Abstract
Currently, the diagnostic role of medical thoracoscopy in childhood pleural tuberculosis remains uncertain. Therefore, this retrospective study was conducted to evaluate the diagnostic performance of histological examination of tissue samples obtained by medical thoracoscopy in childhood pleural tuberculosis. Hospitalized children who underwent medical thoracoscopy between May 2012 and March 2016 were included in the study. Tissue samples obtained by thoracoscopy were submitted for histological examination (hematoxylin and eosin staining). Descriptive statistical methods were used for data interpretation, and the data were expressed as the mean ± standard deviation. The childhood tuberculosis patients had the following characteristics: 11 had pleural tuberculosis and 9 had pleural tuberculosis + pulmonary tuberculosis, the average age was 13.0 ± 2.2 years old, 60% were male, 26.3% (5/19) of patients tested positive for acid-fast bacilli positive in smears, 21.1% (4/19) of patients were positive for TB-PCR, and 90% (18) of pleural tuberculosis patients were positive in the culture for Mycobacterium tuberculosis. The sensitivity of histological examinations of tissue samples obtained by thoracoscopy in the detection of pleural tuberculosis was 80% (16/20). Complications were reported in 15 cases, and all complications disappeared spontaneously without any specific treatment. Therefore, we concluded that medical thoracoscopy was a sensitive and safe tool for the detection of childhood pleural tuberculosis.
Similar content being viewed by others
Introduction
Tuberculosis (TB) remains one of the world’s most serious infectious diseases. Approximately one-third of the human population is infected with Mycobacterium tuberculosis (M.TB), with 9.6 million new cases and 1.7 million deaths per year1. China ranks second among the 22 high-burden countries for TB. In 2014, the WHO reported that 1.3 million new cases of TB were estimated to occur. For childhood TB, it was estimated that 7.6 million children were infected by M.TB, and one-tenth developed the disease2. Despite causing morbidity and mortality, childhood TB remains a neglected disease: (1) childhood TB, which is paucibacillary and smear-negative, is not prioritized by national TB control programs; (2) current TB assays have performed poorly in the detection of childhood TB; and (3) obtaining specimens for TB examination is difficult. Therefore, more research, prevention and diagnosis of TB among children are urgently needed.
In a previous study, we described the clinicopathologic characteristics of childhood pleural TB patients3. The data showed that TB assays, such as acid-fast bacilli (AFB) smears, PCR and mycobacterial cultures, have limited diagnostic value in childhood pleural TB. Timely diagnosis is critical to ensure optimized therapy and avoid unnecessary treatment. The ideal methods of diagnosing TB are histological examination and mycobacterial culture. However, often in children this is not possible due to the low bacterial load and difficulty in collecting specimens4,5,6.
Medical thoracoscopy has proved to be an effective and safe procedure for diagnosing pleural effusions of undetermined causes and is particularly helpful in the detection of tuberculous pleural effusion in high TB prevalence areas7. However, the diagnostic role of medical thoracoscopy in childhood pleural tuberculosis remains uncertain. In the study, our goal was to evaluate the diagnostic performance of histological examination of tissue samples obtained by thoracoscopy in the detection of childhood pleural TB.
Patients and Methods
The study was conducted at the Department of Laboratory Medicine, Shandong Provincial Chest Hospital (SPCH). Ethical approval was provided by the ethics committee of SPCH. All patients gave informed consent to undergo thoracoscopy. However, informed consent was waived for the study by the ethics committee of SPCH given the retrospective study design. All patient records were anonymized and de-identified prior to analysis. The SPCH is one of the largest provincial referral TB hospitals in China.
Between May 2012 and March 2016, hospitalized children who underwent medical thoracoscopy were included in the study. Defined pleural TB cases were diagnosed if mycobacterial culture or TB-PCR was positive or if histological examination was positive. Probable cases were diagnosed based on AFB smears, and a response to anti-TB medications was revealed by clinical symptoms and chest radiographs. A control subject was defined if an alternative diagnosis was made.
Briefly, thoracoscopy was performed in the lateral decubitus position. Preoperative thoracic ultrasounds (Logiq 5, GE, Waskesha, USA) were performed to evaluate pleural adhesions, thickenings, nodules and masses and were also suggested to identify the optimal site of entry. After local or total anesthesia, an incision of approximately 1 cm was made, and a 5-mm thoracoscope (Richard Wolf, Knittlingen, Germany) was inserted via a 5-mm trocar. The pleural tissues were retrieved with grasping forceps. Abnormal areas, such as those exhibiting hyperemia, edema and a diffuse, single nodule, were biopsied. Usually, 3 or 5 biopsy specimens with 1 cm to 2 cm in margins were obtained. The chest tubes were left routinely.
