Abstract
To evaluate whether a recombinant serine protease inhibitor (rBmTI-A) modulates inflammation in an experimental model of chronic allergic lung inflammation. Balb/c mice were divided into four groups: SAL (saline), OVA (sensitized with ovalbumin), SAL + rBmTI-A (control treated with rBmTI-A) and OVA + rBmTI-A (sensitized with ovalbumin and treated with rBmTI-A). The animals received an intraperitoneal injection of saline or ovalbumin, according to the group. The groups received inhalation with saline or ovalbumin and were treated with rBmTI-A or saline by nasal instillation. After 29 days, we evaluated the respiratory mechanics; bronchoalveolar lavage fluid (BALF); cytokines; MMP-9, TIMP-1; eosinophils; collagen and elastic fibre expression in the airways; and the trypsin-like, MMP-1, and MMP-9 lung tissue proteolytic activity. Treatment with rBmTI-A reduced the trypsin-like proteolytic activity, the elastance and resistance maximum response, the polymorphonuclear cells, IL-5, IL-10, IL-13 and IL-17A in the BALF, the expression of IL-5, IL-13, IL-17, CD4+, MMP-9, TIMP-1, eosinophils, collagen and elastic fibres in the airways of the OVA + rBmTI-A group compared to the OVA group (p < 0.05). rBmTI-A attenuated bronchial hyperresponsiveness, inflammation and remodelling in this experimental model of chronic allergic pulmonary inflammation. This inhibitor may serve as a potential therapeutic tool for asthma treatment.
Similar content being viewed by others
Introduction
Asthma is a chronic inflammatory disease of the airway that is considered one of the most common chronic conditions, affecting both children and adults, and is associated with high morbidity and mortality, representing a worldwide health problem1.
Many cells of the innate and adaptive immune system act together with epithelial cells in asthma, causing bronchial hyperreactivity, increased mucus production, remodelling and narrowing of the airways2, vasodilation and plasma exudation3.
There is evidence that an imbalance between proteases and their inhibitors plays an important role in the development of asthma4. This effect can be observed more clearly in periods of exacerbation5.
Protein enzyme inhibitors play an important regulatory role in the cells that participate in inflammatory processes, suggesting that there is a possible use for these molecules for pharmacological purposes6. In respiratory disease models, some protease inhibitors have been tested, and their potential airway anti-inflammatory effects have been demonstrated7,8,9.
BmTI-A (Boophilus microplus trypsin inhibitor), a serine protease inhibitor extracted from the Rhipicephalus Boophilus microplus tick, showed inhibitory activities on bovine trypsin, human plasma kallikrein and human neutrophil elastase (HNE)10,11. In a mouse model of pulmonary emphysema, rBmTI-A caused a reduction in the total number of cells in the BALF, in the number of positive cells for MMP-12 and in the collagen fibre volume12.
The search for new effective therapies for the treatment of asthma is necessary and is a high priority, especially for asthmatic individuals whose symptoms are not well controlled by the medications that are currently available13. There is also a need to develop new therapeutic approaches that are capable of reversing and preventing asthma remodelling because corticosteroids do not act directly on the structural alterations of the airways14.
Considering the need for new therapies for asthma treatment and the great potential of serine protease inhibitors as therapeutic agents in respiratory disease models, the present study investigated the effects of rBmTI-A, a recombinant serine protease inhibitor, as a treatment for chronic allergic pulmonary inflammation in mice.
Results
Respiratory system mechanics
The respiratory system elastance (Ers) values for all animals are shown in Fig. 1(A). The OVA group had increased Ers values compared to those of the control groups (p < 0.05). The animals treated with the proteinase inhibitor rBmTI-A had decreased Ers values compared to those of the OVA group (p < 0.05).
Effects of rBmTI-A treatment on the pulmonary mechanics. (A) Respiratory system elastance (Ers) and (B) respiratory system resistance (Rrs) of all experimental groups after a challenge with methacholine (300 mg/mL). Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
Figure 1(B) presents the respiratory system resistance (Rrs) values for all the experimental groups. There was a significant increase in the Rrs of the OVA group compared to those of the control groups (p < 0.05). The group that was sensitized and received rBmTI-A (OVA + rBmTI-A) had a reduction in Rrs values compared to those of the OVA group (p < 0.05).
Morphometric analysis
Eosinophils density
The eosinophil recruitment to the airway walls is presented in Fig. 2. There was an increase in the number of eosinophils (cells/104 μm2) in the ovalbumin-exposed animals (OVA and OVA + rBmTI-A) compared with that in the control groups (p < 0.001). The sensitized animals that were treated with rBmTI-A (OVA + rBmTI-A) had a reduction in the number of eosinophils compared to that of the OVA group (p < 0.05).
Extracellular matrix remodelling
Figure 3(A,B) show the volume fractions of collagen and elastic fibres in the airway walls, respectively. There was an increase in the volume fraction of the collagen and elastic fibres (p < 0.05) in the airway walls of the OVA group compared to those in the control groups. Compared with the OVA group, treatment with the inhibitor rBmTI-A reduced the fractions of collagen and elastic fibres (p < 0.05) in the airway walls.
Effects of rBmTI-A treatment on extracellular matrix remodelling. (A) Collagen fibres and (B) elastic fibre volume fractions in the airway walls. (C) MMP-9 and (D) TIMP-1 expression in the airway walls of the four experimental groups. Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
The MMP-9- and TIMP-1-positive cells in the airway walls are shown in Fig. 3(C,D). The numbers of MMP-9- and TIMP-1-positive cells were greater in the OVA group compared with those in the control groups (p < 0.05). The OVA + rBmTI-A group had a decreased number of MMP-9- and TIMP-1-positive cells compared to those in the OVA group (p < 0.05).
