Abstract
This prospective study examined 58 eyes with branch retinal vein occlusion (BRVO) to investigate the effects of the nonperfusion area (NPA), clinical subtype, and crossing pattern on the 2-year outcomes of ranibizumab therapy for the macular edema (ME). All eyes received three initial monthly injections, followed by additional pro re nata (PRN) injections. The final best corrected visual acuity (BCVA) and ranibizumab injection number were not associated with the macular NPA or total NPA at baseline or month 12, and they showed no significant differences between the clinical subtypes. However, the incidence of neovascular changes was higher in the major BRVO group than in the macular BRVO group (P = 0.030). Twelve and 19 of the 34 eyes with major BRVO exhibited arterial overcrossing and venous overcrossing, respectively. At baseline, the total NPA did not differ according to the crossing pattern, however, the total NPA was significantly larger in the venous overcrossing group at month 12 (P = 0.047). At month 24, the incidence of neovascular changes was higher in the venous overcrossing group (P = 0.030). Following ranibizumab therapy for BRVO-associated ME, the clinical subtype and the arteriovenous crossing pattern may be associated with neovascular changes.
Similar content being viewed by others
Introduction
Branch retinal vein occlusion (BRVO) is the second-most frequent retinal vascular disorder1,2,3,4. In the majority of cases, BRVO occurs when a first- or second-order retinal vein focally occludes at an arteriovenous (AV) crossing5,6,7,8,9, and results in the development of macular edema (ME)4,10 and a retinal nonperfusion area (NPA)4,10,11,12 under upregulation of vascular endothelial growth factor (VEGF)13,14. NPA extending to the macular area can directly deteriorate the central vision15,16,17, while a large peripheral NPA can cause vitreous hemorrhage due to retinal or disc neovascularization in the chronic phase3,4,10.
Using ultra-widefield angiography, Prasad et al. reported that untreated NPA may be the source of the increase in VEGF that promotes ME18. In contrast, the RELATE trial19 and WAVE study20 reported that the addition of laser photocoagulation for NPA did not substantially affect the treatment burden or morphological outcomes of intravitreal ranibizumab injections for eyes with retinal vein occlusion. Therefore, the effects of macular and peripheral NPAs on the functional and morphological outcomes of anti-VEGF therapy for BRVO-associated ME may remain unclear.
Recent advances in optical coherence tomography (OCT) and OCT angiography have enabled detailed longitudinal and quantitative observations of retinal vasculature changes16,21,22,23. Investigations based on sequential thin sectioning with OCT24, and OCT angiography25 reported that the mechanism underlying BRVO and affecting the NPA size may differ according to the relative anatomical position of the crossing vessels. However, the duration from onset to OCT angiography examination and the duration of observation varied among patients in those studies because of the retrospective study designs; furthermore, the researchers were unable to include patients with macular BRVO or examine any neovascular changes24,25.
In the present prospective study, we included patients with both major BRVO and macular BRVO and obtained quantitative measurements of central macular NPAs using OCT angiography and total NPAs using ultra-widefield angiography. In addition, we investigated the effects of these NPA measurements, the clinical subtype of BRVO, and the vascular crossing pattern on the 2-year outcomes of ranibizumab treatment for ME, including the incidence of neovascular complications.
Results
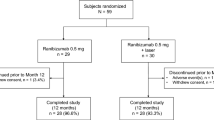
We included 58 eyes of 58 patients with treatment-naïve BRVO in the present study. Table 1 shows the clinical characteristics of the patient groups. At baseline, the mean symptom duration was 2.2 ± 1.4 months (range: 0–4 months). In accordance with previous reports9,26, we defined major BRVO as an occlusion of the temporal arcade vein or the branch that extended to the retinal periphery beyond the retinal vascular arcades9. We defined macular BRVO as an occlusion limited to a smaller venous tributary draining a section of the macula, located between the superior and inferior temporal arcades26. We included 34 eyes (58.6%) in a major BRVO group (the affected retinal areas are beyond the retinal vascular arcades) and 24 eyes (41.4%) in a macular BRVO group (the affected retinal areas are restricted within the retinal vascular arcades). Using OCT angiography images of the affected AV crossing, we included 32, 23, and three eyes in arterial overcrossing, venous overcrossing, and undetermined groups, respectively (Table 1). Intraclass correlation coefficients (ICCs) for the central macular NPA measurements in the superficial and deep plexuses were 0.992 and 0.998, respectively.
Time-Dependent Changes in Clinical Parameters
Table 2 and Fig. 1 show the time-dependent changes in best corrected visual acuity (BCVA), central foveal thickness (CFT), the central macular NPA, and the total NPA after the initial ranibizumab injections. At baseline, the mean BCVA (logarithm of the minimal angle of resolution [logMAR]) was 0.28 ± 0.27 and the mean CFT was 495.6 ± 141.0 µm. Relative to the baseline values, BCVA improved at both 12 and 24 months, while CFT significantly decreased at both time points (P < 0.001 for all). The central macular NPAs showed no significant changes from baseline to 12 or 24 months, while the total NPA was significantly larger at month 12 than at baseline in all eyes (P < 0.001, Table 2). Ultrawide-field fluorescein angiography performed at month 12 occasionally showed NPA enlargement, particularly in the peripheral retina of eyes with major BRVO (Fig. 2C,D). ICC for the total NPA measurements was 0.932.
