Abstract
Respiratory syncytial virus (RSV) infection is a leading cause of severe acute lower respiratory tract infection in infants and children worldwide. Vitamin A deficiency (VAD) is one of the most prevalent nutrition-related health problems in the world and is a significant risk factor in the development of severe respiratory infections in infants and young children. Bovine RSV (BRSV) is a primary cause of lower respiratory tract disease in young cattle. The calf model of BRSV infection is useful to understand the immune response to human RSV infection. We have previously developed an amphiphilic polyanhydride nanoparticle (NP)-based vaccine (i.e., nanovaccine) encapsulating the fusion and attachment proteins from BRSV (BRSV-NP). Calves receiving a single, intranasal dose of the BRSV-NP vaccine are partially protected from BRSV challenge. Here, we evaluated the impact of VAD on the immune response to the BRSV-NP vaccine and subsequent challenge with BRSV. Our results show that VAD calves are unable to respond to the mucosal BRSV-NP vaccine, are afforded no protection from BRSV challenge and have significant abnormalities in the inflammatory response in the infected lung. We further show that acute BRSV infection negatively impacts serum and liver retinol, rendering even well-nourished individuals susceptible to VAD. Our results support the use of the calf model for elucidating the impact of nutritional status on mucosal immunity and respiratory viral infection in infants and underline the importance of VA in regulating immunity in the respiratory mucosa.
Similar content being viewed by others
Introduction
Vitamin A deficiency (VAD) is one of the most common nutritional disorders in the world. An estimated 250 million preschool-aged children are VAD, with at least 5 million showing clinical signs1. VAD is associated with increased susceptibility to disease, poor response to vaccination and increased mortality2,3. Although frank VAD is generally considered a disease of the developing world, marginal VAD can be problematic even in developed countries such as the U.S.1,4,5,6. Over 20% of the population in the developed world does not reach the recommended intake, and has plasma and liver concentrations of vitamin A lower than those accepted as normal4,5. Premature infants are born VAD, and despite supplementation, can remain biochemically deficient for months to years after birth7,8. Even at subclinical levels, VAD has been linked to increased incidence and severity of respiratory diseases4,5,9.
Vitamin A refers to a group of fat-soluble retinoids, including retinol, retinal and retinyl esters. Animals are incapable of de novo VA synthesis; therefore, dietary VA is obtained in the diet as preformed VA from animal sources, or as provitamin carotenoids such as beta-carotene from plant sources. VA is stored in the liver, and when needed, is released into the blood stream in the form of retinol. Retinol is converted to its bioactive form, retinoic acid (RA), by a series of enzymes including alcohol dehydrogenases and retinaldehyde dehydrogenases. VA and RA play complex roles in regulating the immune system. VAD causes reduced or altered T and B cell responses to a number of pathogens10,11,12,13,14,15; dysregulated production of type I IFN16; and alterations in numbers and functions of innate immune populations including monocytes, NK cells, and dendritic cell subsets16,17. The roles of VA and RA have been studied in the context of immunity in the gastrointestinal tract. RA plays an important role in regulating the homing of T cells to the gut18, and in promoting the development of FoxP3+ regulatory T cells19. Less is known about the importance of VA and RA in lung immune function. Given the known epidemiologic link between VAD and respiratory disease, there is a need to define the role of VA and RA immunity in the respiratory tract.
Human respiratory syncytial virus (RSV) is a leading cause of severe acute lower respiratory tract disease in infants and young children worldwide20,21 and accounts for up to 70% of hospitalized bronchiolitis cases in industrialized countries22. Globally, there are an estimated 33 million new episodes of HRSV-associated disease in children under 5 years of age with more than 100,000 resultant deaths23. Severe RSV infection has been linked with the development and exacerbation of recurrent wheezing and asthma24, and is a predisposing factor to the development of otitis media25. Despite the high burden, treatment for RSV infection is largely supportive, and there is no vaccine available to prevent or reduce disease.
Bovine respiratory syncytial virus (BRSV) is closely related to human RSV and is a primary cause of severe acute lower respiratory tract disease in young cattle. BRSV infection in calves is strikingly similar to RSV infection in humans, with similarities in age dependence, innate and adaptive immune responses, and disease pathogenesis26,27,28. The calf model is useful to understand the immune response to RSV infection because it is a physiologic host-pathogen interaction, represents a tractable model of the infant immune system, and is a scalable model which can be used to test novel therapeutics and intervention strategies.
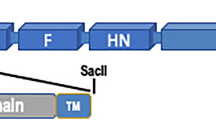
Nanoparticles (NP) composed of biodegradable polyanhydrides have shown impressive versatility and immunogenicity as carriers for vaccine antigens29,30,31,32,33. We have recently published on the development of an amphiphilic polyanhydride copolymer NP based vaccine (i.e. nanovaccine) comprised of a 50:50 molar composition of 1,8-bis(p-carboxyphenoxy)-3,6-dioxaoctane (CPTEG) and 1,6-bis(p-carboxyphenoxy)hexane (CPH), encapsulating the fusion (F) and attachment (G) proteins from BRSV (BRSV-NP)34. The BRSV-NP vaccine exhibited sustained release kinetics of antigen in vitro and maintained the immunogenicity of the antigen payload. Calves receiving a single, intranasal dose of the BRSV-NP vaccine were partially protected from BRSV challenge, with reduced viral loads in the lung, reduced virus shedding and significantly reduced lung pathology compared to their unvaccinated cohorts34. In this study, protection in calves was associated with the induction of virus-specific IgA responses in nasal secretions and bronchoalveolar lavage fluid, and virus-specific cellular immune responses in the lower airways and peripheral blood34.
Given the high burden of RSV disease in both humans and animals, development of a safe and effective vaccine is a critical goal. Importantly, however, a vaccine is only half of the equation and the status of the host immune system has a profound impact on vaccine efficacy, and ultimately, disease susceptibility. Understanding the factors that may negatively affect the efficacy of vaccines in target populations is also vital for an effective immunization program. VAD is endemic in the geographical regions which are hit hardest by RSV1, and is also highly prevalent in premature infants, a population known to be at increased risk from RSV7,8. Epidemiologically, there is significant correlation between VAD and increased susceptibility to and severity of RSV infection35,36; however, the impact of the deficiency on mucosal immune function has not been explored in this context experimentally. To this end, we generated a calf model of VAD, assessed the immune response to mucosal BRSV-NP vaccination and subsequent BRSV challenge, and compared the responses to VA sufficient (VAS) calves. Here, we report that while VAS, BRSV-NP immunized calves are protected from severe RSV-associated disease, VAD calves fail to respond to intranasal BRSV-NP vaccination and develop severe BRSV-associated disease. VAD, BRSV-NP immunized calves do not mount an IgA response in the respiratory tract, nor do they generate virus-specific T cell responses in the lungs or peripheral blood. Gene expression studies demonstrated that VAD calves present with significant abnormalities in the inflammatory milieu in the infected lung, with alterations in Th1 and Th17 immune responses, and impaired mucin production. We further show that acute respiratory viral infection has a significant negative impact on circulating and stored VA levels, causing even vitamin-replete calves to become VA deficient. Thus, our results show that VA status has a significant impact on the mucosal immune system and resistance to respiratory viral infection.
