Abstract
To evaluate the repeatability of corneal biomechanical parameters in normal and keratoconus eyes, and explore factors that affects the repeatability, and further assess the diagnostic ability of new parameters. Seventy-seven keratoconus eyes of 47 patients and 77 right eyes of 77 normal subjects were recruited in current study. All participants received three repeated measurements with 2 to 5 minutes interval. The interclass correlation coefficient (ICC), Cronbach’ α and repeatability coefficient (RC) were evaluated. The liner regression analysis was used to identify factors that affect the repeatability, and linear mixed effects model was performed to compare the parameters differences. The receiver operating characteristic (ROC) curve was used to evaluate the diagnostic ability of new parameters. Eighteen parameters in normal eyes and twenty-two parameters in keratoconus eyes showed excellent repeatability (ICC ≥ 0.90). Age, axial measurement (AL), spherical equivalent, astigmatism, gender, mean keratometry (Kmean), intraocular pressure (IOP) and central corneal thickness (CCT) could affect the repeatability of new Corvis ST parameters. Compared with normal eyes, the Ambrósio’s Relational Thickness horizontal (ARTh), biomechanical corrected IOP (bIOP), stiffness parameter at first applanation (SP A1) were low and the Max Inverse Radius, deformation amplitude (DA) Ratio Max [2 mm], Pachy Slope, DA Ratio Max [1 mm], Integrated Radius and Corvis Biomechanical Index (CBI) were high in keratoconus eyes (All P < 0.05). Both ARTh and CBI had high Youden index (0.870), and the corresponding cut-off values were 379.29 and 0.44. The repeatability of Corvis ST parameters was acceptable both in normal and keratoconus eyes, and new parameters could effectively diagnose keratoconus eyes from normal eyes.
Similar content being viewed by others
Introduction
Corneal biomechanics, which reflects the corneal deformation in response to external forces, is a determinant of corneal shape1. Recent studies have demonstrated that corneal biomechanics played an important role in assessing glaucoma2 and detecting patients with corneal ectasia diseases especially for keratoconus3. Keratoconus is a progressive corneal disorder that could modify the normal architecture into a conical shape and lead to corneal apex thinning4. As a non-inflammatory disease, Keratoconus usually happens in adolescence and progresses until the third or fourth decade of life, and results in serious vision loss in advanced stages5. Recent study reported the corneal tomographic or topographic maps could help to diagnose keratoconus in the alteration of corneal shape6. However, the diagnoses for early and subclinical keratoconus presenting few or no symptom are still difficult7. Previous study found that the abnormal biomechanics occurred before the keratoconus patients had tomographic changes and clinical symptoms, and the corneal biomechanical parameters could be detected by ophthalmology device8. In addition, the corneal refractive surgery is widely accepted all over the world, and the detection of abnormal biomechanics before refractive surgery is particularly important to avoid complications9. Therefore, it is crucial to estimate the characters of corneal biomechanical parameters.
The Corneal Visualisation Scheimpflug Technology (Corvis-ST) is a relatively new noncontact tonometer, making it available to estimate the corneal biomechanical properties10,11. Previous studies reported that the repeatability of corneal biomechanical parameters was acceptable in normal eyes12,13,14,15. While limited study found the repeatability of intraocular pressure (IOP), central corneal thickness (CCT) and deformation amplitude were adequate in normal and keratoconus eyes16. In addition, the new parameters that improved smoothing algorithm and edge detection have been used in clinical application with the improvement of software. The new Corvis ST Software provides parameters such as the maximum value of the ratio between deformation amplitude at the apex 1 mm and 2 mm from central cornea (DA Ratio Max [1 mm], DA Ratio Max [2 mm]), biomechanical corrected IOP (bIOP), Ambrósio’s Relational Thickness horizontal (ARTh), stiffness parameter at first applanation (SP A1), Corvis Biomechanical Index (CBI)17,18. Recent study found that these new parameters had detectability for distinguishing keratoconus eyes from normal eyes18. However, it had not been reported that the repeatability of these new parameters in keratoconus. Even though repeatability of older parameters has been well established using the Corvis ST, it cannot be assumed that the newer parameters given by the manufacturer’s software are also repeatable. Therefore, the current study aimed to assess the repeatability of the Corvis ST parameters, and explore the factors that influenced the repeatability of new parameters. In addition, we also investigated the differences of parameters between normal and keratoconus eyes, and further evaluated the diagnostic ability of new parameters in detecting keratoconus from normal eyes.