Time-dependent changes in the best corrected visual acuity (BCVA; A), central foveal thickness (CFT; B), macular nonperfusion area (NPA; C), and total NPA (D) in patients treated with ranibizumab injections for macular edema caused by branch retinal vein occlusion (BRVO). At month 24, BCVA (logarithm of the minimum angle of resolution units) has improved while CFT has significantly decreased (P < 0.001 vs. baseline measurements for both). In contrast, the macular NPA in the superficial capillary plexus (dotted line) and deep capillary plexus (solid line) has not changed (C). The total NPA has significantly increased in the overall patient sample (circle) and in the subgroup of patients with major BRVO (square), whereas it has not changed for patients with macular BRVO (triangle; D).
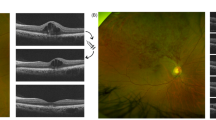
Enlargement of retinal nonperfusion areas (NPAs) according to the anatomical position of the retinal vessels at affected arteriovenous crossings in eyes with branch retinal vein occlusion (BRVO). Ultrawide-field fluorescein angiography showing an arterial overcrossing pattern (A,B) and a venous overcrossing pattern (C,D). (A,C) Images at baseline. (B,D) Images at month 12. Images inset in panels A, and C show enlargements of the affected crossing sites. In images for a representative case of venous overcrossing (C,D), a marked increase in NPA, especially in the periphery, can be observed. In contrast, NPA enlargement is unremarkable in representative images for a case of arterial overcrossing (A,B).
Prognostic Factors Associated with the Final Visual Acuity and Ranibizumab Injection Number
Table 3 shows the associations between the final BCVA and clinical factors at baseline and month12. The final BCVA (logMAR) was positively associated with age (P < 0.001), the BCVA at baseline and month 12 (P < 0.001 for both), the baseline CFT (P = 0.014), whereas it showed no association with the central macular NPA or total NPA at baseline or month 12.
Table 4 shows the associations between the number of ranibizumab injections required and clinical factors at baseline and month12. The mean number of ranibizumab injections was 5.4 ± 2.2. No factor at baseline or month 12 was found to be associated with the number of ranibizumab injections.
Comparison of Outcomes Between the Major and Macular BRVO Groups
To confirm the insignificant associations between the total NPA and other clinical outcomes, we compared the clinical outcomes between the major BRVO and macular BRVO groups (Table 5).
At baseline, both CFT and the total NPA were significantly greater in the major BRVO group than in the macular BRVO group (P = 0.023 and P = 0.001, respectively); however, BCVA showed no significant differences between groups.
At month 12, both the total NPA and the increase in NPA from baseline were significantly larger in the major BRVO group than in the macular BRVO group (50.8 ± 27.9 DA vs. 0.92 ± 2.11 DA and 30.9 ± 22.0 DA vs. 0.02 ± 0.70 DA, respectively, P < 0.001 for both). NPA in eyes with macular BRVO showed no significant changes throughout the 24-month observation period. The final BCVA and ranibizumab injection number were not significantly different between the major BRVO and macular BRVO groups. However, the incidence of neovascular changes was significantly higher in the major BRVO group (six eyes, 17.6%) than in the macular BRVO group (0 eyes, 0.0%, P = 0.030).
Comparison of Outcomes Between the Arterial Overcrossing and Venous Overcrossing Groups
To investigate the effects of the vessel position at the affected AV crossing, we compared the clinical outcomes between the arterial overcrossing and venous overcrossing groups (Table 6). To consider the effect of the clinical subtype, we separately investigated outcomes with or without macular BRVO-patients.
Among the 58 eyes included, 32 (55.2%) showed arterial overcrossing and 23 (39.7%) showed venous overcrossing on OCT angiography (Tables 1 and 6). Three (5.2%) eyes were categorized into the undetermined group, and these were excluded from all analyses comparing clinical characteristics and AV crossing patterns.
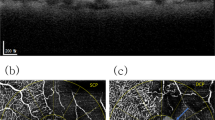
At baseline, CFT, BCVA, and the central macular NPA were not significantly different between the two groups. Likewise, the total NPA of eyes with major BRVO were not significantly different between the two groups. At month 12, BCVA, and the central macular NPA showed no significant differences between groups; however, the total NPA was significantly larger in the venous overcrossing group than in the arterial overcrossing group (55.3 ± 22.1 DA vs. 34.7 ± 27.8 DA, P = 0.047, Fig. 2). At month 24, BCVA, the central macular NPA, and the ranibizumab injection number did not differ between the crossing patterns, whereas the incidence of neovascular changes was significantly higher in the venous overcrossing group than in the arterial overcrossing group (P = 0.030, Fig. 3). None of the six eyes with venous overcrossing and neovascular changes showed PVD.
