Abstract
To estimate the gastroschisis seasonality and trend of prevalence in recent years, stratified by maternal age and geographical clusters of São Paulo state, a population–based study was designed. We used data from the Live Births Information System (SINASC) in São Paulo state, Brazil, from 2005 to 2016. Trends of prevalence were evaluated for the specific subgroups using the Prais–Winsten regression model, and the Durbin–Watson test was used, to estimate the regression coefficient, the annual percent change (APC), and 95% confidence interval (CI). We observed 1576 cases of gastroschisis among 7,317,657 live births (LB), a prevalence of 2.154 (95% CI: 2.047–2.260) per 10,000 LB which included, 50.6% males, 67.4% Caucasians, 53.4% preterm births, and 80.9% caesarean births. The prevalence of gastroschisis significantly increased by 2.6% (95% CI: 0.0–5.2) per year, and this trend was higher in mothers aged 30–34 years (APC: 10.2, 95% CI: 1.4–19.4) than in mothers of other age groups. Between 2011 and 2016, we identified the existence of seasonality based on the date of conception in the middle months of the year (p = 0.002). This is the first and largest population–based study summarizing current epidemiology and identifying trend of prevalence of gastroschisis in São Paulo state.
Similar content being viewed by others
Introduction
Gastroschisis is the most common, abdominal wall defect in which paraumbilical herniation of gastrointestinal structures occurs into the amniotic cavity where it is not covered by any membrane1,2,3, although some authors consider it as an umbilical ring defect4. It is one of the main congenital diseases that require neonatal surgical intervention and is generally associated with high hospital costs, high neonatal morbidity, and mortality1,5. While risk factors for gastroschisis have been implicated, including maternal factors, dietary factors, and chemical exposures6,7,8, its etiology is still unknown. The prevalence of this defect has increased in recent decades6,9,10,11,12. According to Mastroiacovo et al., this increasing rate experienced worldwide is an epidemic13.
The aim of this study is to identify trends in prevalence, seasonality and risk factors of gastroschisis using São Paulo state population database.
Results
From 2005–2016, 1576 gastroschisis cases were reported among 7,317,657 live births (LB) in São Paulo which included 50.6% males (95% CI: 48.1–53), 67.4% Caucasians (95% CI: 65.1–69.7), 53.4% preterm births (<37 weeks gestation), 64.5% births with low weight (<2500 g), 59.1% (95% CI: 56.6–61.5) with seven or more prenatal consultations, 98.4% (95% CI: 97.6–98.9) with single gestation, and 80.9% (95% CI: 78.9–82.8) caesarean births. According to the maternal age group, 691 (43.9%) were young mothers (<20 years) and 67.3% (95% CI: 64.9–69.5) of mothers were between 8 to 11 schooling years (Table 1).
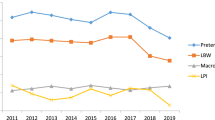
The rate of gastroschisis in São Paulo had increased from 1.75 cases per 10,000 LB in 2005 to 2.23 cases per 10,000 LB in 2016 (overall, 2.15 cases/10,000 LB; 95% CI: 2.05–2.26). The highest and lowest overall prevalence was in 2014 (2.54 cases/10,000 LB; 95% CI: 2.15–2.94) and in 2006 (1.71/10,000 LB; 95% CI: 1.38–2.04), respectively. The highest and lowest overall prevalence was in the Central-South cluster (2.68 cases/10,000 LB; 95% CI: 2.20–3.15) and Taubaté Administrative Region (1.79 cases/10,000 LB; 95% CI: 1.37–2.21), respectively. The highest and lowest number of cases was identified in São Paulo city (471) and Baixada Santista Metropolitan Region (66), respectively. In 2007, the Taubaté Administrative Region presented the lowest annual prevalence (0.31/10,000 LB; 95% CI: 0–0.92), and the highest annual prevalence was in the Central-South cluster (4.4/10,000 LB; 95% CI: 2.26–6.62) (Table 2). To facilitate the visualization of the trends in prevalence, in clusters that present significant results (p < 0.05), we reduced the random variation in the graph, using the third-order centred moving averages technique (Fig. 1).