Methods
Study subjects
A prospective, randomized comparative study was performed. Normal subjects and keratoconus patients at Henan Eye Hospital & Henan Eye Institute between September 2017 and December 2018 were enrolled. The diagnosis of keratoconus was based on the following criteria: asymmetric bowtie pattern with or without skewed axes revealed by corneal topography or keratoconus sign detected by slit-lamp examination, such as localized stromal thinning, conical protrusion, Vogt’s striae, Fleischer’s ring or anterior stromal scar19. Keratoconus severity was classified according to the Keratoconus Severity Score Ranking Scheme20. The mild or moderate keratoconus patients without anterior stromal scar and previous ocular surgery, such as corneal collagen cross-linking, intracorneal ring segments or corneal transplantation, were recruited in current study. Subjects eligible for refractive surgery with spherical equivalent <8.00 diopters (D), corneal astigmatism <1.50 D, the value of Best Corrected Visual Acuity (BCVA) in LogMAR ≤ 0.1 were enrolled as the control group. The exclusion criteria was that eyes with pre-existing corneal pathology or previous ocular surgery, rigid contact lens wears within 4 weeks, soft contact lens wears within 2 weeks, serious diabetes, and other eye diseases. Finally, 77 normal subjects (77 right eyes) and 47 mild or moderate keratoconus patients (77 keratoconus eyes) were recruited in current analysis.
Examinations
The data of age, gender, and history of eye diseases was collected from medical records. All the measurements were obtained by the same experienced operator between 9:00 and 17:00. The ocular examinations such as visual acuity, ocular position, slit lamp, ophthalmoscope examination, mydriatic examination and lens insertion optometry were performed by a professional ophthalmologist. The axial measurement (AL) was measured using laser interferometer (IOLMaster, Carl Zeiss Meditec, Germany). The values of steep keratometry (Ks), flat keratometry (Kf), and mean keratometry (Kmean) were detected using Visante Omni anterior segment OCT (Carl Zeiss Jena GmBH, Germany).
All participants received three repeated Corvis ST (Oculus 72100, Wetzlar, Germany) measurements with 2 to 5 minutes interval. The instrument takes Scheimpflug images of the anterior segment at a rate of 4330 frames/s and collects approximately 140 horizontal section images. The following parameters were detected by Corvis ST: IOP, CCT, time from the initiation of air puff until the first applanation (A1T), second applanation (A2T) and maximum deformation (HCT); corneal velocity at the first (A1V) and sccond applanation (A2V); deformation amplitude at the first applanation (A1DA), second applanation (A2DA) and maximum deformation (HCDA); deflection length at the first applanation (A1DLL), second applanation (A2DLL) and maximum deformation (HCDLL); deflection amplitude at the first applanation (A1DLA), second applanation (A2DLA) and maximum deformation (HCDLA); deflection area at the first applanation (A1DLAr), second applanation (A2DLAr) and maximum deformation (HCDLAr); delta arc length at the first applanation (A1dArcL), second applanation (A2dArcL) and maximum deformation (HCdArcL); deformation amplitude Max (DA Max); peak distance (PD) and radius of curvature (Radius); max time and length at deflection amplitude (DLAMT, DLAML); max time and amplitude of whole eye movement (WEMT, WEMA); delta arc length max (dArcLM) and Pachy Slope. The current study used a beta version of Corvis ST Software. Except for the parameters enumerated above, the following new parameters were analyzed: DA Ratio Max [1 mm], DA Ratio Max [2 mm], Max Inverse Radius, bIOP, Integrated Radius, ARTh, SP A1, and CBI. The new Corvis ST parameters in normal eyes and keratoconus eyes were shown in Figs 1 and 2, respectively. A list of abbreviations has been shown in Supplementary Table 1.
