Abstract
Polycystic ovarian syndrome (PCOS) is a multispectral disorder requiring lifelong management. Its pathophysiology is still being explored which makes its treatment options restrained. Present study explores impact of oral contraceptive mode of treatment on metabolic, hormonal, inflammation and coagulation profile of PCOS women. 50 subjects diagnosed with Rotterdam criteria receiving no drug treatment served as controls whereas 50 subjects receiving only OCPs (Ethinyl estradiol 0.03 mg, Levonorgestrel 0.15 mg) as a mode of treatment at least for six-months served as cases. Ferriman-Gallwey score and hormonal profile improved on OCP treatment. However, parameters like weight, Body mass index, waist-hip ratio, Oral glucose tolerance test, lipid profile, insulin, HOMA-IR, adiponectin, interleukin1β, visfatin, resistin, tissue factor, PT and APTT showed considerable derangements in OCP group. All above parameters are associated with the risk of diabetes mellitus, dyslipidemia, coronary vascular disease, cancers, hypercoagulable state, venous thromboembolism and thrombotic events. Long-term use of OCPs needs to be considered carefully for PCOS patients who are already burdened with associated risk factors. This study was conducted in a region where women do not have much access to high-end screening and diagnostic facilities that further exacerbates their clinical outcomes. Large scale, long-term studies need to be designed to further evaluate safety use of OCPs in PCOS women.
Similar content being viewed by others
Introduction
Polycystic ovarian syndrome (PCOS) is a multifactorial disorder involving both reproductive as well as endocrine systems. Based on current Rotterdam criteria the prevalence of PCOS is between 5–10% in reproductive age women1. Metabolic issues like inflammation, increased coagulability, visceral obesity, insulin resistance and androgen excess are considered as key features in PCOS2,3,4. Insulin resistance and increased adiposity leads to elevated production of adipocytokines notably adiponectin, visfatin, leptin, resistin, tissue necrosis factor (TNF-α), interleukin-6 (IL-6) and interleukin-1 (IL-1)5. These adipocytokines in turn cause the activation of macrophages that leads to production of various proinflammatory mediators6,7. Insulin resistance promotes hyperandrogenism in this syndrome8 and the interaction of these two conditions with the hemostatic-fibrinolytic systems is of importance and not fully evaluated with reports suggesting that the hyperinsulinemia may alter fibrinolysis9,10. Cardiovascular risk markers and atherosclerosis cluster in women with PCOS11,12,13,14,15. As a consequence of their hyperandrogenism and insulin-resistant metabolic milieu they are predisposed to prothrombotic state and endothelial dysfunctions16,17,18,19,20,21.
Oral contraceptive pills (OCPs) (estrogen + progestin) are considered as the first-line therapy for PCOS. But there is conflicting data regarding effects of this mode of treatment on metabolism of carbohydrates, lipids, also on insulin, coagulation and inflammation profile in PCOS subjects.
In one of the earlier reports the effect of drug treatment using sample number as 30 OCP users and 30 metformin users indicated OCP has worsening effect on metabolism22. In yet another study where 30 women taking OCPs for varying time period were assessed for fibrinogen and platelet count showed derangements in these values23.
In present study, our aim was to evaluate PCOS subjects taking OCP treatment versus drug naive PCOS subjects emphasizing evaluation of their metabolic, hormonal, inflammation and coagulation profiles. For this study design we have particularly focused on parameters viz. adiponectin, IL-1β, visfatin, resistin, tissue factor, prothombin time (PT) and activated partial thromboplastin time (APTT) whose brief description is given as follows:-
Adiponectin
Adiponectin is a chemokine secreted from visceral fat cells and is the only adipo-cytokine that gets down regulated in obesity24. It possesses anti-inflammatory, anti-atherogenic and insulin-sensitizing actions25,26. Glucose-lowering and anti-inflammatory effects of adiponectin are mediated by the activation and up regulation of the adiponectin receptors27.
Interleukin 1β
Interleukin-1beta (IL-1β) is an effective pro-inflammatory mediator produced by activated macrophages that plays an important role in defense responses to injury and infection28. IL-1β is involved in lipid metabolism by regulating insulin levels and has lipase activity under physiological conditions29. Further IL-1β is implicated in various diseases like atherosclerosis, chronic heart failure and type 2 diabetes mellitus (T2DM), which are considered as associated risk factors of PCOS30.
Visfatin
Visfatin is an adipocytokine secreted from adipose tissues, hepatocytes, lymphocytes, bone marrow, fetal membranes, liver, muscles and trophoblasts31. Visfatin possesses an insulin mimetic effect and binds to insulin receptor, therefore, stimulating glucose uptake in muscle cells and adipocytes while suppressing glucose release from liver cells32,33. It also exhibits modulated immune functions and proinflammatory characteristics34.