During 2005–2016, São Paulo state, São Paulo Metropolitan Region and São Paulo City presented an increasing trend of prevalence of gastroschisis, with an annual percent change rate of 2.6%, 4.7%, and 5.0% respectively. According to 2 periods of 6 years each (2005–2010 and 2011–2016), São Paulo state presents an increasing trend of prevalence of gastroschisis only in the first period (APC = 6.7%; 95% CI: 4.0–9.6). Moreover, similar results were found at the Central–North cluster (APC = 36.1%; 95% CI: 8.4–71.4) and at the Northwest cluster (APC = 4.7%; 95% CI: 0.9–8.6) in the second period. All other clusters presented stationary trends (Table 3).
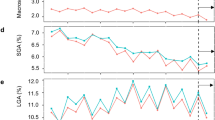
In young mothers (<20 years), the number of LB decreased by 24.4%, from 2005 (104,919) to 2016 (79,298), whereas in older mothers (≥30 years), there was an increase of 30% (182,438 to 237,213), in the same period. Moreover, 691 (43.84%) and 121 (7.68%) cases of gastroschisis were detected in young mothers and older mothers, respectively. The highest gastroschisis prevalence was in mothers aged ≤14 years (9.6/10,000 LB; 95% CI: 6.59–12.62) followed by 15–19 years (6.09/10,000 LB; 95% CI: 5.62–6.56), 20–24 years (3.1/10,000 LB; 95% CI: 2.84–3.36), 25–29 years (1.07/10,000 LB; 95% CI: 0.92–1.22), 30–34 years (0.54/10,000 LB; 95% CI: 0.54–0.66) and ≥35 years (0.39/10,000 LB; 95% CI: 0.26–0.51) (Table 4). Further, to facilitate the visualization of the gastroschisis trends in prevalence by maternal age group, we used the third-order centred moving averages technique (Fig. 2).
The overall prevalence of gastroschisis increased over the course of the study period (2005–2016) in three out of five maternal age groups (Table 4, Fig. 2). The highest increase in gastroschisis prevalence occurred in mothers aged 30–34 years (APC = 10.2%; 95% CI: 1.4–19.4) followed by mothers aged 25–29 years (APC = 6.9%; 95% CI: 0.9–13.0) and 15–19 years (APC = 3.5%; 95% CI: 2.1–5.0), the other age groups presented a stationary trend. A significant increase in gastroschisis prevalence occurred in the 20–24-year age group until 2012, followed by a progressive decrease until 2015, and in 2016, a new increase in the peak was observed that lead to an overall stationary result. In the first period (2005–2010), the highest increasing trend of prevalence occurred in the maternal age group of 25–29 years (APC = 19.7% 95% CI: 0.7 to 42.2). However, in the second period (2011–2016), all maternal age groups had a stationary prevalence trend. (Table 5)
In 2011–2016 a significant seasonal variation in gastrosquisis monthly prevalence rate, based on the month of conception, was found, and it was, on average, 7.4% higher in the middle months of the year compared to the end or beginning months (95% CI: 0.013–0.053; p = 0.002) (Fig. 3).
Discussion
To the best of our knowledge, this is the first population–based study that used the Live Births Information System in São Paulo state to describe the recent seasonality, and prevalence trend of gastroschisis in Brazil.
The prevalence of gastroschisis in São Paulo state from 2005–2016 was 2.15 (95% CI: 2.05–2.26) cases per 10,000 LB, and it significantly increased by 27.61% from 1.74 (95% CI: 1.42–2.08) to 2.23 (95% CI: 1.85–2.61) cases per 10,000 LB, with an increasing annual percent change of 2.6% (95% CI: 0.0–5.2). The increasing prevalence in São Paulo state is concordant with other studies worldwide3,9,10,11,14,15,16,17,18, but not with Li et al.2, which found a decreasing prevalence of gastroschisis in all 14 cities of the Liaoning Province in China from 6.87 to 0.80 per 10,000 LB during 2006–2015.
Although an increasing trend in gastroschisis prevalence was observed in São Paulo from 2005–2016 (APC = 2.6%; 95% CI: 0.0–5.2), significant increasing trend results were observed only in São Paulo city (APC = 5.0%; 95% CI: 1.6–8.4) and São Paulo Metropolitan Region (APC = 4.7%; 95% CI: 0.2–9.1), and this is because all gastroschisis cases in São Paulo city were counted in the São Paulo Metropolitan region as well. When we excluded these cases from the São Paulo Metropolitan Region (SPMR without SPC), the result is a stationary trend (APC = 4,5%; 95% CI: –0.1–10.2) similar to other presented clusters.