Results
Serum and liver retinol levels
To determine the impact of VAD on the response to mucosal vaccination and subsequent RSV challenge, we first established two groups of calves with differing levels of serum and liver retinol. Calves are born with low VA levels and colostrum is a major source of VA and other fat-soluble micronutrients37. Therefore, all calves received fractionated colostrum replacer with or without VA restored, and were placed on a VAS or VAD milk replacer diet. Serum retinol levels were evaluated weekly, starting after calves were on the differential diets for 1 week. As shown in Fig. 1A, all animals had low serum retinol levels at week 1, but these levels increased in the VAS group, reaching normal serum retinol concentrations by 5–6 weeks of age. The normal range for serum retinol in juvenile calves (30–300 days) is 0.25–0.33 ppm38. Plasma VA levels are tightly regulated by the liver, and therefore not optimal for determining VA status. To confirm VA status in our two treatment groups, liver samples were collected at the time of necropsy. The normal range for liver retinol in juvenile calves is 75–130 ppm38. As seen in Fig. 1B, calves in the VAD treatment group had below normal retinol stores in the liver at the time of necropsy, while VAS calves had normal liver stores.
Retinol concentrations in the serum and liver of VAS and VAD calves. Calves were divided into two groups. VAD animals (n = 18) were fed fractionated colostrum replacer, milk replacer and calf starter devoid of VA. VAS animals (n = 19) were fed matched control diets with added VA. (A) Serum retinol was measured weekly in calves starting at 1 week of age. Data are presented as mean ± SEM. *p < 0.05, **p < 0.01 by two-way ANOVA and Tukey’s posttest. (B) Liver retinol was measured at necropsy, on day 7 after BRSV infection. Data are presented as mean ± SEM. **p < 0.001 by student’s t-test.
VAD calves are not protected by intranasal BRSV-F/G nanoparticle vaccination
We have previously demonstrated that the intranasal BRSV-F/G nanovaccine induces partial protection from BRSV challenge in young, colostrum-replete calves34. To determine the impact of VAD on the response to intranasal vaccination, 13 calves from the VAS treatment group and 12 calves from the VAD treatment group were immunized with the BRSV-NP vaccine. In prior studies, inclusion of soluble antigen with CPTEG:CPH NP-encapsulated protein has been used to induce rapid immunogenicity of the nanovaccines29,39. Therefore, in this study we also sought to determine whether inclusion of soluble F/G protein improves the efficacy of the BRSV-NP vaccine. Calves were immunized intranasally with a single dose of 145 mg BRSV-F/G NP (encapsulating ~1 mg each of the BRSV F and G proteins), co-administered with 1 mg each of soluble F and G proteins in 5 mL of sterile saline. Six VAS calves and six VAD calves served as unvaccinated controls. Four weeks after immunization, calves were challenged via aerosol inoculation with ~104 TCID50 BRSV strain 375. Calves were monitored daily for clinical signs, including body temperature, appetite, nasal discharge and respiratory effort. Starting on days 4–5 after infection, animals developed fevers and clinical signs of lower respiratory tract disease, including coughing, increased respiration rates and increased respiratory effort. As seen in Fig. 2A, on day 7 post infection, clinical disease was significantly reduced in VAS/BRSV-NP vaccinated calves compared to VAS/unvaccinated animals and compared to VAD/BRSV-NP vaccinated calves. There were no significant differences in the clinical signs observed between VAS/unvaccinated controls, VAD/unvaccinated controls and VAD/BRSV-NP vaccinated calves.
VAD calves are not protected by mucosal BRSV-NP vaccination. VAS (n = 13) and VAD (n = 12) calves, aged 5 weeks, were vaccinated with a single, i.n. dose of the BRSV-NP vaccine. Age-matched VAS (n = 6) and VAD (n = 6) control calves remained unvaccinated. Four weeks after vaccination, all calves were challenged via aerosol inoculation with 104 TCID50 BRSV strain 375. (A) Calves in all four groups were monitored daily and assigned a clinical score using the criteria outlined in Materials and Methods. Data represent means ± SEM. ap < 0.05 between VAS/BRSV-NP vaccinated and VAS, unvaccinated calves; bp < 0.01 between VAS/BRSV-NP vaccinated and VAD/BRSV-NP vaccinated. Results were analyzed by 2-way ANOVA with repeated measures, followed by Tukey’s multiple comparisons test. (B,C) Animals were humanely euthanized on day 7 post infection. The extent of gross pneumonic consolidation was evaluated based upon the percent of lung affected (0 = free of lesions; 1 = 1–5% affected; 2 = 5–15% affected; 3 = 15–30% affected; 4 = 30–50% affected; 5 = > 50% affected). Representative images of lungs from one animal in each group are shown in (B). Top panel: VAS calves (with or without BRSV-NP immunization). Bottom panel: VAD calves (with or without BRSV-NP immunization). Aggregate gross pathology results from all groups and all animals are depicted in (C). *p < 0.05 as determined by Kruskal-Wallis test, followed by Dunn’s multiple comparisons test. NS = not significant. Sections of affected and unaffected lung were collected from multiple locations and microscopic lesions were evaluated by a pathologist in a blinded manner using a scoring system we have previously described (see Materials and Methods). Aggregate histopathology scores from all animals are depicted in (D). *p < 0.05 as determined by Kruskal-Wallis test, followed by Dunn’s multiple comparisons test. NS = not significant.
The animals were euthanized on day 7 p.i. and gross lung pathology was evaluated at necropsy. Both VAS and VAD unvaccinated control calves developed lung lesions that were consistent with our previous studies, with bilateral, multifocal to coalescing areas of pneumonic consolidation (Fig. 2B,C). However, as observed in our prior study, VAS/BRSV-NP vaccinated animals were protected from severe disease and exhibited a significant reduction in gross lung pathology (Fig. 2B,C). Surprisingly, however, VAD/BRSV-NP vaccinated calves were not protected by vaccination and developed lung lesions that were similar to the unvaccinated control calves (Fig. 2B,C). Samples of affected and unaffected lung tissue from each animal were evaluated for microscopic lesions using the histopathology scoring system we have previously described34. The lesions were consistent with experimental BRSV infection27,34,40 with bronchointerstitial pneumonia and necrotizing bronchiolitis. As seen in Fig. 2D, VAS/BRSV-NP vaccinated calves showed significantly reduced histological lesions compared to VAS/unvaccinated calves and VAD/BRSV-NP vaccinated calves. No differences were observed between VAD/unvaccinated and VAD/BRSV-NP vaccinated calves.
Our results corroborate our prior study showing that a single dose of the intranasal BRSV-NP vaccine induces partial protection from BRSV infection in juvenile calves. We observed no benefit from the inclusion of the soluble F/G protein in the BRSV-NP vaccine, as the disease sparing in VAS vaccinated calves was similar to that observed in our prior studies of BRSV-NP vaccinated calves34. Our data show that micronutrient status is an important predictor of mucosal vaccine efficacy, as VAD calves that received the BRSV-NP vaccine showed no protection from subsequent BRSV challenge.
BRSV shedding and lung viral burden
Nasal swabs were collected from the animals on days 0, 2, 4 and 7 p.i. to detect viral shedding. As seen in Fig. 3A, BRSV was consistently detected in the unvaccinated VAS and VAD controls on all days after infection, and the majority of the VAD/BRSV-NP vaccinated calves. However, virus was detected in the nasal swabs of less than 50% of the VAS/BRSV-NP vaccinated calves at any timepoint after challenge. Lung tissue samples were analyzed for viral burden using qPCR to detect the viral NS2 gene. VAS/BRSV-NP vaccinated calves had significantly reduced lung viral burdens on day 7 p.i. compared to all other groups (Fig. 3B). Consistent with the virus isolation data, VAD/BRSV-NP vaccinated calves had high titers of BRSV in the lungs and showed no reduction in lung viral burden compared to unvaccinated VAD controls.