Statistical analysis
Continuous variables were described as mean ± standard deviation (SD), and compared by t test. To evaluate the repeatability, the interclass correlation coefficient (ICC) and 95% Confidence interval (CI), Cronbach’ α, and repeatability coefficient (RC) were calculated for each Corvis ST parameter21. The RC, adopted by the British Standards Institution as an indicator of measurement reliability, is based on the common within-subject SD (S w)22. In addition, coefficient of variation (CV) was calculated. To identify factors associated with the reliability of the measurements, we used subject SD (the SD of repeated measurements within each subject) as an indicator of measurement variability23. The liner regression analysis was used to explore the relationship between the subject SD and baseline factors such as age, AL, spherical equivalent, astigmatism, gender, Kmean, IOP and CCT. Linear mixed effects model was used to explore the differences of the Corvis ST parameters between two groups after adjusting for age, CCT and IOP. In addition, the receiver operating characteristic (ROC) curve was used to evaluate the diagnostic ability of Corvis ST parameters for distinguishing keratoconus eyes from normal eyes, and the values of cut-off, sensitivity, specificity, Youden index (the sum of sensitivity and specificity minus 1), area under the ROC curve (AUC) were recorded. The statistical analysis of the survey data was performed using SPSS 23.0 software package and MedCalc software, and P < 0.05 (two-tailed) was considered as statistically significant.
Ethics approval and informed consent
This study has been registered at Chinese Clinical Trial Register (Registration number: ChiCTR-1900023046) and the design was approved by the Institutional Review Board of Henan Eye Hospital [ethical approval number: HNEECKY-2019 (5)]. Written informed consent was obtained from all patients.
Results
Demographics
Seventy-seven eyes of 77 normal subjects and 77 eyes of 47 keratoconus patients were recruited in the current study. The demographic data of participants was shown in Table 1. The mean age was 25.99 ± 3.71 years and 24.58 ± 5.19 years for normal eyes and keratoconus eyes, respectively, with no significant difference between them (P = 0.056). The absolute values of spherical equivalent, astigmatism, Ks, Kf and Kmean in keratoconus eyes were significantly higher than those in normal eyes (all P < 0.05).
Repeatability of Corvis ST parameters
Table 2 and 3 summarized the repeatability values of the Corvis ST parameters. In normal eyes, 18 of 39 parameters (46.15%) showed excellent repeatability (ICC ≥ 0.90), 10 parameters (25.64%) showed good (ICC ≥ 0.75), and 11 parameters (28.21%) showed poor to moderate repeatability (ICC < 0.75). Similarly, 22 parameters (56.41%) demonstrated excellent repeatability, 7 parameters (17.95%) showed good repeatability, and 10 parameters (25.64%) showed poor to moderate repeatability in keratoconus eyes.
Relationship between baseline factors and new Corvis ST parameters repeatability
The correlations between the baseline factors (age, AL, spherical equivalent, astigmatism, gender, Kmean, IOP and CCT) and within-subject SDs of three repeated measurements were analyzed, and the detail results of normal eyes and keratoconus eyes were shown in Supplementary Tables 2 and 3, respectively. The beta coefficients of baseline factors for new parameters repeatability were shown in Table 4. In normal eyes, the ICC of Max Inverse Radius was 0.85, and was associated with spherical equivalent (β = 0.001). The ICC of DA Ratio Max [2 mm] was 0.91, and was associated with AL (β = −0.027), spherical equivalent (β = 0.015) and CCT (β = −0.001). The ICC of Pachy Slope was 0.96, and was associated with AL (β = −0.292) and spherical equivalent (β = 0.177). The ICC of DA Ratio Max [1 mm] was 0.91, and was associated with AL (β = −0.006), spherical equivalent (β = 0.003) and Kmean (β = 0.003). The ICC of ARTh was 0.90, and was associated with gender (β = −0.023) and IOP (β = 4.516). The ICC of bIOP was 0.93, and was associated with AL (β = −0.119) and spherical equivalent (β = 0.064). The ICC of Integrated Radius was 0.92, and was associated with spherical equivalent (β = 0.033). The ICC of SP A1 was 0.92, and was not associated with the baseline factors (P > 0.05). The ICC of CBI was 0.81, and was associated with AL (β = −0.016), spherical equivalent (β = 0.008), astigmatism (β = −0.021), Kmean (β = 0.011), IOP (β = −0.010) and CCT (β = −0.001).