Lung inflammation
The inflammatory cells in the airway walls of the four experimental groups are shown in Fig. 4(A) (IL-4), 4(B) (IL-5), 4(C) (IL-10), 4(D) (IL-13), 4(E) (IL-17), 4(F) (CD4+) and 4(G) (CD8+). The IL-5, IL-10, IL-13, IL-17, CD4+ and CD8 + positive cells were increased in the OVA group compared to those in the control groups (p < 0.05). The sensitized animals that were treated with the serine protease inhibitor (OVA + rBmTI-A group) showed decreased IL-5, IL-10, IL-13, IL-17 and CD4+ positive cells in the airway walls compared to those in the OVA group (p < 0.05).
Effects of rBmTI-A treatment on the inflammatory response. (A) IL-4, (B) IL-5, (C) IL-10, (D) IL-13, (E) IL-17, (F) CD4+ and (G) CD8+ positive cells in the airway walls in all experimental groups. Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
Bronchoalveolar lavage fluid (BALF)
The inflammatory cells in the BALF samples from all experimental groups are shown in Fig. 5(A) (total cells), 5(B) (polymorphonuclear cells), 5(C) (macrophages) and 5(D) (lymphocytes). In the OVA group, we found an increase in the number of total cells and of polymorphonuclear cells (p < 0.05) compared to those in the control groups. The number of polymorphonuclear cells from the sensitized group was reduced by the treatment in the OVA + rBmTI-A group compared to that in the OVA group (p < 0.05).
Effects of rBmTI-A treatment on the BALF inflammatory cells. (A) Total cells, (B) polymorphonuclear cells, (C) macrophages and (D) lymphocytes in all experimental groups. Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
The cellular inflammation markers are presented in Fig. 6(A) (IL-4), 6(B) (IL-5), 6(C) (IL-10), 6(D) (IL-13), 6(E) (IL-17A) and 6(F) (INF- γ) The concentrations of IL-4, IL-5, IL-13 and IL-17A in the OVA group were higher than those in the control groups (p < 0.05). Treatment with the serine protease inhibitor reduced the concentrations of IL-5, IL-10, IL-13 and IL-17A in the OVA + rBmTI-A group compared to those in the OVA group (p < 0.05).
Effects of rBmTI-A treatment on the BALF inflammatory markers. (A) IL-4, (B) IL-5, (C) IL-10, (D) IL-13, (E) IL-17A and (F) INF-γ levels in all experimental groups. Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
Proteolytic Activity in pulmonary homogenate
There were not significant differences among the groups in the proteolytic activity of MMP-1 and MMP-9, as depicted in Fig. 7(A).
Effects of rBmTI-A treatment on the MMP1-1/MMP-9 (A) and trypsin-like (B) proteolytic activity in the pulmonary homogenate of all experimental groups. Data are presented as the mean and SE. The differences were considered significant when p < 0.05. *p < 0.05 vs. control groups; **p < 0.05 vs. OVA group.
Figure 7(B) shows the trypsin-like serine protease proteolytic activity for all the experimental groups. There was an increase in the trypsin-like activity in the OVA group compared to that in the control groups (p < 0.05). The sensitized group that was treated with the inhibitor rBmTI-A showed a reduction in this activity compared to that in the OVA group (p < 0.05).
Qualitative analysis
Representative airway photomicrographs from the four experimental groups are shown in Figs 8 and 9. The sections were stained with Luna for the detection of eosinophils (Fig. 8(A)); with picrosirius for the detection of collagen content (Fig. 8(B)); and Weigert’s resorcin-fuchsin for the detection of the elastic fibre content (Fig. 8(C)). Figure 9 shows the quantification by immunohistochemistry of the cytokine expression (A–C) and of the metalloproteinase inhibitor expression (TIMP-1, (D)).
Representative photomicrographs of mouse lung airway walls from all experimental groups. The sections underwent specific staining for the detection of (A) eosinophils (stained red); (B) collagen fibres (stained red); and (C) elastic fibres (stained deep purple). 400× magnification. The red arrows indicate positive cells. The inserts with larger magnification show the positive cells in detail.
Inflammatory and extracellular matrix remodelling markers in the airways of all experimental groups. (A) IL-5; (B) IL-10; (C) TIMP-1. 400× magnification. Positive cells are stained brown, and the red arrows indicate positive cells. The inserts with larger magnification show the positive cells in detail.
We observed an increase in the number of eosinophils, collagen and elastic fibre content and in the IL-5, IL-10 and TIMP-1 airway expression in the OVA group compared to those in the control groups (SAL and SAL + rBmTI-A). Treatment with rBmTI-A attenuated these increases in the OVA + rBmTI-A group compared to that in the OVA group.
Discussion
In the present study, we evaluated the effect of the serine protease inhibitor rBmTI-A in an experimental model of chronic allergic pulmonary inflammation. We demonstrated that treatment with rBmTI-A reduced the trypsin-like proteolytic activity in the pulmonary homogenate. Compared to those of the controls, this result, in the animals that were sensitized with ovalbumin and that were treated with rBmTI-A, was associated with the attenuation of airway hyperresponsiveness after challenge with the bronchoconstrictor methacholine; the reduction of eosinophil numbers in the BALF and in the airways; decreased expression of Th2/Th17 (IL-5, IL-10, IL-13 and IL-17) inflammatory cytokines in the BALF and in the airways; the reduction of CD4+ positive cells in the airways; attenuation of the MMP-9 and TIMP-1 expression in the airways; and the decrease of the extracellular matrix remodelling, as evaluated by the reduction of the collagen and elastic fibre content in the airways.
Experimental models of murine chronic allergic lung inflammation have been widely used because they reproduce important characteristics of the immune and inflammatory response in asthma15,16. The Balb/c mice used in our experimental model also have good Th2 profile immunological response17 and good reactivity to methacholine18.