Virus shedding and lung burden in VAS and VAD calves receiving the BRSV-NP vaccine. (A) Nasal swab samples were collected on days 0, 2, 4 and 7 after BRSV challenge. Virus isolation was performed on bovine turbinate cells to determine virus shedding. Results are presented as a ratio of BRSV positive samples/total samples. (B) Tissue samples were collected from 2–3 representative lesion and non-lesion sites of the lungs on day 7 post-challenge and preserved in RNALater. The RNA was extracted using Trizol reagent. The RNA from multiple sites was then pooled and was analyzed by qPCR for the BRSV NS2 gene. Viral NS2 copy numbers were calculated using standard curves and normalized to the housekeeping gene, S9, to correct for differences in input material. Results represent the mean NS2 copy number of each calf, with n = 6–13 animals/group. The graph depicts means ± SEM of each group. **p < 0.01 as determined by Kruskal-Wallis test, followed by Dunn’s multiple comparisons test.
VAD calves fail to mount a vaccine-induced mucosal immune response
We have previously shown that the intranasal BRSV-NP vaccine primes for virus-specific IgA production in the upper and lower respiratory tract, and virus-specific cellular immune responses in the airways and peripheral blood34. Given the reduced protection observed in the VAD vaccinated calves, we next examined virus-specific immune responses in the peripheral blood and respiratory tract to BRSV and the F and G proteins. VAS/BRSV-NP vaccinated calves did not mount a significant IgA response to BRSV or the F and G proteins in the nasal fluid prior to BRSV challenge; a result that is consistent with our previous studies. However, on day 7 following BRSV challenge, VAS vaccinated calves had significantly increased concentrations of virus-specific IgA in the nasal fluid (Fig. 4A) and in the BAL (Fig. 4B) compared to unvaccinated VAS calves. This virus-specific IgA response in the respiratory tract included a response to both the F and G proteins (Fig. 4). In contrast to their VAS cohorts, the VAD/BRSV NP vaccinated animals failed to mount a vaccine-induced IgA response in the BAL or nasal fluid (Fig. 4). In ruminants, IgG1 is produced at significant quantities at the mucosal surface; therefore, we also analyzed BRSV-specific IgG (all isotypes) in nasal fluid and BAL fluid on day 7 after infection (Supplementary Fig. 1). Similar to our IgA results, VAS/BRSV NP vaccinated animals had increased levels of virus-specific IgG in the BAL fluid, while reduced quantities of virus-specific IgG were observed in the nasal secretions of unvaccinated animals (both VAS and VAD) and VAD/BRSV NP vaccinated animals. Quantities of virus-specific IgG in the nasal fluid were not significantly different between groups (Supplementary Fig. 1).
VAD calves fail to produce virus-specific IgA in response to intranasal BRSV-NP vaccination. (A) Nasal fluid and (B) BAL samples were collected on day 7 post infection. The samples were diluted 1:2 and analyzed by indirect ELISA for BRSV-, F-protein or G-protein specific IgA. Data represent means ± SEM. *p < 0.05 as determined by Kruskal-Wallis test, followed by Dunn’s multiple comparisons test.
Calves in this study were colostrum replete and possessed preexisting BRSV-specific antibody titers. We observed no differences in the virus-specific serum IgG levels between any of the treatment groups in response to vaccination. Serum neutralization titers (mean and range) are depicted for all groups in Table 1.
Cellular immune responses were evaluated in the lower airways and peripheral blood using in vitro antigen-recall assays. BAL mononuclear cells (Fig. 5A,B) and PBMC (Fig. 5C,D) were isolated on day 7 after BRSV infection and restimulated in vitro as described in Materials & Methods. Cell culture supernatants were then analyzed by sandwich ELISA for IL-17A (left panels) and IFNγ (right panels). BAL cells and PBMC from VAS/BRSV-NP vaccinated calves secreted IL-17A and IFNγ in response to BRSV restimulation and their response was significantly increased over both VAS/unvaccinated controls and over VAD/BRSV-NP vaccinated animals (Fig. 5). BAL and PBMC samples were also collected immediately prior to challenge and evaluated for vaccine-induced cytokine production. However, similar to the IgA results, we did not detect a vaccine-induced cellular response in either the airways or peripheral blood prior to BRSV challenge.
Impaired cellular immune responses in the airways and peripheral blood of VAD/BRSV-NP vaccinated calves. (A,B) Bronchoalveolar lavage samples were collected during the necropsy on day 7 post infection. BAL cells were stimulated for 72 hours with 0.01 MOI BRSV. Control wells remained unstimulated (M, mock). (C,D) Peripheral blood was collected on day 7 after challenge. PBMC were isolated and stimulated for 6 days with 0.01 MOI BRSV. Control wells remained unstimulated (M, mock). Cell culture supernatants were collected from BAL and PBMC cultures and analyzed by commercial ELISA kit for IL-17 (A,C), and IFNγ (B,D). Data represent means ± SEM. *p < 0.05, **p < 0.01 as determined by one-way ANOVA and Tukey’s multiple comparisons test.
Altered inflammatory cytokine expression in the respiratory tract of VAD calves
VA has a significant impact on cells of the innate and adaptive immune system, particularly in the gastrointestinal tract10,16,17; however, less is understood about the impact of VAD on the immune system in the respiratory tract, particularly in the context of acute viral infection. In a mouse model of pneumovirus infection, VAD animals present with a ‘hyper-inflammatory’ phenotype in the lungs, with elevated expression of multiple proinflammatory cytokines41,42. To investigate the impact of VAD on BRSV infection, lung tissues samples were collected from unvaccinated, BRSV infected VAS and VAD calves on day 7 after infection and analyzed by qPCR for expression of proinflammatory cytokines and chemokines. As seen in Fig. 6, the expression of IFNγ, IL-6, IL-13, CXCL9, CXCL10 and TGF-β was significantly higher in the lungs of VAD animals compared to VAS controls. In contrast, the expression of IL-17 and the mucin gene, MUC5B, were both significantly reduced in VAD animals compared to VAS calves. The expression of TNFα, IL-22, IL-8, and IL-10 were not significantly different between VAD and VAS animals. Thus, VAD can enact profound alterations in the immune response during acute respiratory infection.
VAD significantly alters the lung inflammatory environment during BRSV infection. Lung samples were collected from unvaccinated, BRSV infected, VAS and VAD calves (n = 6 per group) on day 7 post infection and analyzed by qPCR for mRNA expression of the indicated gene targets. Results were normalized to the housekeeping gene RPS9 and expressed relative to lung samples from uninfected, VAS (n = 3) and VAD (n = 3) control calves. Data represent means ± SEM. *p < 0.05, **p < 0.01, as determined by student’s t-test.