Retinal neovascularization in an eye with major branch retinal vein occlusion (BRVO) and affected venous overcrossing. At baseline (A–C), a color fundus photograph (A), an optical coherence tomography (OCT) angiograph (B), and an ultra-wide field fluorescein angiography image (C) shows marked retinal whitening, affected venous overcrossing, and a large retinal nonperfusion area (NPA) without any neovascularization, respectively. The initial Snellen visual acuity was 20/67. At month 9 (D,E), an OCT angiography image shows resolution of narrowing of the affected vein (white circle) and an improvement in the circulation of the venules and capillaries around the affected crossing site (orange circles, D). An OCT-B scan of the retinal area showing improved retinal circulation does not show any retinal neovascularization at the vitreoretinal interface (E). At month 12 (F–H), an OCT angiography image clearly shows retinal neovascularization at the periphery of the crossing site (yellow circle, F) and the vitreoretinal interface (yellow circle, G). An ultra-wide field fluorescein angiography image shows active dye leakage, consistent with retinal neovascularization (H). The patient received three ranibizumab injections (no pro re nata injections were necessary) for macular edema. The time between neovascularization and the last ranibizumab injection was approximately 10 months.
Discussion
The current prospective study examined the effects of NPA, the clinical subtype, and the AV crossing pattern on the morphological and functional outcomes, including neovascular changes, of ranibizumab treatment for BRVO-associated ME over an observational period of 24 months.
In the present study, we administered three monthly ranibizumab injections in the first 2 months, followed by PRN (3 + PRN) injections. Similar to findings in previous clinical trials27,28,29,30, BCVA improved and CFT significantly decreased from baseline during the treatment period (Table 2). The total NPA significantly increased from baseline in eyes with major BRVO, but not in eyes with macular BRVO (Tables 2 and 5, Figs 1 and 2). This suggests that NPAs resulting from BRVO tend to increase in size predominantly in the peripheral retina, not in the central macular area. Under physiological conditions, the retinal artery pressure decreases while the retinal vein pressure increases with an increase in the distance from the optic disc. In eyes with BRVO, the intravascular pressure for the affected vein is considered to increase abnormally in the periphery of the affected crossing site. Therefore, the circulatory status could be expected to deteriorate more in the periphery than in the posterior pole of the eye. Mir et al. reported that monthly ranibizumab injections decreased NPA more than PRN injections in eyes with retinal vein occlusion14. PRN injections for the treatment of ME may be inadequate for suppressing NPA growth or preventing or reversing capillary closure31,32,33.
Advanced age, an initial poor BCVA, and a greater CFT were associated with a poor final BCVA in our study (Table 3). The central macular NPA at baseline and 12 months was not associated with the final BCVA or the total number of ranibizumab injections administered during the study period (Table 3). In eyes with retinal vein occlusion, the clinical relevance of macular NPA remains controversial. Finkelstein reported that the visual prognosis of eyes with incomplete macular perfusion was better than that of eyes with complete macular perfusion12. However, it can be speculated that a macular NPA itself can deteriorate signal phototransduction from the cones to the bipolar and ganglion cells. This deteriorated signal phototransduction may have contributed to the significant negative association between the central macular NPA in the deep capillary plexus (month 24) and the final BCVA in this study (R = 0.364, P = 0.019, data not shown).
The total NPA at baseline and 12 months was not associated with the final BCVA or the total number of ranibizumab injections administered during the study period (Table 3). The insignificant association between the total NPA and the 2-year treatment outcome in this study may be supported by the results of other randomized clinical trials19,20, where the addition of laser photocoagulation to standard ranibizumab injections did not provide substantial additional benefits with regard to the functional and morphological outcomes, including the treatment burden. To verify the findings of the previous studies and the current study, we compared the treatment outcomes between major BRVO and macular BRVO. The results of these comparisons are presented in Table 5. As expected, patients with major BRVO exhibited larger NPAs than did those with macular BRVO at both baseline and month 12. However, this difference did not appear to affect the functional outcomes or the ranibizumab injection number. The total NPA and intraocular VEGF, which is presumably positively associated with the total NPA, may not be directly related to the central macular function in eyes with BRVO. Negative associations between total NPA and ME have also been reported in diabetic retinopathy34,35. Fan et al. found that the NPA for the entire retina was not significantly associated with central macular thickness or macular volume34. Silva et al. also reported that there were no significant associations between NPA and the presence of clinically significant ME or center-involved diabetic ME35. Although the pathogenesis differs between diabetic retinopathy and BRVO, these retinal vascular diseases may have a common feature in terms of the association between total NPA and ME.