A previous study demonstrated that the administration of rBmTI-A had as much of a protective effect against the development and progression of pulmonary emphysema as the effect of treatment after the development of the disease, with a decrease in the distal air spaces in treated animals. This was the first study using animals that were treated with rBmTI-A. This study compared the effect of the treatment with one dose of rBmTI-A (35.54 pmol in 50 μL of saline solution) to the effect of treatment with two doses of rBmTI-A (same concentration), with one dose at the beginning of the sensitization protocol and another at the end12. Based on this study, we designed our treatment protocol.
There is evidence that the imbalance between proteases and their inhibitors plays an important role in the development of asthma4, and that this effect is more pronounced in the periods of disease exacerbation5.
The participation of trypsin-like serine proteases in asthma, such as human plasma kallikrein (HuPK)19, neutrophil elastase4 and trypsin20, has been reported in some studies. The role of neutrophil elastase and trypsin in asthma is even more evident in the presence of a deficiency of alpha-1 antitrypsin, a known serine protease inhibitor, which is able to inhibit some enzymes, such as trypsin, neutrophil elastase and protease-321.
Several trypsin-like serine protease inhibitors have been studied as therapeutic tools for the treatment of several pathologies, such as thrombosis, asthma and COPD22.
Some studies have shown the BmTI-A inhibitory activity for HuPK, neutrophil elastase and trypsin10,11,23. These findings corroborate the results that we obtained using recombinant BmTI-A since we observed a reduction of the trypsin-like proteolytic activity in the pulmonary homogenate of animals that were sensitized and treated with rBmTI-A compared to that in the sensitized group that did not receive the inhibitor.
Experimental models of chronic allergic inflammation showed a significant elevation of the Ers and Rrs when treated with an intravenous administration of methacholine18,24. In the present study, the animals that were sensitized and treated with the serine protease inhibitor rBmTI-A showed a reduction of approximately 30% in the Ers and 37% in the Rrs when compared to those in the sensitized and untreated groups. Other serine protease inhibitors have also showed the ability to attenuate these pulmonary responses; for example, the CrataBL inhibitor reduced the Ers and Rrs values in mice with chronic allergic pulmonary inflammation25. Three inhibitors of serine proteases, FOY, FUT and UTI, reduced the Ers and Rrs values in a model of chronic allergic pulmonary inflammation26. Saw and Arora (2015) also observed a reduction of the pulmonary resistance in murine with airway allergic inflammation that were treated with the serine protease inhibitor AEBSF27.
Remodelling is related to the decreased lung function in individuals with asthma and in asthmatic animal models and may be a determining factor for hyperresponsiveness16. In asthma, the remodelling process involves the deposition of collagen and elastic fibres28; MMP-9 is one of the main metalloproteases involved in this process, as it is capable of degrading many types of collagen, gelatin, elastin proteins, fibronectin and other extracellular matrix components14, and MMP-9 is directly related to the severity of asthma29.
The inhibitor rBmTI-A effectively attenuated remodelling, decreasing the percentage of collagen and elastic fibres in the airways of the sensitized animals compared to those in the controls. In a murine model of elastase-induced pulmonary emphysema, rBmTI-A also reduced the percentage of collagen and elastic fibres in the pulmonary parenchyma30; however, in a previous study with a different experimental model, rBmTI-A attenuated only the percentage of collagen fibres12. The CrataBL serine protease inhibitor also reduced the fraction of collagen and elastic fibres in a murine asthma model12. Another protease inhibitor, EcTI, also attenuated the deposition of these fibres in a pulmonary emphysema model9.
In association with the increase of collagen and elastic fibres in the airways of the OVA group, we observed an increase in the expression of MMP-9. The sensitized animals that received rBmTI-A showed a decrease in airway MMP-9 expression.
The regulation of MMP-9 secretion in the airways is complex since several inflammatory and structural cells are able to produce this protease31. The activation of MMPs involves other MMPs and serine proteases, which may explain the reduction of MMP-9 release in the sensitized group that received the rBmTI-A serine protease inhibitor32. The protease-activated receptor (PAR-2) releases MMP-9 through the airway epithelial cells and is activated primarily by serine proteases such as trypsin and tryptase33. Considering that there was a decrease in the trypsin-like proteolytic activity in the pulmonary homogenate of the sensitized animals that received rBmTI-A compared to that of the controls, possibly also occurred a reduction of PAR-2 activation by trypsin and a consequent decrease in the release of MMP-9, deposition of collagen and elastic fibres observed in this same group.
One of the regulatory mechanisms of MMPs is the balance between the proteolytic/anti-proteolytic activity since the deregulation of MMPs and their endogenous tissue inhibitors, TIMPs, plays an important role in tissue remodelling processes34. Righetti et al.35 showed an increase in the MMP-9-specific metalloprotease inhibitor TIMP-1 in asthma, as was also observed in our experimental model. In addition, treatment with rBmTI-A attenuated the increase in TIMP-135. This attenuation probably occurred in association with the reduction of MMP-9 expression in the sensitized and rBmTI-A treated groups, maintaining the balance of the proteolytic activity in this group. This decrease was also observed in another study using the same experimental asthma model that was treated with the CrataBL serine protease inhibitor25.
Our data also showed that there was an increase in the eosinophilic infiltrate in the airways of animals that were sensitized with ovalbumin. Notwithstanding, treatment with rBmTI-A significantly attenuated this response in the animals sensitized and treated with the inhibitor. The CrataBL serine protease inhibitor also reduced the eosinophilic infiltrate in the airways of mice that were sensitized with ovalbumin25. This effect was also observed in response to treatment with the inhibitors FOY, FUT and UTI in another model of chronic allergic pulmonary inflammation26.
Eosinophilic inflammation is increased in several asthma models16,36,37. In humans, there is evidence that even in mild forms of asthma, there is persistent chronic inflammation of the airways, with increasing numbers of eosinophils and other inflammatory cells3.
In the bronchoalveolar lavage fluid(BALF) cell evaluation, as observed in other studies, the numbers of total cells, polymorphonuclear cells and lymphocytes were increased in the BALF of the sensitized group compared to those in the control groups16,25,38.
