control homogenized rat tissue with each primary antibody to check for overlapping fluorescent bands (see Supplementary S-Fig. 1). The linear range of detection was determined for a range of total protein on these blots. Band intensity was quantified by densitometry using ImageJ software and normalized to β-Actin expression.
Assessment of FMO metabolic activation and inhibition
Metabolic activation was explored as a potential mechanism of increased FMO activity. Metabolic activation was assessed using the experimental conditions described above for the determination of FMO activity. However, male Sprague-Dawley rat liver microsomes (purchased from Sekisui XenoTech, Kansas City, KS) were used in these experiments. The reference point of FMO activity in these microsomes was consistent with the experimental control rats. Also, potential activating compounds (0.01–2 mM octylamine or 0.5 and 2 mM L-arginine), and human serum were added to the microsomal incubations prior to the start of the reaction. The FMO inhibitor methimazole (1 mM) was added to 5 replicates of the 50 μM trimethylamine incubates. TMAO formation rates were assessed to measure changes in FMO metabolic activity.
In experiments with human serum, appropriate volumes were added to achieve the 5, 10 and 20% of total reaction volume. Baseline concentrations of trimethylamine and TMAO in the human serum were quantified before starting the incubation reactions (Supplementary Table S1). Final TMAO formation was calculated by taking the final TMAO concentration minus the baseline TMAO concentration. Concentrations of baseline trimethylamine in serum were below the limit of quantification, and therefore were negligible (Supplementary Table S1). Baseline TMAO did not undergo any quantifiable metabolism or retro-reduction into trimethylamine in the microsomal incubations. Healthy human control serum was purchased from a local blood bank and serum from a hemodialysis patient (pre-dialysis sample; serum creatinine, 14.6 mg/dL; BUN, 77 mg/dL) was obtained with informed consent and approval from the University of Kansas Medical Center Institutional Review Board. All serum was ultra-filtered using 10 Kda Satorius Vivaspin® spin columns.
Data and statistical analysis
Individual rat serum TMAO concentrations were adjusted based on kidney function by dividing by the corresponding serum creatinine values. The formation rate of TMAO was determined from LC-MS/MS quantified TMAO concentrations in the microsomal incubates. Non-linear regression Michaelis-Menten kinetic models were used to fit FMO-mediated TMAO formation data, and the maximum velocity (Vmax) and the affinity constant (Km) were estimated and compared by extra-sum-of-squares F-tests with GraphPad Prism (Version 8.0.2; San Diego, CA). Hepatic mRNA levels were normalized to β-Actin and expressed relative to the controls using absolute quantification. Densitometry units of protein expression were normalized to that of β-Actin. Gene and protein expression were not performed in one control rat liver sample due to limited tissue quantity. Student’s t-test or Mann-Whitney test for data exhibiting non-normal distribution were used to compare CKD to control rats. P-values of < 0.05 were considered significant. All results are presented as mean ± SD, unless otherwise stated.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108, 2154–2169 (2003).
Ramezani, A. et al. Role of the Gut Microbiome in Uremia: A Potential Therapeutic Target. Am J Kidney Dis 67, 483–498 (2016).
Meyer, T. W. & Hostetter, T. H. Approaches to uremia. J Am Soc Nephrol 25, 2151–2158 (2014).
Wang, Z. et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63 (2011).
Shafi, T. et al. Trimethylamine N-Oxide and Cardiovascular Events in Hemodialysis Patients. J Am Soc Nephrol 28, 321–331 (2017).
Tang, W. H. et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res 116, 448–455 (2015).
Kim, R. B. et al. Advanced chronic kidney disease populations have elevated trimethylamine N-oxide levels associated with increased cardiovascular events. Kidney Int 89, 1144–1152 (2016).
Tang, W. H. et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 368, 1575–1584 (2013).
Stubbs, J. R. et al. Serum Trimethylamine-N-Oxide is Elevated in CKD and Correlates with Coronary Atherosclerosis Burden. J Am Soc Nephrol 27, 305–313 (2016).
Tang, W. H. et al. Intestinal microbiota-dependent phosphatidylcholine metabolites, diastolic dysfunction, and adverse clinical outcomes in chronic systolic heart failure. J Card Fail 21, 91–96 (2015).
House, A. A. et al. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 95, 1304–1317 (2019).
Zeisberg, E. M. et al. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat Med 13, 952–961 (2007).
Johnson, C., Prokopienko, A. J., West, R. E., III, Nolin, T. D. & Stubbs, J. R. Decreased Kidney Function is Associated with Enhanced Hepatic Flavin Monooxygenase Activity and Increased Circulating Trimethylamine N-oxide Concentrations in Mice. Drug Metab Dispos (2018).
Ziegler, D. M., Poulsen, L. L. & McKee, E. M. Interaction of primary amines with a mixed-function amine oxidase isolated from pig liver microsomes. Xenobiotica 1, 523–531 (1971).
Miao, J. et al. Flavin-containing monooxygenase 3 as a potential player in diabetes-associated atherosclerosis. Nat Commun 6, 6498 (2015).