In addition to the total NPA, other clinical parameters were compared between major BRVO and macular BRVO (Table 5). Interestingly, except for the initial CFT, both CFT and the central macular NPA were comparable between the major BRVO and macular BRVO groups. Hayreh et al. reported that major BRVO and macular BRVO are two distinct clinical entities4,10. However, Hayreh and Zimmerman also reported that fluorescein dye leakage and microaneurysm formation in the macular area were comparable between major BRVO and macular BRVO groups although these vascular changes at the posterior pole were more severe in the major BRVO group36. The functional outcomes of eyes with BRVO might be more strongly related to the central macular perfusion status than to the overall perfusion status. Quite obviously, the area of occlusion in a macular tributary branch vein is more subtle than that in a major arcade vein; therefore, we may have to reconsider the clinical relevance and angiographic features of macular BRVO.
In the present study, six of the 58 eyes (10.3%) showed retinal or disc neovascularization within the 24-month observational period. Previously, the RAVE trial for eyes with severe central retinal vein occlusion reported that VEGF inhibition by ranibizumab injections could delay the occurrence of neovascular complications, although it could not ameliorate the risk of such complications37. A regimen involving three initial injections followed by PRN injections, as followed in the present study, may not have been adequate for the complete suppression of neovascular complications in eyes with BRVO. The six eyes that showed neovascular changes in the current study belonged to the major BRVO group, and this is consistent with the findings in previous studies4,10. With regard to the incidence of neovascular changes, major BRVO and macular BRVO can be considered distinct entities with regard to the use of anti-VEGF agents for ME treatment. The number of ranibizumab injection required of this study appeared to be smaller compared to those of the previous studies14,38,39, a reason of which may be due to strict criteria in the additional ranibizumab injections of this study. However, we considered that it was not undertreatment at least for the treatment ME because the final BCVAs of this study were not inferior to those of previous large cohort study14,39,40.
Relative to fluorescein angiography or alternative modalities, OCT angiography is advantageous because of its high depth resolution40, which was useful for determining the anatomical positions of the retinal vessels at affected AV crossings in the present study. Similar to the findings in a previous OCT angiography study25, we observed that the OCT angiography-determined AV crossing pattern was significantly associated with the total NPA and the central macular NPA (Table 6). Using OCT B-scan images of the affected AV crossing, Muraoka et al. reported that occluded veins at the crossing were compressed and obstructed between ILM and the arterial wall in eyes with venous overcrossing, while the venous lumen was generally preserved in eyes with arterial overcrossing24. We speculated that these findings could explain the reasons for a larger NPA in eyes with venous overcrossing and a smaller NPA in eyes with arterial overcrossing on OCT angiography. The occluded vein in a venous overcrossing pattern may be too narrow to be clearly detected by previous imaging modalities, and this may be a reason for the disparity in the crossing pattern frequency between previous studies7,8,9 and more recent studies based on OCT or OCT angiography24,25.
In our major BRVO group, the final total NPA was significantly larger in eyes with venous overcrossing than in eyes with arterial overcrossing (Table 6). The markedly narrowed veins at the affected AV crossing, as previously demonstrated by OCT B-scans24 and OCT angiography25, may have contributed to the larger NPAs observed in eyes with venous overcrossing in our study. The crossing pattern were not associated with the final BCVA, and the ranibizumab injection number. However, it was significantly associated with the incidence of neovascular changes. All six eyes with neovascular changes in our study showed venous overcrossing. This suggests that eyes with BRVO and venous overcrossing but no PVD are at a higher risk of neovascularization, regardless of treatment with anti-VEGF injections, if the treatment target is suppression of ME, not neovascularization. To prevent neovascular changes, laser photocoagulation for peripheral NPA may be clinically important as an adjunct to anti-VEGF therapy for the management of ME.
The Branch Vein Occlusion Study previously classified the nonischemic type as that in which the NPA was less than five disc diameters in diameter; the ischemic type was classified as that in which the NPA was more than five disc diameters in diameter, using panoramic images made by five conventional fundus photographs41. However, recent clinical settings involving common use of ultra-widefield fluorescein angiography, we have been able to detect peripheral retinal lesions more easily than in previous clinical settings without ultra-widefield fluorescein angiography. If the present study had used the previous criteria, most patients with major BRVO would be classified into the ischemic type. Additionally, in recent BRVO treatments, we have aggressively used anti-VEGF agents that strongly inhibit neovascular complications. In the context of recent clinical settings involving the use of ultra-widefield fluorescein angiography or anti-VEGF agents, the previous criteria41 appear to be incompatible with modern clinical practice for BRVO. In this study, we thus quantified the NPA areas and statistically analyzed these measurements without using the previous criteria.