Tissues were submitted for histological examination (hematoxylin and eosin staining), and each case was reviewed independently by two pathologists. The histopathological examination of pleural biopsies was reported as probable or definite TB according to the findings of epithelioid cells, multinucleated giant cells or caseous necrosis (definite). Mycobacterial cultures (Löwenstein-Jensen method), AFB (Auramine O stain) and TB-PCR (DAAN, Guangzhou, China) were conducted on several types of specimens, such as sputum, pleural effusions and tissues. It was worth noting that fewer than 2% of cultures became contaminated in the laboratory, and until now, none of tissue cultures contaminated. Pleural biochemistry tests, such as total protein (Siemens, Tarrytown, NY, USA), total bilirubin (Siemens, Tarrytown, NY, USA), glucose (Siemens, Tarrytown, NY, USA), lactate dehydrogenase (Kehua, Shanghai, China) and adenosine deaminase (Maker, Chengdou, Sichuan, China), were assayed on an Advia 2400 chemistry analyzer (Siemens, Tarrytown, NY, USA). Data were expressed as the mean ± standard deviation (SD), and the sensitivities of the histological examination of tissue samples obtained by medical thoracoscopy in the detection of pleural TB were calculated. The data that support the findings of this study are available from the corresponding author on reasonable request.
Results
Patient characteristics
As shown in Table 1, a total 22 patients were enrolled in our study (Fig. 1). Among them, two patients were diagnosed as pleural disease, not TB (one was lung cancer and the other was interstitial lung disease), and the remaining 20 patients were pleural TB, including 11 with pleural TB and 9 with pleural TB + pulmonary TB. Thirteen (59.1%, 13/22) patients were tested for HIV, and all were seronegative. For the 20 pleural TB patients, the average age was 13.0 ± 2.2 years; 60% (12/20) were male; and fever was the most common presenting symptom (90%, 18/20), followed by chest pain (55%, 11/20), cough (45%, 9/20) and dyspnea (20%, 4/20). Two patients had a contact history with TB patients. The individual patient characteristics were included in Table 2.
Pleural analysis
Pleural effusions from 14 patients (including one pleural disease, not TB) were evaluated for biochemistry and all were classified as exudates. Pleural cytology was evaluated in 7 patients (including one pleural disease, not TB) and all were lymphocyte-dominant. Biochemical analysis was performed on pleural effusions in pleural TB, total protein was 48.9 ± 5.6 g/L, and total bilirubin was 11.27 ± 10.56 mmol/L. Glucose was 3.17 ± 1.57 mmol/L, lactate dehydrogenase was 1021 ± 843 U/L, and adenosine deaminase was 62.5 ± 32.4 U/L.
Thoracoscopic findings
Fifteen patients were locally anesthetized with 1% lidocaine, and the remaining seven were anesthetized with intravenous fentanyl citrate (0.1 mg/kg intravenously). Seventeen patients have detailed clinical information on the procedure: two patients were biopsied from visceral pleura, 15 from parietal pleura and the locations of the biopsied tissues from the remaining five were unclear. Thoracoscopic findings showed loculation in 16 cases (72.7%, 16/22), adhesion in 16 cases (72.7%, 16/22) and pleural thickening in 19 cases (86.4%, 19/22).
Diagnostic performance of medical thoracoscopy
In the study, sensitivity was calculated using the clinical diagnosis as the reference: 26.3% (5/19) of pleural TB patients were classified AFB positive from their smears, TB-PCR yielded positive results in 21.1% (4/19) of pleural TB patients, and 90% of pleural TB patients (18/20) were positive in culture for M.TB. The sensitivity of histological examinations of tissue samples obtained by medical thoracoscopy in the detection of pleural TB was 80% (16/20), including 13 definite cases and 3 probable cases.
Complications and outcomes
Complications of thoracoscopy were reported in 15 cases, including postoperative pain (12 cases, 54.5%), mild bleeding (6 cases, 27.3%), nausea (1 case, 4.5%) and pneumothorax (1 case, 4.5%). All complications disappeared spontaneously without any specific treatment. None of the TB patients required thoracic surgery or developed infections.