Resistin
Resistin, an adipokine stimulates SOCS-3 (Suppressor of cytokine-3), which causes inhibition of insulin pathway in the tissues. Moreover, it prevents the phosphorylation of AMPK pathway that is associated with fatty acid oxidation, prevention of cholesterol synthesis and insulin secretion by beta cells of pancreas. Thus elevated levels of resistin down-regulates β-oxidation of fatty acids and glycogen metabolism resulting in dyslipidemia and T2DM consequently35,36,37. Resistin being involved in the processes like inflammation and autoimmune diseases38 has been linked to the development of other disease processes like insulin resistance (IR), T2DM, Coronary vascular disease (CVD), atherosclerosis as well which are again considered as risk factors for PCOS39.
Tissue factor
Tissue factor (a trans-membrane lipoprotein) initiates extrinsic pathway which results in the generation of active serine protease i.e., coagulant mediators: FVIIa, FXa & FIIa and thus stimulates fibrin formation. Tissue factor has contribution in producing both hypercoagulability and inflammation that in turn augment each other40. This viscous cycle of coagulation-inflammation-thrombosis emerges in the form of various pathologies like diabetes mellitus, cardiovascular diseases, obesity and disseminated intravascular coagulation (DIC) etc.41,42.
PT and APTT
PT gives an indication of the concentration of prothrombin in the blood. Thus PT measures the time taken for fibrin formation or coagulation time through extrinsic pathway. APTT or partial thrombin time (PTT) is a measurement of the intrinsic coagulation pathway and the common pathway. APTT/PTT together measures the time taken for fibrin formation through the intrinsic pathway. PT and APTT are part of lab coagulation screen tests and these are direct reflection of circulating activated coagulation factors present in plasma. One of the indications of hypercoagulable state is decreased APTT values that in turn predict increased risk for future adverse thrombotic and cardiovascular events43,44,45,46.
Results
Basic clinical characteristics of PCOS controls Vs OCP treated cases
PCOS subjects who received no drug treatment served as drug naive PCOS controls (n = 50) while as PCOS subjects who received only OCPs as a mode of treatment served as cases (n = 50). Following parameters like Anthropometry (BMI, Weight, waist-hip ratio), Lipid profile (Cholesterol, TG), OGTT (Blood glucose fasting, Blood glucose 1 hr, Blood glucose 2 hr) were found deranged in cases as compared to controls (Table 1). Moreover, Hormonal profile i.e., LH, FSH and Testosterone assessed in controls as well as in cases improved in cases i.e., OCP treated group compared to PCOS controls. Insulin profile (HOMA-IR, QUICKI) signified increase in insulin resistance in OCP treated group (Table 2).
Evaluation of inflammation profile of PCOS controls Vs OCP treated PCOS cases
The inflammation profile indicates worsening of inflammatory markers in cases compared to controls as depicted: Adiponectin levels were found decreased in cases compared to controls. Statistically significant and negative Pearson’s correlation of Adiponectin was found with weight (r = −0.731, p < 0.0001), waist (r = −0.656, p < 0.0001), hip (r = −0.631, p = 0.0002), waist-hip ratio (r = −0.443, p = 0.014), BMI (r = −0.634, p = 0.0002) and cholesterol (r = −0.751, p < 0.0001) (Tables 3 and 4). Multiple regression analysis of Adiponectin shows association with cholesterol and LH-FSH ratio (R square = 0.646, Adjusted R square = 0.620, p < 0.001). Interleukin 1β levels were found elevated in cases compared to controls. Statistically significant and positive Pearson’s correlation of Interleukin 1β was found with weight (r = 0.871, p < 0.0001), waist (r = 0.774, p < 0.0001), hip (r = 0.709, p < 0.0001), waist-hip ratio (r = 0.580, p < 0.008), BMI (r = 0.826, p < 0.0001), and cholesterol (r = 0.852, p < 0.0001) (Tables 3 and 4). Multiple regression analysis of Interleukin 1β shows association with age (R square = 0.142, Adjusted R square = 0.111, p = 0.040). Visfatin levels were found elevated in cases compared to controls. Statistically significant Pearson’s correlation of Visfatin was observed with various parameters: weight (r = 0.380, p = 0.015), height (r = −0.328, p = 0.038), waist (r = 0.470, p = 0.002), hip (r = 0.317, p = 0.046), BMI (r = 0.562, p = 0.002), cholesterol (r = 0.391, p = 0.013), LH (r = −0.311, p = 0.051) and FSH (r = −0.304, p = 0.056) (Tables 3 and 4). Multiple regression analysis of visfatin shows association with BMI, TG and LH-FSH ratio (R square = 0.652, Adjusted R square = 0.612, p < 0.001). Resistin levels were found elevated in cases compared to controls. We did not find any statistically significant Pearson’s correlation of Resistin with the given parameters except with BMI (r = 0.334, p = 0.035) (Tables 3 and 4). Multiple regression analysis of Resistin shows association with BMI and SGOT (R square = 0.342, Adjusted R square = 0.293, p = 0.004).
