Abstract
Metabolic syndrome (MetS) is a growing public health concern worldwide. It has been demonstrated that individuals with MetS are at an increased risk of cardiovascular events and diabetes. We aimed to investigate the prevalence of MetS and its components among Turkic and Kurds ethnic groups in a bi-ethnic (Turk and Kurd) population. This cross-sectional study is part of the national health transformation plan created in response to the emerging epidemic of non-communicable diseases (Iran’s Package of Essential Non-communicable Disease study), launched in 2014 in Naqadeh, Iran. In total, 3506 participants aged 30–70 years were randomly included in the study from urban and rural regions. Cardio-metabolic risk factors related to MetS diagnosis and other related sociodemographic factors were assessed for men and women in both the Turk and the Kurd population. Multivariate logistic regressions were applied to identify MetS -associated factors among both the Turk and the Kurd population. The mean (SD) age of the participants was 49.6 (12.3) years. Of the participants, 56.2% (n = 1969) were women, and 43.8% (n = 1537) were men. Three-fifths of the participants were Turk (60.3%, n = 1751). The overall prevalence of MetS was 37.05%, with a higher prevalence in women (49.8% versus 24.3% in men). The prevalence of MetS and its components among Turk people (41.6%) were significantly higher than that among Kurd people (33.9%) (p < 0.0001). In addition, the prevalence of MetS was higher among women, urban, and older people for both ethnicities. Strong associations were found between MetS prevalence and being older, being female, being overweight, being obese, having a higher waist-to-hip ratio, and having a history of diabetes and cardiovascular disease (CVD) in the family for both Turks and Kurds. The raised waist circumference (WC) is the most prevalent MetS component for Turk men and women. Meanwhile, the most prevalent MetS component for Kurd participants is low high-density lipoprotein for women and a raised WC for men. Significant differences were found between Kurdish men and women for all components, except for a raised WC and a raised fasting blood glucose (p < 0.05). Because the Iranian population features multiple ethnicities, the recognition of the prevalence of MetS components is a major step in establishing intervention strategies for modifying cardio-metabolic risk factors based on the population ethnicities and their socio-demographic, cultural, and lifestyle factors. We recommend future studies for planning an efficient and sustainable health education and promotion program to halt MetS prevalence.
Similar content being viewed by others
Introduction
Metabolic syndrome (MeTS) is a growing public health concern worldwide. It is a cluster of related MeTS risk factors that are characterized by abdominal obesity, increased triglycerides (TG), hypertension, an elevated fasting blood glucose (FBG) level, and reduced high-density lipoprotein (HDL) cholesterol1. Various definitions for the diagnosis of MetS currently exist2,3. The National Cholesterol Education Program Adult Treatment Panel (ATP) III defines METS as having three or more of the following conditions: an HDL of <40 mg/dl in men and <50 mg/dl in women, a systolic/diastolic blood pressure (BP) of ≥130/85 mm Hg, a triglyceride level at least 150 mg/dl, an FBG level of ≥100 mg/dl, and a waist circumference (WC) > 102 cm in men and >88 cm in women4.
The International Diabetes Federation (IDF) proposed another definition, viewing central obesity as an essential part of METS3. Meanwhile, the American Heart Association/National Heart Lung and Blood Institute focuses on the accumulation of risk factors and does not place emphasis on central obesity5. An important step for MetS control is designing tailored interventions to various ethnic groups and to assess MetS elements with people from different ethnic backgrounds. In several countries, ethnic differences in the prevalence of cardiovascular diseases risk factors have been described6,7,8. However, only limited attention has been paid to ethnic differences in the prevalence of MetS and its components. A systematic review of Dalvand et al.9 has demonstrated an emerging high prevalence of MetS in general and in particular among Iranian people.
According to the IDF, central obesity is defined based on ethnicity-specific criteria, and for various ethnic groups, a cut-off for central obesity should be applied based on the population features10. Several studies in Iran have recommended that an optimal WC for the Iranian population is greater than 90 cm11,12. It has been demonstrated that individuals with METS are at an increased risk of cardiovascular events and diabetes13. A meta-analysis of 34 studies with 26,609 participants showed that 4.8–7% of young adults had METS between 2004 to 201514. The prevalence of METS among Iranians is increasing. The Tehran Lipid and Glucose Study (TLGS) reported MetS for women at 42% and for men at 24%15.