The present study has some limitations. First, the sample size was small and the treatment regimen was the same for all eyes (three injections in the initial 2 months followed by PRN injections). Therefore, we could not compare outcomes by using a consistent monthly injection regimen. In addition, the effect of this anti-VEGF agent on the retinal vasculature remains unknown, and we did not include a control group of eyes that did not receive ranibizumab treatment. Second, unequal magnification is necessary in ultra-widefield imaging, particularly for the peripheral retina, because of the need to accommodate the spherical shape of the fundus. In this study, we measured peripheral NPA without performing any correction because we assumed that the degree of image distortion would be constant among participants. Third, because the status of systemic hypertension was not evaluated in detail, its association with retinal vasculature changes remains unclear. Fourth, to obtain higher-resolution OCT angiograms, we used a viewing angle of 3 × 3-mm2 (the smallest viewing angle) and only examined the center of the macular area. However, the macula includes a larger area of the retina than the area sampled in our study. Finally, we did not take intraocular samples or measure VEGF levels in our patient group. Therefore, we were unable to investigate the association between NPA and VEGF levels.
In conclusion, the findings of the current prospective study suggest that advanced age, a poor baseline visual acuity, and a greater CFT are associated with for a worse final BCVA in eyes with BRVO-associated ME treated by ranibizumab (3 + PRN injections). In contrast, the macular NPA or the total NPA may not be associated with the functional outcomes or the treatment burden. These speculations are supported by our finding of no significant differences in clinical outcomes between eyes with major BRVO and those with macular BRVO. Moreover, the total NPA was significantly larger in eyes with venous overcrossing than in eyes with arterial overcrossing. Therefore, the clinical BRVO subtype and the AV crossing pattern may be associated with a risk of neovascular changes, regardless of treatment with ranibizumab injections for ME. An understanding of the association between the NPA size and the AV crossing pattern would contribute to the development of an optimized treatment protocol for individual cases of BRVO. To confirm the current findings and develop a novel treatment regimen for lowering the risk of neovascular complications, further prospective studies should be conducted with a larger cohort and a longer follow-up duration.
Methods
Patients
This prospective study was approved by the Institutional Review Board (IRB) of Kyoto University Graduate School of Medicine, Kyoto, Japan, and adhered to the tenets of the Declaration of Helsinki (clinical trial registration numbers: NCT01968616; date of registration: 24/October/2013, last updated: 20/October/2017). Written informed consent was obtained from each participant during the initial visit prior to enrollment in this study.
We included patients who presented at our clinic with acute BRVO involving the macular area, with a symptom duration of less than 4 months before the initial examination, between September 2013 and July 2015. We excluded eyes in which the occluded site was located within the optic disc or on the disc margin. In addition, we excluded eyes with hemicentral retinal vein occlusion, those with multiple retinal vein occlusions, those that received any interventions for ME prior to the study period, those with coexisting ocular diseases (diabetic retinopathy, hypertensive retinopathy, retinal macroaneurysm, glaucoma, or epiretinal membrane), those with keratoconus, those with high myopia (worse than −6 diopters), those with high astigmatism (worse than ±3 diopters), and those with poor-quality OCT angiograms (signal strength index, <50) due to eye movement or media opacities. Eventually, 58 eyes of 58 consecutive patients met these inclusion/exclusion criteria and were included in our study. Because of partial overlap between the recruitment period for the current study and our previously published study, we included three patients from the previous study25.
Examinations and Treatments for ME
At the initial visit, each patient underwent a comprehensive ophthalmic examination, which included measurement of the BCVA using a Landolt chart, 45° digital fundus photography (TRC-50LX; Topcon, Tokyo, Japan; 3,216 × 2,136 pixels), and OCT imaging (Spectralis HRA + OCT, Heidelberg Engineering, Heidelberg, Germany).
All eyes received three monthly ranibizumab injections, and were examined every month for 24 months. We administered additional injections if cystoid spaces and/or serous retinal detachment, extending to the foveal center and the unaffected side became evident on OCT sections. No eyes received any other form of treatment, such as scatter or grid laser photocoagulation, steroid therapy, surgical intervention, or intravitreal injections of anti-VEGF agents other than ranibizumab.
To evaluate the perfusion status of the entire retina, we performed ultra-widefield fluorescein angiography (Optos 200Tx imaging system, Optos PLC, Dunfermline, UK) before and 1 year after the initial ranibizumab injections or when fresh retinal hemorrhage, peripheral white vessels, or neovascular changes appeared during routine ophthalmic examinations.
OCT Evaluation of the Foveal Thickness
We measured the CFT using macular volume scans obtained by OCT. A whole-retinal thickness map centered on the foveal center was created using the Early Treatment Diabetic Retinopathy Study grid. In cases where we obtained an OCT B-scan with a segmentation error, we manually corrected the delineated line at each B-scan. We obtained retinal thickness values for each grid using the manufacturer’s built-in software (Spectralis Acquisition and Viewing Modules, version 6.0, Heidelberg Engineering, Heidelberg, Germany); CFT was defined as the average value derived from retinal thickness measurements for the central grid.