Evaluation of coagulation profile of PCOS controls Vs OCP treated PCOS cases
The coagulation markers assessed in our study were also changed in OCP treated PCOS group in comparison to drug naive group as depicted: Tissue factor levels were increased in cases compared to controls. Significant positive Pearson’s correlation of Tissue Factor was found with various anthropometric parameters like BMI (r = 0.34, p = 0.01), waist-hip ratio (r = 0.34, p = 0.02), FG-score (r = 0.29, p = 0.04) and LH-FSH ratio (r = 0.42, p = 0.003) (Tables 3 and 4). Multiple regression analysis of Tissue Factor shows association with BMI, LH-FSH ratio (R Square = 0.267, Adjusted R Square = 0.236, p = 0.001) and QUICKI (R Square = 0.160, Adjusted R Square = 0.130, p = 0.029). PT was found decreased in cases compared to controls and its multiple regression analysis shows association with IR only (R Square = 0.137, Adjusted R Square = 0.107, p = 0.044) (Tables 3 and 4). APTT was found decreased in cases compared to controls but has not shown correlation with any of the PCOS diagnostic parameters (Tables 3 and 4).
Discussion
Numerous studies are available which are in favor of considering OCPs as first mode of treatment in PCOS women exhibiting that treatment with OCPs results in decreased free androgens reducing new hair growth and the growth of terminal hair. It also helps to reduce inflammatory acne count by 30–60% with improvement in 50–90% of patients47. Estrogen component of OCPs have shown to suppress LH secretion, thus reducing the ovarian androgen production, and also increases sex hormone binding globulin (SHBG) that helps reduce free testosterone. Our results are in agreement with these reports as the present study also showed significant decrease in LH, testosterone and FG-score in OCP treated PCOS women as compared to drug naive PCOS women. There is controversial data available in the literature regarding the impact of OCP use on glucose tolerance and insulin sensitivity in PCOS women. Some reports suggest no change in glucose tolerance and insulin sensitivity while others are suggestive of adverse impact of the drug on these parameters48,49,50,51,52,53,54,55. In the present study, we observed the worsening of biochemical parameters like OGTT, lipid profile, fasting insulin, HOMA-IR and QUICKI in OCP treated PCOS women as compared to drug naive PCOS women. This data is suggestive of negative metabolic effects of oral contraceptives in PCOS women as has been reported earlier49,56. Our data has also shown statistically significant increase in total cholesterol but insignificant increase in TG in OCP treated PCOS women when compared to drug naive PCOS women. Metabolic disruptions like above for OGTT, lipid and insulin profiles can increase the long-term risk of various metabolic diseases such as T2DM, IR and CVD. Further in our study there was significant increase in waist-hip circumferences and BMI in OCP users as compared to non-users implying obesity with the use of OCPs.
We evaluated various anti and pro-inflammatory cytokines like adiponectin, interleukin 1β, visfatin and resistin in PCOS women and found their levels altered with the use of OCPs. We observed a significant decrease in adiponectin levels in OCP treated PCOS women as compared to drug naive PCOS women. Earlier reports suggest reduced plasma levels of adiponectin are associated with diabetes, obesity, dyslipidemia, hypertension and CVD57,58,59,60. The results from the present study depict hypoadiponectinaemia in OCP users. Interleukin 1β levels in OCP treated PCOS women were raised as compared to drug naive PCOS women. Increased secretion of IL-1β has been found linked with various autoimmune and auto-inflammatory diseases, also with metabolic deregulations associated with T2DM and impaired beta cell function61,62,63.
Visfatin and resistin in OCP treated PCOS women were both raised as compared to drug naive PCOS women. The circulating levels of visfatin and resistin are found increased in obesity like conditions and their decreased levels are observed in patients using anti-diabetic drugs34. Visfatin has been found associated with different types of cancers as it plays an important role in normal cell growth and apoptosis64. A link between visfatin induced inflammation and associated malignancies has been reported elsewhere65. Visfatin is known as a good marker for endometrial cancer prognosis66. Moreover, visfatin levels are raised in various metabolic disorders like obesity, insulin resistance and T2DM, which are well known risk factors for other type of cancers67.