Iran is a multi-ethnic country with various ethnic groups, including Persians, Kurds, Lurs, Arabs, Turkics, Baluchi, and Turkmen. Turkics or Azeris are the second-largest ethnic group in Iran, making up an estimated 16% of the total population, and can be found in the northwestern part of the country. Meanwhile, Kurds are the third-largest ethnic groups in Iran and make up 10% of the population16. Naqadeh is a city in the western part of Azebaijan province in Iran and features the two largest ethnic groups of Trukic and Kurds17.
In this study, we aimed to investigate the prevalence of MetS and its components among the Turkic and Kurd ethnic groups in Naqadeh. MetS as a cluster of several risk factors is a useful metric for measuring the CDV health of the population in Naqadeh. Additionally, estimates of MetS prevalence will prove useful in evaluating the effectiveness of population-based lifestyle interventions across Iran’s Package of Essential Non-communicable Disease study (IraPEN program).
Methods
About iraPEN program in naqadeh
IraPEN is part of the national health transformation plan created in response to the emerging epidemic of non-communicable diseases, launched in 2014 by the Iranian Ministry of Health and Medical Education, to provide universal health coverage, including access to noncommunicable disease prevention and care as well as mental health services18. Naqadeh is a city in the western part of Azebaijan province, Iran, and features the two largest ethnic groups of Turks and Kurds and a population of 127,671. IraPEN has been successfully piloted in Iran’s four main districts, and its nationwide scale-up has begun in at least one district per province. All the methods were performed in accordance with the relevant guidelines and regulations.
Participants
Participants were all people 30–70 years old from urban and rural regions. Participants were recruited using household health files from health centers in urban areas and health houses in rural regions.
MeTS measurements
Prevalence of MetS was defined based on the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) as the presence of three or more of the following criteria (except for waist circumference which was defined as ≥90 cm for both genders for Iranian population): triglycerides level <150 mg dl−1, HDL level <40 mg dl−1 in men and <50 mg dl−1 in women, systolic/diastolic blood pressure 130/85 mmHg or higher and fasting blood glucose level 110 mg dl−1 or higher4. The International Diabetes Federation (IDF) has declared that WC is both a gender and ethnic-group specific indicator and that using this approach may provide a better assessment of obesity-related risk globally than using a single cut-off point19. The current definitions of central adiposity or waist circumference are based on data from western populations. However, several studies in Iran have suggested that a more realistic waist circumference for Iranians is >90 cm for both genders11,12,20. Blood sampling was collected for measurements of total cholesterol, triglycerides, LDL cholesterol, HDL-cholesterol, and fasting blood glucose for all participants. Overnight fasting for 12–14 hours was needed before blood sampling. Venous blood samples (5 ml) were collected. Fasting blood glucose (FBG) was measured by using the glucose oxidase method (intra- and inter assay coefficients of variation 2.1% and 2.6%, respectively). Body Mass Index (BMI) was measured by individual’s weight divided by the square of the height. Waist-to-hip ratio was calculated by waist circumference divided by hip circumference.
The WC was evaluated using a measuring tape to the nearest 0.1 cm. The weight of an individual dressed in light clothing without shoes was recorded each time using a calibrated scale to the nearest 0.1 kg. Height was measured without shoes using a stadiometer to the nearest 0.1 cm. BP was measured with a mercury sphygmomanometer twice in the same arm after the individual had been seated at rest for 10–15 minutes. The systolic and diastolic BP measurements were the mean of the two readings. Blood samples were collected for the measurement of total cholesterol, TG, low-density lipoprotein cholesterol, HDL cholesterol, and FBG for all participants. FBG was measured using the glucose oxidase method (intra- and inter-assay coefficients of variation of 2.1% and 2.6%, respectively).
All participants also responded to sociodemographic questions about their gender, age, marital status (single, married, divorced/widowed), educational qualifications (illiterate, primary, secondary, university degree), personal history, and family history of diabetes and hypertension (yes/no).
Statistical analysis
Statistical analyses were performed with Statistical Package for Social Science (SPSS 18 for windows, SPSS Inc.® headquarter, Chicago, USA). Normality of data was analyzed by Kolmogorov-Smirnov test. Continuous and discrete variables are presented with mean and ± SD, and number and percentage, respectively. Chi-square analyses were used to test the difference between biochemical variables between two groups. Multiple logistic regressions analysis was used to examine the associations between risk factors of metabolic syndrome and socio demographic factors as independent and dependent variables, respectively. Adjusted odds ratio and 95% confidence intervals were calculated for all metabolic syndrome parameters. P values less than 0.05 were regarded as statistically significant.