OCT Angiography of the Central Macular Area and Affected AV Crossing
We evaluated the central macular perfusion status at every visit by scanning a central 3 × 3-mm2 area of the macula using OCT angiography (RTVue XR Avanti, Optovue Inc., Fremont, CA). We also used this tool to classify the relative anatomical vessel positions (arterial or venous overcrossing) at affected AV crossings.
The built-in software in the OCT angiography device automatically recognized the inner limiting membrane (ILM) and inner plexiform layer (IPL). We obtained images of the superficial capillary layer using previously published methods16,25. Briefly, the slab containing the superficial capillary plexus was considered to extend from ILM to 15 μm below IPL, while that containing the deep capillary plexus was considered to extend from 15 μm to 70 μm below IPL.
Measurement of the Central Macular NPA Using OCT Angiography
To avoid segmentation errors in each retinal layer42, we measured NPA using OCT angiography when we observed substantial resolution of ME on OCT sections. We defined the central macular NPA as the capillary dropout area within a 3 × 3-mm2 section, including the foveal avascular zone. Two fully trained retina specialists (YI-M, YI) blinded to all clinical information about the affected eyes independently reviewed the presence or absence of capillary dropouts in the 3 × 3-mm2 section. The central macular NPA was then measured using the manufacturer’s built-in software (AngioVue Clinical Release, v2015.100.0.3, Optovue Inc.). We corrected the NPA measurements for axial length-related magnification using a modified Littmann formula, which applies measurements of the axial length, flatter and steeper meridians, and spherical equivalent (Bennett procedure)16,25,43.
The detection of central macular NPAs was partially based on subjective judgments. Therefore, to confirm the validity of central macular NPA measurements in the superficial and deep capillary plexuses, we calculated the ICC for 58 measurements derived for the 58 eyes by three independent examiners.
Classification of the AV Crossing Pattern Using OCT Angiography
We classified the relative anatomical vessel positions at the affected AV crossings into three groups: arterial overcrossing, venous overcrossing, and undetermined. Arterial overcrossing was defined when the affected artery coursed over the adjacent vein, while venous overcrossing was defined when the affected vein coursed over the adjacent artery. We classified the pattern on the basis of OCT angiograms and the B-scan images of the original OCT scans.
Because classification of the AV crossing pattern was also subjective, we obtained different judgments of the AV crossing pattern in order to avoid misclassification or to minimize classification into the undermined group. Two independent retinal specialists (YI-M and YI) determined the pattern on each image. When the two raters recorded different patterns, a senior retinal specialist (YM) determined the final pattern.
Measurement of the Total NPA Using Ultra-Widefield Fluorescein Angiography
On ultra-widefield angiography performed 1 min after dye injection, we detected NPA based on subjective judgments for each patient, and measured the NPA size in pixels using a software plugin in the ImageJ program (National Institutes of Health, Bethesda, MD, USA)25. For measurement of total NPA, we measured disc area (DA) in pixels for each patient (Supplementary Information), and calculated the mean DA. Using the value of the average DA, total NPA was expressed in units of DA.
To confirm the validity of the total NPA measurements, we calculated the interclass correlation coefficient (ICC) for 58 measurements obtained for the 58 eyes by three independent examiners.
Determination of the Presence or Absence of Posterior Vitreous Detachment (PVD)
We determined the presence or absence of PVD during the initial examination for each patient. PVD was considered present if we observed a Weiss ring on fundus ophthalmoscopy or ultra-widefield angiography and complete absence of the vitreous cortex on a peripapillary circular OCT scan.
Statistical Analysis
We statistically analyzed the acquired data using PASW Statistics version 18.0 (SPSS, Chicago, IL). All continuous values are presented as mean ± standard deviation. We obtained BCVA values using a Landolt chart and subsequently converted them to logMAR units for statistical analysis. Comparisons between two groups were performed using unpaired t-tests. Differences in each parameter among the different examination time points (baseline and months 12 and 24 after the initial injections) were determined using repeated measures analysis of variance, with a post hoc paired t-test used to compare each baseline measurement with each measurement after the initial ranibizumab injections. We used chi-square tests to determine significant differences in the sampling distribution and calculated ICCs to examine the reproducibility and validity of the NPA measurements obtained via fluorescein angiography and OCT angiography. A P-value of <0.05 was considered statistically significant. We determined statistical significance after Bonferroni correction for the post hoc test.
YI-M, and YM had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Klein, R., Klein, B. E., Moss, S. E. & Meuer, S. M. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 98, 133–141 (2000).
Klein, R., Moss, S. E., Meuer, S. M. & Klein, B. E. The 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye Study. Arch Ophthalmol 126, 513–518 (2008).
Jonas, J., Paques, M., Mones, J. & Glacet-Bernard, A. Retinal vein occlusions. Dev Ophthalmol 47, 111–135 (2010).
Hayreh, S. S. Ocular vascular occlusive disorders: natural history of visual outcome. Prog Retin Eye Res 41, 1–25 (2014).