In keratoconus eyes, the ICC of Max Inverse Radius was 0.79, and was not associated with the baseline factors (P > 0.05). The ICC of DA Ratio Max [2 mm] was 0.98, and was associated with Kmean (β = 0.017) and CCT (β = −0.002). The ICC of Pachy Slope was 0.98, and was associated with age (β = −0.247), AL (β = −0.824), Kmean (β = 0.453), IOP (β = −0.749) and CCT (β = −0.048). The ICC of DA Ratio Max [1 mm] was 0.96, and was not associated with the baseline factors (P > 0.05). The ICC of ARTh was 0.99, and was associated with IOP (β = 1.773) and CCT (β = 0.167). The ICC of bIOP was 0.94, and was not associated with the baseline factors (P > 0.05). The ICC of Integrated Radius was 0.98, and was associated with Kmean (β = 0.028), IOP (β = −0.053) and CCT (β = −0.004). The ICC of SP A1 was 0.98, and was associated with spherical equivalent (β = 0.185) and CCT (β = 0.016). The ICC of CBI was 0.95, and was associated with IOP (β = 0.013) and CCT (β = 0.001).
ROC curve analyses of new Corvis ST parameters
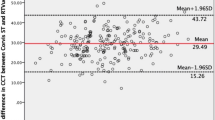
Supplementary Table 4 indicated the differences of Corvis ST parameters between normal eyes and keratoconus eyes. The new parameters except for bIOP were different when adjusting for age, CCT and IOP (Table 5). Compared to normal eyes, the keratoconus eyes had lower values of ARTh, SP A1 and higher values of Max Inverse Radius, DA Ratio Max[2 mm], Pachy Slope, DA Ratio Max[1 mm], Integrated Radius and CBI (All P < 0.05). Further ROC curve analyses of Corvis ST parameters were shown in Supplementary Table 5. Both ARTh and CBI had high Youden index (0.870). With a CBI cut-off value of 0.44, 87.0% of the keratoconus were correctly classified with 88.31% sensitivity and 98.70% specificity. With the ARTh cut-off value of 379.29, 87.0% of the keratoconus were correctly classified with 89.61% sensitivity and 97.40% specificity (P < 0.001, Fig. 3).
Discussion
The corneal biomechanical properties were important in evaluating the ophthalmic examinations before refractive surgery and detecting keratoconus. The current study found that the repeatability of 39 Corvis ST parameters in normal eyes and keratoconus eyes were acceptable and new Corvis ST measurements could help to diagnose keratoconus eyes in clinical application.
The current study showed that the new Corvis ST measurements had relatively high ICC and low RC values, which was consistent with previous study to some extent. Compared with the study conducted in 61 emmetropia subjects, our study found higher repeatability values of CCT, A1V, A2T, HCT, PD, A2DA, and A1DLL parameters, but lower repeatability values of IOP, DA Max, A1T, A2V, A1DA and A2DLL parameters24. Bak-Nielsen et al.13 studied the considerable variation in repeatability of Corvis indices and found the RC values of IOP, CCT, A1T, A1V, A2T and A2V were 1.2, 14, 0.2, 0.1, 0.5 and 0.1, respectively, which was almost in accordance with current results. In addition, studies performed separately by Chen et al.25, Noor et al.12 and Wu et al.26 found that Corvis ST measurements for IOP, CCT, deformation amplitude indices, PD and other corneal parameters were reliable. The controversial results might be attributed to different software versions and different populations. The repeatability research of the Corvis ST parameters in keratoconus eyes was still limit. Only Ye et al.16 reported that the ICC values of IOP, CCT, A1DLL, A2DLL, A1V, A2V, PD and Radius were 0.78, 0.98, 0.30, 0.32, 0.81, 0.50, 0.56 and 0.20 in keratoconus eyes, which were lower than those in our study. Considering there were 12 keratoconus patients in Ye et al.16 study, and the sample size discrepancy might cause this phenomenon. Thus, multi-center researches need to be conducted in further study to certify the repeatability of corneal biomechanics parameters.