In the first period (2005–2010), São Paulo state presented a significant increasing trend in gastroschisis prevalence (APC = 6.7%; 95% CI: 4.0–9.6) and again, only two clusters presented a significant increasing trend, the Central North cluster (APC = 36.1%; 95% CI: 8.4–71.4) and the Northwest cluster (APC = 4.7%; 95% CI: 0.9–8.6), and all other clusters presented a stationary trend. Considering that the Central North cluster and Northwest cluster are predominantly rural areas, it can be suggested that, as in other studies6,7,8, that agricultural exposures, such as the use of pesticides, may have influenced the increasing number of gastroschisis cases in these clusters. At the second period (2011–2016), São Paulo state and all clusters presented a stationary trend, and this is mainly explained by the decrease in gastroschisis prevalence observed since 2015.
The association between young maternal age and gastroschisis is a well–documented risk factor14,15,16,19,20. However, the increase in gastroschisis prevalence is not because of an increase in teen births, since birth rates have decreased among mothers <25 years, and the highest increase in prevalence trend occurred among mothers aged 30–34 years. Our results confirm that young maternal age is a significant risk factor for gastroschisis in São Paulo state. The highest gastroschisis prevalence was in the maternal age group <14 years (9.6 cases/10,000 LB; 95% CI: 6.59–12.62). The lowest gastroschisis prevalence was in the maternal age group >35 years (0.39 cases/10,000 LB; 95% CI: 0.26–0.51). Moreover, the number of LB decreased by 19,76% in the young maternal age groups such as, <14 years, 15–19 years, 20–24 years and 25–29 years, from 2005 (436,188 LB) to 2016 (364,208 LB), and in the same period, the number of gastroschisis cases increased by 17.47%, from 103 (2005) to 121 (2016).
The highest increase in gastroschisis trend of prevalence from 2005–2016 occurred in the maternal age group 30–34 years (APC = 10.2%; 95% CI: 1.4–19.4) despite having a stationary trend in the separated periods (2005–2010 and 2011–2016). In the first period (2005–2010), the highest increase in gastroschisis trend of prevalence occurred among the maternal age group 25–29 years (APC = 19.7%; 95% CI: 0.7–42.2), and at the second period (2011–2016) all maternal age groups presented a stationary trend.
Our findings are consistent with those of other studies that showed that neonates born with gastroschisis are often Caucasian, born preterm, and with low birthweight8,14,15,21,22. Most mothers usually have low educational status, and they are more likely to give birth by cesarean delivery, as in USA1,10,23 and Australia18,24. In the Kirollos et al.25 meta–analysis report, no quantifiable advantage of caesarean section over a vaginal delivery was observed for infants with gastroschisis. In the Salihu et al.26 study, the mode of delivery was not found to be associated with neonatal survival of infants with gastroschisis. Skarsgard27 suggest that as caesarean delivery has not demonstrated any benefits, vaginal delivery should be preferred, unless obstetric factors dictate otherwise.
We observed a significant increase in gastroschisis prevalence when conceptions occurred during the winter months (June, July and August) from May 2011 to April 2016 (95% CI 0.01–0.05, p = 0.002). Waller et al.8 found that from 1987 to 2006 in the Washington state, 805 cases of gastroschisis were detected in conceptions during the spring period. However, from 1995 to 2012 in California state, Anderson et al.10 reported that the risk of gastroschisis did not vary by the season of conception.
This is the first study to demonstrate a significant seasonal variation in the most important state of a large middle–income country such as Brazil, and this may raise some questions: Can the influence of climate change, or ambient air pollution, the use of vaccines or drugs before and/or during pregnancy influence the occurrence of gastroschisis?
There are some limitations to this study. There may have been mistakes during the registration of designations for congenital anomalies in the live birth declaration at the public database. Moreover, we did do not have data regarding stillbirths with gastroschisis.
The strength of this study are as follows. It is a population–based study describing the time trend and seasonality of gastroschisis prevalence in the most populous state in Brazil28 with the highest birth rate28 and with reliable public database29,30. We studied a relatively long time period of data up to 2016 and used, the most recent reports from the Brazilian Unified Health System (DATASUS), which allowed us to analyse both in the total period and in the 2 subperiods of 6 years each.