Shih, D. M. et al. Flavin containing monooxygenase 3 exerts broad effects on glucose and lipid metabolism and atherosclerosis. J Lipid Res 56, 22–37 (2015).
Robinson-Cohen, C. et al. Association of FMO3 Variants and Trimethylamine N-Oxide Concentration, Disease Progression, and Mortality in CKD Patients. PLoS One 11, e0161074 (2016).
Novick, R. M., Mitzey, A. M., Brownfield, M. S. & Elfarra, A. A. Differential localization of flavin-containing monooxygenase (FMO) isoforms 1, 3, and 4 in rat liver and kidney and evidence for expression of FMO4 in mouse, rat, and human liver and kidney microsomes. J Pharmacol Exp Ther 329, 1148–1155 (2009).
Randrianarisoa, E. et al. Relationship of Serum Trimethylamine N-Oxide (TMAO) Levels with early Atherosclerosis in Humans. Sci Rep 6, 26745 (2016).
Ripp, S. L., Itagaki, K., Philpot, R. M. & Elfarra, A. A. Species and sex differences in expression of flavin-containing monooxygenase form 3 in liver and kidney microsomes. Drug Metab Dispos 27, 46–52 (1999).
Bennett, B. J. et al. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab 17, 49–60 (2013).
Kielstein, J. T. et al. Marked increase of asymmetric dimethylarginine in patients with incipient primary chronic renal disease. J Am Soc Nephrol 13, 170–176 (2002).
Hutzler, J. M., Hauer, M. J. & Tracy, T. S. Dapsone activation of CYP2C9-mediated metabolism: evidence for activation of multiple substrates and a two-site model. Drug Metab Dispos 29, 1029–1034 (2001).
Ziegler, D. M., McKee, E. M. & Poulsen, L. L. Microsomal flavoprotein-catalyzed N-oxidation of arylamines. Drug Metab Dispos 1, 314–321 (1973).
Ziegler, D. M. & Mitchell, C. H. Microsomal oxidase. IV. Properties of a mixed-function amine oxidase isolated from pig liver microsomes. Arch Biochem Biophys 150, 116–125 (1972).
Velenosi, T. J. et al. Untargeted plasma and tissue metabolomics in rats with chronic kidney disease given AST-120. Sci Rep 6, 22526 (2016).
Prokopienko, A. J. & Nolin, T. D. Microbiota-derived uremic retention solutes: perpetrators of altered nonrenal drug clearance in kidney disease. Expert Rev Clin Pharmacol 11, 71–82 (2018).
Pfeifer, N. D., Harris, K. B., Yan, G. Z. & Brouwer, K. L. Determination of intracellular unbound concentrations and subcellular localization of drugs in rat sandwich-cultured hepatocytes compared with liver tissue. Drug Metab Dispos 41, 1949–1956 (2013).
Midgley, I. et al. Pharmacokinetics and metabolism of the prodrug DB289 (2,5-bis[4-(N-methoxyamidino)phenyl]furan monomaleate) in rat and monkey and its conversion to the antiprotozoal/antifungal drug DB75 (2,5-bis(4-guanylphenyl)furan dihydrochloride). Drug Metab Dispos 35, 955–967 (2007).
Nishimura, Y. et al. Inhibitory effects of adenine nucleotides and related substances on UDP-glucuronosyltransferase: structure-effect relationships and evidence for an allosteric mechanism. Biochim Biophys Acta 1770, 1557–1566 (2007).
Dorner, A. J. & Kaufman, R. J. The levels of endoplasmic reticulum proteins and ATP affect folding and secretion of selective proteins. Biologicals 22, 103–112 (1994).
Ishii, Y., An, K., Nishimura, Y. & Yamada, H. ATP serves as an endogenous inhibitor of UDP-glucuronosyltransferase (UGT): a new insight into the latency of UGT. Drug Metab Dispos 40, 2081–2089 (2012).
Lang, D. H. et al. Isoform specificity of trimethylamine N-oxygenation by human flavin-containing monooxygenase (FMO) and P450 enzymes: selective catalysis by FMO3. Biochem Pharmacol 56, 1005–1012 (1998).
Jaworska, K. et al. Hypertension in rats is associated with an increased permeability of the colon to TMA, a gut bacteria metabolite. PLoS One 12, e0189310 (2017).
Mitchell, S. C. & Smith, R. L. Trimethylaminuria: the fish malodor syndrome. Drug Metab Dispos 29, 517–521 (2001).
Fennema, D., Phillips, I. R. & Shephard, E. A. Trimethylamine and Trimethylamine N-Oxide, a Flavin-Containing Monooxygenase 3 (FMO3)-Mediated Host-Microbiome Metabolic Axis Implicated in Health and Disease. Drug Metab Dispos 44, 1839–1850 (2016).
Bain, M. A., Faull, R., Fornasini, G., Milne, R. W. & Evans, A. M. Accumulation of trimethylamine and trimethylamine-N-oxide in end-stage renal disease patients undergoing haemodialysis. Nephrol Dial Transplant 21, 1300–1304 (2006).