Recently, new indices of Corvis ST have been used in clinical examination18. However, there was still limited study related to the repeatability of new parameters. The current study found DA Ratio Max [2 mm], Pachy Slope, DA Ratio Max [1 mm], ARTh, bIOP, Integrated Radius, and SP A1 have excellent repeatability both in normal and keratoconus eyes. The results were consistent with Lopes et al.14 who demonstrated that the new variables presented good precision in healthy eyes, and the corresponding RCs of DA Ratio Max [2 mm], DA Ratio Max [1 mm], integrated radius, Max Inverse Radius, and SP A1 were 0.3601, 0.05263, 0.7202 and 0.00831, respectively. The CBI repeatability in keratoconus eyes was higher than that in normal eyes. The potential reason was that the CBI was calculated by a logistic regression analysis, and the new software could only show a number range of 0–1.
Previous studies found that age, IOP and other basic characters were significantly associated with corneal biomechanical parameters27,28. In addition, Miki et al.15 found that age, AL and CCT had significantly influences on the repeatability of several corneal deformation parameters in healthy subjects. However, the study that explored the effect of baseline factors on the new Corvis ST parameters repeatability in keratoconus eyes has not been reported. The current study indicated that age, AL, spherical equivalent, astigmatism, gender, Kmean, IOP and CCT could affect the repeatability of Corvis ST parameters. The correlations in normal eyes and keratoconus eyes were not absolutely same, and there might be the differences of clinical characters in two groups. Previous studies showed that keratoconus manifested with progressive myopia, serious irregular astigmatism, great values of AL and Kmean, thin cornea thickness, and poor visual acuity29,30. Thus, the baseline factors of subjects should be considered when the Corvis ST parameters were used in clinical application.
The Corvis ST Software is a relatively new device that describes the cornea biomechanical characters, and provides new parameters in diagnosing keratoconus31. The Max Inverse Radius is defined as the maximum value of radius of curvature during concave phase of the deformation32. The DA ratio Max [1 mm] and DA ratio Max [2 mm] are deformation amplitude measured at 1 or 2 mm from the center, and a greater value describes a less resistant for the cornea deformation or a softer cornea. The current study found the values of Max Inverse Radius, DA ratio Max [2 mm], and DA ratio Max [1 mm] in keratoconus eyes were higher than those in normal eyes, which was consistent with Chan et al.17 finding. In addition, Chan et al.17 reported DA Ratio Max [2 mm] (AUC = 0.946), DA Ratio Max [1 mm] (AUC = 0.937), and Max Inverse Radius (AUC = 0.954) offered sufficient discriminative ability in diagnosing keratoconus eyes. Our study had a slightly low AUC value, which might be due to the inconsistent criteria of keratoconus. The Pachy Slope reflects the cornea thickness difference from the center to the periphery, and the study related to the parameter has not been reported. We found the keratoconus eyes had higher values than normal eyes, and age was only found negatively associated with Pachy Slope in keratoconus eyes. The potential reason was that keratoconus patients tend to be young, and the corneal stiffness would change with the age increased33. The ARTh is calculated by the division between corneal thickness at the thinnest point and pachy metric progression index, and lower value means a faster thickness increase toward the periphery or a thinner cornea18. We found keratoconus eyes had lower ARTh value than normal eyes, the Youden index was 0.87 and the AUC was 0.956 at a cut-off value of 379.29. The distinguishing ability of ARTh was effective, which was similar to other studies34,35,36. Hwange et al.34 reported the AUC of ARTh max (AUC = 0.739) could distinguish normal eyes from minimally affected eyes of patients with highly asymmetric keratoconus. Eman et al.35 also found ARTh (AUC = 0.88) was a highly sensitive objective parameter in the fellow eye of unilateral keratoconus. However, Shajari et al.36 demonstrated ARTh max (AUC = 0.613) was no well in differentiating populations at early stages of keratoconus. Considering the discrepancy among different studies, further study of ARTh detection ability would be conducted in the future. The bIOP was derived by finite element simulations that took into account the effects of age, CCT and other dynamic corneal response parameters. The SP A1 is a novel stiffness parameter that defined as resultant pressure divided by deflection at the first applanation, and the force between the external air pressure and IOP were balance at that time18. The CBI was developed based on logistic regression analysis considering the deformation response indices and corneal thickness information. The current study showed the diagnostic ability was 0.870 with 98.70% specificity, 88.31% sensitivity and 0.443 CBI cut-off value. Vinciguerra et al.18 found the keratoconus was corrected with 100% specificity and 94.1% sensitivity when the CBI cut-off value was 0.5. Wang et al.17 found the AUC of CBI was 0.785 in differentiating keratoconus from normal eyes. The CBI and ARTh parameters have the highest Youden index compared with other parameters, which indicated they have good screening ability of detecting keratoconus eyes from normal eyes. In addition, the Youden indexes of DA Ratio Max [1 mm], Integrated Radius, Radius, DA Ratio Max [2 mm] and Pachy Slope were also above 0.70, and further multi-center studies of their diagnostic abilities are warranted in later researches.