Hyperinsulinemia - a key feature in PCOS causes impairment in fibrinolysis resulting in hypofibrinolysis in PCOS women16,68,69. Increased fibrinogen contributes to CVD by increasing fibrin formation, plasma viscosity and platelet aggregation70. Among OCP users we found significant increase in tissues factor values and statistically significant decrease in PT and APTT values compared to drug naive PCOS women. An earlier study by Zakai NA et al., observed that even a mild reduction of APTT could increase the risk of thrombotic events in larger population studies71. Hyperandrogenism is another key player of PCOS that along with insulin resistance affects the hemolytic-fibrinolytic system in PCOS women. Although some studies have reported that hyperandrogenism affects coagulation factors and plasma fibrinolytic activity but this aspect needs to be further explored for better understanding. Correlation analysis of inflammatory and coagulatory profile with PCOS diagnostic parameters in the present study using Pearson’s correlation tool showed a general trend of strong association with obesity associated conditions like weight gain, waist, hip, waist-hip ratio, BMI and cholesterol in OCP treated PCOS women. Hence, weight gain is detected as one of the side effects of oral contraceptive treatment that is undesired and can predispose the users to various obesity associated risk conditions.
The present study clearly affirms that on one side the OCP use improves hyperandrogenism and regulates menstrual cyclicity but the other arm i.e., hyperinsulinemia and obesity induced metabolic changes can lead to a mirage of inflammation and coagulation changes which puts the OCP treated PCOS women at risk for various future complications be it T2DM, CVD, VTE, DIC, cancers etc. Decreased risk of endometrial and ovarian cancers has been indicated with the use of OCPs as they are known to regularize the menstrual cyclicity and thus prevents endometrial hyperplasia, however, their long term use can increase the risk of other type of cancers like cervical and breast cancer as has been reported elsewhere72,73. Further, it has been reported that OCP use for a period of 10 years doubles the risk of cervical cancer74. Our study does not deal directly with oral contraceptive use and the risk of developing cancers, however, our data regarding weight gain, insulin resistance, deranged metabolism and inflammatory markers in OCP treated subjects indicate possibility of increased risk for various cancers in addition to other depicted impediments of this syndrome.
Conclusion
Our study suggests that OCP as a mode of treatment has indicated efficacy in terms of regularizing menstrual cycles and improving hyperandrogenism thus reducing clinical symptoms like hirsutism, alopecia and acne, but at the same time use of OCPs does contribute to the worsening of disease process. Our data showed worsening of anthropometric, glucose, lipid, insulin, inflammation and coagulation parameters indicating adverse effect of the drug treatment. Thus the interaction of this drug with diverse metabolic pathways leads to increased risk for development of obesity, T2DM, CVD, DIC and VTE. Instead of generalizing OCP as a mode of treatment consideration should be given for high-risk individuals in terms of alternative therapeutic agents and lifestyle modification strategies for better management of disease.
Materials and Methods
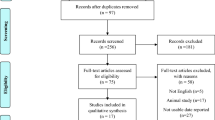
Study subjects
This observational pilot study (Conducted from Jan. 2014–Mar 2017) was approved by our Institutional Board of Research Studies (BORS), Department of Biochemistry, University Of Kashmir (No: f (BORS-Biological Science, Res/KU/15-10, SIMS 131/1EC-SKIMS/2013-6479) and informed written consent was obtained from the participants (all from Kashmir). Subjects who attended the Endocrinology and Gynecology Clinics, and presented with menstrual disturbances (oligo-/amenorrhea), hyperandrogenism (alopecia, acne and acanthosis), infertility or polycystic ovaries on USG were enrolled. PCOS subjects were selected according to Rotterdam 2003 criteria with all the relevant guidelines strictly followed. Subjects not taking any kind of drug treatment were considered as drug naive PCOS controls (n = 50) and those subjects (n = 50) who took only OCPs (Ethinyl estradiol 0.03 mg, levonorgestrel 0.15 mg) as a mode of treatment for minimum period of six months served as cases. All women had normal renal, hepatic and thyroid functions. Exclusion criteria for the study were ongoing pregnancy, lactation, Non classic adrenal hyperplasia, Cushing’s syndrome, thyroid dysfunction, hyperprolactinaemia, androgen producing tumors, diabetes mellitus, history of coronary artery diseases and coagulation abnormalities. The drug history and smoking status was also evaluated for exclusion criteria.
Clinical and anthropometric measures
All the study subjects were weighed on an electronic scale in light clothes without shoes. Height without shoes was measured to the nearest centimeter in a standing position with the feet fairly close together. Waist circumference was measured midway between the lower rib margin and iliac crest whereas the hip was measured at the maximum circumference over the buttocks using a non-folded tape. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m²). The clinical assessment included menstrual history and quantitation of hyperandrogenism (i.e., acne vulgaris, alopecia, acanthosis nigricans and hirsutism). Hirsutism assessment has been done using modified FG score. A score of >8 out of 36 has been taken significant and further evidence of PCOS on USG as the presence of 12 or more follicles, measuring 2–9 mm in diameter, in each ovary and/or increased ovarian volume (>10 cm3).