This is the first and largest population–based study summarizing the current epidemiology and identifying trend of prevalence and seasonality of gastroschisis in the São Paulo state. Our findings demonstrate an increasing trend of prevalence in São Paulo state in recent years, being higher in older mothers and in São Paulo city. The highest overall prevalence was in the Central–South cluster, and the lowest was in Taubaté administrative region. Significant seasonal variation of gastroschisis prevalence was found, being higher, when conceptions occurred during the winter months of the year during 2011–2016.
Methods
Study design & settings
This is a population–based study with time trend31, using official microdata of all cases of gastroschisis identified by the Live Births Information System (SINASC – Sistema de Informação sobre Nascidos Vivos) in São Paulo state, Brazil, from 2005 to 2016 and using data from the Unified Health System Department of Informatics32 (DATASUS – Departamento de Informática do Sistema Único de Saúde), maintained by the Ministry of Health of Brazil. We used the International Classification of Diseases 10th Edition33, code Q79.3 to identify all the cases of gastroschisis, at the LB declaration, among all LB in the period of study.
The unit of analysis selected for this study was São Paulo state, which is the most populous state in Brazil, with a population (41,262,199 in 2010)28 and birth rate (610,000/year)32 comparable to many countries in Europe34,35,36 and Latin America37,38, and where the completeness of public data is more reliable29,30 than other states. Birth data correspond to the period between January 1, 2005, and December 31, 2016.
Participants
We included all LB of mothers residing in São Paulo state, Brazil, whose information in the field of congenital malformations of the Live Birth Certificate was completed with Gastroschisis, identified by the following International Classification of Diseases, 10th Revision, ICD–10: Q79.3. We excluded patients who had a main or secondary diagnosis of Gastroschisis and who had Omphalocele/Exonphalia (ICD–10: Q79.2), hypoplasia/malformation of the abdominal muscles (ICD–10: Q79.5), or umbilical hernia (ICD–10: K42).
Variables
To describe the outcome of this study, sociodemographic and clinical explanatory variables were selected: gender, race/color, gestational age, birth weight, maternal age, maternal schooling, maternal occupation, type of gestation, type of delivery and the number of prenatal consultations.
The number of LB in São Paulo state is provided by SINASC. To construct the rates, they were stratified according to maternal age group and territorial clusters, year by year (for trend) and month by month (for seasonality).
Gastroschisis trends of prevalence were calculated according to maternal age (≤14 years, 15–19 years, 20–24 years, 25–29 years, 30–34 years, ≥35 years) and for territorial clusters determined by the maternal address (São Paulo city – SPC, São Paulo metropolitan region without São Paulo city – SPMR without SPC, São Paulo metropolitan region – SPMR, Baixada Santista metropolitan region – BSMR, Taubaté Administrative region – TAR, Central South cluster – CSC (Sorocaba and Registro Administrative regions), Campinas region cluster – CRC (Campinas, Piracicaba and São João da Boa Vista Administrative regions), Central North cluster – CNC (Bauru, Araraquara, Ribeirão Preto e Franca Administrative regions), Northwest cluster – NWC (Marília, Presidente Prudente, Araçatuba, São José do Rio Preto and Barretos Administrative regions), and São Paulo state – SPS) in São Paulo state (Fig. 4). These clusters were grouped by similar territorial characteristics from the geographical delimitation of the administrative areas previously stipulated by government agencies39 and used by DATASUS. This procedure ensured a sufficient number of cases and stabilized the analyzis.
Data sources
The microdata was extracted from the file transfer service provided by DATASUS. The TABNET and TABWIN programs were used to consult the data. Those tabs were developed to perform fast tabulations on.DBF files, then the files were exported to.XLS version; further, the variables selected for this study were classified in EXCEL®. In order to minimize possible discrepancies, the data were collected by two different researchers independently.
The Live Birth Information System was developed by DATASUS to gather epidemiological information on births reported throughout the country to subsidize interventions related to women’s and children’s health for all levels of the Unified Health System (SUS – Sistema Único de Saúde), such as actions of attention to the pregnant woman and to the newborn, as well as the monitoring of the evolution of the SINASC’s historical series, that allows the identification of intervention priorities and contribution to the effective improvement of this information system. Through the Internet, DATASUS and the Health Surveillance Service (SVS – Sistema de Vigilância em Saúde) provide the main information for tabulation on the SINASC’s Databases.
Bias
Only the population of LB was used to obtain the prevalence rates and the proportion of maternal age range did not differ in the linear regression model by clusters in São Paulo state (p > 0.05). With this, the result obtained by the analysis can be used for comparison to other studies.