Ethical considerations
The ethics committee of Tabriz University of Medical Sciences approved the study (IRTBZMED.REC.1396.965). A signed informed consent form explaining the study purposes was obtained from each participant.
Results
Of 3691 participants, 3506 were evaluated, and 185 records were removed because of incomplete demographic or clinical information to assess accurate MetS measurements.
Demographic characteristics
The mean (SD) age of the participants was 49.6 (12.3) years. A total of 56.2% of participants were women, and 43.8 were men. About 35% of the participants were illiterate, and about two-thirds lived in urban areas. Regarding the participants’ ethnicity, three-fifths of them were Turks (60.3 Turks vs. 39.7 Kurds). See Table 1 for an overview.
Prevalence of metabolic syndrome
The overall prevalence of MetS was 37.05%, with a higher prevalence in women (49.8% versus 24.3% in men). There was a progressive increase in the prevalence of MetS with the increasing age of the participants (particularly those 50–59 years old). The percentages of the prevalence of MetS among Turks and Kurds was 41.6% and 33.9%, respectively. About half of the illiterate participants (47.8%) had MetS, and this percentage decreased with the increase of the education level. Also, about two-fifths of the participants in urban areas have MetS.
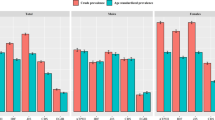
Prevalence of metabolic syndrome components
Table 2 depicts the prevalence of MetS components according to the ethnicities and sociodemographic characteristics of the study population. By comparing MetS components between both Turk and Kurd participants, we found that a raised WC is the most prevalent MetS component for Turk men and women and that the most prevalent MetS component for Kurd participants is low HDL for women and a raised WC for men. Significant differences were found between Kurdish men and women for all components except for a raised WC and raised FBS (p < 0.05).
The prevalence of a raised BP increases significantly by age among both the Turk and the Kurd people, and people 60–69 years of age have the most prevalent WC. By comparing the components based on education level, the WC is the most prevalent among illiterate Turk and Kurd participants. Also, an increased WC is the most prevalent component among rural and urban Turk people, and low HDL is the most prevalent among both rural and urban Kurds.
Based on the categorizing of the BMI into three groups (normal or underweight, overweight, and obese), the BMI is the most prevalent MetS component for obese Turks and Kurds. The association of metabolic syndrome and sociodemographic characteristics was assessed with multi-variate analyses (see Table 3) for both Turks and Kurds separately. Among both ethnicities, being a female Turk [OR 3.44, 95% CI: 2.58–4.58; p < 0.0001], a female Kurd [OR 2.8, 95% CI: 1.92–4.08; p < 0.0001], increasing in age, having overweight or obesity, having a higher waist-to-hip ratio, and having a history of diabetes and CVD in the family showed strong associations with MetS.
Discussion
This cross-sectional study was conducted in a bi-ethnic population in Naqadeh, Iran, to estimate MetS prevalence by covering more than 3000 participants. Our main findings showed that the total prevalence of MetS is 37.7%, with a higher prevalence among the Turk population (41.6%) versus the Kurd population (33.9%) and among the urban population (41.4%) versus the rural population (32.6%). Our study showed similar total MetS prevalence rates compared with other reports from Iran (22.8–42.3%)21,22,23 and other Asian countries and neighbors of Iran (16–50%)24,25,26,27. The wide prevalence range can be explained by the variety of populations and the times of the study in recent decades. Moreover, in our study, the Turk population had a relatively higher MetS prevalence compared with the Kurd population and other reported estimations form Iran28. Comparing MetS components of the Turk and Kurd populations revealed that both men and women of the Turk population had higher prevalence rates of a raised BP, abdominal obesity, a raised FBS, and TG but not low HDL. The cultural and lifestyle patterns of the Turk population may further contribute to their higher prevalence of MetS. No evidence exists regarding the level of physical activity and diet habit differences of both Turk and Kurd individuals.
An unhealthy lifestyle and dietary pattern can explain the high prevalence of MetS in urban areas23,29.