Sample collection
The sampling was done in morning after an overnight fast during early follicular phase (day 2–7) of cycle. The blood samples required for basic biochemical, insulin and hormonal investigations were collected in clot–activator tubes whereas the blood samples required for analysis of adiponectin, IL1- β, visfatin, resistin, tissue factor, PT and APTT were collected in tri-sodium citrate vials.
Investigations and assays
-
Basic biochemistry and metabolic profile: Oral glucose tolerance test (OGTT)
Kidney function test (KFT) - creatinine, uric acid, urea
Liver function test (LFT) - Serum glutamic pyruvic transaminase (SGPT) and
Serum glutamic oxaloacetic transaminase (SGOT)
Lipids –triglyceride, total cholesterol
Insulin.
-
Hormones: Testosterone, Luteinizing hormone (LH), Follicle stimulating hormone (FSH), Thyroid stimulating hormone (TSH), T4 & T3- to rule out thyroid dysfunction, 17-hydroxy progesterone (17-OHP)- to rule out Non classic adrenal hyperplasia and Prolactin (PRL)- to rule out hyperprolactinaemia.
-
Inflammation Profile: Adiponectin, IL 1β, Visfatin and Resistin.
-
Coagulation Profile: Tissue factor (FIII), Prothrombin time (PT) and Activated partial thromboplastin time (APTT).
Oral glucose tolerance test (OGTT) was performed after 10–14 hour fasting with 75 grams of oral anhydrous glucose load dissolved in 300 ml of water. Blood samples were drawn after every one-hour for OGTT. All the basic biochemical parameters (OGTT, KFT, LFT and Lipid profile) were estimated on semi-automated analyzer (TRANSASIA ERBA CHEM-7) by using ERBA diagnostic Mannheim Gmbh kits. Hormonal analysis (17-OHP, T4, TSH, LH, FSH, Testosterone and PRL) was done by using Chemiluminescence Immunoassays. The sampling for hormonal analysis was done on 2nd to 7th day of the follicular phase of menstrual cycle. Insulin, Adiponectin, Visfatin, Resistin and Tissue factor levels were measured by ELISA on BIORAD analyzer using Raybiotech kits. Interleukin-1β levels were quantified by ELISA on BIORAD analyzer using Boster’s human IL-1β ELISA kit. Levels of PT and APTT were estimated on CA-500 automated analyzer by using SIEMENS kits according to their respective protocols. Quick’s one stage method and Activated partial thromboplastin time method were used for measuring PT and APTT respectively. Insulin resistance and insulin sensitivity were calculated by Homeostatic model assessment of insulin resistance (HOMA-IR) and Quantitative insulin sensitivity check index (QUICKI) respectively75.
Calculations
HOMA-IR was calculated by formula:
QUICKI was calculated by a formula:
High HOMA-IR and low QUICKI scores denote Insulin resistance (low Insulin sensitivity).
Statistics
Statistical analysis was done using SPSS 16.0 version (IBM, Armonk, NY, USA). Parameters like anthropometry, basic biochemistry, hormones and insulin etc measures were compared between cases and controls using two-sampled t-test. Results are expressed as Mean ± SD. Threshold for statistical significance was set at p < 0.05. Pearson’s correlation coefficient (r) and stepwise Multiple regression analysis was used to analyze association among various study variables.
References
Azziz, R. et al. The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab. 89, 2745–2749 (2004).
Kebapcilar, L., Taner, C. E., Kebapcilar, A. G. & Sari, I. High mean platelet volume, low-grade systemic coagulation and fibrinolytic activation are associated with androgen and insulin levels in polycystic ovary syndrome. Arch. Gynaecol. Obstet. 280, 187–193 (2009).
Sirmans, S. M. & Pate, K. A. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol. 6, 1 (2013).
Setji, T. L. & Brown, A. J. Polycystic ovary syndrome: update on diagnosis and treatment. Am. J. Med. 127, 912–919 (2014).
Tilg, H. & Moschen, A. R. Adipocytokines: Mediators Linking Adipose Tissue, Inflammation and Immunity. Nat. Rev. Immunol. 6, 772–783 (2006).
Copaci, I., Micu, L. & Voiculescu, M. The role of cytokines in non-alcoholic steatohepatitis. A review. J. Gastrointestin. Liver Dis. 15, 363–373 (2006).