Acute BRSV infection negatively impacts plasma and liver retinol in vitamin replete animals
Acute illness leads to a sharp decrease in circulating retinol concentrations43, an outcome which has been termed hyporetinemia and is linked to the acute phase response. In rodents challenged with endotoxin, retinol is transiently sequestered in the liver and other tissues, but reappears in the plasma shortly after, with no appreciable irreversible retinol loss44. In human patients, however, acute illness has been linked to increased VA deficiency43. Observationally, respiratory infections in particular have been implicated in depletion of liver VA stores in children45; however, to our knowledge, there have been no studies to date investigating the impact of RSV infection on VA levels in nutritionally-replete infants. Given the potential link between acute infection and VA status, we more closely examined retinol levels in the VAS animals undergoing acute viral infection. Serum samples were collected from VAS/BRSV-NP vaccinated and VAS/unvaccinated calves on days 0, 2, 4 and 6 post infection and were analyzed for serum retinol. As seen in Fig. 7, consistent with reports of hyporetinemia in other species, serum VA levels declined in VAS/unvaccinated calves during acute BRSV infection. In contrast, VA levels were maintained in VAS/BRSV-NP immunized calves, which were undergoing a significantly reduced clinical disease (Fig. 2A). When liver VA levels from VAS calves (Fig. 1B) were further analyzed based on vaccination status, we observed that unvaccinated calves had reduced liver VA levels compared to the vaccinated cohort (Fig. 7B). In fact, the mean liver retinol levels fell below the accepted normal range for animals of this age38, rendering them VA deficient, despite their VA replete diet. We also analyzed liver retinol data from all VAS calves based on BRSV-associated lung pathology scores. As seen in Fig. 7C, liver retinol concentrations were negatively correlated with lung pathology (as an indicator of disease pathology). Thus, acute RSV infection has a significant negative impact on both circulating and stored retinol levels, even in vitamin-replete individuals.
Acute BRSV infection negatively impacts VA status in vitamin-replete animals. (A) Serum retinol in VAS/BRSV-NP vaccinated and VAS unvaccinated calves on days 2, 4 and 6 after BRSV infection. **p < 0.01 by two-way ANOVA and Tukey’s post-test. (B) Liver retinol concentrations in VAS calves on day 7 after BRSV infection (as in Fig. 1B), grouped according to vaccination status (unvaccinated, grey bars; BRSV-NP vaccinated, black bars). **p < 0.01, as determined by student’s t-test. (C) Correlation plot comparing liver retinol concentrations from individual VAS calves (y-axis) with gross lung pathology scores (x-axis, as in Fig. 1B). Data were analyzed for correlation by nonparametric Spearman’s correlation test.
Discussion
Developing efficacious vaccines for RSV is challenging due to the nature of the virus, but also because the target population poses significant obstacles. RSV infection is most severe in premature infants, neonates and young children; and complications from RSV infection are most prevalent in developing countries21,23. VAD is endemic in the geographical regions which are hit hardest by RSV1, and is also a significant problem in premature infants in both developing and developed countries7,8. Also concerning, while VAD is thought to be a disease of the developing world, some studies have suggested that subclinical VAD may be quite prevalent1,4,5,46. It is critical to identify and address comorbidities and host factors which have potential to undermine the effectiveness of a vaccine, such as VAD, in target populations. Here, in the calf model of BRSV infection, we show that VAD has a profound negative impact on the capacity of the host to respond to an intranasal, polyanhydride NP vaccine and to resist the subsequent viral challenge. VAD calves have altered inflammatory cytokine profiles in the lungs, and do not produce virus-specific IgA or cellular immune responses in the lungs or peripheral blood. VA and RA play defined roles in gut immune function and homeostasis; however, our results emphasize that VA also plays an important role in immune function in the respiratory tract.
VAD calves demonstrated a heightened inflammatory cytokine profile in the lungs during BRSV infection, with increased expression of IFNγ, IL-13, IL-6 and the IFNγ-inducible chemokines CXCL9 and CXCL10. This result is consistent with a previous report by Penkert et al. in a mouse model of Sendai virus (SeV) infection41, where levels of IL-6, CXCL10, IFNγ and RANTES were increased in nasal washes from VAD, infected animals. In this model, similar to ours, VAD mice fail to produce virus-specific IgA and have reduced frequencies of CD8 T cells in the lungs following infection42. RA promotes the development of FoxP3+ regulatory T cells, while inhibiting Th17 cell differentiation47. The dysregulated hyper-inflammatory phenotype that has been observed in some models of VAD has been attributed to deficiencies in FoxP3+ Treg cells48. However, Penkert et al. showed that there is no defect in Treg cell differentiation in SeV-infected mice41. Given the reciprocal relationship between Treg and Th17 cells in the presence of RA47, one would predict increased Th17 development and increased IL-17 expression in a VAD system, thus explaining the altered inflammatory profile. However, this is not consistent with our findings in the lungs of VAD calves, as we observed significantly reduced expression of IL-17. Similarly, IL-17 was not detected in the nasal washes of VAD animals during SeV infection41. In a report by Cha et al., VAD mice have significantly reduced expression of IL-17 and reduced numbers of Th17 cells in the lamina propria49. Rudraraju et al. attributed the altered inflammatory profile in the lungs of SeV infected mice to increased viral antigen and viral persistence in the respiratory tract. When animals are sacrificed at the peak of the infection (day 7), the authors observe no difference in the viral titers between VAS and VAD animals42; however, on day 10 after infection, VAS animals had significantly reduced viral loads compared to VAD animals41. The authors speculate that antigen persistence and defects in viral clearance mechanisms contribute to the heightened inflammation in the lungs of the VAD animals, rather than defects in Tregs or Th17 skewing. We detected no differences in virus shedding or viral load between VAD or VAS calves on day 7 after infection. In future studies, it will be important to determine if VAD calves display similar defects in viral clearance in the later stages of the disease, thus explaining the dysregulated cytokine production we observed in the lungs, or if instead, this defect may be attributed to other mechanisms during RSV infection such as an imbalance in the Treg/Th17 axis. Importantly, we observed no significant differences in IL-10 expression in the lungs of VAD calves compared to VAS controls, suggesting that the Treg response may be intact in these animals. However, we did observe increased expression of TGF-β in the lungs of our VAD calves. While TGF-β expression can play a regulatory role, it is also an important cytokine that is elevated during during tissue repair and can contribute to lung fibrosis and mucin expression50. Further investigation into the impact of VAD on the respiratory immune system and response to RSV infection is warranted.
Nutritionists have long recognized that acute infection exacerbates the risk of malnutrition in children43. Measles, chickenpox, respiratory infections and diarrhea have all been implicated in the depletion of liver VA stores and increased risk of xerophthalmia, the principal clinical manifestation of VA deficiency45,51. However, there have been relatively few studies that have specifically addressed the impact of acute respiratory viral infection on retinol status in vitamin replete individuals. As we observed, serum retinol declines over the course of a severe BRSV infection. This result is not surprising, as serum VA is regulated during the acute phase response. In VA-adequate rats, serum retinol declines rapidly following LPS or IL-6 challenge, but returns to normal levels during the resolution phase of the response44,52. There is a minimal loss of retinol through the urine, and studies of radiolabeled retinol have revealed that the majority of retinol is redistributed in the liver and tissues during infection and returns to circulation53. However, contrary to these reports and consistent with the epidemiologic data from humans, our own data suggests that acute infection causes an overall loss in liver stores. In our studies, it is not clear if retinol stores are consumed during the inflammatory response or excreted during the illness. However, the severe impact of acute viral infection on VA stores is cause for concern, as there is potential to fall into a ‘vicious circle’ of acute illness, deficiency and susceptibility to secondary infection.