The increased number of polymorphonuclear cells in the BALF from the OVA group was probably due to the increase in eosinophils since in the analysis of the tissues with eosinophil-specific staining (LUNA), we observed that the cells around the airways were mostly eosinophils. An increase in the number of eosinophils in the BALF has been consistently reported among asthmatic individuals, and the increase correlates with the severity of the disease39.
In the group that was sensitized and treated with rBmTI-A, there was a reduction in the number of polymorphonuclear cells in the BALF. However, rBmTI-A treatment did not attenuate the lymphocyte response, as in another study that evaluated the effect of rBmTI-A on pulmonary emphysema in a murine model12. The reduction in the eosinophil content in the sensitized murine BALF was also observed in studies that used other serine protease inhibitors, such as CrataBL25, Nafamostat Mesylate40, FOY, FUT, UTI26 and the AEBSF inhibitor27.
We evaluated the concentration of cytokines in the BALF and in the airways, and in both analyses, we observed a reduction in IL-5, IL-10, IL-13 and IL-17 in the animals that were sensitized and treated with rBmTI-A compared to those in the OVA group. Studies that were performed with other serine protease inhibitors have shown reduced levels of these cytokines in a murine model of airway inflammation that was treated with other serine protease inhibitors. The serine protease inhibitors FOY, FUT and UTI reduced the concentration of IL-5, IL-6, IL-13 and IL-17 in BALF in an experimental model of chronic allergic inflammation in mice26. Others studies have reported the reduction of the IL-4, IL-5 and IL-13 concentration in the murine BALF of sensitized mice that were treated with CrataBL and AEBSF inhibitors25,27, and Ishizaki et al.40 showed that there was a reduction in IL-13 in a group of animals that was sensitized and treated with Nafamostat Mesylate40.
IL-5 is a cytokine that is essential for the growth, maturation, activation, and suppression of eosinophil apoptosis41. IL-5 has also been implicated in the induction of hyperresponsiveness42. Data have demonstrated that the inhibition of IL-5 effectively reduces exacerbation, which occurs often in severe asthma, especially in the eosinophilic pathogenesis subgroup43.
The identification of Th2/Th17 cells in allergic asthma led to the observation that different clinical phenotypes can coexist in the same patient and are related to greater severity of the disease38. Th2 cytokines (IL-4 and IL-13) induce remodelling and hyperresponsiveness in asthma44.
In some murine airway inflammation models, IL-17 controls airway hyperresponsiveness and remodelling45 and induces the resistance of bronchial epithelial cells to the effects of steroids46.
IL-10 is different from the cytokines mentioned above and is known for its anti-inflammatory role, as IL-10 is capable of inhibiting various cytokines47. Nonetheless, IL-10 is also paradoxically associated with hyperresponsiveness and IL-5 production48.
The effect of rBmTI-A on cytokine levels can be attributed to the role of trypsin-like serine proteases in the activation of the PAR-1 and PAR-2 protease-activated receptors, which appear to be involved in the production and release of these inflammatory components. According to Shigetomi et al.49, the effects of basic pancreatic trypsin (BPTI) are mediated by anti-inflammatory mechanisms through the protection of the high affinity thrombin receptor and the protease-activated receptor PAR-1. PAR-1 can be activated by trypsin, thrombin and matrix-1 metalloproteinase (MMP-1), which leads to the production of various proinflammatory cytokines and chemokines. Other studies have observed a reduction in hyperresponsiveness, eosinophilia and IL-2, IL-3, IL-4, IL-5, IL-6, IL-7, IL-13 and IL-7 in asthma models that received PAR-2 inhibitors and PAR-2 signalling blockers50.
The increase in CD4+ positive cells in the airways of the sensitized group was attenuated by treatment with the serine protease inhibitor rBmTI-A. Activated T cells, especially CD4+ T cells, are protagonists in the pathophysiology of allergic asthma, modulating the production of cytokines51.
Cytokines play an essential role in the development and regulation of asthma, which explains the importance of the effect of rBmTI-A on the inflammatory process.
This study has some limitations. For example, rBmTI-A was tested in an experimental model of chronic allergic pulmonary inflammation. Therefore, we cannot extrapolate our findings directly to humans. In addition, we did not evaluate the toxicity of the inhibitor.
The results obtained in this study showed that the rBmTI-A serine protease inhibitor was effective in attenuating the changes in lung mechanics, inflammation, and remodelling of the airways in this animal model of chronic allergic pulmonary inflammation. Although more studies need to be performed to elucidate the mechanisms responsible for these changes, this inhibitor appears to be a possible pharmacological tool for the treatment of asthma.
Conclusion
In this experimental model of chronic allergic pulmonary inflammation, we can conclude that the rBmTI-A serine protease inhibitor was effective in reducing the following responses:
Proteolytic activity of trypsin-like proteases in the pulmonary homogenate;
Maximum response of elastance and resistance of the respiratory system;
The number of eosinophils in the airways;
The number of polymorphonuclear cells in the bronchoalveolar lavage fluid;
The concentration of the IL-5, IL-10, IL-13, IL-17A cytokines in the bronchoalveolar lavage fluid;
The expression of IL-5, IL-10, IL-13, IL-17, CD4+, MMP-9 and TIMP-1 in the airways; and
The fraction of collagen and elastic fibres of the airways.
Therefore, our results showed that the rBmTI-A serine protease inhibitor was effective in reducing methacholine hyperresponsiveness, airway inflammation and remodelling in this experimental model of chronic allergic pulmonary inflammation. Although more studies need to be performed, this inhibitor may contribute as a potential therapeutic tool for the treatment of asthma.
Methods
The animals (male Balb/c mice) used in this study initially weighed 25–30 g and were approximately 6–8 weeks old. All the mice received humane care in compliance with the “Guide for the Care and Use of Laboratory Animals” (NIH publication 85–23, revised 1985), and all the experiments described in this study were approved by the institutional review board of the University of Sao Paulo (Sao Paulo, Brazil).