Pleural tissues were taken from all patients, and nine children (9/22, 40.9%) subsequently underwent an interventional procedure (such as decortication of pleural fibrous tissue and peeling off the additional adhesions) using thoracoscopy. Of the nine children, four (cases 5, 8, 13 and 14) had a repeat thoracoscopy for intervention. Although anti-TB treatment had been completed in case 9, a relapse occurred. Case 22 underwent thoracoscopic surgery for pulmonary bulla.
Discussion
After several decades of neglect, childhood TB is receiving some of the attention it deserves. In 2014, the WHO developed the Roadmap for Childhood TB. Its plan, to reach zero TB deaths among children worldwide is within our grasp8. There are several reasons childhood TB has been neglected. Most important is the misconception that childhood TB is difficult to diagnose because it can be culture-confirmed in only 20% to 40% of cases (compared with 90% of adult cases)9. As a result, many childhood TB cases are never diagnosed and most children are diagnosed clinically. This would cause a significant delay in the diagnosis of childhood TB. In addition, diagnostic accuracy has a significant impact on the successful treatment of childhood TB.
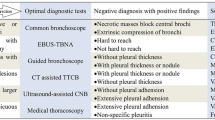
Histology can provide strong supportive evidence for a diagnosis of TB. Histological examination has several advantages, such timeline, low cost, and no need for special equipment. However, the accuracy of histological examination is dependent on obtaining an adequate tissue sample10. Several tissue sampling techniques have been evaluated in children for TB diagnosis, such as, endobronchial ultrasound-guided transbronchial needle aspiration11, ultrasound-guided biopsy12,13, and CT-guided biopsy14.
For pleural disease, thoracoscopy seems to be a safe, simple, and accurate tool15,16. In tuberculous pleuritis, the combined sensitivity of histology and culture for rigid thoracoscopy was nearly 100%17,18. In our study, we showed the technique has a sensitivity of 80%. It was a sensitive diagnostic method in detecting childhood pleural TB in high TB burden country. Similarly, a small sample size was used to conduct research in children in a low-TB burden country19. That study reviewed the results of seven children examined by medical thoracoscopy, and proposed a similar conclusion as that in this study. Although several types of complications have been reported in our study, only one child required further therapy for pneumothorax.
It should be worthy to be noted that CT- or ultrasound-guided biopsy have been demonstrated to be useful for determining the causes of pleural effusions20,21,22, and it has been suggested that the image-guided pleural needle biopsy has advantages in some aspects22,23. However, there were no randomized research studies performed in children, and the technique may not be applicable to childhood pleural TB.
Several limits should be taken into account when interpreting these results. First, this study has a retrospective nature and incomplete information about the patient’s characteristics. Second, the sample size was small, and few patients in the control group underwent thoracoscopy, because our hospital is a referral TB hospital. Third, unstandardised thoracoscopy was performed in the study, and this could lead to a biased sample set and uncertain generalisability of the results. Fourth, for detection of childhood pleural TB, further analysis must be performed to validate the role of CT in assessing childhood TB prior to thoracoscopy and to compare diagnostic values of thoracoscopy and image-guided pleural biopsy24.
Conclusions
In conclusion, in a high-TB burden country, medical thoracoscopy was a sensitive and safe tool in the detection of childhood pleural TB.
References
Rappuoli, R. & Aderem, A. A 2020 vision for vaccines against HIV, tuberculosis and malaria. Nature 473, 463–469 (2011).
Dodd, P. J., Gardiner, E., Coghlan, R. & Seddon, J. A. Burden of childhood tuberculosis in 22 high-burden countries: a mathematical modelling study. Lancet Glob Health 2, e453–459 (2014).
Wang, J. L., Zhao, G. W., Zhang, Z. Q., Wang, X. F. & Wang, M. S. Clinicopathologic characteristics of pediatric tuberculous pleural effusion: a retrospective analysis of 112 consecutive cases. Eur Rev Med Pharmacol Sci 19, 2978–2982 (2015).
Mukhopadhyay, S. Role of histology in the diagnosis of infectious causes of granulomatous lung disease. Curr Opin Pulm Med 17, 189–196 (2011).
Nicol, M. P. & Zar, H. J. New specimens and laboratory diagnostics for childhood pulmonary TB: progress and prospects. Paediatr Respir Rev 12, 16–21 (2011).
Zar, H. J. et al. Rapid diagnosis of pulmonary tuberculosis in African children in a primary care setting by use of Xpert MTB/RIF on respiratory specimens: a prospective study. Lancet Glob Health 1, e97–104 (2013).