The prevalence of MetS and its components among women were significantly higher than those of men in both the Turk and the Kurd ethnicity except for abdominal obesity (P < 0.0001). Abdominal obesity was defined for the Iranian population as a WC ≥ 90 cm in men and women. Although the prevalence of abdominal obesity in this study was estimated based on Iranian ethnic cut-off points, making it greater than the ATP (III) definition (>102 cm for men and >88 cm for women), about half of the women in our study (49.8) had MetS. Thus, when one considers the ATP (III) criteria for abdominal obesity for women, the gender differences of MetS prevalence seem to be controversial. This result is consistent with other studies form Iran16,24 and other countries30,31 and it is inconsistent with Novak et al.’s results32, which found a higher MetS rate among men than women.
Strong associations of MetS prevalence were found with being older, being female, being overweight or obese, having a higher waist-to-hip ratio, and having a history of diabetes and CVD in the family in both the Turk and the Kurd ethnicity in the multivariate model. In our study, overweight and obese individuals had a higher risk of MetS by four and two times, respectively, among both Turks and Kurds. The prevalence of MetS increased with age and reached the highest risk at ages 70 and over among the Turk participants, with people 70 and older facing a five-times-greater risk of MetS.
Strength and limitations
Our study is the first large community-based survey comparing MetS prevalence between two large ethnic groups of the Iranian population in the region. In addition, the findings of the study can be generalized to the population due to the large sample size and sampling procedures. However, as this study is part of the IraPEN project in Naqadeh, we have no information about the dietary habits and lifestyle of the populations.
Conclusion and recommendations
This community-based study of the IraPEN survey identified the prevalence of MetS and its components among the two large ethnicities of Turks and Kurds in the Iranian population. The current study revealed that the prevalence of MetS and its components among the Turk people were significantly higher than those of the Kurds. Being female, living in a rural area, increasing age, being overweight or obesity, having a higher waist-to-hip ratio, and having a history of diabetes and CVD in the family were the strongest sociodemographic predictors of MetS. Due to the multiple ethnicities of the Iranian population, the recognition of the prevalence of MetS components is a major step in establishing intervention strategies for modifying cardio-metabolic risk factors based on the population’s ethnicities and their socio-demographic, cultural, and lifestyle factors. We recommend future research for planning an efficient and sustainable health education and promotion program to halt the prevalence of MetS.
Declaration
The study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IRTBZMED.REC.1396.965). All participants gave written informed consent. The data and material is available.
References
Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106 (2002).
Grundy, S. M. et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol. 44 (2004).
Alberti, K. G. M., Zimmet, P. & Shaw, J. The metabolic syndrome—a new worldwide definition. The Lancet. 366(9491), 1059–62 (2005).
Cleeman, J. et al. Expert panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP III). JAMA. 2001, 285 (2001).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 112(17), 2735–52 (2005).
Agyemang, C. et al. Hypertension control in a large multi-ethnic cohort in Amsterdam, The Netherlands: The HELIUS study. Int J Cardiol (2015)
Modesti, P. et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PloS one. 11, 1 (2016).
Agyemang, C. et al. Ethnicity and cardiovascular health research: pushing the boundaries by including comparison populations in the countries of origin. Ethn Health. (2012).
Dalvand, S. et al. Prevalence of Metabolic Syndrome among Iranian Population: A Systematic Review and Meta-analysis. Iranian Journal of Public Health. 46(4), 456–67 (2017).
Misra, A. et al. Waist circumference criteria for the diagnosis of abdominal obesity are not applicable uniformly to all populations and ethnic groups. Nutrition. 21(9), 969–76 (2005).
Esteghamati, A. et al. Optimal waist circumference cut-offs for the diagnosis of metabolic syndrome in Iranian adults: results of the third national survey of risk factors of non-communicable diseases (SuRFNCD-2007). Diabet Med. 26 (2009).
Delavar, M. A. et al. Dietary patterns and the metabolic syndrome in middle aged women, Babol. Iran Asia Pac J Clin Nutr. 18 (2009).
Azizi, F. et al. Appropriate waist circumference cut-off points among Iranian adults: the first report of the Iranian National Committee of Obesity. Arch Iran Med. 13 (2010)
Nolan, P. B. et al. Prevalence of metabolic syndrome and metabolic syndrome components in young adults: A pooled analysis. Preventive medicine reports. 7, 211–5 (2017).
Azizi, F. et al. Prevalence of metabolic syndrome in an urban population: Tehran Lipid and Glucose Study. Diabetes Res Clin Pract. 61 (2003)
WorldAtlas.com LEGII, https://www.worldatlas.com/articles/largest-ethnic-groups-in-iran.html.