Experimental groups and study design
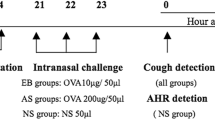
The animals were randomly divided into the following 4 groups of 8 animals each, according to the protocol (Fig. 10):
- (A)
SAL: animals that received saline solution (0.9% NaCl) by inhalation and nasal instillation;
- (B)
SAL + rBmTI-A: animals that received saline solution (0.9% NaCl) by inhalation with and rBmTI-A by nasal instillation;
- (C)
OVA: animals that received ovalbumin solution by inhalation; and
- (D)
OVA + rBmTI-A: animals that received ovalbumin solution by inhalation and rBmTI-Aby nasal instillation.
Timeline of the experimental protocol. On the first and fourteenth day of the protocol, the animals received intraperitoneal injections with ovalbumin or saline solution. On days 22, 24, 26 and 28, the animals received ovalbumin or saline by aerosol inhalation. On days 22 and 28, 2 hours after inhalation, the animals received an intranasal instillation with saline (SAL and OVA) or with rBmTI-A (SAL + rBmTI-A and OVA + rBmTI-A). On the twenty-ninth day, the animals were anaesthetized, tracheostomized and the evaluation of the pulmonary mechanics and BALF were performed; the lungs were removed to perform the other analyses.
Experimental model of chronic allergic pulmonary inflammation
Mice received intraperitoneal injection (i.p.) with a solution of 50 μg ovalbumin grade III (Sigma - Aldrich) and 6 mg of aluminium hydroxide (Pepsamar ®, Sanofi - Synthelabo SA, Rio de Janeiro, Brazil) in a total volume of 0.2 ml on days 0 and 14. On days 22, 24, 26 and 28, the animals were placed in an acrylic display box (30 × 15 × 20 cm) coupled to an ultrasonic nebulizer (Pulmoclear II, Soniclear, Sao Paulo, Brazil) and underwent an aerosol inhalation of OVA diluted in NaCl 0.9% (saline) at a concentration of 10 mg/mL (1%) for 30 minutes. The control groups received saline solution (NaCl 0.9%) and aluminium hydroxide (6 mg) i.p., and on the days of the inhalation challenges control animals were exposed to aerosol saline 0.9%, for 30 minutes.
Inhibitor expression and purification
The cloning of the recombinant inhibitor, rBmTI-A, used in this design was performed with an Rhipicephalus Boophilus microplus tick intestine cDNA library by the constructing of the recombinant vector rBmTI-A/pPIC9K, as described by Sasaki and Tanaka (2008)52.
The rBmTI-A purification was carried out using affinity chromatography with a trypsin-Sepharose column that had been previously equilibrated with 0.05 M Tris-HCl buffer, pH 8.0. Subsequently, 0.05 M Tris-HCl buffer containing 0.2 M NaCl, pH 8.0, was passed through the column until the collected material reached an absorbance reading of 0.05 at 280 nm with a spectrophotometer. The material was then eluted using a 0.5 M KCl/HCl solution, pH 2.0. The eluted fractions were immediately neutralized with 1 M Tris–HCl buffer, pH 8.0. The samples with high absorbance were pooled, and their concentration and inhibitory constants (Ki) were determined. rBmTI-A was further purified by gel filtration chromatography with a Sephadex 75 column (ÄKTA purifier System, GE Healthcare), and equilibration and elution were performed with PBS buffer52.
Treatment protocol
Mice were treated by intranasal instillation 2 hours after the inhalation at the first and last inhalation (days 22 and 28). Animals received a nasal instillation of 35.54 pmol of the recombinant inhibitor (rBmTI-A) in 50 μl of saline solution (0.9% NaCl)12, following the protocol shown in Fig. 10. The control animals received 50 μl of saline solution (0.9% NaCl) by nasal instillation.
Respiratory mechanics evaluation
Thirty days after the initiation of the sensitization protocol (twenty-four hours after the last inhalation challenge), the animals were anaesthetized with thiopental (80 mg/kg, i.p.) and were tracheostomized. The mice were mechanically ventilated in an acrylic plethysmograph (120 cycles/min, 10 mL/kg) connected to a Harvard 683 small animal ventilator (Harvard Apparatus, Massachusetts, USA). Tracheal pressure signals and lung volume were measured with differential pressure transducers (Honeywell 163PC01D36, Freepot, IL) and converted by an analogue digital board (DT01EZ, Data Translation, Marlboro, MA). The values of elastance (Ers) and resistance (Rrs) of the respiratory system were calculated using the equation of motion of the respiratory system, Ptr (t) = Rrs. V′(t) + Ers. V (t) where t represents time, Ptr represents tracheal pressure, V′ represents airflow and V represents lung volume. Basal and maximal Rrs and Ers values were calculated after methacholine aerosol administration (3, 30 and 300 mg/mL for 1 minute - Dose-Response Curve).
Bronchoalveolar lavage fluid
Bronchoalveolar lavage fluid (BALF) collection was performed by washing the lungs with three 0.5 mL PBS injections through the tracheal cannula. The recovered volume was approximately 90% of the volume injected. This procedure was repeated three times.
Total and differential balf cell counts
The collected BALF was centrifuged at 800 revolutions per minute (rpm) for ten minutes at 4 °C. The cell pellet was resuspended in 0.3 ml of 0.9% sterile saline solution. From this solution, 20 μl was removed for total cell analysis using a Neubauer haemocytometer chamber and optical microscope at 1000x magnification. The differential cell counts were performed using 100 μl of the supernatant, which was centrifuged (450 rpm for 10 minutes) to generate the slides. The slides were stained with the Diff-Quick reagent. The differential cell count was determined with 300 cells/slide with an optical microscope.