Braunersreuther, V., Viviani, G. L., Mach, F. & Montecucco, F. Role of cytokines and chemokines in non-alcoholic fatty liver disease. World J.Gastroenterol. 18, 727–735 (2012).
Goodarzi, M. O. & Korenman, S. G. The importance of insulin resistance in polycystic ovary syndrome. Fertil. Steril. 77, 255–258 (2002).
Morange, P. E. & Alessi, M. C. Thrombosis in central obesity and metabolic syndrome: mechanisms and epidemiology. Thromb. Haemost. 110, 669–680 (2013).
Stegenga, M. E. et al. Hyperglycemia stimulates coagulation, whereas hyperinsulinemia impairs fibrinolysis in healthy humans. Diabetes. 55, 1807–1812 (2006).
Frank, G., John, P. K., Neal, S. R. & Judi, M. Elevated Circulating Levels of Tissue Factor in Polycystic Ovary Syndrome. Clin. Appl. Thromb./Hemostasis. 19, 66–72 (2013).
Legro, R. S. Polycystic ovary syndrome and cardiovascular disease: a premature association? Endocr. Rev. 24, 302–312 (2003).
Apridonidze, T., Essah, P. A., Iuorno, M. J. & Nestler, J. E. Prevalence and characteristics of the metabolic syndrome in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metabol. 90, 1929–1935 (2005).
Luque-RamÃrez, M. et al. Comparison of ethinyl-estradiol plus cyproterone acetate versus metformin effects on classic metabolic cardiovascular risk factors in women with the polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 92, 2453–2461 (2007).
Talbott, E. O. et al. Evidence for an association between metabolic cardiovascular syndrome and coronary and aortic calcification among women with polycystic ovary syndrome. J. Clin Endocrinol. Metab. 89, 5454–5461 (2004).
Yildiz, B. O., Haznedaroglu, I. C., Kirazli, S. & Bayraktar, M. Global fibrinolytic capacity is decreased in polycystic ovary syndrome, suggesting a prothrombotic state. J. Clin. Endocrinol. Metab. 87, 3871–3875 (2002).
Paradisi, G. et al. Polycystic ovary syndrome is associated with endothelial dysfunction. Circulation. 103, 410–1415 (2001).
Sakkinen, P. A., Wahl, P., Cushman, M., Lewis, M. R. & Tracy, R. P. Clustering of procoagulation, inflammation, and fibrinolysis variables with metabolic factors in insulin resistance syndrome. Am. J. Epidemiol. 152, 897–907 (2000).
Steinberg, H. O. et al. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J. Clin. Invest. 97, 2601 (1996).
Escobar-Morreale, H. C. F. & San Millán, J. L. Abdominal adiposity and the polycystic ovary syndrome. Trends. Endocrinol. Metab. 18, 266–272 (2007).
Alvarez-Blasco, F., Botella-Carretero, J., San Millan, J. & Escobar-Morreale, H. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch. Intern. Med. 166, 2081–2086 (2006).
Teede, H. J. et al. Endothelial function and insulin resistance in polycystic ovary syndrome: the effects of medical therapy. Fertil and steril. 93, 184–191 (2010).
Akhter, Q. S., Akhter, N., Begum, U. N. & Rahman, F. Assessment of Coagulation Disorder in Women Taking Oral Contraceptives. J Bangladesh Soc Physiol. 9, 1–5 (2014).
Carmina, E. et al. Phenotypic variation in hyperandrogenic women influences the findings of abnormal metabolic and cardiovascular risk parameters. J. Clin. Endocrinol. Metab. 90, 2545–9 (2005).
Weyer, C., Tataranni, P. A., Bogardus, C. & Pratley, R. E. Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care. 24, 89–94 (2001).
Kadowaki, T. & Yamauchi, T. Adiponectin and adiponectin receptors. Endocr. Rev. 26, 439–451 (2005).
Tan, B. K. et al. Upregulation of adiponectin receptor 1 and 2 mRNA and protein in adipose tissue and adipocytes in insulin-resistant women with polycystic ovary syndrome. Diabetologia 49, 2723–2728 (2006).
Dinarello, C. A. Biologic basis for interleukin-1 in disease. Blood. 87, 2095–147 (1996).
Matsuki, T., Horai, R., Sudo, K. & Iwakura, Y. IL-1 plays an important role in lipid metabolism by regulating insulin levels under physiological conditions. J. Exp. Med. 198, 877–88 (2003).
Maedler, K., Dharmadhikari, G., Schumann, D. M. & Størling, J. Interleukin-1 beta targeted therapy for type 2 diabetes. Expert. Opin. Biol. Ther. 9, 1177–88 (2009).
Garten, A. et al. Nicotin amide phosphoribosyl transferase (NAMPT/PBEF/visfatin) is constitutively released from human hepatocytes. Biochem. Biophys. Res. Commun. 391, 376–381 (2010).