The current study investigated the repeatability of the new Corvis ST parameters in normal and keratoconus eyes. However, it needs to be considered that the current study subjects were mostly from Henan Province of China. Therefore, the results can not directly be extrapolated to other regions and further multicenter study should be conducted in the later study.
In conclusion, this study indicated that the repeatability of Corvis ST parameters were acceptable both in normal and keratoconus eyes, and baseline factors could affect the repeatability of new parameters. Furthermore, the new Corvis ST parameters could effectively differentiate the keratoconus from normal eyes, which might help clinicians to diagnose keratoconus.
Data availabilty
All relevant data are included in the paper and its Supporting Information files. Contact to Dr. Shengwei Ren (shengweiren1984@163.com) for additional information regarding data access.
References
Kling, S. & Hafezi, F. Corneal biomechanics - a review. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians 37, 240–252, https://doi.org/10.1111/opo.12345 (2017).
Grise-Dulac, A. et al. Assessment of corneal biomechanical properties in normal tension glaucoma and comparison with open-angle glaucoma, ocular hypertension, and normal eyes. Journal of glaucoma 21, 486–489, https://doi.org/10.1097/IJG.0b013e318220daf0 (2012).
Krachmer, J. H., Feder, R. S. & Belin, M. W. Keratoconus and related noninflammatory corneal thinning disorders. Survey of ophthalmology 28, 293–322 (1984).
Mas Tur, V., MacGregor, C., Jayaswal, R., O’Brart, D. & Maycock, N. A review of keratoconus: Diagnosis, pathophysiology, and genetics. Survey of ophthalmology 62, 770–783, https://doi.org/10.1016/j.survophthal.2017.06.009 (2017).
Mannis, M. J., Ling, J. J., Kyrillos, R. & Barnett, M. Keratoconus and Personality-A Review. Cornea 37, 400–404, https://doi.org/10.1097/ICO.0000000000001479 (2018).
Xu, Z. et al. Characteristic of entire corneal topography and tomography for the detection of sub-clinical keratoconus with Zernike polynomials using Pentacam. Scientific reports 7, 16486, https://doi.org/10.1038/s41598-017-16568-y (2017).
Pniakowska, Z. & Jurowski, P. Detection of the early keratoconus based on corneal biomechanical properties in the refractive surgery candidates. Indian journal of ophthalmology 64, 109–113, https://doi.org/10.4103/0301-4738.179725 (2016).
Dienes, L. et al. Evaluation of intereye corneal asymmetry in patients with keratoconus. A scheimpflug imaging study. PloS one 9, e108882, https://doi.org/10.1371/journal.pone.0108882 (2014).
Ambrosio, R. Jr. et al. Corneal ectasia after LASIK despite low preoperative risk: tomographic and biomechanical findings in the unoperated, stable, fellow eye. Journal of refractive surgery 26, 906–911, https://doi.org/10.3928/1081597X-20100428-02 (2010).