Determination of the cytokine concentration by flow cytometry (cytometric bead array - CBA)
The cytokine levels in the BALF was measured using the CBA method with CBA Mouse Enhanced Sensitivity Flex Set (BD Pharmingen) kits specific for the cytokines IL-4, IL-5, IL-10, IL-13, IL-17A and INF-γ according to the manufacturer’s instructions. Samples were incubated with capture microspheres with different fluorescence intensities that were coated with a capture antibody specific for each cytokine. Thereafter, a second incubation was performed with high sensitivity detection antibodies labelled with phycoerythrin (PE), which emits a fluorescent signal that is proportional to the amount of protein. After the incubations, 1 mL of the wash solution was added, and the material was centrifuged for 10 minutes at 1100 rpm. The supernatant was discarded, and in 300 μL of the wash buffer, the samples were resuspended for the analysis of the complexes with a flow cytometer (LSRFortessa - BD Biosciences). The results were analysed with the program BD FCAPArray 3.0 (BD Biosciences) and are displayed in a graphic format.
Morphometric analysis
The left lung was fixed with 10% formalin and, after twenty-four hours, was transferred to 70% ethanol. After fixation, the lung was cut on its largest axis, was paraffin embedded and 4 μm thick histological sections were cut and stained with LUNA (for eosinophil analysis), picrosirius (for the analysis of the collagen fibres), Weigert’s resorcin-fuchsin (for the analysis of elastic fibres); the sections were also used for immunohistochemical evaluation. Morphometric analysis was performed using an optical microscope (CH30, Olympus, Japan), and approximately three fields of three to five airways of each animal were randomly selected and were evaluated36,53,54,55.
Measurement of eosinophil density
To evaluate the eosinophil density, the LUNA technique was used, which identifies eosinophil granules. The point counting technique56 was used with a reticulum of a 100 points/50 intercepts grid, which was attached to the microscope eyepiece and superimposed on the tissue (104 mm2 total area). The number of positive cells in the airway wall was calculated as the number of positive cells in each field divided by the number of points coinciding with the area of tissue present in the same field of the reticulum (104 mm2).
Volume Fraction of the collagen and elastic fibres
Picrosirius staining was used to quantify collagen fibres, and resorcin-fuchsin staining was used to identify the elastic fibres in the airways. The measurement of the optical density was used for the morphometric analysis of the collagen and elastic fibres in the airway wall. The images were obtained using a Leica DM4000B microscope (Leica Microsystems, Wetzlar, Germany) and a digital camera Leica DFC420 (Leica Microsystems, Wetzlar, Germany) that were connected to a computer using the Leica Qwin software (Leica Microsystems, Cambridge, England); the images were acquired at 400× magnification. The images were processed by the ImageProPlus software (Media Cybernetics, Bethesda, MD), which allows the user to set a threshold of colour tones that represents the positive areas, in order to quantify a predetermined area. Two binary-colour thresholds were defined: one for the fibre calculation (according to staining) and one for the airways. Thus, the proportion of the collagen or elastic fibres per airway area was quantified. The results are expressed as the percentage of the positive area (volume fraction).
Immunohistochemical evaluation
For the immunohistochemical evaluation, the following antibodies were used: anti-IL-4 (Santa Cruz Biotechnology, California, USA; 1:600), anti-IL-5 (Santa Cruz Biotechnology, California, USA; 1:100), anti-IL-10 (Santa Cruz Biotechnology, California, USA; 1:500), anti-IL-13 (Santa Cruz Biotechnology, California, USA; 1:700), anti-IL-17 (Santa Cruz Biotechnology, California, USA; 1:800), anti-CD4+ (Santa Cruz Biotechnology, California, USA; 1:25), anti-CD8+ (Santa Cruz Biotechnology, California, USA; 1:50), anti-MMP-9 (Santa Cruz Biotechnology, California, USA; 1:500) and anti-TIMP-1 (Santa Cruz Biotechnology, California, USA; 1:100).Immunohistochemistry was performed with the following sequence of procedures: antigenic recovery, endogenous peroxidase blockade and nonspecific binding blockade, incubation with the primary antibody, incubation with the secondary antibody and complex, counterstaining and assembly of the blades. The count was determined as described above for the evaluation of eosinophil density.
Evaluation of the pulmonary homogenate proteolytic activity
The right lung was homogenized in PBS (600 μL) using metal beads, as recommended by the manufacturer (Powerlyzer, MoBio Laboratories Inc., USA).
Pulmonary homogenate was used in an enzymatic assay to analyse the proteolytic activity of MMP-1, MMP-9 and trypsin-like in lung tissue according to the following protocol. For the analysis of MMP-1 and MMP-9 activity, an incubation of 10 μL of the sample (pulmonary homogenate) with 2 μL of the fluorogenic substrates for MMP-1/MMP-9 (MMP-1/MMP-9 substrate – Calbiochem, San Diego, CA) and 88 μL of buffer (0.1 M Tris-HCl, 0.15 M NaCl and 0.1 M Triton X-100) at pH 8.0 was performed. For the analysis of trypsin-like proteolytic activity, 10 μL of sample (pulmonary homogenate), 4 μL of the fluorogenic trypsin-like substrate (Z-Phe-Arg-7-amido-4-methylcoumarin, Hydrochloride-Calbiochem) and 86 μL of buffer (0.1 M Tris-HCl, 0.15 M NaCl and 0.1 M Triton X-100) at pH 8.0 was performed. After 20 minutes of incubation at 37 °C, readings were taken for 30 minutes (at 5-minute intervals) with a spectrophotometer (Biotek - Synergy HT) using the following parameters: Sensitivity 65; “Optic exposition - Top”; Wavelength 380/20 (excitation) and 460/40 (emission).
Change history
13 November 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
GINA. Global Strategy for Asthma Management and Prevention. Revised 2017. http://www.ginaasthma.com (accessed 01 December 2017).
Lambrecht, B. N. & Hammad, H. The immunology of asthma. Nature Immunology. 16, 45–56 (2015).