Fukuhara, A. et al. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science. 307, 426–30 (2005).
Hug, C. & Lodish, H. F. Medicine. Visfatin: a new adipokine. Science. 307, 366–7 (2005).
Fatemeh Farshchian. et al. Visfatin and Resistin Serum Levels in Normal-Weight and Obese Women With Polycystic Ovary Syndrome. Int. J. Endocrinol. Metab. 12, e15503 (2014).
Steppan, C. M., Wang, J., Whiteman, E. L., Birnbaum, M. J. & Lazar, M. A. Activation of SOCS-3 by resistin. Mol. Cell. Biol. 25, 1569–1575 (2005).
Shi, H., Tzameli, I., Bjorbaek, C. & Flier, J. S. Suppressor of cytokine signaling 3 is a physiological regulator of adipocyte insulin signaling. J. Biol. Chem. 279, 34733–34740 (2004).
Qi, Y. et al. Loss of resistin improves glucose homeostasis in leptin deficiency. Diabetes. 55, 3083–3090 (2006).
Konrad, A. et al. Resistin is an inflammatory marker of inflammatory bowel disease in humans. Eur. J. Gastroenterol. Hepatol. 19, 1070–1074 (2007).
Gnacinska, M., Malgorzewicz, S., Stojek, M., Lysiak-Szydlowska, W. & Sworczak, K. Role of adipokines in complications related to obesity: a review. Adv. Med. Sci. 54, 150–157 (2009).
Chu, A. J. Tissue factor mediates inflammation. Arch. Biochem. Biophysics. 440, 123–132 (2005).
Carr, M. E. Diabetes mellitus: a hypercoagulable state. J. Diabet. complications. 15, 44–54 (2001).
Ross, R. Atherosclerosis an inflammatory disease. N. Engl. J. Med. 340, 115–126 (1999).
Mina, A., Favaloro, E. J., Mohammed, S. & Koutts, J. A laboratory evaluation into the short activated partial thromboplastin time. Blood Coagul. Fibrin. 21, 152–157 (2010).
Tripodi, A., Chantarangkul, V., Martinelli, I., Bucciarelli, P. & Mannucci, P. M. A shortened activated partial thromboplastin time is associated with the risk of venous thromboembolism. Blood. 104, 3631–3634 (2004).
Lippi, G. et al. Epidemiological association between fasting plasma glucose and shortened APTT. Clin. Biochem. 42, 118–120 (2009).
Barazzoni, R. et al. Increased fibrinogen production in type 2 diabetic patients without detectable vascular complications: correlation with plasma glucagon concentrations. J. Clin. Endocrinol. Metab. 85, 3121–3125 (2000).
James, W. D. Acne. N Engl J Med. 352, 1463–1472 (2005).
Nader, S. & Diamanti-Kandarakis, E. Polycystic ovary syndrome, oral contraceptives and metabolic issues: new perspectives and a unifying hypothesis. Hum. Reprod. 22, 317–22 (2007).
Korytkowski, M. T. et al. Metabolic effects of oral contraceptives in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 80, 3327–34 (1995).
Dahlgren, E. et al. Effects of two antiandrogen treatments on hirsutism and insulin sensitivity in women with polycystic ovary syndrome. Hum. Reprod. 13, 2706–11 (1998).
Nader, S., Raid-Gabriel, M. G. & Saad, M. F. The effect of desogestrel-containing oral contraceptives on glucose tolerance and leptin concentrations in hyperandrogenic women. J. Clin. Endocrinol. Metab. 82, 3074–3077 (1997).
Armstrong, V. L. et al. Insulin action and insulin secretion in polycystic ovary syndrome treated with ethinyloestradiol/cyproterone acetate. QJM. 94, 31–7 (2001).
Cibula, D. et al. Increased risk of non-insulin dependent diabetes mellitus, arterial hypertension and coronary artery disease in perimenopausal women with a history of the polycystic ovary syndrome. Hum. Reprod. 15, 785–9 (2000).
Elter, K. et al. Clinical, endocrine and metabolic effects of metformin added to ethinyl estradiol-cyproterone acetate in non-obese women with polycystic ovarian syndrome: a randomized controlled study. Hum. Reprod. 17, 1729–37 (2002).
Morin-Papunen, L. C. et al. Metformin versus ethinyl estradiol-cyproterone acetate in the treatment of non obese women with polycystic ovary syndrome: a randomized study. J. Clin. Endocrinol. Metab. 88, 148–156 (2003).
Dahlgren, E., Janson, P. O., Johansson, S., Lapidus, L. & Oden, A. Polycystic ovary syndrome and risk for myocardial infarction, evaluated from a risk factor model based on a prospective study of women. Acta. Obstet. Gynecol. Scand. 71, 599–604 (1992b).