Frangieh, G. T., Green, W. R., Barraquer-Somers, E. & Finkelstein, D. Histopathologic study of nine branch retinal vein occlusions. Arch Ophthalmol 100, 1132–1140 (1982).
Osterloh, M. D. & Charles, S. Surgical decompression of branch retinal vein occlusions. Arch Ophthalmol 106, 1469–1471 (1988).
Duker, J. S. & Brown, G. C. Anterior location of the crossing artery in branch retinal vein obstruction. Arch Ophthalmol 107, 998–1000 (1989).
Weinberg, D., Dodwell, D. G. & Fern, S. A. Anatomy of arteriovenous crossings in branch retinal vein occlusion. Am J Ophthalmol 109, 298–302 (1990).
Feist, R. M., Ticho, B. H., Shapiro, M. J. & Farber, M. Branch retinal vein occlusion and quadratic variation in arteriovenous crossings. Am J Ophthalmol 113, 664–668 (1992).
Hayreh, S. S. & Zimmerman, M. B. Branch retinal vein occlusion: natural history of visual outcome. JAMA Ophthalmol 132, 13–22 (2014).
Rogers, S. L. et al. Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology 117, 1094–1101 (2010).
Finkelstein, D. Ischemic macular edema. Recognition and favorable natural history in branch vein occlusion. Arch Ophthalmol 110, 1427–1434 (1992).
Campochiaro, P. A., Aiello, L. P. & Rosenfeld, P. J. Anti-Vascular Endothelial Growth Factor Agents in the Treatment of Retinal Disease: From Bench to Bedside. Ophthalmology 123, S78–S88 (2016).
Mir, T. A. et al. Changes in Retinal Nonperfusion Associated with Suppression of Vascular Endothelial Growth Factor in Retinal Vein Occlusion. Ophthalmology 123, 625–634 (2016).
Ota, M. et al. Retinal sensitivity after resolution of the macular edema associated with retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 250, 635–644 (2012).
Kadomoto, S. et al. Evaluation of macular ischemia in eyes with branch retinal vein occlusion: an optical coherence tomography angiography study. Retina 38, 272–282 (2018).
Manabe, S. et al. Association between parafoveal capillary nonperfusion and macular function in eyes with branch retinal vein occlusion. Retina 10, 10 (2016).
Prasad, P. S., Oliver, S. C., Coffee, R. E., Hubschman, J. P. & Schwartz, S. D. Ultra wide-field angiographic characteristics of branch retinal and hemicentral retinal vein occlusion. Ophthalmology 117, 780–784 (2010).
Campochiaro, P. A. et al. Scatter photocoagulation does not reduce macular edema or treatment burden in patients with retinal vein occlusion: the RELATE trial. Ophthalmology 122, 1426–1437 (2015).
Wykoff, C. C. et al. Peripheral Laser for Recalcitrant Macular Edema Owing to Retinal Vein Occlusion: The WAVE Trial. Ophthalmology 124, 919–921 (2017).
Sellam, A. et al. Qualitative and quantitative follow-up using optical coherence tomography angiography of retinal vein occlusion treated with anti-VEGF: optical coherence tomography angiography follow-up of retinal vein occlusion. Retina 28, 28 (2016).
Suzuki, N. et al. Microvascular abnormalities on optical coherence tomography angiography in macular edema associated with branch retinal vein occlusion. Am J Ophthalmol 161, 126–132 (2016).
Tsuboi, K., Ishida, Y. & Kamei, M. Gap in capillary perfusion on optical coherence tomography angiography associated with persistent macular edema in branch retinal vein occlusion. Invest Ophthalmol Vis Sci 58, 2038–2043 (2017).
Muraoka, Y. et al. Morphologic and functional changes in retinal vessels associated with branch retinal vein occlusion. Ophthalmology 120, 91–99 (2013).
Iida, Y. et al. Morphologic and functional retinal vessel changes in branch retinal vein occlusion: an optical coherence tomography angiography study. Am J Ophthalmol 182, 168–179 (2017).
Joffe, L., Goldberg, R. E., Magargal, L. E. & Annesley, W. H. Macular branch vein occlusion. Ophthalmology 87, 91–98 (1980).
Heier, J. S. et al. Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 119, 802–809 (2012).
Brown, D. M. et al. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology 118, 1594–1602 (2011).
Campochiaro, P. A. et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: the 24-week results of the VIBRANT study. Ophthalmology 122, 538–544 (2015).
Miwa, Y. et al. Ranibizumab for macular edema after branch retinal vein occlusion: one initial injection versus three monthly Injections. Retina 37, 702–709 (2017).
Lu, M. et al. VEGF increases retinal vascular ICAM-1 expression in vivo. Invest Ophthalmol Vis Sci 40, 1808–1812 (1999).
Miyamoto, K. et al. Vascular endothelial growth factor (VEGF)-induced retinal vascular permeability is mediated by intercellular adhesion molecule-1 (ICAM-1). Am J Pathol 156, 1733–1739 (2000).