Bousquet, J. et al. Asthma - From bronchoconstriction to airways inflammation and remodeling. American Journal of Respiratory and Critical Care Medicine 161, 1720–1745 (2000).
Vignola, A. M. et al. Increased levels of elastase and alpha(1)-antitrypsin in sputum of asthmatic patients. American Journal of Respiratory and Critical Care Medicine 157, 505–511 (1998).
Nishioka, T. et al. Alpha-1-antitrypsin and complement component C7 are involved in asthma exacerbation. Proteomics Clinical Applications 2, 46–54 (2008).
Pabinger, I. & Schneider, B. Thrombotic risk in hereditary antithrombin III, protein C, or protein S deficiency - A cooperative, retrospective study. Arteriosclerosis Thrombosis and Vascular Biology 16, 742–748 (1996).
Martins-Olivera, B. T. et al. The Plant-Derived Bauhinia bauhinioides Kallikrein Proteinase Inhibitor (rBbKI) Attenuates Elastase-Induced Emphysema in Mice. Mediators Inflamm. 2016, 5346574 (2016).
Almeida-Reis, R. et al. Plant Proteinase Inhibitor BbCI Modulates Lung Inflammatory Responses and Mechanic and Remodeling Alterations Induced by Elastase in Mice. Biomed Res Int 2017, 8287125 (2017).
Theodoro-Junior, O. A. et al. A Plant Proteinase Inhibitor from Enterolobium contortisiliquum Attenuates Pulmonary Mechanics, Inflammation and Remodeling Induced by Elastase in Mice. Int J Mol Sci. 18 (2017).
Tanaka, A. S. et al. A double headed serine proteinase inhibitor - human plasma kallikrein and elastase inhibitor - from Boophilus microplus larvae. Immunopharmacology. 45, 171–177 (1999).
Sasaki, S. D. et al. Boophilus microplus tick larvae, a rich source of Kunitz type serine proteinase inhibitors. Biochimie. 86, 643–649 (2004).
Lourenco, J. D. et al. A Treatment with a Protease Inhibitor Recombinant from the Cattle Tick (Rhipicephalus Boophilus microplus) Ameliorates Emphysema in Mice. Plos One. 9, 9 (2014).
Papaioannou, A. I. et al. Control of asthma in real life: still a valuable goal? Eur Respir Rev 24, 361–9 (2015).
Royce, S. G. et al. The regulation of fibrosis in airway remodeling in asthma. Molecular and Cellular Endocrinology. 351, 167–175 (2012).
Vieira, R. P. et al. Aerobic conditioning and allergic pulmonary inflammation in mice. II. Effects on lung vascular and parenchymal inflammation and remodeling. American Journal of Physiology-Lung Cellular and Molecular Physiology. 295, L670–L679 (2008).
Toledo, A. C. et al. Flavonone treatment reverses airway inflammation and remodelling in an asthma murine model. British Journal of Pharmacology. 168, 1736–1749 (2013).
Fernandez-Rodriguez, S. et al. Establishing the phenotype in novel acute and chronic murine models of allergic asthma. International Immunopharmacology. 8, 756–763 (2008).
Gueders, M. M. et al. Mouse models of asthma: a comparison between C57BL/6 and BALB/c strains regarding bronchial responsiveness, inflammation, and cytokine production. Inflammation Research. 58, 845–854 (2009).
Monteseirin, J. et al. Plasma kallikrein amidolytic activity in bronchial asthma. Allergol Immunopathol (Madr). 20, 211–4 (1992).
Chambers, L. S. et al. Functional effects of protease-activated receptor-2 stimulation on human airway smooth muscle. Am J Physiol Lung Cell Mol Physiol. 281, L1369–78 (2001).
Camelier, A. A. et al. Deficiência de alfa-1 antitripsina: diagnóstico e tratamento. Jornal Brasileiro de Pneumologia. 34, 514–527 (2008).
Liang, G. & Bowen, J. P. Development of Trypsin-Like Serine Protease Inhibitors as Therapeutic Agents: Opportunities, Challenges, and their Unique Structure-Based Rationales. Curr Top Med Chem. 16, 1506–29 (2016).
Sasaki, S. D. & Tanaka, A. S. rBmTI-6, a Kunitz-BPTI domain protease inhibitor from the tick Boophilus microplus, its cloning, expression and biochemical characterization. Vet Parasitol. 155, 133–41 (2008).
Arantes-Costa, F. M. et al. Effects of ventilation, humidity and temperature on airway responsiveness to methacholine in rats. European Respiratory Journal. 19, 1008–1014 (2002).
Dos Santos, A. S. A. et al. Effect Of Proteinase Inhibitor Of Plant Origin Cratabl In An Experimental Model Of Chronic Allergic Pulmonary Inflammation. American Journal of Respiratory and Critical Care Medicine. 189 (2014).
Lin, C.-C. et al. The Effect of Serine Protease Inhibitors on Airway Inflammation in a Chronic Allergen-Induced Asthma Mouse Model. Mediators of Inflammation. (2014).
Saw, S. & Arora, N. Protease Inhibitor Reduces Airway Response and Underlying Inflammation in Cockroach Allergen-Induced Murine Model. Inflammation. 38, 672–682 (2015).
Flood-Page, P. et al. Anti-IL-5 treatment reduces deposition of ECM proteins in the bronchial subepithelial basement membrane of mild atopic asthmatics. Journal of Clinical Investigation 112, 1029–1036 (2003).
Mattos, W. et al. Matrix metalloproteinase-9 expression in asthma - Effect of asthma severity, allergen challenge, and inhaled corticosteroids. Chest. 122, 1543–1552 (2002).
Lourenco, J. D. et al. The tick-derived rBmTI-A protease inhibitor attenuates the histological and functional changes induced by cigarette smoke exposure. Histol Histopathol. 11927 (2017).
Atkinson, J. J. & Senior, R. M. Matrix metalloproteinase-9 in lung remodeling. American Journal of Respiratory Cell and Molecular Biology 28, 12–24 (2003).