VA supplementation is an obvious solution to VAD. The WHO currently recommends large-dose, oral Vitamin A supplementation at immunization contact points1. VA supplementation has a significant positive impact on incidence of measles54,55,56. However, its effects on other diseases are less clear. Some studies have reported significant reductions, while others have found little effect or even increased incidence and severity of diarrhea and respiratory infections in children receiving vitamin A supplementation36,57,58,59,60. Studies specifically examining the impact of oral VA supplementation during RSV infection have shown no effect36,57,61 or in one study, have observed increased length of hospital stay for infants receiving VA58. We speculate that oral supplementation at the time of vaccination may not be ideal for addressing VAD and its effects on the respiratory immune response, primarily due to kinetics. A similar principle applies to supplementation during acute infection. Changes in VA homeostasis due to acute inflammation likely limits VA access to inflamed tissues and prevents any modulation to the ongoing immune response. Thus, in the future, we are interested in investigating the utility of a mucosal VA supplementation strategy, which may be a more efficient approach to addressing the immunologic lesions observed in VAD individuals during respiratory vaccination or infection.
In our previous studies we have shown that a single dose of the BRSV-NP vaccine affords partial protection against BRSV infection34. In some early studies in murine models, inclusion of a soluble protein bolus with NP encapsulated antigens has been used to boost the immunogenicity of the NP vaccine29,39. Therefore, in the current study, we hypothesized that administration of soluble F and G protein in suspension with the NP encapsulated proteins, would enhance efficacy. When comparing the vaccine-induced immune responses, viral burden and lung pathology from this study to our prior results34, we observed no increase in immunogenicity or protection mediated by this modified approach. This result is consistent with other recent reports from our groups, wherein a free protein component was not required for polyanhydride nanovaccine efficacy in a mouse model of influenza A virus32 or Streptococcus pneumoniae62 infection. In future studies, a heterologous prime-boost approach or use of additional RSV target proteins may prove more efficacious in the neonate.
In summary, we have confirmed our prior studies, showing that a single, intranasal dose of a BRSV-NP vaccine primes for protective immunity in neonatal calves, resulting in significant reductions in virus-associated clinical disease, lung pathology and viral lung burden following BRSV challenge. VAD enacts major changes in the lung inflammatory response during BRSV infection and has a severe negative effect on the immunogenicity of the mucosal BRSV-NP vaccine. We further show that acute RSV infection has the potential to induce or exacerbate VAD, even in well-nourished individuals, indicating that particular care should be taken in managing the nutrition of convalescent infants and children to avoid long-term micronutrient deficiencies and thus, susceptibility to secondary infections or complicating sequalae.
Materials and Methods
Recombinant F and G proteins
The recombinant fusion (F) protein was produced by Genscript (Piscataway, NJ) using a recombinant baculovirus expression system as we have previously described34. The recombinant attachment (G) protein was expressed in E. coli as we have previously described34.
BRSV-F/G Nanovaccine
The BRSV-F/G nanovaccine was prepared as previously described34, with minor modifications. Briefly, 50:50 CPTEG:CPH copolymer was dissolved in methylene chloride at a concentration of 20 mg/mL. The F and G proteins were suspended in this solution at a total protein concentration of 7.4 mg/mL (3.7 mg/mL of each protein), sonicated for approximately 30 seconds, and the suspension poured into pentane at a 1:200 volumetric ratio (methylene chloride:pentane). The suspension was vacuum filtered to collect the nanoparticles and the nanoparticles were placed in a −20 °C freezer until further use. The nanoparticle yield was 73% with a protein encapsulation efficiency of ca. 100% ([actual protein mass encapsulated]/[theoretical protein mass encapsulated]).
Animals
All animal procedures were conducted in strict accordance with federal and institutional guidelines and were approved by the Kansas State University Institutional Animal Care and Use Committee. The animal care protocol included provisions for a humane endpoint as determined by the discretion of the attending clinical veterinarian. Methods to minimize pain and distress included the avoidance of prolonged restraint and the inclusion of euthanasia as an intervention strategy.
A total of forty-three, mixed-gender (n = 21 males; n = 22 females) Holstein calves were purchased from two dairy farms, one in southern Nebraska (n = 37) and one in central KS (n = 6), and were enrolled in the study at birth. Calves were randomly assigned to the VAD or VAS treatment group. All calves were prevented suckling from their dams, and instead received a first feeding of colostrum replacer within 4 h of birth. Each animal received 375 g of fractionated colostrum replacer (Milk Products, Chilton, WI) reconstituted in 1.9 L of water at approximately 40 °C. The colostrum replacer contained 150 g of bovine globulin protein concentrated from colostral whey and was essentially devoid of all fat-soluble vitamins A, D3, and E. Vitamins D3 (150,000 IU of cholecalciferol/dose) and E (1,500 IU alpha-tocopheral/dose) were added back to the colostrum replacer for all calves. VA (150,000 IU retinyl palmitate) was added back to the VAS treatment group. VA was omitted from the colostrum replacer for the VAD calves. Animals were then placed on a VAS or VAD milk replacer diet for the remainder of the study (Milk Products, Chilton, WI). Calves were transported to the Large Animal Research Center at Kansas State University at 3–4 days of age and housed in groups of 2–3 calves per pen on pine chip bedding. Calves were bottle-fed three times per day (~8 hours apart) until 3 weeks of age, then twice per day (~12 hours apart). The milk replacer consisted of 21% crude protein and 20% fat, and was fed at a rate of 1.5 lbs/day and 14% solids. VAS calves received 45,000 IU VA (retinyl palmitate) per day. VAD animals received the same milk replacer formulation without VA. Calves were also provided ab libitum access to calf starter pellets (18% crude protein, 8% ADF) starting at ~2 weeks of age. Starter grain was formulated without added VA (VAD calves) or with 1820 IU/lb (VAS calves).
Serum retinol levels were monitored weekly. Samples were submitted to the Iowa State University Veterinary Diagnostic Laboratory for evaluation. At 6 weeks of age, animals were divided into 4 groups: 1) VAS, no vaccine (n = 6; 3 females and 3 males); 2) VAS, BRSV-NP vaccine (n = 13; 7 males and 6 females); 3) VAD, no vaccine (n = 6, 2 males and 4 females); 4) VAD, BRSV-NP vaccine (n = 12; 5 males and 7 females). Calves were vaccinated intranasally with 145 mg BRSV-F/G loaded CPTEG:CPH nanoparticles (~2 mg recombinant F and G proteins) with 2 mg soluble recombinant F and G proteins. The vaccine was suspended in 5 mL of sterile saline, with 2.5 mL delivered into each nostril. The calf was restrained and its head was tilted up, then the vaccine was administered into the nose using a syringe fitted with a 2-inch nasal cannula, equipped with a plastic depth control ring. Following vaccination, immune responses were monitored weekly in the serum, peripheral blood, and upper (nasal fluid collection) and lower (bronchoalveolar lavage fluid collection) respiratory tract. Six calves (VAS, n = 3, all calves were male; VAD, n = 3, 2 females and 1 male) were sacrificed prior to challenge and samples of lung and liver tissues were collected to verify retinol concentrations and to serve as control tissues for immunology and gene expression studies.
Bronchoalveolar lavage fluid collection
Pre-challenge bronchoalveolar lavage (BAL) fluid was collected from all animals, 4–5 days prior to BRSV infection, using a protocol we have previously described63. A modified stallion catheter was blindly passed through the nose and advanced through the trachea until lodging in the bronchus. A total of 180 mL of sterile saline was divided into three aliquots. An aliquot was introduced to the lower respiratory tract, followed by immediate suction to obtain lower airway washes. The procedure was repeated twice more. All three aliquots were pooled at the end of the procedure. BAL samples were kept on ice, filtered over sterile gauze, and centrifuged at 200 x g for 10 minutes. Contaminating red blood cells were removed using hypotonic lysis. Cells were washed, counted and stimulated as described below for antigen recall assays.