Stefan, N. & Stumvoll, M. Adiponectin—its role in metabolism and beyond. Horm Metab Res. 34, 69–474 (2002).
Matsubara, M., Maruoka, S. & Katayose, S. Decreased plasma adiponectin concentrations in women with dyslipidemia. J. Clin. Endocrinol. Metab. 87, 2764–2769 (2002).
Trujillo, M. E. & Scherer, P. E. Adiponectin-journey from an adipocytes secretory protein to biomarker of the metabolic syndrome. J. Intern. Med. 257, 167–75 (2005).
Hotta, K. et al. Circulating concentrations of the adipocytes protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes. 50, 1126–33 (2001).
Dinarello, C. A. Immunological and inflammatory functions of the interleukin-1 family. Acta. Obstet. Gynecol. Scand. 27, 519–50 (2009).
Mandrup-Poulsen, T., Bendtzen, K. & Nerup, J. Affinity-purified human interleukin I is cytotoxic to isolated islets of Langerhans. Diabetologia. 29, 63–7 (1998).
Eizirik, D. L. Interleukin-1 induced impairment in pancreatic islet oxidative metabolism of glucose is inhibitory protein-mediated β -cell proliferation in human pancreatic islets. Diabetes. 55, 2713–22 (1988).
Kang, J. H., Yu, B. Y. & Youn, D. S. “Relationship of serum adiponectin and resistin levels with breast cancer risk”. J. Korean Med. Sci. 22, 117–121 (2007).
Kim, S. R. et al. Visfatin enhances ICAM-1 and VCAM-1 expression through ROS-dependent NF-κB activation in endothelial cells. Biochimet Biophys Acta (BBA)-Mol Cell Res. 1783, 886–895 (2008).
Cymbaluk-Płoska, A. et al. Circulating Serum Level of Visfatin in Patients with Endometrial Cancer. Bio Med res int (2018).
Chang, Y. H., Chang, D. M., Lin, K. C., Shin, S. J. & Lee, Y. J. Visfatin in overweight/obesity, type 2 diabetes mellitus, insulin resistance, metabolic syndrome and cardiovascular diseases: a meta‐analysis and systemic review. Diabetes Metab Res rev. 27, 515–527 (2011).
Schuring, A. N., Schulte, N., Sonntag, B. & Kiesel, L. Androgens and insulin two key players in polycystic ovary syndrome. Gynakol. Geburtshilfliche. Rundsch. 48, 9–15 (2008).
Carmassi, F. et al. Insulin resistance causes impaired vasodilation and hypofibrinolysis in young women with polycystic ovary syndrome. Thromb. Res. 116, 207–214 (2005).
Danesh, J., Collins, R., Appleby, P. & Peto, R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. Jama. 279, 1477–1482 (1998).
Zakai, N. A., Ohira, T., White, R., Folsom, A. R. & Cushman, M. Activated partial thromboplastin time and risk of future venous thromboembolism. Am. J. Med. 121, 231–238 (2008).
Vessey, M. P. & Painter, R. Endometrial and ovarian cancer and oral contraceptives-findings in a large cohort study. British J cancer. 71, 1340 (1995).
Cogliano, V. et al. For the WHO International Agency for Research on Cancer. Carcinogenicity of combined oestrogen-progestagen contraceptives and menopausal treatment. Lancet Oncol. 6, 552–53 (2005).
Smith, J. S. et al. Cervical cancer and use of hormonal contraceptives: a systematic review. The Lancet. 361, 1159–1167 (2003).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetolgia. 28, 412–419 (1985).
Acknowledgements
Authors acknowledge research grants provided by J&K, DST (Grant No. ST/P&S/R&E/2012–13/121) and UGC, New Delhi (F.42-1051/2013(SR)).
Author information
Authors and Affiliations
Contributions
S.M. performed majority of experiments, manuscript writing and data analysis. M.A.G. main Endocrinology Consultant recruited and supervised all subjects. F.R. conception and design of the project along with M.A.G., manuscript writing and revision, project management and funding. Z.A.S., I.A.B. and S.A. provided lab facilities and helped in some experimental procedures. S.D.Y. data analysis is part of various other OCP related research works of our group. H.J., I.A.K. and Q.F. sample collection and basic diagnostic tests of PCOS women. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manzoor, S., Ganie, M.A., Amin, S. et al. Oral contraceptive use increases risk of inflammatory and coagulatory disorders in women with Polycystic Ovarian Syndrome: An observational study. Sci Rep 9, 10182 (2019). https://doi.org/10.1038/s41598-019-46644-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-46644-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.