Weed, K. H., MacEwen, C. J., Giles, T., Low, J. & McGhee, C. N. The Dundee University Scottish Keratoconus study: demographics, corneal signs, associated diseases, and eye rubbing. Eye 22, 534–541, https://doi.org/10.1038/sj.eye.6702692 (2008).
Toprak, I., Kucukatay, V., Yildirim, C., Kilic-Toprak, E. & Kilic-Erkek, O. Increased systemic oxidative stress in patients with keratoconus. Eye 28, 285–289, https://doi.org/10.1038/eye.2013.262 (2014).
Ali, N. Q., Patel, D. V. & McGhee, C. N. Biomechanical responses of healthy and keratoconic corneas measured using a noncontact scheimpflug-based tonometer. Investigative ophthalmology & visual science 55, 3651–3659, https://doi.org/10.1167/iovs.13-13715 (2014).
Bak-Nielsen, S., Pedersen, I. B., Ivarsen, A. & Hjortdal, J. Repeatability, reproducibility, and age dependency of dynamic Scheimpflug-based pneumotonometer and its correlation with a dynamic bidirectional pneumotonometry device. Cornea 34, 71–77, https://doi.org/10.1097/ICO.0000000000000293 (2015).
Lopes, B. T. et al. Repeatability and Reproducibility of Intraocular Pressure and Dynamic Corneal Response Parameters Assessed by the Corvis ST. Journal of ophthalmology 2017, 8515742, https://doi.org/10.1155/2017/8515742 (2017).
Miki, A., Maeda, N., Asai, T., Ikuno, Y. & Nishida, K. Measurement repeatability of the dynamic Scheimpflug analyzer. Japanese journal of ophthalmology 61, 433–440, https://doi.org/10.1007/s10384-017-0534-9 (2017).
Ye, C., Yu, M., Lai, G. & Jhanji, V. Variability of Corneal Deformation Response in Normal and Keratoconic Eyes. Optometry and vision science: official publication of the American Academy of Optometry 92, e149–153, https://doi.org/10.1097/OPX.0000000000000628 (2015).
Chan, T. C., Wang, Y. M., Yu, M. & Jhanji, V. Comparison of corneal dynamic parameters and tomographic measurements using Scheimpflug imaging in keratoconus. The British journal of ophthalmology 102, 42–47, https://doi.org/10.1136/bjophthalmol-2017-310355 (2018).
Vinciguerra, R. et al. Detection of Keratoconus With a New Biomechanical Index. Journal of refractive surgery 32, 803–810, https://doi.org/10.3928/1081597X-20160629-01 (2016).
Mas Tur, V. et al. A review of keratoconus: Diagnosis, pathophysiology, and genetics. Survey ophthalmology 62, 770–783 (2017).
McMahon, T. T. et al. A new method for grading the severity of keratoconus: the Keratoconus Severity Score (KSS). Cornea 25, 794–800 (2006).
Shrout, P. E. & Fleiss, J. L. Intraclass correlations: uses in assessing rater reliability. Psychological bulletin 86, 420–428 (1979).
Bland, J. M. & Altman, D. G. Measurement error. Bmj 312, 1654 (1996).
Bland, J. M. & Altman, D. G. Measurement error proportional to the mean. Bmj 313, 106 (1996).
He, M., Wang, W., Ding, H. & Zhong, X. Corneal Biomechanical Properties in High Myopia Measured by Dynamic Scheimpflug Imaging Technology. Optometry and vision science: official publication of the American Academy of Optometry 94, 1074–1080, https://doi.org/10.1097/OPX.0000000000001152 (2017).
Chen, X. et al. Reliability of corneal dynamic scheimpflug analyser measurements in virgin and post-PRK eyes. PloS one 9, e109577, https://doi.org/10.1371/journal.pone.0109577 (2014).
Wu, Y., Tian, L. & Huang, Y. F. In Vivo Corneal Biomechanical Properties with Corneal Visualization Scheimpflug Technology in Chinese Population. BioMed research international 2016, 7840284, https://doi.org/10.1155/2016/7840284 (2016).
Leung, C. K., Ye, C. & Weinreb, R. N. An ultra-high-speed Scheimpflug camera for evaluation of corneal deformation response and its impact on IOP measurement. Investigative ophthalmology & visual science 54, 2885–2892, https://doi.org/10.1167/iovs.12-11563 (2013).