BRSV inoculum and aerosol challenge model
BRSV strain 375 was prepared from virus stock re-isolated from the lung of an infected animal and passaged less than 4 times on bovine turbinate (BT) cells. The viral inoculum was determined free of BVDV contamination by PCR. Calves were inoculated via aerosol challenge with ~104 TCID50/mL of BRSV strain 375 as previously described28.
Clinical Illness scoring
Calves were monitored twice daily for clinical illness by a trained, blinded observer. Calves were scored using an adaptation of the University of Wisconsin Calf Health Respiratory Scoring Chart, originally established by Dr. Sheila McGuirk (https://www.vetmed.wisc.edu/dms/fapm/fapmtools/8calf/calf_respiratory_scoring_chart.pdf). The scoring chart assigns numbers (0–3) based upon fever and severity of clinical signs including cough, nasal discharge, ocular discharge and ear position. For our scoring chart we include one additional category for respiratory effort (0 = no effort to 3 = significant effort).
Virus isolation
Nasal swabs were collected from each calf on days 0, 3 and 7 post infection and placed in virus isolation media (serum free MEM with antibiotics). Virus isolations were performed as previously described28.
Necropsy and pathological evaluation
Calves were euthanized on day 7 post-infection (p.i.) by barbiturate overdose. Pathological evaluation was performed similar to previous descriptions28,64. The extent of pneumonic consolidation was evaluated using the scoring system we have published34.
Post-infection BAL fluid was collected at necropsy by removing the lungs and trachea and introducing 500 mL of sterile, ice-cold saline through the trachea. The lungs were massaged, and then fluid was poured back out of the trachea into sterile collection bottles. Samples of affected and unaffected lungs were collected from multiple sites for histopathological evaluation. Tissues were fixed by immersion in 10% neutral buffered formalin and processed by routine paraffin-embedment and sectioning. 5 μM sections were stained for hematoxylin and eosin. Microscopic lesions were evaluated by a pathologist (Dr. Henningson) in a blinded manner. The severity of the lung lesions were scored based upon the criteria we have previously published34.
Antigen recall assays
Peripheral blood mononuclear cells (PBMC) were prepared as previously described34. 5 × 106 cells/mL were plated in round-bottom 96-well plates. Bronchoalveolar lavage fluid (BAL) samples were filtered through 2-layer sterile gauze and centrifuged a 500xg for 10 minutes. 106 cells/well were resuspended in cRPMI and plated in 24 well plates. PBMC and BAL cells were stimulated with 5 μg/mL recombinant BRSV F or G protein or 0.01 MOI of BRSV. Plates were incubated for 6 days (PBMC) or 72 hours (BAL cells) at 37 °C in a 5% CO2 incubator. Cell culture supernatants were stored at −80 °C until ELISA analysis.
Real-time PCR
RNA isolation, cDNA preparation and qPCR were performed as described34 using primer sequences which have been published28. Relative gene expression was determined using the 2−ΔΔCt method65, with RPS9 as the reference housekeeping gene. Samples were normalized to uninfected control lung tissue collected from either VAS or VAD calves, as appropriate. NS2 qPCR was performed using the Taqman RNA-to-CT 1-step kit (Applied Biosystems) as in34. Viral NS2 copy numbers were calculated using standard curves. For lung tissue, NS2 copy numbers were normalized to the S9 housekeeping gene to correct for differences in input material. qPCR was run on an Agilent MX3000P Real-Time PCR machine or a ThermoFisher Scientific QuantStudio 3 Real-Time PCR machine.
ELISAs
Bovine IL-17A and IFNγ VetSet ELISA Development kits were purchased from Kingfisher Biotech, Inc and performed according to manufacturer’s instructions.
Indirect ELISAs were used to quantify IgA and IgG in the nasal and BAL fluid. ELISA plates were coated overnight at 4 °C with 3 μg/mL F or G protein (IgA only), or with 100 μL/well of BRSV stock (~104 TCID50). Negative control wells were coated with 100 μL/well cell culture media prepared from uninfected BT cells. Nasal fluid samples were diluted 1:2 and treated with 10 mM dithiothreitol (DTT) for one hour at 37 °C prior to performing the ELISAs. BAL fluid samples were diluted 1:2 with wash buffer. All samples were plated in duplicates, incubated for 2 h at room temperature and then washed. Mouse anti-bovine IgA-HRP (Bethyl Laboratories) or mouse anti-bovine IgG-HRP was used at 0.5 μg/mL. Plates were developed using Pierce 1-Step Ultra TMP Substrate (ThermoScientific Pierce). The reaction was stopped with the addition of 0.2 M H2SO4 and plates were read at an optical density of 450 nm and 540 nm using an automated plate reader.
Serum neutralization assays
Baseline (prior to vaccination) and pre-challenge (day 0) serum samples were collected and submitted to the Kansas State University Veterinary Diagnostic Laboratory for evaluation of BRSV-specific virus neutralization titers.
Statistics
Statistical analysis was performed using Prism v6.0 f software (Graphpad Software, Inc.). The data were analyzed using a Kruskal-Wallis test followed by Dunn’s Multiple Comparison’s test or by Student’s t-test. Correlation analysis in Fig. 7 was performed using Spearman’s nonparametric correlation test.
References
World Health Organization. Global prevalence of vitamin A deficiency in populations at risk 1995-2005: WHO global database on vitamin A deficiency. (World Health Organization, 2009).
Rahman, M. M. et al. Simultaneous vitamin A administration at routine immunization contact enhances antibody response to diphtheria vaccine in infants younger than six months. J Nutr 129, 2192–2195 (1999).
Bhaskaram, P. & Rao, K. V. Enhancement in seroconversion to measles vaccine with simultaneous administration of vitamin A in 9-months-old Indian infants. Indian J Pediatr 64, 503–509 (1997).
Timoneda, J. et al. Vitamin A Deficiency and the Lung. Nutrients 10, https://doi.org/10.3390/nu10091132 (2018).
Stephens, D., Jackson, P. L. & Gutierrez, Y. Subclinical vitamin A deficiency: a potentially unrecognized problem in the United States. Pediatr Nurs 22(377–389), 456 (1996).
Gregory, J. & Lowe, S. National diet and nutrition survey: Young people aged 4-18 years. Vol. 1:Report of the Diet and Nutrition Survey. London: The Stationery Office (2000).
Brandt, R. B. et al. Serum vitamin A in premature and term neonates. J Pediatr 92, 101–104 (1978).
Shenai, J. P., Chytil, F. & Stahlman, M. T. Liver vitamin A reserves of very low birth weight neonates. Pediatr Res 19, 892–893 (1985).
Sommer, A., Katz, J. & Tarwotjo, I. Increased risk of respiratory disease and diarrhea in children with preexisting mild vitamin A deficiency. Am J Clin Nutr 40, 1090–1095 (1984).
Chattha, K. S., Kandasamy, S., Vlasova, A. N. & Saif, L. J. Vitamin A deficiency impairs adaptive B and T cell responses to a prototype monovalent attenuated human rotavirus vaccine and virulent human rotavirus challenge in a gnotobiotic piglet model. PLoS One 8, e82966, https://doi.org/10.1371/journal.pone.0082966 (2013).