Noel, A. et al. Membrane associated proteases and their inhibitors in tumour angiogenesis. J Clin Pathol 57, 577–84 (2004).
Vliagoftis, A. et al. Proteinase-activated receptor-2-mediated matrix metalloproteinase-9 release from airway epithelial cells. Journal of Allergy and Clinical Immunology 106, 537–545 (2000).
Gueders, M. M. et al. Matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs in the respiratory tract: potential implications in asthma and other lung diseases. Eur J Pharmacol 533, 133–44 (2006).
Righetti, R. F. et al. Effects of Rho-kinase inhibition in lung tissue with chronic inflammation. Respir Physiol Neurobiol 192, 134–46 (2014).
Leick-Maldonado, E. A. et al. Comparison of glucocorticoid and cysteinyl leukotriene receptor antagonist treatments in an experimental model of chronic airway inflammation in guinea-pigs. Clinical and Experimental Allergy 34, 145–152 (2004).
Prado, C. M. et al. Effects of nitric oxide synthases in chronic allergic airway inflammation and remodeling. American Journal of Respiratory Cell and Molecular Biology 35, 457–465 (2006).
Brandenberger, C. et al. Enhanced allergic airway disease in old mice is associated with a Th17 response. Clinical and Experimental Allergy 44, 1282–1292 (2014).
Walters, E. H. et al. Bronchoalveolar lavage in asthma research. Respirology. 1, 233–45 (1996).
Ishizaki, M. et al. Nafamostat Mesilate, a Potent Serine Protease Inhibitor, Inhibits Airway Eosinophilic Inflammation and Airway Epithelial Remodeling in a Murine Model of Allergic Asthma. Journal of Pharmacological Sciences 108, 355–363 (2008).
Menzies-Gow, A. et al. Anti-IL-5 (mepolizumab) therapy induces bone marrow eosinophil maturational arrest and decreases eosinophil progenitors in the bronchial mucosa of atopic asthmatics. Journal of Allergy and Clinical Immunology 111, 714–719 (2003).
Leckie, M. J. et al. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 356, 2144–8 (2000).
Schuijs, M. J. et al. Cytokine targets in airway inflammation. Current Opinion in Pharmacology 13, 351–361 (2013).
Hamid, Q. & Tulic, M., Immunobiology of Asthma, in Annual Review of Physiology. Annual Reviews: Palo Alto. 489–507 (2009).
Bellini, A. et al. Interleukin (IL)-4, IL-13, and IL-17A differentially affect the profibrotic and proinflammatory functions of fibrocytes from asthmatic patients. Mucosal Immunology 5, 140–149 (2012).
Zijlstra, G. J. et al. Interleukin-17A induces glucocorticoid insensitivity in human bronchial epithelial cells. European Respiratory Journal 39, 439–445 (2012).
Malefyt, R. D. et al. interleukin-10 (IL-10) and viral-IL-10 strongly reduce antigen-specific human t-cell proliferation by diminishing the antigen-presenting capacity of monocytes via down-regulation of class-ii major histocompatibility complex expression. Journal of Experimental Medicine 174, 915–924 (1991).
Kita, H. et al. Cytokine production at the site of disease in chronic eosinophilic pneumonitis. American Journal of Respiratory and Critical Care Medicine 153, 1437–1441 (1996).
Shigetomi, H. et al. Anti-inflammatory actions of serine protease inhibitors containing the Kunitz domain. Inflammation Research. 59, 679–687 (2010).
Asaduzzaman, M. et al. Functional inhibition of PAR2 alleviates allergen-induced airway hyperresponsiveness and inflammation. Clin Exp Allergy 45, 1844–55 (2015).
Bochner, B. S. et al. Immunological aspects of allergic asthma. Annu Rev Immunol 12, 295–335 (1994).
Sasaki, S. D. & Tanaka, A. S. rBmTI-6, a Kunitz-BPTI domain protease inhibitor from the tick Boophilus microplus, its cloning, expression and biochemical characterization. Veterinary Parasitology. 155, 133–141 (2008).
Tiberio, I. et al. Effects of neurokinin depletion on airway inflammation induced by chronic antigen exposure. American Journal of Respiratory and Critical Care Medicine 155, 1739–1747 (1997).
Weibel, E. R. The challenge of measuring lung structure. On the “Standards for the Quantitative Assessment of Lung Structure”. Nihon Kokyuki Gakkai Zasshi 48, 637–43 (2010).
Righetti, L. et al. Group detection of DON and its modified forms by an ELISA kit. Food Addit Contam Part A Chem Anal Control Expo Risk Assess 34, 248–254 (2017).
Weibel, E. R., Morphometry of the human lung, New York: Academic Press (1963).
Acknowledgements
This study was supported by the following Brazilian Scientific Agencies: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), and Faculdade de Medicina da Universidade de São Paulo - Brazil (LIM-20-HC-FMUSP). The authors declare no competing financial interests.
Author information
Authors and Affiliations
Contributions
A.F. designed and performed the majority of the experiments and the morphometric analysis, performed the statistical analysis and drafted the manuscript. R.A. assisted in performing the experiments. S.S. and A.D. expressed and purified the inhibitor. B.S.-R. assisted in the BALF evaluation, and F.L. and F.M.-C. assisted in the mechanics evaluation. I.T. helped with the statistical analysis. M.M. participated in the design and discussion of the study. E.L. supervised the study, participated in its design and in the interpretation of the results as well as in the writing of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Florencio, A.C., de Almeida, R.S., Arantes-Costa, F.M. et al. Effects of the serine protease inhibitor rBmTI-A in an experimental mouse model of chronic allergic pulmonary inflammation. Sci Rep 9, 12624 (2019). https://doi.org/10.1038/s41598-019-48577-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-48577-4
This article is cited by
-
Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2
Signal Transduction and Targeted Therapy (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.