Manor, O. et al. A Multi-omic Association Study of Trimethylamine N-Oxide. Cell Rep 24, 935–946 (2018).
Sirich, T. L. et al. Limited reduction in uremic solute concentrations with increased dialysis frequency and time in the Frequent Hemodialysis Network Daily Trial. Kidney Int 91, 1186–1192 (2017).
Hai, X. et al. Mechanism of Prominent Trimethylamine Oxide (TMAO) Accumulation in Hemodialysis Patients. PLoS One 10, e0143731 (2015).
Nolin, T. D. et al. ESRD impairs nonrenal clearance of fexofenadine but not midazolam. J Am Soc Nephrol 20, 2269–2276 (2009).
Miyake, T. et al. Involvement of Organic Cation Transporters in the Kinetics of Trimethylamine N-oxide. J Pharm Sci 106, 2542–2550 (2017).
Teft, W. A. et al. Identification and Characterization of Trimethylamine-N-oxide Uptake and Efflux Transporters. Mol Pharm 14, 310–318 (2017).
Duranton, F. et al. Normal and pathologic concentrations of uremic toxins. J Am Soc Nephrol 23, 1258–1270 (2012).
Leblond, F. A., Giroux, L., Villeneuve, J. P. & Pichette, V. Decreased in vivo metabolism of drugs in chronic renal failure. Drug Metab Dispos 28, 1317–1320 (2000).
Alshogran, O. Y. et al. Effect of experimental kidney disease on the functional expression of hepatic reductases. Drug Metab Dispos 43, 100–106 (2015).
Ocque, A. J., Stubbs, J. R. & Nolin, T. D. Development and validation of a simple UHPLC-MS/MS method for the simultaneous determination of trimethylamine N-oxide, choline, and betaine in human plasma and urine. J Pharm Biomed Anal 109, 128–135 (2015).
Bustin, S. A. et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55, 611–622 (2009).
Dou, L. et al. Aryl hydrocarbon receptor is activated in patients and mice with chronic kidney disease. Kidney Int 93, 986–999 (2018).
Celius, T. et al. Aryl hydrocarbon receptor-dependent induction of flavin-containing monooxygenase mRNAs in mouse liver. Drug Metab Dispos 36, 2499–2505 (2008).
Leblond, F. et al. Downregulation of hepatic cytochrome P450 in chronic renal failure. J Am Soc Nephrol 12, 326–332 (2001).
Acknowledgements
We thank Samuel Poloyac, PharmD, PhD, Raman Venkataramanan, PhD, Paul Johnston, PhD, Lee McDermott, PhD, MBA, Jessica Kosanovich, MS, Fanuel Hagos, PhD, Nathalie Henley, MSc, and Amina Shehu, PhD, for their guidance and/or technical assistance. This work was presented in part at Kidney Week 2016, the American Society of Nephrology Annual Meeting, Chicago, IL, November 2016 (Prokopienko AJ, Schrum DP, Fitch A, Morris A, Leblond FA, Pichette V, Nolin TD. Effect of Experimental Kidney Disease on the Formation of TMAO by Flavin-Containing Monooxygenases. J Am Soc Nephrol 2016;27:748 A), and at ASCPT 2019, the American Society for Clinical Pharmacology & Therapeutics Annual Meeting, March 2019 (Prokopienko AJ, West III R, Joshi A, Stubbs JR, Pichette V, Venkataramanan R, Nolin TD. Mechanistic Evaluation of Increased Flavin-Containing Monooxygenase Formation of the Gut-Derived Cardiovascular Disease Risk Factor TMAO in Experimental Kidney Disease. Clin Pharmacol Ther 2019;105:S68-S69). This work was supported in-part by the National Institutes of Health grants TL1TR001858 [AJP], R01-GM107122 [TDN], and R21-DK108093 [JRS, TDN]. Additional support was provided by the American College of Clinical Pharmacy Research Institute Futures Grant Program and the American Foundation for Pharmaceutical Education Fellowship Program [AJP].
Author information
Authors and Affiliations
Contributions
Participated in research design: A.J.P., F.A.L., V.P. and T.D.N.; Conducted experiments: A.J.P., F.A.L., R.E.W. and D.P.S.; Contributed new reagents or analytic tools: J.R.S., F.A.L., V.P. and T.D.N.; Performed data analysis: A.J.P., T.D.N.; Wrote or contributed to the writing of the manuscript: A.J.P., R.E.W., D.P.S., F.A.L., V.P., J.R.S. and T.D.N.; All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prokopienko, A.J., West, R.E., Schrum, D.P. et al. Metabolic Activation of Flavin Monooxygenase-mediated Trimethylamine-N-Oxide Formation in Experimental Kidney Disease. Sci Rep 9, 15901 (2019). https://doi.org/10.1038/s41598-019-52032-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52032-9
This article is cited by
-
The role of gut-dependent molecule trimethylamine N-oxide as a novel target for the treatment of chronic kidney disease
International Urology and Nephrology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.