Jee, J. et al. Effects of dietary vitamin A content on antibody responses of feedlot calves inoculated intramuscularly with an inactivated bovine coronavirus vaccine. Am J Vet Res 74, 1353–1362, https://doi.org/10.2460/ajvr.74.10.1353 (2013).
Lavasa, S., Kumar, L., Chakravarti, R. N. & Kumar, M. Early humoral immune response in vitamin A deficiency–an experimental study. Indian J Exp Biol 26, 431–435 (1988).
Rombout, J. H. et al. Effect of vitamin A deficiency and Newcastle disease virus infection on IgA and IgM secretion in chickens. Br J Nutr 68, 753–763 (1992).
Sijtsma, S. R., Rombout, J. H., West, C. E. & van der Zijpp, A. J. Vitamin A deficiency impairs cytotoxic T lymphocyte activity in Newcastle disease virus-infected chickens. Vet Immunol Immunopathol 26, 191–201 (1990).
Stephensen, C. B., Blount, S. R., Schoeb, T. R. & Park, J. Y. Vitamin A deficiency impairs some aspects of the host response to influenza A virus infection in BALB/c mice. J Nutr 123, 823–833 (1993).
Vlasova, A. N., Chattha, K. S., Kandasamy, S., Siegismund, C. S. & Saif, L. J. Prenatally acquired vitamin A deficiency alters innate immune responses to human rotavirus in a gnotobiotic pig model. J Immunol 190, 4742–4753, https://doi.org/10.4049/jimmunol.1203575 (2013).
Klebanoff, C. A. et al. Retinoic acid controls the homeostasis of pre-cDC-derived splenic and intestinal dendritic cells. J Exp Med 210, 1961–1976, https://doi.org/10.1084/jem.20122508 (2013).
Iwata, M. et al. Retinoic acid imprints gut-homing specificity on T cells. Immunity 21, 527–538, https://doi.org/10.1016/j.immuni.2004.08.011 (2004).
Bakdash, G., Vogelpoel, L. T., van Capel, T. M., Kapsenberg, M. L. & de Jong, E. C. Retinoic acid primes human dendritic cells to induce gut-homing, IL-10-producing regulatory T cells. Mucosal Immunol 8, 265–278, https://doi.org/10.1038/mi.2014.64 (2015).
Collins, P. L. & Melero, J. A. Progress in understanding and controlling respiratory syncytial virus: still crazy after all these years. Virus Res 162, 80–99, https://doi.org/10.1016/j.virusres.2011.09.020 (2011).
Welliver, R. C. Sr. et al. Fatality rates in published reports of RSV hospitalizations among high-risk and otherwise healthy children. Curr Med Res Opin 26, 2175–2181, https://doi.org/10.1185/03007995.2010.505126 (2010).
Hall, C. B. Respiratory syncytial virus and parainfluenza virus. N Engl J Med 344, 1917–1928, https://doi.org/10.1056/NEJM200106213442507 (2001).
Nair, H. et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet 375, 1545–1555, https://doi.org/10.1016/S0140-6736(10)60206-1 (2010).
Silvestri, M., Sabatini, F., Defilippi, A. C. & Rossi, G. A. The wheezy infant–immunological and molecular considerations. Paediatr Respir Rev 5(Suppl A), S81–87 (2004).
Hall, C. B., Walsh, E. E., Long, C. E. & Schnabel, K. C. Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis 163, 693–698 (1991).
Bem, R. A., Domachowske, J. B. & Rosenberg, H. F. Animal models of human respiratory syncytial virus disease. Am J Physiol Lung Cell Mol Physiol 301, L148–156, https://doi.org/10.1152/ajplung.00065.2011 (2011).
Sacco, R. E., McGill, J. L., Pillatzki, A. E., Palmer, M. V. & Ackermann, M. R. Respiratory syncytial virus infection in cattle. Vet Pathol 51, 427–436, https://doi.org/10.1177/0300985813501341 (2014).
Sacco, R. E. et al. Differential expression of cytokines in response to respiratory syncytial virus infection of calves with high or low circulating 25-hydroxyvitamin D3. PloS one 7, e33074, https://doi.org/10.1371/journal.pone.0033074 (2012).
Haughney, S. L. et al. Retention of structure, antigenicity, and biological function of pneumococcal surface protein A (PspA) released from polyanhydride nanoparticles. Acta Biomater 9, 8262–8271, https://doi.org/10.1016/j.actbio.2013.06.006 (2013).
Ross, K. A. et al. Structural and antigenic stability of H5N1 hemagglutinin trimer upon release from polyanhydride nanoparticles. J Biomed Mater Res A 102, 4161–4168, https://doi.org/10.1002/jbm.a.35086 (2014).
Ulery, B. D. et al. Design of a protective single-dose intranasal nanoparticle-based vaccine platform for respiratory infectious diseases. PLoS One 6, e17642, https://doi.org/10.1371/journal.pone.0017642 (2011).
Zacharias, Z. R. et al. Polyanhydride Nanovaccine Induces Robust Pulmonary B and T Cell Immunity and Confers Protection Against Homologous and Heterologous Influenza A Virus Infections. Frontiers in Immunology 9, https://doi.org/10.3389/fimmu.2018.01953 (2018).
Dhakal, S. et al. Biodegradable nanoparticle delivery of inactivated swine influenza virus vaccine provides heterologous cell-mediated immune response in pigs. J Control Release 247, 194–205, https://doi.org/10.1016/j.jconrel.2016.12.039 (2017).
McGill, J. L. et al. Efficacy of mucosal polyanhydride nanovaccine against respiratory syncytial virus infection in the neonatal calf. Sci Rep 8, 3021, https://doi.org/10.1038/s41598-018-21292-2 (2018).
Neuzil, K. M. et al. Serum vitamin A levels in respiratory syncytial virus infection. J Pediatr 124, 433–436 (1994).
Quinlan, K. P. & Hayani, K. C. Vitamin A and respiratory syncytial virus infection. Serum levels and supplementation trial. Arch Pediatr Adolesc Med 150, 25–30 (1996).
Drackley, J. K. Calf nutrition from birth to breeding. Vet Clin North Am Food Anim Pract 24, 55–86, https://doi.org/10.1016/j.cvfa.2008.01.001 (2008).
Puls, R. Vitamin levels in animal health: diagnostic data and bibliographies. (Sherpa International, 1994).
Ross, K. A. et al. Hemagglutinin-based polyanhydride nanovaccines against H5N1 influenza elicit protective virus neutralizing titers and cell-mediated immunity. Int J Nanomedicine 10, 229–243, https://doi.org/10.2147/IJN.S72264 (2015).
Guerra-Maupome, M., Palmer, V. M., McGill, L. J. & Sacco, E. R. Utility of the Neonatal Calf Model for Testing Vaccines and Intervention Strategies for Use against Human RSV Infection. Vaccines 7, https://doi.org/10.3390/vaccines7010007 (2019).
Penkert, R. R. et al. Vitamin A deficient mice exhibit increased viral antigens and enhanced cytokine/chemokine production in nasal tissues following respiratory virus infection despite the presence of FoxP3+ T cells. Int Immunol 28, 139–152, https://doi.org/10.1093/intimm/dxv064 (2016).
Rudraraju, R. et al. Reduced frequencies and heightened CD103 expression among virus-induced CD8(+) T cells in the respiratory tract airways of vitamin A-deficient mice. Clin Vaccine Immunol 19, 757–765, https://doi.org/10.1128/CVI.05576-11 (2012).