Wang, X. J. et al. Efficacy and safety of diagnostic thoracoscopy in undiagnosed pleural effusions. Respiration 90, 251–255 (2015).
Acosta, C. D. et al. A new roadmap for childhood tuberculosis. Lancet Glob Health 2, e15–17 (2014).
Starke, J. R. & Cruz, A. T. The global nature of childhood tuberculosis. Pediatrics 133, e725–727 (2014).
Ofiara, L. M., Navasakulpong, A., Beaudoin, S. & Gonzalez, A. V. Optimizing tissue sampling for the diagnosis, subtyping, and molecular analysis of lung cancer. Front Oncol 4, 253 (2014).
Dhooria, S. et al. A multicenter study on the utility and safety of EBUS-TBNA and EUS-B-FNA in children. Pediatr Pulmonol (2016).
Izquierdo, R., Shankar, R., Kort, K. & Khurana, K. Ultrasound-guided fine-needle aspiration in the management of thyroid nodules in children and adolescents. Thyroid 19, 703–705 (2009).
Matos, H., Noruegas, M. J., Goncalves, I. & Sanches, C. Effectiveness and safety of ultrasound-guided percutaneous liver biopsy in children. Pediatr Radiol 42, 1322–1325 (2012).
Ballah, D. et al. Percutaneous CT-guided vertebral bone biopsy in children. Pediatr Radiol 43, 582–588 (2013).
Rozman, A., Camlek, L., Marc-Malovrh, M., Triller, N. & Kern, I. Rigid versus semi-rigid thoracoscopy for the diagnosis of pleural disease: a randomized pilot study. Respirology 18, 704–710 (2013).
Dhooria, S., Singh, N., Aggarwal, A. N., Gupta, D. & Agarwal, R. A randomized trial comparing the diagnostic yield of rigid and semirigid thoracoscopy in undiagnosed pleural effusions. Respir Care 59, 756–764 (2014).
Diacon, A. H. et al. Diagnostic tools in tuberculous pleurisy: a direct comparative study. Eur Respir J 22, 589–591 (2003).
Yap, K. H., Phillips, M. J. & Lee, Y. C. Medical thoracoscopy: rigid thoracoscopy or flexi-rigid pleuroscopy? Curr Opin Pulm Med 20, 358–365 (2014).
Keys, C., McLeod, E., Pesti, C. & Armstrong, D. Thoracoscopic pleural biopsy as an aid to diagnosis in pediatric tuberculosis with pleural involvement. Eur J Pediatr Surg 22, 315–317 (2012).
Koegelenberg, C. F. et al. Direct comparison of the diagnostic yield of ultrasound-assisted Abrams and Tru-Cut needle biopsies for pleural tuberculosis. Thorax 65, 857–862 (2010).
Koegelenberg, C. F. et al. The utility of ultrasound-guided thoracentesis and pleural biopsy in undiagnosed pleural exudates. Thorax 70, 995–997 (2015).
Metintas, M. et al. Medical thoracoscopy vs CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: a randomized, controlled trial. Chest 137, 1362–1368 (2010).
Maturu, V. N. et al. Role of medical thoracoscopy and closed-blind pleural biopsy in undiagnosed exudative pleural effusions: a single-center experience of 348 patients. J Bronchology Interv Pulmonol 22, 121–129 (2015).
Hallifax, R. J., Talwar, A. & Rahman, N. M. The role of computed tomography in assessing pleural malignancy prior to thoracoscopy. Curr Opin Pulm Med 21, 368–371 (2015).
Author information
Authors and Affiliations
Contributions
W.M.S. collection, analysis and interpretation of data, drafting of the manuscript. H.C. analysis and interpretation of data. H.Y. study conception and design, analysis and interpretation of data.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, M., Han, C. & He, Y. Diagnostic role of medical thoracoscopy in childhood pleural tuberculosis. Sci Rep 9, 8399 (2019). https://doi.org/10.1038/s41598-019-44860-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44860-6
This article is cited by
-
Application of ultrasound-guided medical thoracoscopy in patients with small amounts or without pleural effusion
BMC Pulmonary Medicine (2024)
-
Factors associated with negative pleural adenosine deaminase results in the diagnosis of childhood pleural tuberculosis
BMC Infectious Diseases (2021)
-
Treatment delay in childhood pleural tuberculosis and associated factors
BMC Infectious Diseases (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.