Liu, Y. et al. Reversible retinal vessel closure from VEGF-induced leukocyte plugging. JCI Insight 2, 95530 (2017).
Fan, W. et al. Distribution of nonperfusion area on ultra-widefield fluorescein angiography in eyes with diabetic macular edema: DAVE study. Am J Ophthalmol 180, 110–116 (2017).
Silva, P. S. et al. Diabetic retinopathy severity and peripheral lesions are associated with nonperfusion on ultrawide field angiography. Ophthalmology 122, 2465–2472 (2015).
Hayreh, S. S. & Zimmerman, M. B. Fundus changes in branch retinal vein occlusion. Retina 35, 1016–1027 (2015).
Brown, D. M. et al. Ranibizumab in preproliferative (ischemic) central retinal vein occlusion: the rubeosis anti-VEGF (RAVE) trial. Retina 34, 1728–1735 (2014).
Sophie, R. et al. Long-term outcomes in ranibizumab-treated patients with retinal vein occlusion; the role of progression of retinal nonperfusion. Am J Ophthalmol 156, 693–705 (2013).
Clark, W. L. et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: 52-week results of the VIBRANT study. Ophthalmology 123, 330–336 (2016).
Coscas, F. et al. Optical coherence tomography angiography in retinal vein occlusion: evaluation of superficial and deep capillary plexa. Am J Ophthalmol 161, 160–171 (2016).
Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol 104, 34–41 (1986).
Matt, G. et al. Comparison of retinal thickness values and segmentation performance of different OCT devices in acute branch retinal vein occlusion. Eye 25, 511–518 (2011).
Miyata, M. et al. Detection of myopic choroidal neovascularization using optical coherence tomography angiography. Am J Ophthalmol 165, 108–114 (2016).
Acknowledgements
This study was supported, in part, by the Japan Society for the Promotion of Science (JSPS), Tokyo, Japan (Grant-in-Aid for Scientific Research, no. 21592256); the Japan National Society for the Prevention of Blindness, Tokyo, Japan; Novartis Pharma K.K., Tokyo, Japan; and the Innovative Techno-Hub for Integrated Medical Bio-Imaging of the Project for Developing Innovation Systems, from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan. No additional external funding was received for this study. The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Y.I.-M. and Y.M. wrote the manuscript; Y.I.-M., Y.M., Y.I. analyzed data; Y.I.-M.,Y.M. and Y.I. prepared figures; Y.I.-M. and Y.M. provided conception and design of research. Y.I., S.O., T.M., K.S. and A.T. edited and reviewed the manuscript. All authors accepted the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
None of the authors has a proprietary interest in any product described in the article. Yuki Muraoka received grant support from Bayer, Novartis Pharma K.K., Senju and Nidek. Sotaro Ooto received grant support from Alcon Pharma, Bayer, Santen, Senju, Japan Focus, Nidek, and Pfizer. Kiyoshi Suzuma received grant support from Novartis Pharma K.K., Bayer, Nihon Alcon, Santen, Senju, HOYA, Topcon, Nidek, SANWA KAGAKU, SANOFI, Kowa-Pharmaceutical, Bausch & Lomb, Otsuka Pharmaceutical, Pfizer, and WAKAMOTO. Tomoaki Murakami received grant support from Bayer, Novartis Pharma K.K., Santen, Senju, Kowa-Pharmaceutical, and SANWA KAGAKU, as well as financial support from Novartis Pharma K.K. Akitaka Tsujikawa received grant support from Pfizer, Novartis Pharma K.K., Bayer, Alcon, Santen, Senju, Nidek, AMO Japan, Kowa-Pharmaceutical, Chugai Pharmaceutical, SANWA KAGAKU, Kyoto Drug Discovery & Development, HOYA, Otsuka Pharmaceutical, Daiichi-Sankyo Company, WAKAMOTO, Johnson and Johnson, and Janssen Pharmaceutical K.K., as well as financial support from Novartis Pharma K.K., Bayer, Santen, Canon, Alcon, Alcon Pharma, HOYA, Kowa-Pharmaceutical, Pfizer, AMO Japan, Senju, WAKAMOTO, JMIA, Tomey Corporation, JFC Sales Plan, and Atsuzawa Prosthese Osaka. The following authors have no conflicts of interest to declare: Yuko Iida-Miwa, Yuto Iida.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iida-Miwa, Y., Muraoka, Y., Iida, Y. et al. Branch Retinal Vein Occlusion: Treatment Outcomes According to the Retinal Nonperfusion Area, Clinical Subtype, and Crossing Pattern. Sci Rep 9, 6569 (2019). https://doi.org/10.1038/s41598-019-42982-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-42982-5
This article is cited by
-
Classification of good visual acuity over time in patients with branch retinal vein occlusion with macular edema using support vector machine
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Factors associated with extremely poor visual outcomes in patients with central retinal vein occlusion
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.