Valbon, B. F., Ambrosio, R. Jr., Fontes, B. M. & Alves, M. R. Effects of age on corneal deformation by non-contact tonometry integrated with an ultra-high-speed (UHS) Scheimpflug camera. Arquivos brasileiros de oftalmologia 76, 229–232 (2013).
Mukhtar, S. & Ambati, B. K. Pediatric keratoconus: a review of the literature. International ophthalmology 38, 2257–2266, https://doi.org/10.1007/s10792-017-0699-8 (2018).
Ernst, B. J. & Hsu, H. Y. Keratoconus association with axial myopia: a prospective biometric study. Eye & contact lens 37, 2–5, https://doi.org/10.1097/ICL.0b013e3181fb2119 (2011).
Mercer, R. N. et al. Comparison of Corneal Deformation Parameters in Keratoconic and Normal Eyes Using a Non-contact Tonometer With a Dynamic Ultra-High-Speed Scheimpflug Camera. Journal of refractive surgery 33, 625–631, https://doi.org/10.3928/1081597X-20170621-03 (2017).
Roberts, C. J. Concepts and misconceptions in corneal biomechanics. Journal of cataract and refractive surgery 40, 862–869, https://doi.org/10.1016/j.jcrs.2014.04.019 (2014).
Kotecha, A., Elsheikh, A., Roberts, C. R., Zhu, H. & Garway-Heath, D. F. Corneal thickness- and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Investigative ophthalmology & visual science 47, 5337–5347, https://doi.org/10.1167/iovs.06-0557 (2006).
Hwang, E. S., Perez-Straziota, C. E., Kim, S. W., Santhiago, M. R. & Randleman, J. B. Distinguishing Highly Asymmetric Keratoconus Eyes Using Combined Scheimpflug and Spectral-Domain OCT Analysis. Ophthalmology 125, 1862–1871, https://doi.org/10.1016/j.ophtha.2018.06.020 (2018).
Awad, E. A., Abou Samra, W. A., Torky, M. A. & El-Kannishy, A. M. Objective and subjective diagnostic parameters in the fellow eye of unilateral keratoconus. BMC ophthalmology 17, 186, https://doi.org/10.1186/s12886-017-0584-2 (2017).
Shajari, M. et al. Early Tomographic Changes in the Eyes of Patients With Keratoconus. Journal of refractive surgery 34, 254–259, https://doi.org/10.3928/1081597X-20180124-01 (2018).
Acknowledgements
This research was supported by the Open Program of Shandong Provincial Key Laboratory of Ophthalmology (2018–04) and Henan Natural Science Foundation (182300410362). The present study was also supported by the Henan Key Laboratory of Ophthalmology and Visual Science and National Key Clinical Specialties Construction Program of China. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
S.W.R. and D.Q.Z. conceived and designed the experiments. K.L.Y. analyzed the data and take responsibility for the integrity and accuracy of the information. L.Y.X. and Q.F. contributed to the reagents/materials/analysis tools. K.L.Y. and S.W.R. drafted and revised the manuscript. All authors have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, K., Xu, L., Fan, Q. et al. Repeatability and comparison of new Corvis ST parameters in normal and keratoconus eyes. Sci Rep 9, 15379 (2019). https://doi.org/10.1038/s41598-019-51502-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51502-4
This article is cited by
-
Keratoconus cone location influences ocular biomechanical parameters measured by the Ocular Response Analyzer
Eye and Vision (2024)
-
Corneal biomechanics in normal and subclinical keratoconus eyes
BMC Ophthalmology (2023)
-
Long-Term Outcomes of Posterior Capsular Opacification in Highly Myopic Eyes and Its Influencing Factors
Ophthalmology and Therapy (2023)
-
Reliability analysis of successive Corvis ST® measurements in keratoconus 2 years after accelerated corneal crosslinking compared to untreated keratoconus corneas
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Die Biomechanik der Hornhaut vor und nach Crosslinking bei Patienten mit Keratokonus
Die Ophthalmologie (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.