Rubin, L. P., Ross, A. C., Stephensen, C. B., Bohn, T. & Tanumihardjo, S. A. Metabolic Effects of Inflammation on Vitamin A and Carotenoids in Humans and Animal Models. Adv Nutr 8, 197–212, https://doi.org/10.3945/an.116.014167 (2017).
Gieng, S. H., Raila, J. & Rosales, F. J. Accumulation of retinol in the liver after prolonged hyporetinolemia in the vitamin A-sufficient rat. J Lipid Res 46, 641–649, https://doi.org/10.1194/jlr.M400415-JLR200 (2005).
Rahman, M. M. et al. Acute respiratory infections prevent improvement of vitamin A status in young infants supplemented with vitamin A. J Nutr 126, 628–633, https://doi.org/10.1093/jn/126.3.628 (1996).
JR, G. et al. (HMSO, London, 2000).
Omenetti, S. & Pizarro, T. T. The Treg/Th17 Axis: A Dynamic Balance Regulated by the Gut Microbiome. Front Immunol 6, 639, https://doi.org/10.3389/fimmu.2015.00639 (2015).
Bai, A. et al. All-trans retinoic acid down-regulates inflammatory responses by shifting the Treg/Th17 profile in human ulcerative and murine colitis. J Leukoc Biol 86, 959–969, https://doi.org/10.1189/jlb.0109006 (2009).
Cha, H. R. et al. Downregulation of Th17 cells in the small intestine by disruption of gut flora in the absence of retinoic acid. J Immunol 184, 6799–6806, https://doi.org/10.4049/jimmunol.0902944 (2010).
Crane, M. J., Lee, K. M., FitzGerald, E. S. & Jamieson, A. M. Surviving Deadly Lung Infections: Innate Host Tolerance Mechanisms in the Pulmonary System. Front Immunol 9, 1421, https://doi.org/10.3389/fimmu.2018.01421 (2018).
Sommer, A., Tarwotjo, I. & Katz, J. Increased risk of xerophthalmia following diarrhea and respiratory disease. Am J Clin Nutr 45, 977–980, https://doi.org/10.1093/ajcn/45.5.977 (1987).
Rosales, F. J. & Ross, A. C. Acute inflammation induces hyporetinemia and modifies the plasma and tissue response to vitamin A supplementation in marginally vitamin A-deficient rats. J Nutr 128, 960–966, https://doi.org/10.1093/jn/128.6.960 (1998).
Gieng, S., Green, M., Green, J. & Rosales, F. Model-based compartmental analysis indicates a reduced mobilization of hepatic vitamin A during inflammation in rats. Journal of Lipid Research 48, 904–913, https://doi.org/10.1194/jlr.M600528-JLR200 (2007).
Barclay, A. J., Foster, A. & Sommer, A. Vitamin A supplements and mortality related to measles: a randomised clinical trial. Br Med J (Clin Res Ed) 294, (294–296 (1987).
Benn, C. S. et al. Vitamin A supplementation and BCG vaccination at birth in low birthweight neonates: two by two factorial randomised controlled trial. BMJ 340, c1101, https://doi.org/10.1136/bmj.c1101 (2010).
Diness, B. R. et al. The effect of high-dose vitamin A supplementation given with bacille Calmette-Guerin vaccine at birth on infant rotavirus infection and diarrhea: a randomized prospective study from Guinea-Bissau. J Infect Dis 202(Suppl), S243–251, https://doi.org/10.1086/653569 (2010).
Dowell, S. F. et al. Treatment of respiratory syncytial virus infection with vitamin A: a randomized, placebo-controlled trial in Santiago, Chile. Pediatr Infect Dis J 15, 782–786 (1996).
Bresee, J. S. et al. Vitamin A therapy for children with respiratory syncytial virus infection: a multicenter trial in the United States. Pediatr Infect Dis J 15, 777–782 (1996).
Long, K. Z., Montoya, Y., Hertzmark, E., Santos, J. I. & Rosado, J. L. A double-blind, randomized, clinical trial of the effect of vitamin A and zinc supplementation on diarrheal disease and respiratory tract infections in children in Mexico City, Mexico. Am J Clin Nutr 83, 693–700 (2006).
Dibley, M. J., Sadjimin, T., Kjolhede, C. L. & Moulton, L. H. Vitamin A supplementation fails to reduce incidence of acute respiratory illness and diarrhea in preschool-age Indonesian children. J Nutr 126, 434–442 (1996).
Neuzil, K. M., Gruber, W. C., Chytil, F., Stahlman, M. T. & Graham, B. S. Safety and pharmacokinetics of vitamin A therapy for infants with respiratory syncytial virus infections. Antimicrob Agents Chemother 39, 1191–1193 (1995).
Wagner-Muñiz, D. A., Haughney, S. L., Kelly, S. M., Wannemuehler, M. J. & Narasimhan, B. Room Temperature Stable PspA-Based Nanovaccine Induces Protective Immunity. Front Immunol 9, 325, https://doi.org/10.3389/fimmu.2018.00325 (2018).
Guerra-Maupome, M., Vang, D. X. & McGill, J. L. Aerosol vaccination with Bacille Calmette-Guerin induces a trained innate immune phenotype in calves. PLOS ONE 14, e0212751, https://doi.org/10.1371/journal.pone.0212751 (2019).
Viuff, B. et al. Replication and clearance of respiratory syncytial virus: apoptosis is an important pathway of virus clearance after experimental infection with bovine respiratory syncytial virus. Am J Pathol 161, 2195–2207, https://doi.org/10.1016/s0002-9440(10)64496-3 (2002).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25, 402–408, https://doi.org/10.1006/meth.2001.1262 (2001).
Acknowledgements
The authors wish to thank Dr. Timothy Reinhardt at the National Animal Disease Center, USDA, for his helpful discussions on Vitamin A and immunity in the calf. The authors wish to thank David Wood, Ronelle Blome and Animix, LLC for their assistance with formulating the custom colostrum and milk replacers. The authors wish to thank Rachel Rusk for her excellent technical assistance. The authors also wish to thank Dr. Brooke Bloomberg, Jenny Downard, Julie Higgins and the Kansas State University Comparative Medicine Group for their tentative care of the animals. This project was supported by the National Institutes of Health NIAID grant number R21 AI121729 and NIGMS COBRE grant number P20 GM103638 to JLM.
Author information
Authors and Affiliations
Contributions
J.M., R.S. and B.N. designed the study. J.M., S.K., M.G.M., E.W. and J.H. performed the experiments and analyzed the data. J.M., S.K., R.S. and B.N. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McGill, J.L., Kelly, S.M., Guerra-Maupome, M. et al. Vitamin A deficiency impairs the immune response to intranasal vaccination and RSV infection in neonatal calves. Sci Rep 9, 15157 (2019). https://doi.org/10.1038/s41598-019-51684-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51684-x
This article is cited by
-
Evaluation of vitamin A and E deficiency with severity of SARS-COV-2 disease: a case–control study
The Egyptian Journal of Bronchology (2023)
-
The role of retinoic acid in the production of immunoglobulin A
Mucosal Immunology (2022)
-
Review on bovine respiratory syncytial virus and bovine parainfluenza – usual suspects in bovine respiratory disease – a narrative review
BMC Veterinary Research (2021)
-
The correlation between vitamin a status and refractory Mycoplasma Pneumoniae pneumonia (RMPP) incidence in children
BMC Pediatrics (2020)
-
Innovative use of animal models to advance scientific research
Cell and Tissue Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.