Some limitations have been identified, inherent in the recording of public data, in the data collection stages and, in the quality of the information where there were fields with missing data, until the transmission of the data to the information systems.
Statistical methods
Gastroschisis prevalence rates were calculated for 10,000 LB by maternal age group and territorial clusters. For prevalence, in addition to the global period (2005–2016) 2 time intervals of 6 consecutive years each (2005–2010 and 2011–2016) were used.
For trends analysis, the Prais–Winsten regression model, following Antunes and Cardoso31 methodological indications, were used. The dependent variable was the logarithm of the rates, and the independent variable, and the years of the historical series. The Annual Percent Change (APC) of the rates was also calculated, as suggested by Antunes and Waldman (2002)40.
The data modelling process includes, transforming the standardized rates into a base 10 logarithmic function using the Durbin–Watson test to measure the existence of the first–order autocorrelation of the time series composed of the annual coefficients, as well as to verify that the correlation was compatible with the random regression residuals hypothesis. Annual rates of increase or decrease (APC), according to maternal age and geographic clusters, were then calculated, with the respective confidence intervals (95% CI). This procedure makes it possible to classify gastroschisis trend, as increasing, decreasing, or stationary. The trend was, considered to be stationary when the coefficient was not significantly different from zero (p > 0.05)31. To facilitate the visualization of trends, the third order centred moving averages technique was performed for trends and for seasonality40,41, without the outliers (Figs 1–3).
To model seasonality we used monthly measurements for LB with gastroschisis. For monthly measurements, calendar month was numbered sequentially (totalling 66 months during 2011–2016). In addition, to identify seasonal variations, gastroschisis monthly prevalence rates were calculated on the basis of the date of conception. Antunes and Waldman40 methodological indications were used for the seasonality hypothesis test. The seasonal variation was considered significant if one or more of the coefficients of the seasonal term (B3 and B5 for Seno and B2 and B4 for Cosseno) were statistically different from zero (p < 0.05)31. All statistical analyses, were performed using STATA 15.1 (CollegeStation, TX, 2018) conducted between February 2018, and August 2019.
Data Availability
The microdata used for this study are administered by the Live Births Information System (SINASC – Sistema de Informação sobre Nascidos Vivos), using data from the Unified Health System Department of Informatics (DATASUS – Departamento de Informática do Sistema Único de Saúde), maintained by the Ministry of Health of Brazil. DATASUS provides open public access to these data for any purposes. www.datasus.saude.gov.br, http://datasus.saude.gov.br/informacoes-de-saude/tabnet/estatisticas-vitais.
References
Fullerton, B. S. et al. Contemporary Outcomes of Infants with Gastroschisis in North America: A Multicenter Cohort Study. The Journal of pediatrics 188, 192–197.e196, https://doi.org/10.1016/j.jpeds.2017.06.013 (2017).
Li, N. et al. Decreasing prevalence and time trend of gastroschisis in 14 cities of Liaoning Province: 2006–2015. Scientific reports 6, 33333, https://doi.org/10.1038/srep33333 (2016).
Mastroiacovo, P. et al. Gastroschisis and associated defects: an international study. American journal of medical genetics. Part A 143a, 660–671, https://doi.org/10.1002/ajmg.a.31607 (2007).
Rittler, M., Vauthay, L. & Mazzitelli, N. Gastroschisis is a defect of the umbilical ring: evidence from morphological evaluation of stillborn fetuses. Birth defects research. Part A, Clinical and molecular teratology 97, 198–209, https://doi.org/10.1002/bdra.23130 (2013).
Apfeld, J. C. et al. Infant, maternal, and geographic factors influencing gastroschisis related mortality in Zimbabwe. Surgery 158, 1475–1480, https://doi.org/10.1016/j.surg.2015.04.037 (2015).
Souther, C., Puapong, D. P., Woo, R. & Johnson, S. M. Possible etiologies of increased incidence of gastroschisis. Pediatr Surg Int 33, 1209–1213, https://doi.org/10.1007/s00383-017-4166-4 (2017).
Agopian, A. J., Langlois, P. H., Cai, Y., Canfield, M. A. & Lupo, P. J. Maternal residential atrazine exposure and gastroschisis by maternal age. Matern Child Health J 17, 1768–1775, https://doi.org/10.1007/s10995-012-1196-3 (2013).