Alberti, K. G., Zimmet, P. & Shaw, J. Metabolic syndrome–a new world-wide definition. A Consensus Statement from the InternationalDiabetes Federation. Diabet Med 23, 469–480 (2006).
Hajian-Tilaki, K. et al. Prevalence of metabolic syndrome and the association with socio-demographic characteristics and physical activity in urban population of Iranian adults: A population-based study. Diabetes & Metabolic Syndrome. Clinical Research & Reviews. 8(3), 170–6 (2014).
Noshad, S. et al. Prevalence of metabolic syndrome in Iran: A 2011 update. Journal of Diabetes. 9(5), 518–25 (2017).
Esmailnasab, N. et al. Risk Factors of Non-Communicable Diseases and Metabolic Syndrome. Iranian Journal of Public Health. 41(7), 77–85 (2012).
Zabetian, A. et al. Prevalence of metabolic syndrome in Iranian adult population, concordance between the IDF with the ATPIII and the WHO definitions. Diabetes Research and Clinical Practice. 77(2), 251–7 (2007).
Ravikiran, M. et al. Prevalence and risk factors of metabolic syndrome among Asian Indians: a community survey. Diabetes research and clinical practice. 89(2), 181–8 (2010).
Zuo, H. et al. Prevalence of metabolic syndrome and factors associated with its components in Chinese adults. Metabolism. 58(8), 1102–8 (2009).
Park, S.-Y. et al. Normal Range Albuminuria and Metabolic Syndrome in South Korea: The 2011–2012 Korean National Health and Nutrition Examination Survey. PLoS ONE. 10(5), e0125615 (2015).
Ansarimoghaddam, A. et al. Prevalence of metabolic syndrome in Middle-East countries: Meta-analysis of cross-sectional studies. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 12(2), 195–201 (2018).
Harikrishnan, S. et al. Prevalence of metabolic syndrome and its risk factors in Kerala, South India: Analysis of a community based cross-sectional study. PLOS ONE. 13(3), e0192372 (2018).
Jahangiry, L. et al. Modifiable lifestyle risk factors and metabolic syndrome: opportunities for a web-based preventive program. Journal of research in health sciences 14(4), 303–307 (2014).
Beigh, S. H. et al. Prevalence of metabolic syndrome and gender differences. Bioinformation. 8(13), 613–6 (2012).
Ogbera, A. O. et al. Prevalence and gender distribution of the metabolic syndrome. Diabetology & Metabolic Syndrome. 12(2(1)), 1 (2010).
Novak, M. et al. Gender differences in the prevalence of metabolic syndrome in 50-year-old Swedish men and women with hypertension born in 1953. Journal Of Human Hypertension. 27, 56 (2011).
Acknowledgements
This manuscript originated from a MSc. thesis (IRTBZMED.REC.1396.965) by LKHF, Department of Health Education and Promotion, faculty of Health, Tabriz, Iran. We are grateful to Tabriz University of Medical Sciences for providing facilities for the study. We wish to thank Urmia University of Medical Sciences for its support for the project. This study was not funded by special institutes.
Author information
Authors and Affiliations
Contributions
L.J., L.K., A.K. and R.E. were designed the project. L.K. was the main investigator, collected the data, L.J. and P.S. did the statistical analysis and wrote the first draft of the manuscript. L.J. was the research supervisor. A.K. and R.E. contributed to the statistics. R.E. helped as a consultant on the study design and questionnaire, and L.J. and K.P. critically and substantially revised the final article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jahangiry, L., Khosravi-far, L., Sarbakhsh, P. et al. Prevalence of metabolic syndrome and its determinants among Iranian adults: evidence of IraPEN survey on a bi-ethnic population. Sci Rep 9, 7937 (2019). https://doi.org/10.1038/s41598-019-44486-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44486-8
This article is cited by
-
Lifestyle patterns, nutritional, and metabolic syndrome determinants in a sample of the older Iranian population
BMC Geriatrics (2024)
-
Sex-specific prevalence of metabolic syndrome in older adults: results from the Neyshabur longitudinal study on aging, Iran
Journal of Diabetes & Metabolic Disorders (2022)
-
Prevalence of metabolic syndrome and its associated risk factors among staffs in a Malaysian public university
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.