Waller, S. A., Paul, K., Peterson, S. E. & Hitti, J. E. Agricultural-related chemical exposures, season of conception, and risk of gastroschisis in Washington State. American journal of obstetrics and gynecology 202(241), e241–246, https://doi.org/10.1016/j.ajog.2010.01.023 (2010).
Anderson, J. E. et al. Incidence of Gastroschisis in California. JAMA surgery. https://doi.org/10.1001/jamasurg.2018.1744 (2018).
Anderson, J. E. et al. Epidemiology of gastroschisis: A population-based study in California from 1995 to 2012. J Pediatr Surg, https://doi.org/10.1016/j.jpedsurg.2018.08.035 (2018).
Kirby, R. S. The prevalence of selected major birth defects in the United States. Seminars in perinatology 41, 338–344, https://doi.org/10.1053/j.semperi.2017.07.004 (2017).
Loane, M., Dolk, H. & Bradbury, I. Increasing prevalence of gastroschisis in Europe 1980-2002: a phenomenon restricted to younger mothers? Paediatric and perinatal epidemiology 21, 363–369, https://doi.org/10.1111/j.1365-3016.2007.00820.x (2007).
Mastroiacovo, P., Lisi, A. & Castilla, E. E. The incidence of gastroschisis: research urgently needs resources. BMJ (Clinical research ed.) 332, 423–424, https://doi.org/10.1136/bmj.332.7538.423-a (2006).
Allman, R. et al. The epidemiology, prevalence and hospital outcomes of infants with gastroschisis. Journal of perinatology: official journal of the California Perinatal Association 36, 901–905, https://doi.org/10.1038/jp.2016.99 (2016).
Friedman, A. M., Ananth, C. V., Siddiq, Z., D’Alton, M. E. & Wright, J. D. Gastroschisis: epidemiology and mode of delivery, 2005–2013. American journal of obstetrics and gynecology 215(348), e341–349, https://doi.org/10.1016/j.ajog.2016.03.039 (2016).
Jones, A. M. et al. Increasing Prevalence of Gastroschisis–14 States, 1995-2012. MMWR. Morbidity and mortality weekly report 65, 23–26, https://doi.org/10.15585/mmwr.mm6502a2 (2016).
Castilla, E. E., Mastroiacovo, P. & Orioli, I. M. Gastroschisis: international epidemiology and public health perspectives. American journal of medical genetics. Part C. Seminars in medical genetics 148c, 162–179, https://doi.org/10.1002/ajmg.c.30181 (2008).
Kong, J. Y. et al. Outcomes of infants with abdominal wall defects over 18 years. J Pediatr Surg 51, 1644–1649, https://doi.org/10.1016/j.jpedsurg.2016.06.003 (2016).
Nazer, H. J., Karachon Essedin, L., Cifuentes Ovalle, L. & Assar Cuevas, R. Gastroschisis: A pandemic with increasing rates? ECLAMC experience in Chile 1982–2015. Revista chilena de pediatria 87, 380–386, https://doi.org/10.1016/j.rchipe.2016.06.003 (2016).
Shariff, F. et al. Maternal and community predictors of gastroschisis and congenital diaphragmatic hernia in Canada. Pediatr Surg Int 31, 1055–1060, https://doi.org/10.1007/s00383-015-3797-6 (2015).
Feldkamp, M. L., Botto, L. D., Byrne, J. L., Krikov, S. & Carey, J. C. Clinical presentation and survival in a population-based cohort of infants with gastroschisis in Utah, 1997–2011. American journal of medical genetics. Part A 170a, 306–315, https://doi.org/10.1002/ajmg.a.37437 (2016).
Frolov, P., Alali, J. & Klein, M. D. Clinical risk factors for gastroschisis and omphalocele in humans: a review of the literature. Pediatr Surg Int 26, 1135–1148, https://doi.org/10.1007/s00383-010-2701-7 (2010).
Duncan, J. et al. Mode of delivery in pregnancies with gastroschisis according to delivery institution. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet, 1–4, https://doi.org/10.1080/14767058.2018.1450860 (2018).
Abdel-Latif, M. E., Bolisetty, S., Abeywardana, S. & Lui, K. Mode of delivery and neonatal survival of infants with gastroschisis in Australia and New Zealand. J Pediatr Surg 43, 1685–1690, https://doi.org/10.1016/j.jpedsurg.2008.03.053 (2008).
Kirollos, D. W. & Abdel-Latif, M. E. Mode of delivery and outcomes of infants with gastroschisis: a meta-analysis of observational studies. Archives of disease in childhood. Fetal and neonatal edition 103, F355–f363, https://doi.org/10.1136/archdischild-2016-312394 (2018).
Salihu, H. M. et al. Mode of delivery and neonatal survival of infants with isolated gastroschisis. Obstetrics and gynecology 104, 678–683, https://doi.org/10.1097/01.aog.0000139513.93115.81 (2004).
Skarsgard, E. D. Management of gastroschisis. Current opinion in pediatrics 28, 363–369, https://doi.org/10.1097/mop.0000000000000336 (2016).
IBGE. Censo Demográfico 2010, https://biblioteca.ibge.gov.br/visualizacao/periodicos/93/cd_2010_caracteristicas_populacao_domicilios.pdf (2011).
Gabriel, G. P. et al. Evaluation of Data on Live Birth Certificates from the Information System on Live Births (SINASC) in Campinas, São Paulo, 2009. Revista Paulista de Pediatria 32, 183–188 (2014).
Prado, M. F. & Marques, C. C. A. Health Information Systems: An Experience of decentralized production of information on mortality and live births for use in health surveillance in the State of Sao Paulo. BEPA. Boletim Epidemiológico Paulista (Online) 9, 04–15 (2012).
Antunes, J. L. F. & Cardoso, M. R. A. Using time series analysis in epidemiological studies. Epidemiologia e Serviços de Saúde 24, 565–576 (2015).
Brasil, M. d. S. DATASUS - Base de Dados do Sistema Único de Saúde, http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvsp.def (2018).
Organization, W. H. International statistical classification of diseases and related health problems. Vol. 1 (World Health Organization, 2004).
Castagnaro, C., Guarneri, A. & Prati, S. ISTAT (ed ISTA) 10 (ISTAT, ISTAT, 2018).
(Spain), I. N. d. E. Birth Statistics. Vital statistics, https://www.ine.es/dyngs/INEbase/en/operacion.htm?c=Estadistica_C&cid=1254736177007&menu=resultados&secc=1254736195442&idp=1254735573002 (2018).
Haines, N. (ed. Office for National Statistics) 10 (ONS, www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2016, (2017).
Salud, D. d. E. e. I. d. Natalidad, http://www.deis.cl/wp-content/uploads/2011/05/SerieNacimientos_2000_2015.html (2019).
(Colombia), S. E. N. Nascimientos 2017, https://www.dane.gov.co/index.php/estadisticas-por-tema/salud/nacimientos-y-defunciones/nacimientos/nacimientos-2017 (2019).
Redes de Atenção à Saúde e respectivas Regiões de Saúde. Estado de São Paulo, http://www.saude.sp.gov.br/resources/ses/perfil/gestor/documentos-de-planejamento-em-saude/mapa-de-saude/estado_rras_drs_rs.jpg (2012).
Ferreira Antunes, J. L. & Alves Waldman, E. Trends and spatial distribution of deaths of children aged 12–60 months in São Paulo, Brazil, 1980–1998 (2002).
Perea, L. M. E., Peres, M. A., Boing, A. F. & Antunes, J. L. F. Trend of oral and pharyngeal cancer mortality in Brazil in the period of 2002 to 2013. Rev Saude Publica 52, 10, https://doi.org/10.11606/S1518-8787.2018052000251 (2018).
Author information
Authors and Affiliations
Contributions
M.G.C., E.F.S.S. and R.D.R. designed research; M.G.C. and E.F.S.S. conducted research, M.G.C., E.F.S.S., L.C.A. and R.D.R. analyzed data, L.C.A. and R.D.R. conducted critical analysis and M.G.C. wrote the manuscript. All authors read, reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Calderon, M.G., Santos, E.F.d.S., Abreu, L.C.d. et al. Increasing prevalence, time trend and seasonality of gastroschisis in São Paulo state, Brazil, 2005–2016. Sci Rep 9, 14491 (2019). https://doi.org/10.1038/s41598-019-50935-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50935-1
This article is cited by
-
Predictors of length of stay for simple gastroschisis: analysis of ACS NSQIP-P database
Pediatric Surgery International (2022)
-
Congenital heart diseases trends in São Paulo State, Brazil: a national live birth data bank analysis
World Journal of Pediatrics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.